Keywords
Obsessive-Compulsive-Disorder (OCD); Positive and Negative-Syndrome- Scale (PANSS); Quality-of-life (QOL); Schizophrenia (SCH); Yale-Brown Obsessive- Compulsive-Scale (Y-BOCS)
Abbreviations
DCR: Diagnostic Criteria for Research; DSM: Diagnostic and Statistical manual of Mental disorders (Edition IV/5); PANSS: Positive and Negative Syndrome Scale; Y-BOCS: Yale Brown Obsessive Compulsive Scale; QOL-D1: Physical Domain; QOL-D2: Psychological Domain; QOL-D3: Social Domain; QOL-D4: Environmental Domain; BAS: Burden Assessment Schedule; ICD-10: International Statistical Classification of Diseases and Related Health Problems – Tenth Revision; QOL: Quality of Life; WHO: World Health Organization; WHO ICF: The World Health Organization International Classification of Functioning; FBIS: Family Burden Interview Schedule; ECI: Experience of Caregiving Inventory; CCL: Coping Checklist; SSQ: Social Support Questionnaire; GHQ-12: General Health Questionnaire-12a.
Introduction
The Swiss psychiatrist Eugen Bleuler coined the word schizophrenia in 1908. It is characterized by the disintegration of function among thinking, memory, perception and personality. In this condition intellectual capacity and consciousness are usually restored. But a certain cognitive deficit may develop on the course of time [1]. According to the World Health Organization, the prevalence of schizophrenia is homogeneous globally [2]. On the other hand, Obsessive Compulsive Disorder (OCD) is a debilitating neuropsychiatric condition characterized by intrusive unwanted thoughts (obsessions). It may also be evolved with some repetitive, compulsive behaviours, or mental rituals. Social stigma against people with mental disorders prevents them from accessing and receiving the help they need to stay healthy [3]. Generally, stigma is a social practice experienced and characterized by exclusion, rejection and blame or depreciation about a person. The quality of life (QOL) is hampered in this disease condition. The character of well-being and health status of an individual is the main determinants of his/her QOL [4].
The World Health Organization International Classification of Functioning (ICF), disability, and Health are a model designed to provide a description of health and health states of a person [5]. Burden refers to the difficulties or adverse event that affects the lives of psychiatric patients. Caregiver is usually recognized as an individual who has the responsibility of dealing with the physical and psychological needs of the dependent patient. During the long period of care-giving procedure caregiver remain at a great risk of mental and physical health anomalies. Several studies have been reported on the incidents of stigmatization of people with mental illnesses and its adverse consequences. Scanty studies have addressed the issue in developing-societies. Few comparative studies of family burden between caregivers of schizophrenia patients and caregivers of obsessive-compulsive disorder (OCD) patients have been performed. For these types of study, patients were evaluated with burden assessment schedule (BAS) with standard protocol. The objectives of the current study were to compare stigma between caregivers of schizophrenia and obsessive compulsion disorder and to compare QOL, family burden in care-givers between patients of schizophrenia and obsessive compulsion disorder. Efforts were made to determine the correlation between severity of illness and stigma, QOL and family burden. Relevance of socio-demographic variables and different clinical variables on schizophrenia and obsessivecompulsive disorder were also tested by the application of suitable statistical procedure.
Materials and Methods
Ethical clearance
The protocol was approved by the ethics committee of institute of post graduate medical education and research (IPGMER), Calcutta. Informed consent was taken from each patient and caregivers participating in the study.
This is a descriptive and cross-sectional study. Sixty patients and their caregivers (30 schizophrenia patients with caregivers and 30 OCD patients with caregivers) were included in this study. Consecutive patients had been selected from the pool of outdoor patient of the Department of Institute of Psychiatry, Calcutta (West Bengal, India), a Centre Of Excellence, Institute of Post Graduate Medical Education and Research (IPGMER, Calcutta-25). The study was conducted in the period of January 2016 to October 2017.
Inclusion criteria for individuals
The following are the inclusion criteria of the patients.
• The age group of 18-55 year for both schizophrenia and OCD patients who came with caregivers in OPD. Both diseases group had been age and gender match.
• Caregiver, a key relative was defined who had cared the patient continuously for the last two years and spent a lot of time and emotion in caring the patient.
• Patients ready to give written and informed consent. Patients having continuous illness for the previous 2 years.
• Patients should be free from psychiatric co-morbidity and substance dependence. We attempted to control for severity of the illness in both the groups by recruiting at least 'moderately ill' patients so that both the groups were similar with respect to severity.
Exclusion criteria for individuals
• Psychiatric co-morbidities like substance dependence, mental retardation, bipolar disorder.
• Patients suffering from any co-morbid medical illness dementia, seizures, cerebrovascular accidents, Parkinson’s disease.
Tools used for the investigation
• ICD-10 (DCR) Diagnostic criteria for research.
• Semi structured proforma that contains details of the demographics, complete medical History of the patient, education profile of caregiver with occupation and annual income and other socio-demographic variables.
