Marjan Asadollahi1, Mahtab Ramezani1, Ehsan Sakhaii1 and Ehsan Karimialavijeh2*
1Shahid Beheshti University of Medical Sciences, Loghman Hakim Hospital, Iran
2Tehran University of Medical sciences, Shariati Hospital, Kargar Ave, Tehran, Iran
Corresponding Author:
Ehsan Karimialavijeh
Tehran University of Medical sciences
Shariati Hospital, Kargar Ave
Tehran, 14117-13137, Iran
Tel: +982161192240
Fax: +982166904848
E-mail: e-karimi@sina.tums.ac.ir
Received date: June 03, 2016; Accepted date:July 11, 2016; Published date: July 15, 2016
Citation: Asadollahi M, Ramezani M, Sakhaii E, et al. A Case of Post-traumatic Cerebral Venous Sinus Thrombosis Special Issue. J Neurol Neurosci. 2016, 7:4.
Keywords
Cerebral venous thrombosis; Head injury
Background
Cerebral venous sinus thrombosis (CVST) is a potentially lifethreatening condition. It may lead to a considerable mortality if not recognized and treated in a timely manner [1,2]. Nonetheless, Due to its nonspecific clinical presentations, early diagnosis is not always possible. There are several predisposing factors for CVST, of which the most common conditions are hereditary thrombophilia, post-operative states; and use of oral contraceptives [3]. Hereby we report an interesting case of CVST following brain contusion. It is important to always keep a high degree of suspicion for CVST, even when other diagnoses seem more possible.
Case Presentation
A 21-year-old male was admitted to our hospital because of horizontal diplopia and headache. He had a history of head trauma 12 days prior to his admission. He did not have any other problem including nausea, vomiting, seizure or loss of consciousness in the past 12 days.
