Research Article - (2023) Volume 17, Issue 11
A Comparative Study on Nutritional States and Anemia among Women at Reproductive Age in Pastoralist and Agro-Pastoral Setting of Ethiopian Somali Region
Meka Kedir1,
Tewodros Desalegn Nebi2 and
Solomon Bereka2*
1Department of Nursing, Jigjiga University, Gondar, Ethiopia
2Department of Public Health, Arsi University, Asela, Ethiopia
*Correspondence:
Solomon Bereka, Department of Public Health, Arsi University, Asela,
Ethiopia,
Tel: 251949320147,
Email:
Received: 15-Nov-2019, Manuscript No. IPHSJ-23-2932;
Editor assigned: 20-Nov-2019, Pre QC No. IPHSJ-23-2932(PQ);
Reviewed: 04-Dec-2019, QC No. IPHSJ-23-2932;
Revised: 02-May-2023, Manuscript No. IPHSJ-23-2932(R);
Published:
30-May-2023
Abstract
Background: In Ethiopia, anemia prevalence among women age 15-49 increased to 24% in 2016 from 17% in 2011. Where the highest burden has been observed in Somali region, 60% of the women were anemic in 2016. This study was aimed at assessing the prevalence and associated factors of anemia among women of reproductive Agein Fafan zone, Somali regional state of Ethiopia.
Methods: The community based cross sectional study using simple random sampling was conducted in Nov 2014-Jun 2015. Interview using pretested structured questionnaire as well as measurement of hemoglobin level and nutritional characteristics were used. Binary logistic regression were used to determine associated factors of anemia.
Results: Prevalence of anemia is 65.2% (95% CI: 60.35, 69.91) out of 400 participants included in the study, where 33.2%, 28.25% and 3.75% were mildly, moderately and severely anemic respectively. Pastoral community (AOR=19.03, 95% CI: 6.59, 54.95), normal body weight (AOR=0.21, 95% CI: 0.10, 0.41) and using any kind of toilet (AOR=0.39, 95% CI: 0.18, 0.82) were significantly associated with anemia status at 5% level of significance.
Conclusion: Anemia is a major public health problem in the study area. More efforts should be applied on pastoralist in order to reduce the burden of anemia.
Keywords
Anemia; Prevalence; Associated factors; Women;
Pastoralist; Agro-pastoralist; Somali; Ethiopia
Introduction
Anemia is a condition characterized by a low level of
hemoglobin in the blood. It is one of the most frequently
observed nutritional deficiency diseases in the world today. Its
adverse health consequences that affect people with varied
degrees of affluence and from all age-groups, particularly women of childbearing age and children. Sub Saharan Africa is
home to some of the most nutritionally insecure people in the
world. Anemia remains a major public-health problem, affecting
about a quarter of the world's population. In Ethiopia, even
though tremendous efforts has been applied to reduce the
burden of anemia, anemia prevalence among women age 15-49
increased to 24% in 2016 from 17% in 2011. Where the highest
burden has been observed in Somali region, 60% of the women
were anemic in 2016. Iron deficiency remains the major cause of
anemia and is the most widespread single nutrient deficiency in
the world. About two billion people are iron-deficient, with half
of them manifesting clinical signs of anemia. It is estimated that
75% of anemia is related to iron deficiency, followed by folate
and vitamin B12 deficiencies [1].
Besides, anemia can result from other nutritional and nonnutritional
factors, including hemorrhage, infection, chronic
disease states, or drug toxicity, certain vitamins, copper and
protein. Poor infrastructure and limited resources compounded
with conflict, HIV, and poor access to health service are factors
that contribute to the staggering levels of under nutrition and
food insecurity on the continent. Under nutrition could be due
to low dietary intakes inequitable distribution of food within the
household improper food storage and preparation dietary
diversity, infectious diseases, and care particularly for women
also contribute significantly to their poor nutritional status. It
may also be affected by lifestyle (pastoralist vs. agro-pastoralist)
of the women in the study area. That is, the pastoralism is a
subsistence system for producing meat, milk, and other animal
products from domestic animals such as goats, sheep, cattle and
camels. Pastoralist diets generally change seasonally and interannually
with changing climatic and socioeconomic
circumstances. Agro-pastoralism is a set of practices that
combine pastoral livelihoods with production of diversified crops
like millet, sorghum, maize, vegetables, fruits and pulses (annual
legumes). Identifying the magnitude of anemia and its
determinants in high risk groups, such as women of
reproductive age, would be essential for evidence based
intervention modalities, particularly in developing countries,
such as Ethiopia, where the social conditions pose serious
challenges to women [2].
Therefore, this study was aimed at assessing the prevalence
and associated factors of anemia among women of reproductive
age in pastoral and agro-pastoral communities of Fafan zone in
Somali regional state of Ethiopia. This study would help us to
assess the severity levels of anemia, nutritional status, dietary
diversity, food security and associated factors of anemia among
women of reproductive age in pastoral and agro pastoral
communities.
Materials and Methods
Study setting
Fafan (Somali: Faafan) is one of the nine zones of the Somali
regional state of Ethiopia. Based on the 2007 Census, the Zone
has a total population of 967, 652, of whom 526,398 are men
and 441,254 women. While 21.0% were urban inhabitants and
11.6% were pastoralists. Two largest ethnic groups reported in
Jigjiga were the Somalis (95.6%) and Amhara (1.83%); all other
ethnic groups made up 2.57%. Somali language is spoken by
nearly all individuals and majority of the individuals are Muslims
in the zone. There are three settlements in the zone for refugees
from Somalia, with 40,060 registered individuals [3].