• Scales: (A) Positive and Negative Syndrome Scale (PANSS): It is a rigorous and objective method for the evaluation of positive, negative, and other syndrome dimensions in schizophrenia. The PANSS assessment is derived from behavioral information collected from a number of sources. This includes observations during the interview, a clinical interview, and reports by the primary care or hospital staff or family members. In this procedure the ratings provide summary scores on a sevenitem positive scale, a seven-item negative scale, and a 16-item general psychopathology scale. The PANSS ratings should be based on all the information relating to a specified period, normally identified as the previous week. If the item is absent, it is scored as 1; increased levels of psychopathology are assigned scores from 2 (minimal) to 7 (extreme) [6].
(B) Yale-Brown Obsessive-Compulsive Scale (Y-BOCS): This is a 10-item balanced scale designed to rate both the severity and the type of symptoms in patients with OCD. The scale includes assessments of time occupied, interference with ordinary social activities, and degree of distress, resistance, and control. This scale was designed to measure symptoms, on a scale of 0-4, and a maximum total score of 40 without being influenced by the type of obsessions or compulsions [7].
(C) Family Interview Schedule (STIGMA SECTION): It measure Stigma of the family due patient. The family interview schedule (FIS): Stigma section is an interviewer- administered scale, contained 14 items on negative, mental health related experiences. All responses will be given on a four-point scale from „not at all? to „a lot?. Where items related to situations that are not relevant to the participant (e.g.in relation to having children or seeking employment), or if a diagnosis could not have been known about in that situation, a „not applicable? option will be us [8].
(D) WHO (QOL) BREF: The WHO QOL-BREF is a 26-item, selfadministered, generic questionnaire that is a short version of the WHOQoL-100 scale which emphasizes the subjective responses of patients rather than their objective life conditions. The response options range from 1 (very dissatisfied/very poor) to 5 (very satisfied/very good). Assessments are performed over the preceding weeks. It consists of domains and facets (or sub domains). The items on 'overall rating of QOL' and subjective satisfaction with health constitute the general facet on overall rating of QOL and health. The more popular model for interpreting the scores has four domains, namely, physical health (seven items), psychological health (six items), social relations (three items), and environment (eight items) [9].
(E) Burden Assessment schedule (BAS): Caregiver's burden will be assessed with burden assessment schedule (BAS), a structured instrument with forty items. Each item is rated on a three-point scale (not at all, to some extent and very much). The items of the schedule are categorized under nine domains such as spouserelated factor, physical and mental health, external support, caregiver's routine, support of patient, taking responsibility, other relations, patients behaviour and caregiver strategy. This schedule measures both subjective as well as objective burden adequately, and, it has been proven to have good interrater reliability and face, content and criterion validity [10].
Method
Study subjects have been selected by consecutive sampling from patient coming to the OPD of the Institute of Psychiatry Diagnosed by two consultant psychiatrists as having schizophrenia and obsessive-compulsive disorder by applying ICD-10. The severity of OCD was tested by using Y-BOCS and the severity of schizophrenia was evaluated by using PANSS.
Caregivers of two groups have been screened with family interview schedule (FIS): Stigma section to determine stigma of the respective group. WHO QOL BREF scales had been applied to assess quality of life (QOL) of both patient groups. Burden Assessment Schedule (BAS) had been applied to the caregiver to assess family burden.
Statistical analysis
Data analysis was done by SPSS, version 20.0. By using parametric statistics, i.e., t-test to assess the level of significant difference between the two groups (Schizophrenia and OCD). Chi-square was used for socio-demographic nonparametric variables. Pearson’s correlation test was done to evaluate the dependence of different socio-demographic and clinical variables in relation to the disease severity.
Results
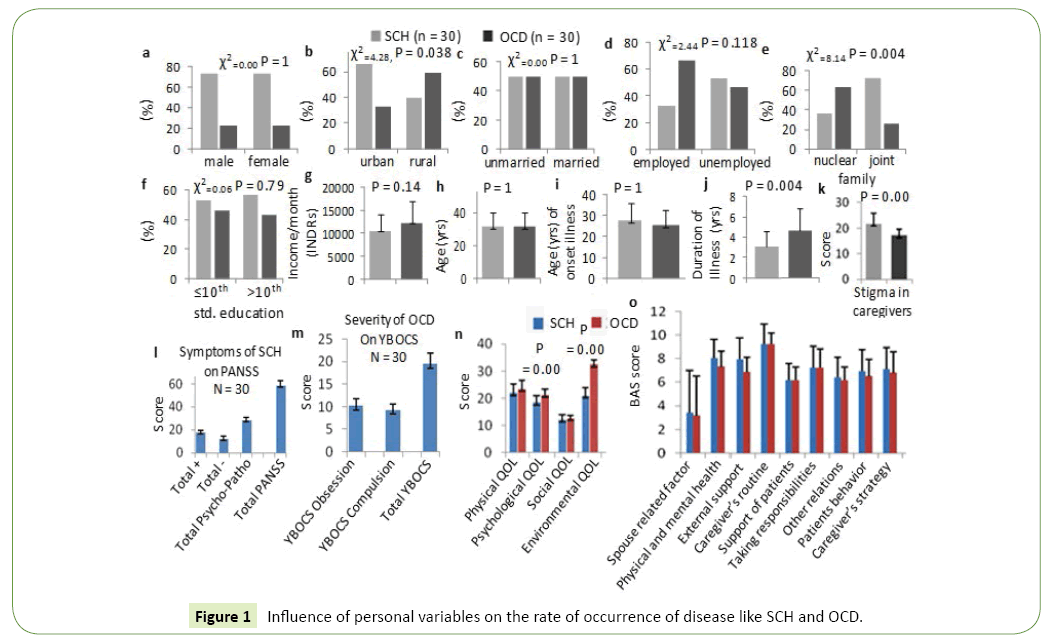
Influence of personal variables like age, gender, marital status, education, employment etc. on the rate of occurrence of disease like SCH and OCD have been verified and the data are presented as bar diagram in the Figure 1. These results show that among the schizophrenic patients 23 (73.7%) are male, 7 (23.3%) are female and among the OCD patients 23 (73.7%) are male 7 (23.3%) are female (Figure 1a).