In systemic examination, the only remarkable finding was the presence of several stitches in his right occipital region. In neurological examination, the patient had bilateral sixth cranial nerve palsy. Fondoscoy examination revealed papilledema and retinal hemorrhage. Other neurological examinations were normal.
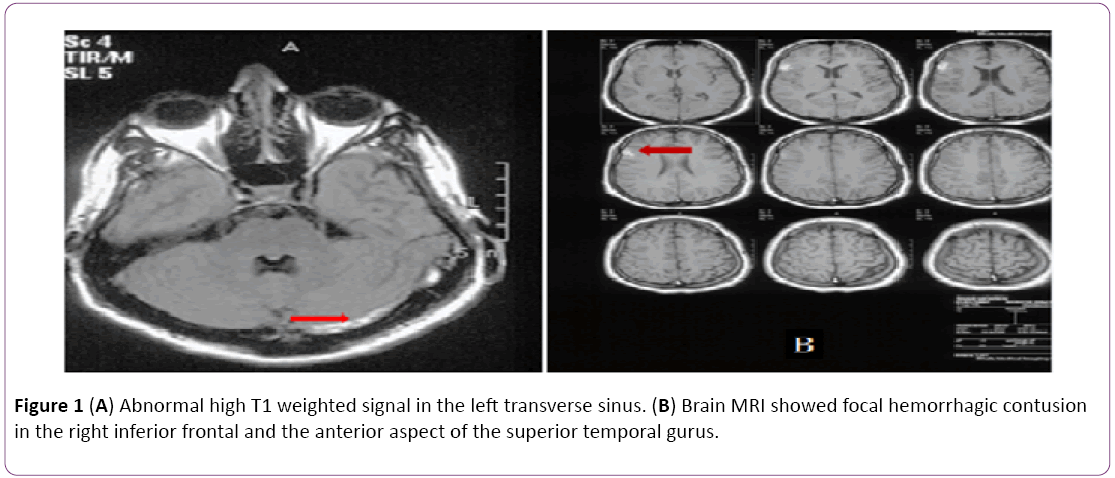
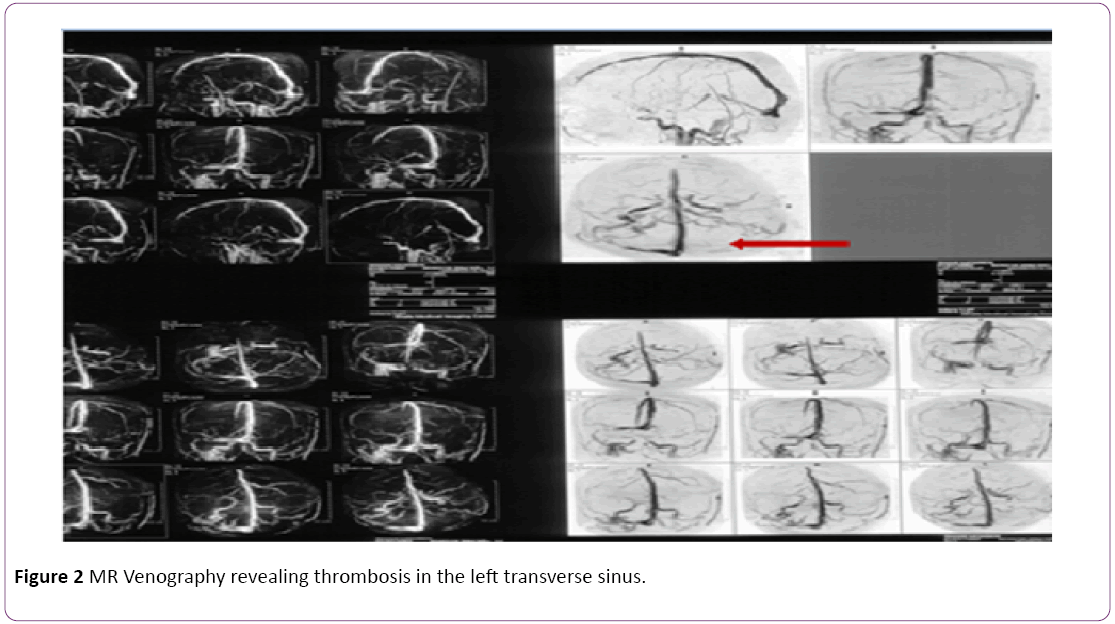
Brain Computer tomography (CT) scan showed a small hemorrhagic area in the right frontoparietal cortex compatible with cerebral contusion, without any significant edema or mass effect. Still, the patient’s symptoms could not be explained by this small lesion. In order to detect any additional lesions explaining the patient’s symptoms, Brain Magneticresonance imaging (MRI) was performed. Brain MRI showed a small cortical frontoparietal lesion in the right side of the brain, compatible with the cerebral contusion. In addition abnormal hyper signal changes were present in the left transverse sinus in T1 and T2 sequences, which were compatible with cerebral venous thrombosis (Figures 1A and 1B). Following this, MR venography revealed cerebral venous sinus thrombosis (CSVT) in the left transverse sinus (Figure 2).
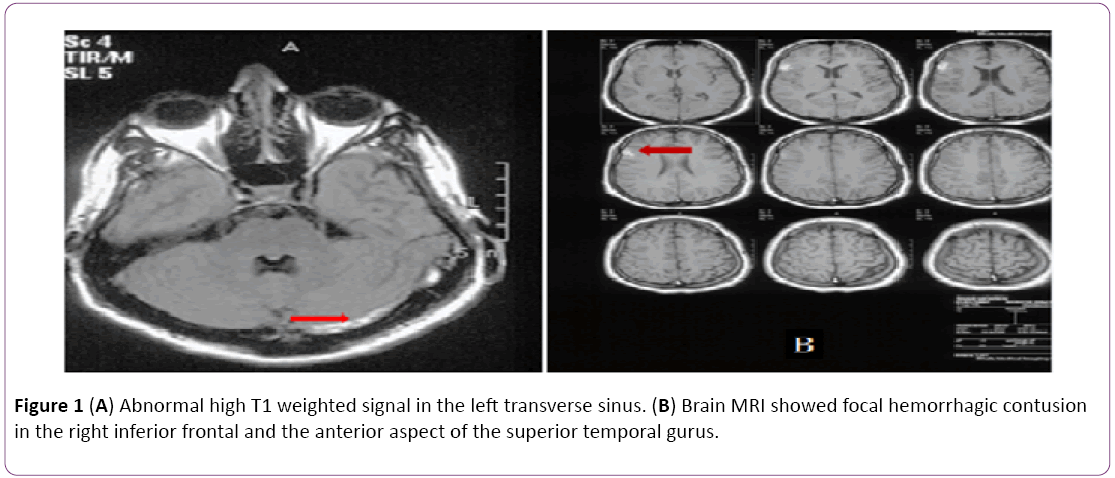
Figure 1: (A) Abnormal high T1 weighted signal in the left transverse sinus. (B) Brain MRI showed focal hemorrhagic contusion in the right inferior frontal and the anterior aspect of the superior temporal gurus.
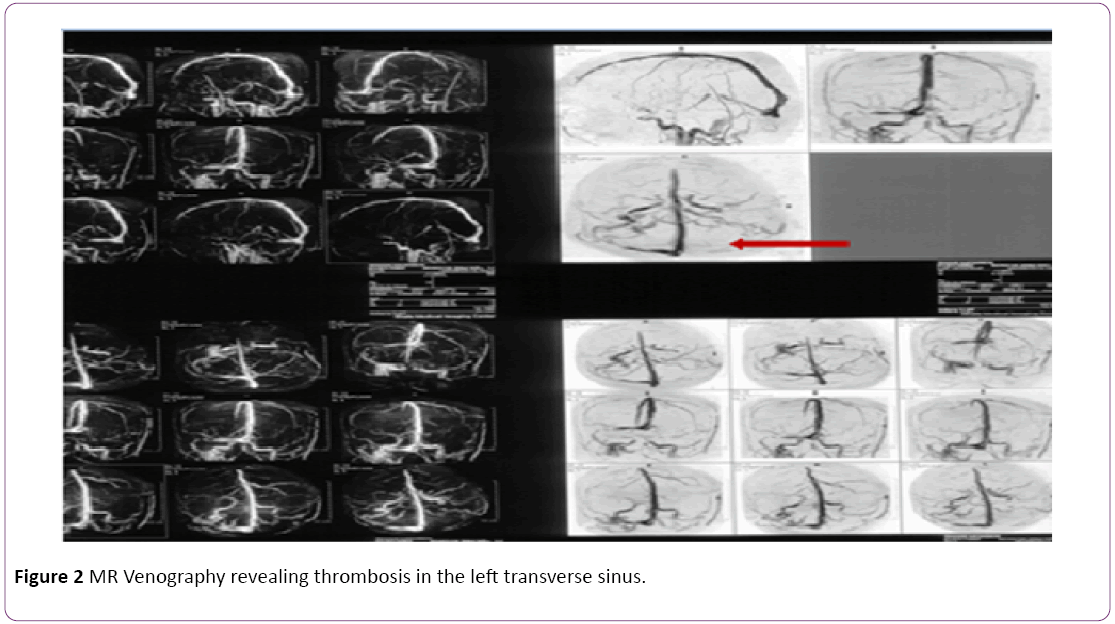
Figure 2: MR Venography revealing thrombosis in the left transverse sinus.