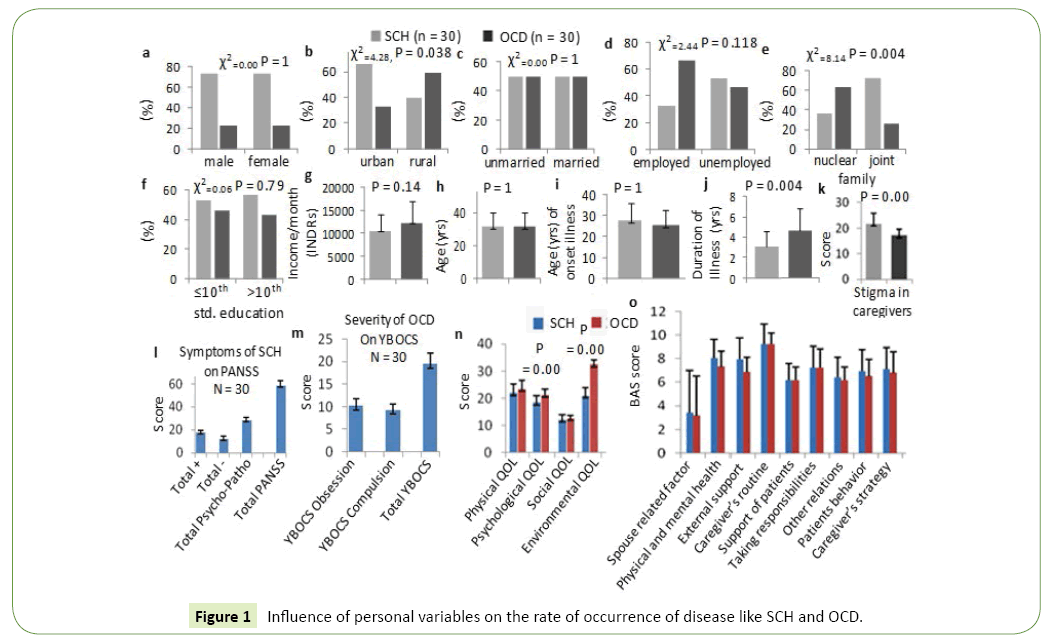
Figure 1: Influence of personal variables on the rate of occurrence of disease like SCH and OCD.
Figures 1b-1d shows comparison between Schizophrenia group and OCD group in respect to family background (rural or urban). Chi-square test shows significant difference among the groups these two disease groups (x2=4.28; p value=0.038*). Figures 1e and 1f shows that 36.7% schizophrenic patients are from nuclear family and 63.3% are from joint family. Among OCD patients 73.3% are from nuclear family and 26.7% are from joint family. Chi-square test shows significant difference among the groups (x2=8.14, p value=0.004*). Figures 1g -1i demonstrates that age is matched in patients of schizophrenia group (31.80 + 8.66) and OCD group (31.80 + 8.66) for a reasonable comparison. Duration of illness was noticed to be more in obsessive compulsive disorder (4.60 + 2.15) than schizophrenia (3.16 + 1.44) and it was significantly higher in OCD (p value is 0.004. t=3.02 at df=58) (Figure 1j). Stigma in caregiver was found to be significantly higher (p=0.00) in SCH than the OCD patients (Figure 1k).
Figure 1l-1n demonstrates that there is significant (p<0.01) differences between the QOL of SCH and OCD patients. The psychological and environmental factor is found to be linked with the QOL during the disease assessment (t-test=5.44, df=58, p value is 0.000**).
Table 1 demonstrates that total QOL is better in OCD patients than schizophrenic patients (71.50 + 7.78 vs. 87.6 + 5.31, t-test=-9.04, df=58, p value=0.000**). Psychological Domain (18.43 + 2.50 vs. 21.33 + 2.12, t-test is -4.84, df -58, p-value=0.000**). Environmental Domain (21.06 + 2.89 vs. 32.40 + 1.81, t-test=18.15, df-58, p-value is .000**) significantly higher in OCD patients. Physical domain (22.03 + 3.10 vs. 23.46 + 3.14, t-test is -1.77, df-58, p value=0.081) and Social Domain (12.20 + 1.84 vs. 12.73 + 0.94, t-test=-1.40, df=58, p value=0.164) are Comparable in both groups. Table 1 sub group of family Burden of both groups are comparable. Mean total BAS score of schizophrenia is 62.70 + 8.52 (SD), mean total BAS score of OCD is 59.56 + 4.91 (SD). There is no significant difference (t-test=1.58, df=58, p-value=0.119) and all subgroup of BAS are also comparable in both groups.
Table 1 Pearson correlation between socio-demographic variables and clinical profiles of schizophrenia.
| Variables |
stigma |
Domain 1 |
Domain 2 |
Domain 3 |
Domain 4 |
Total QOL |
Spouse related factor |
Physical and Mental health |
External support |
Caregiver routine |
Support of patient |
Taking responsibility |
Other relation |
Patient behaviour |
Caregiver strategy |
BAS |
| Positive syndrome score |
Pearson Correlation |
0.564** |
-0.385* |
-0.496** |
-0.284 |
-0.637** |
-0.634** |
0.282 |
0.086 |
-0.133 |
0.295 |
0.176 |
0.220 |
0.067 |
0.017 |
0.266 |
0.302 |
| Sig. (2- tailed) |
0.001 |
0.036 |
0.005 |
0.129 |
0.000 |
0.000 |
0.131 |
0.653 |
0.484 |
0.113 |
0.351 |
0.242 |
0.724 |
0.931 |
0.156 |
0.104 |
| Negative Syndrome score |
Pearson Correlation |
0.754** |
-0.362* |
-0.395* |
-0.108 |
-0.293 |
-0.403* |
0.124 |
0.198 |
0.159 |
0.336 |
0.272 |
0.333 |
0.230 |
0.203 |
0.298 |
0.436* |
| Sig. (2- tailed) |
0.000 |
0.049 |
0.031 |
0.572 |
0.116 |
0.027 |
0.515 |
0.295 |
0.402 |
0.069 |
0.146 |
0.072 |
0.221 |
0.281 |
0.109 |
0.016 |
| General Psycho pathology |
Pearson Correlation |
0.701** |
-0.633** |
-0.461* |
-0.041 |
-0.502** |
-0.607** |
0.107 |
0.387* |
0.073 |
0.435* |
0.236 |
0.323 |
0.083 |
0.312 |
0.351 |
0.475** |
| Sig. (2- tailed) |
0.000 |
0.000 |
0.010 |
0.829 |
0.005 |
0.000 |
0.574 |
0.035 |
0.702 |
0.016 |
0.209 |
0.081 |
0.664 |
0.093 |
0.057 |
0.008 |
| Total PANSS |
Pearson Correlation |
0.811** |
-0.571** |
-0.472** |
-0.117 |
-0.528** |
-0.611** |
0.239 |
0.230 |
-0.011 |
0.459* |
0.206 |
0.313 |
0.063 |
0.198 |
0.339 |
0.454* |
| Sig. (2- tailed) |
0.000 |
0.001 |
0.008 |
0.537 |
0.003 |
0.000 |
0.204 |
0.222 |
0.954 |
0.011 |
0.276 |
0.092 |
0.742 |
0.295 |
0.067 |
0.012 |
| Duration of illness |
Pearson Correlation |
0.329 |
-0.248 |
-0.164 |
0.324 |
-0.366* |
-0.198 |
0.019 |
0.365* |
0.095 |
-0.073 |
0.069 |
0.269 |
0.053 |
0.146 |
0.229 |
0.263 |
| Sig. (2- tailed) |
0.076 |
0.186 |
0.386 |
0.080 |
0.047 |
0.293 |
0.921 |
0.047 |
0.619 |
0.702 |
0.716 |
0.150 |
0.779 |
0.441 |
0.223 |
0.161 |
| Monthly family income |
Pearson Correlation |
0.208 |
-0.201 |
0.004 |
-0.086 |
0.067 |
-0.070 |
0.206 |
-0.152 |
-0.076 |
0.249 |
-0.009 |
-0.008 |
-0.04 |
-0.084 |
-0.119 |
0.016 |
| Sig. (2- tailed) |
0.270 |
0.288 |
0.983 |
0.653 |
0.723 |
0.714 |
0.276 |
0.422 |
0.690 |
0.185 |
0.964 |
0.965 |
0.833 |
0.659 |
0.530 |
0.933 |
**Significant correlation<0.01 level (2- tailed), *significant correlation<0.05 level (2- tailed)
Table 2 demonstrates that significant positive correlation between positive syndromes of schizophrenia and stigma (Pearson’s r=-0.564, P=0.001**) which means severity of various positive symptoms of schizophrenia shows high stigma positive syndrome has significant negative correlation with all domain of QOL D1 (r=-0.385, p=0.036*), D2 (r=-0.496, p=0.005**), D4 (r=- 0.637, p=0.000**) Except social domain (D3 r=-284, p=0.129). A positive correlation has shown between positive syndrome and with all subgroup of burden assessment schedule and with total BAS score. But there has no significant correlation. Negative syndrome of schizophrenia has shown significant positive correlation with stigma (r=0.754, p=0.000**), And negative correlation of all domain of QOL. But significant correlation with Domain=1 (r=-0.362, p=0.49*), Domain-2 (r=-0.395, p=0.031*) except Domaim-3 ( r=-0.108, p=0.572) and domain-4 (r=-0.293, p=0.116). There has positive correlation with all subgroup family burdens, spouse related (r=0.124, p=0.515), Physical and mental health ( r=0.198, p=0.295). External support (r=0.159 p=0.402) Care givers routine (r=0.336 p=0.069) Support of patients (r=0.272 p=0.146), Taking Responsibility (r=0.333, p=0.072) Other relations (r=0.230, p=0.221) Patient behavior (r=0.203, p=0.281), Caregiver strategy (r=0.298, p=0.109), total BAS (r=0.436, p=0.016*).