In order to exclude any associated infections in CVST we performed Lumbar puncture on patient. The lumbar puncture demonstrated increased intracranial pressure with an opening pressure of 25 cm H2O (normal 5–20 cm H2O) with normal CSF analysis.
Initial laboratory values revealed normal liver, thyroid and renal function, electrolyte levels were also within normal limits and there was no evidence of acute infection.
Results of thrombophilia screen tests revealed normal levels of anti-thrombin III, factor V Leiden, protein C activity, free protein S antigen, anti-phospholipid antibody, lupus anticoagulant and anti-cardiolipin antibody.
Anticoagulation therapy was initiated for the patient. The anticoagulation regimen was consisted of intravenous Heparin (80 IU/kg bolus , and 18 IU/kg/hour continues infusion), after 24 hours warfarin 5 mg p. o. daily was added to the treatment. After five days of admission we discontinued the intravenous heparin. 2 weeks after admission, the headache and diplopia were resolved completely. Fortunately the patient did not develop any complication of anticoagulation therapy especially cerebral hemorrhage.
Discussion
Cerebral venous thrombosis is a common disease in medical practice. This disorder is potentially fatal but treatable and sometimes is overlooked. Most patients with CVST present with symptoms of elevated intracranial pressure. Clinical manifestations of CVST are often nonspecific, making it difficult to diagnose the condition definitely especially in uncommon backgrounds [4]. There are several predisposing factors for CVST but the most common ones include hereditary thrombophilia, pregnancy and puerperium, post-operative state and use of OCP.
CVT after head trauma is not common. Dalgic et al. reported a case of CVST following minor head trauma. The patient did not have any skull fracture on Brain CT-Scan but he had intracerebral hematoma on right posterior parietal cortical area. They concluded that post traumatic CVST is usually accompanied by depressed skull fracture, epidural or subdural hematoma [5].
Delmando et al. identified 15.9% CVST in 195 patients with acute blunt head trauma. The majority of their patients had skull fracture with extension to at least one dural venous or jugular bulb. In their study they did not identified any case of traumatic CVT in the absence of skull fracture [6].
Dobbs et al. presented a case of traumatic extradural hematoma successfully evacuated and then the patient deteriorated and died because of CVST. They concluded that CVST is a rare important cause of deterioration in posttraumatic head injury [7].
Our patient had interesting points. First, there was development of post traumatic CVST without associated skull fracture (contrary to the instances previously described in literature). Another interesting point was that the patient had coincidental cerebral contusion on brain imaging, making it difficult to diagnose CVST in his clinical setting.
Conclusion
Although, Head trauma is a rare cause of CVST it should be considered in any head traumatic patient who develops symptoms of increased intracranial pressure.
Conflict of Interest
Authors declare that there is no conflict of interest in regard of this paper.
10579
References
- Rael JR (1997) Direct thrombolysis of superior sagittal sinus thrombosis with coexisting intracranial hemorrhage. American Journal of Neuroradiology 18: 1238-1242.
- Spearman MP (1997) Endovascular thrombolysis in deep cerebral venous thrombosis. American Journal of Neuroradiology 18: 502-506.
- Khatri IA, Alkawi A, Ilyas A (2006) Unusual causes of cerebral venous thrombosis.J Pak Med Assoc56: 501-505.
- Chiewvit P, Piyapittayanan S, Poungvarin N (2011) Cerebral venous thrombosis:diagnosis dilemma. Neurology International 3: e13.
- Dalgic A, Secer M, Ergungor F (2008) Dural sinus thrombosis following head injury: report of two cases and review of literature. Turkish Neurosurgery 18: 70-77.
- Delgado Almandoz JE, Kelly HR, Schaefer PW (2010) Prevalence of traumatic dural venous thrombosis in high-risk acute blunt head trauma patients evaluated with multi-detector CT Venography. Radiology 255: 570-577.
- Dobbs TD, Barber ZE, Squier WL, Green AL (2012) Cerebral venous sinus thrombosis complicating traumatic head injury. J ClinNeurosci 19: 1058-1059.