Table 2 Pearson correlations between socio-demographic variables and clinical profiles of OCD.
| Variables |
stigma |
Domain 1 |
Domain 2 |
Domain 3 |
Domain 4 |
Total QOL |
Spouse related factor |
Physical and Mental health |
External support |
Caregiver routine |
Support of patient |
Taking responsibility |
Other relation |
Patient behaviour |
Caregiver strategy |
BAS |
| Obsession score |
Pearson Correlation |
0.319 |
-0.111 |
-0.415* |
-0.076 |
0.198 |
-0.235 |
-0.104 |
-0.110 |
0.268 |
0.105 |
0.075 |
0.160 |
0.250 |
0.197 |
0.030 |
0.196 |
| Sig. (2- tailed) |
0.086 |
0.558 |
0.023 |
0.689 |
0.293 |
0.211 |
0.586 |
0.563 |
0.152 |
0.582 |
0.692 |
0.398 |
0.182 |
0.296 |
0.874 |
0.298 |
| Compulsion score |
Pearson Correlation |
0.421* |
-0.177 |
-0.439* |
0.057 |
-0.159 |
-0.399* |
-0.032 |
0.237 |
0.075 |
-0.151 |
-0.005 |
0.088 |
0.263 |
0.143 |
-0.027 |
0.168 |
| Sig. (2- tailed) |
0.021 |
0.349 |
0.015 |
0.766 |
0.400 |
0.029 |
0.869 |
0.206 |
0.694 |
0.427 |
0.979 |
0.644 |
0.161 |
0.452 |
0.886 |
0.376 |
| Total YBOCS score |
Pearson Correlation |
0.406* |
-0.150 |
-0.485** |
-0.022 |
0.048 |
-0.345 |
-0.102 |
0.036 |
0.216 |
0.023 |
0.047 |
0.148 |
0.283 |
0.212 |
0.019 |
0.208 |
| Sig. (2- tailed) |
0.026 |
0.428 |
0.007 |
0.907 |
0.800 |
0.062 |
0.593 |
0.849 |
0.251 |
0.903 |
0.805 |
0.435 |
0.130 |
0.261 |
0.921 |
0.269 |
| Duration of illness |
Pearson Correlation |
0.227 |
-0.240 |
-0.181 |
-0.020 |
-0.253 |
-0.307 |
0.475** |
0.181 |
0.367* |
0.180 |
0.064 |
-0.028 |
0.285 |
-0.055 |
-0.012 |
0.542** |
| Sig. (2- tailed) |
0.228 |
0.201 |
0.340 |
0.915 |
0.178 |
0.099 |
0.008 |
0.338 |
0.046 |
0.342 |
0.736 |
0.883 |
0.127 |
0.774 |
0.949 |
0.002 |
| Monthly family income |
Pearson Correlation |
0.210 |
0.106 |
0.079 |
0.186 |
0.233 |
0.207 |
-0.176 |
0.325 |
0.122 |
-0.135 |
0.031 |
0.150 |
-0.063 |
0.215 |
0.305 |
0.186 |
| Sig. (2- tailed) |
0.264 |
0.578 |
0.678 |
0.326 |
0.216 |
0.271 |
0.353 |
0.080 |
0.519 |
0.478 |
0.871 |
0.430 |
0.742 |
0.254 |
0.101 |
0.325 |
**Significant correlation<0.01 level (2- tailed), *significant correlation<0.05 level (2- tailed)
Discussion
Several studies show that stigma of caregivers usually arises from the lack of awareness, education and perception. The nature and the complications of mental illness, for example odd behaviours and violence might have been detracting factors that affect the caregivers [11]. Stigma of caregivers related to schizophrenia in India is particularly high [12].
Stigma and discrimination linked to schizophrenia was found to have a significant impact on the lives of the affected individuals from a study investigating patient's perceptions of stigma. It was reported that a strikingly large percentage of participants (97%) believed that stigma was caused by a lack of awareness about the disease schizophrenia, followed by the nature of the illness itself (73%). Behavioural symptoms associated with schizophrenia were also thought to cause stigma, whereas drug-related complications were observed as less influential role in stigma [13]. Angermeyer MC, Matschinger et al. [14] reported that the finding of stigma among family members of patients with schizophrenia can be easily understood according to their visible behaviour. The public-image of a person with schizophrenia is built up on the basis of his/her actual abnormal behaviour. It includes delusions, hallucinations, self-talking, self-smiling and that lead to increase stigma. Li SX, Phillips MR et al. has explained that in many parts of the world, it is believed that schizophrenia is a punishment for the sins committed by the patient or his family members [15].
These causal beliefs further enhance stigma. The caregivers perceive that they are stigmatized or have experienced some sort of stigma due to the presence of mental illness in the family. Those from the older age group and rural caregivers were more likely to perceive stigma as a major problem. But otherwise, there were few differences between socio-demographic groups. In case of OCD, compulsion scale of YBOCS and total YBOCS score had significant and positive correlation with stigma in caregivers of OCD patients. This may be due to the presence of socially unacceptable behaviour seen predominantly during the acute phase of the illness. Behaviours such as hallucinations, delusions, and suspicion were found to be very distressing and associated with the development of stigma. Another possible reason may be that since perceived stigma was the result of perception of public stigma, through time, the patient may develop resistance to stigma through experience. These results were consistent with the previous studies in India and Europe [16,17]. In case of OCD patients, though mean obsessive scores has been higher than mean compulsion score. Compulsion score of OCD has formed significant positive correlation with stigma of caregivers of OCD patients. This might be due to repetitive behaviours that are socially un-expectable, that hamper patient’s daily activities and occupational function, and only the expressing symptoms by the patients. In this study shows that QOL of schizophrenia patients is significantly lower than OCD patients, OCD patients has been found better psychological and environmental quality of life than those with schizophrenia. We have found that the environmental domain of QOL is more affected in schizophrenic patients in compare to OCD patients. Lower score on QOL in schizophrenics might be due to the negative symptoms present in these patients, among which asociality, avolition and apathy are known to be prominent in patients of schizophrenia. Socio demographic factors like unemployment, low monthly family income could be other contributing factors. This finding is supported by an earlier study by Gururaj et al. [18]. Bobes and Gonzαlez et al. [19] documented that OCD patients reported the same QOL as schizophrenia patients in the area of mental health, but better quality of life in the areas of physical health.
In the present study, social domain is similar in both groups of patients. Similar result has been found in a study, conducted by Bystritsky et al. [20]. Positive syndrome of schizophrenia has shown significant negative correlation with all domains of QOL except social domain of QOL.
Negative syndrome of schizophrenia has shown significant negative correlation with physical domain, psychological domain, and total QOL scores. In general psychopathology of schizophrenia has shown significant negative correlation with physical, psychological and environmental domain of this disease except social domain of QOL.
Similar result was found in another study, conducted by Patra and Misra et al., [21], they reported that more sever positive as well as negative symptoms predicted a poorer quality of life. All domains of psychopathology were found to be negatively correlated with all the domains of QOL. The correlation of PANSS general and total scores with physical, psychological and environment component of QOL was statistically significant [22].
Several authors reported that negative QOL/subjective wellbeing correlate more strongly with depression and anxiety than with psychotic symptoms [23].
Many studies reported that there is inverse correlation between severity of symptoms and quality of life [21,24]. Galletly et al. [25] demonstrated that changes in QOL were more highly correlated with changes in general psychopathology. These correlations were higher than correlations between changes in QOL and changes in negative symptoms or changes in overall PANSS score. These results and the above studies imply that all levels of general psychopathology are more highly associated with subjective QOL than that of core positive and negative symptoms. General psychopathology contains items that include symptoms of depression and anxiety. The review of studies suggested that anxiety and depression may be more critical than any other symptoms of schizophrenia [22].
Our study has shown that obsession, compulsion subscale and total YBOCS score have form negatively correlated with psychological domain and compulsion subscale have shown significant negative correlation with total QOL. Psychological domain has found significant correlation with obsession and compulsion. This finding may be due to increased distress and anxiety of the patients of OCD. A Study was conducted by Moritz et al. [26], which reported that QOL impairment is to be highly associated with the severity or numbers of compulsions. Another Study was conducted by Hou and Yen et al. [27] which reported that patients with OCD had worse QOL on the general, physical, psychological and social relationship domains compared with the control group.
Many studies reported that Psychological QOL in OCD patients negatively correlated with severity of obsessions, total score of the YBOCS. In addition, those patients without depression had better psychological QOL [28,29]. One study reported that Poor psychological and social QOL in OCD could be due to the associated anxiety/distress [30]. So, findings of this study corroborate with the other studies. In relation to family burden, in our study caregivers of schizophrenic patients and caregivers of OCD have shown comparable burden on BAS. All subgroup of BAS is comparable in both groups. Obsessive and compulsive subscales have formed positive correlation with BAS (Barden assessment schedule) and no significant correlation among them has been found in this study. It is understandable that burden of care is somewhat higher in schizophrenia than in OCD because of lack of insight in patients as well as reduced involvement in treatment. It would appear that caregiver burden in OCD is somewhat smaller than in schizophrenia. Sometimes patients with OCD keep their problems to themselves and do not reveal them to others. They may try to cope with their symptoms on their own. In comparison, patients with schizophrenia have impaired reality contact and lack insight about their illness, which makes things difficult for their caregivers. Socio-occupational impairment is also significant in schizophrenia. spouse-related factor, physical and mental health, external support, caregiver's routine, support of patient, taking responsibility, other relations, patients’ behavior and caregiver strategy all nine subscales show higher burden in the schizophrenia group than that of the OCD group. But the difference is not statistically significant except for disruption of routine family activities, a finding similar to that of Thomas et al. [31].
In the present study, families of patients with schizophrenia reported greater burden than the OCD group this finding is more or less in line with a study by Veltro et al. [32] Caregiver’s routine is the area in which the burden experienced by caregivers of patients with schizophrenia is statistically significant. Caregivers’ physical and mental health had affected due to decrease in time for self-care. Similar results emerged in studies by Kate et al. [33] and Verma et al. [34], they reported that caregivers in both OCD and schizophrenia groups experienced a comparable burden.
An earlier study has revealed that about half of the family members of patients with OCD face financial hardships [35]. Another studies, reported that primary caregivers in patients with OCD reported deterioration in the quality of relationships with family members and friends as well as family stability, although, the degree of impairment was comparable with that in schizophrenia [36]. In the past studies, authors had found difference in results in different study. Harsh oza, minakshi et al. [37] reported that Burden of care was higher in caregivers of schizophrenia patients in 5 domains - financial burden, disruption of family routine, disruption of family leisure, disruption of family interaction and effect on physical health. However, a statistically significant higher score was observed only for the domain of disruption of family routine. Abou-Zaid and El-Tawil et al. [38] compared the burden of care between the caregivers of patients with obsessive compulsive disorder (OCD) and schizophrenia.
Conclusion
Negative syndrome like emotional withdrawal, difficulty in abstract thinking, low conversation all these symptoms might be responsible for significant correlation with total family burden. General psychopathology of schizophrenia has shown significant positive correlation with Caregiver’s routine and total BAS score. Total PANSS Scores has shown significant positive correlation with physical and mental health, caregiver’s routine and total BAS scores. This may be due to anxiety depression, uncooperativeness of patients, unusual thought, lack of judgment and insight, disturbance of volition, active social avoidance ,others sociodemographic factors like low family monthly income, rural background responsible for poor physical and mental health of caregiver of schizophrenic patients, this symptom also hampered caregivers routine.
Obsession and compulsion subscale have shown no significant correlation with any subgroups of OCD. This is possibly because our sample constituted mainly moderately ill OCD subjects as reflected in the YBOCS scores.
24697
References
- International classification Disease-10 (2007) https://www.who.int/classifications/icd/en/
- Mateos A, Luis J (2013) Global burden of schizophrenia in the year 2000. World Health Organization, Geneva, Switzerland.
- World Health Organization (2014) The world health report, Approach to Mental Health, WHO, Geneva, Switzerland.
- Lehman AF (1997) Instrument to measuring quality of life in mental illness.in quality of life in mental disorder. John Wiley sons, NY, USA. pp: 79-94.
- World Health Organization (2007). International Classification of Functioning, disability, and Health: Children and Youth Version: ICF-CY. World Health Organization, Geneva, Switzerland.
- Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13: 261-276.
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, et al. (1989) The Yale-Brown Obsessive-Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry 46: 1006-1011.
- Thara R, Srinivasan TN (2000) How stigmatising is schizophrenia in India. Int J Soc Psy 46: 135-141.
- World Health Organization (2005) WHO Quality of Life-BREF (WHOQOL-BREF): World Health Organization, Geneva, Switzerland.
- Çapar M, Kavak F (2018) Effect of internalized stigma on functional recovery in patients with schizophrenia. Perspect Psychiatr Care 55: 103-111.
- Ahmad H (2014) Burden experienced by families of Patients with schizophrenia and its related factors. Faculdade de Ciencias Medicas University Nova De Lisboa.
- Vrbova K, Prasko J, Ociskova M, Kamaradova D, Marackova M, et al. (2017) Quality of life, self-stigma, and hope in schizophrenia spectrum disorders: A cross-sectional study. Neuropsychiatr Dis Treat 13: 567-576.
- Shrivastava A, Bureau Y, Rewari N, Johnston M (2013) Clinical risk of stigma and discrimination of mental illnesses: Need for objective assessment and quantification. Indian J Psychiatry 55: 178-182.
- Angermeyer MC, Matschinger H (2003) Public beliefs about schizophrenia and depression: Similarities and differences. Soc Psychiatry Psychiatr Epidemiol 38: 526-534.
- Li SX, Phillips MR (1990) Witch doctors and mental illness in mainland China: A preliminary study. Am J Psychiatry 147: 221-224.
- Brohan E, Elgie R, Sartorius N, Thornicroft G (2010) Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: the GAMIAN-Europe study. Schizophrenia Research 122: 232-238.
- Yanos PT, Roe D, Lysaker PH (2010) The impact of illness identity on recovery from severe mental illness. American Journal of Psychiatric Rehabilitation 13: 73-93.
- Gururaj GP, Math SB, Reddy J, Chandrashekar CR (2008) Family burden, quality of life and disability in obsessive compulsive disorder: An Indian perspective. J Postgrad Med 54: 91-97.
- Bobes J, Gonzαlez MP, Bascarαn MT, Arango C, Sαiz PA, et al. (2001) Quality of life and disability in patients with obsessive-compulsive disorder. Eur Psychiatry 16: 239-245.
- Bystritsky A, Liberman RP, Hwang S, Wallace CJ, Vapnik TRN, et al. (2001) Social functioning and quality of life comparisons between obsessive-compulsive and schizophrenic disorders. ADAA.
- Patra S, Mishra A (2012) Association of psychopathology with quality of life in acute phase of schizophrenia; an experience from east India. Ind Psychiatry J 21: 104-108.
- Gautam S, Nijhawan M (1984) Burden on families of schizophernic and chronic lung disease patients. Indian J Psychiatry 26: 156-159.
- World Health Organization (1980) International Classification of Impairments, Disabilities, and Handicaps: A manual of classification relating to the consequences of disease. World Health Organization, Geneva, Switzerland..
- Ritsner M (2003) Predicting changes in quality of life of schizophrenia patient 191: 287-294.
- Galletly CA, Clark CR, McFarlane AC, Weber DL (1997) Relationships between changes in symptom ratings, neurophysiological test performance and quality of life in schizophrenic patients treated with clozapine. Psychiatry Res 72: 161-166.
- Moritz S, Rufer M, Fricke S, Karow A, Morfeld M, et al. (2005) Quality of life in obsessive-compulsive disorder before and after treatment. Comprehensive Psychiatry 46: 453-459.
- Hou SY, Yen CF, Huang MF, Wang PW, Yeh YC (2010) Kaohsiung quality of life and its correlates in patients with obsessive-compulsive disorder. J Med Sci 26: 8.
- Lochner C, Mogotsi M, Du Toit PL, Kaminer D, Niehaus DJ, et al. (2003) Quality of life in anxiety disorders: a comparison of obsessive-compulsive disorder, social anxiety disorder, and panic disorder. Psychopathology 36: 255-262.
- Zahid MA, Ohaeri JU (2010) Relationship of family caregiver burden with quality of care and psychopathology in a sample of Arab subjects with schizophrenia. BMC Psychiatry 10: 71.
- Gururaj GP, Math SB, Reddy JY, Chandrashekar CR (2008) Family burden, quality of life and disability in obsessive compulsive disorder: an Indian perspective. J Postgrad Med 54: 91-97.
- Josy K, Thomas PN, Suresh AN, Verma VK, Andrade C (2004) Psychosocial dysfunction and family burden in schizophrenia and obsessive compulsive disorder. Indian Journal of Psychiatry 46: 238-243.
- Veltro F, Maglian L, Lobrace S (1994) Burden on the relatives of patients with schizophrenia versus neurotic disorders: A pilot study. Soc Psychiat Epidemiol 29: 66-70.
- Kate N, Grover S, Kulhara P, Nehra R (2013) Caregiving appraisal in schizophrenia: A study from India. Soc Sci Med 98: 135-140.
- Verma M, Sinha UK (2013) Burden of care and stress in family members of patients suffering from obsessive compulsive disorder. Delhi Psychiatry J 16: 375-379.
- Oliver J, Huxley P, Bridges K, Routledge L (2007) Quality Of Life And Mental Health.
- Roick C, Heider D, Bebbington PE, Angermeyer MC, Azorin JM, et al. (2007) Burden on caregivers of people with schizophrenia. Br J Psychiatry 190: 333-338.
- Oza H, Parikh MN, Vankar GK (2017) Comparison of caregiver burden in schizophrenia and obsessive-compulsive disorder. Archives of Psychiatry and Psychotherapy 2: 32-41.
- Abou-Zaid M, El-Tawil M, Abdel-Azhim K, Eisawi H (2005) Caregiver burden among schizophrenic and obsessive compulsive disorder families : A comparative study, Current Psychiatry. Ain Shams University, Egypt. 12: 1.