According to a May 24, 2004 World Bank memorandum, 7% of
the inhabitants of Fafan have access to electricity, this zone has a
road density of 30.5 kilometers per 1000 square kilometers, the
average rural household has 1.3 hectares of land and the
equivalent of 1.0 head of livestock. About twenty eight percent,
28.2% of the population is in non-farm related jobs, compared
to the national average of 25% and a regional average of 28%.
Twenty one percent, 21% of all eligible children are enrolled in
primary school, and 9% in secondary schools. Nearly three
fourth, 74% of the zone is exposed to malaria, and none to
Tsetse fly. The memorandum gave this zone a drought risk rating
of 386. In 2006, the Fafan zone was affected by deforestation
due to charcoal production [4].
Study design and population
The community based cross sectional study was conducted in
Nov 2014-Jun 2015 in Fafan zone, Somali regional state of
Ethiopia. The study population was women of reproductive age
living in pastoral and agro-pastoral areas of Fafan zone, Somali
regional state. Women of 15-45 years of age in the study setting
were included in this study. Pregnant women were not included,
because pregnancy is one factor affecting hemoglobin
concentration and nutritional status.
Sample size and sampling technique
A sample size of 625 was determined using single population
proportion formula with prevalence of anemia among women in
Somali region is 44% (based on previous study of DHS, 2011), a
confidence level of 95%, margin of error 5%, 1.5 design effect
and 10% non-responses. Among six woredas of Fafan zone, two
woredas of pastoral and agro-pastoral were selected
purposively. The kebeles and the study participants were
selected randomly. Using proportional allocation 429 participants from Harshin and 147 participants from
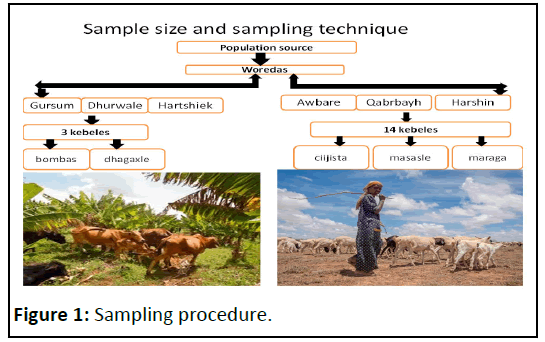
Gursumworeda were interviewed (Figure 1) [5].
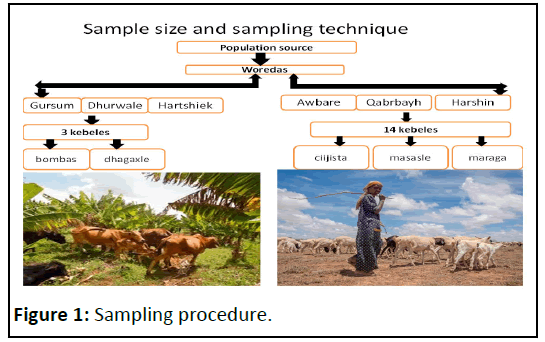
Figure 1: Sampling procedure.
Data collection and procedures
The structured interview schedule consisted of questionnaires
including the socio-demographic and economic characteristics,
24 hours recall on food diversity, two weeks recall on illness,
household food insecurity, hemoglobin level measurements, and
other nutrition related characteristics. The pretested
questionnaire prepared in English and translated to local
language Somali was used. Data were collected by the
researcher and trained data collectors face to face at the
women’s home [6].
Using guidelines for measuring household and individual
dietary diversity, sixteen food groups were considered to assess
dietary diversity of individuals. The 24 hour recall technique
attempts to estimate food intakes of the individuals over the
period of time. Additionally, data were collected using items in
the Household Food Insecurity Access Scale (HFIAS) to compute
four levels of food insecurity developed by a project of the
United States Agency for International Development (USAID).
HFIAS will provide information on food availability and
consumption of the women.
Measurement and instruments
Hemoglobin and anthropometric (weight, height and mid
upper arm circumference) measures were measured by trained
nurses in this study. The hemoglobin level was measured using
digital hemocue (201) photometer.
Hemoglobin was analyzed using finger prick by the
professional nurses for determining hemoglobin status of the
women. All the necessary safety measures were taken during
the activity. Mid Upper Arm Circumference (MUAC) was
measured to the nearest 0.1 cm using a plastic measuring tape.
Measurement was taken at the mid-point of the upper arm,
between the acromion process and the tip of the olecranon
[7,8].
Measurements of height (cm) and weight (kg) useful to
calculate body mass index, were taken twice on the same day as
the interviews using weighting scale with an attached height
scale model. The average of two measurements on each of
weights and heights were recorded on the record sheet. The accuracy of the weighing scale was checked daily against known
weights.
The scale was placed on a flat, hard surface that allowed
participants to stand securely without rocking and tipping. The
participant was weighted with light clothes and without shoes
by standingat the middle of the scale’s platform without
touching anything and with the weight equally distributed on
both feet. Similarly, height of the participants were measured by
standing without shoes, with heels together, arms to the sides,
legs straight, shoulders relaxed and head in the Frankfort
horizontal plane (looking straight ahead). Just before the
measurement was taken the participants was asked to inhale
deeply, hold the breath and maintain an erect posture to
compress the hair [9].
Data management and statistical analysis
Data was entered into Epi-info and exported to the software
Stata 14.0 for data management and further analysis.
Frequencies and percentages were used to describe categorical data of women. Means, standard deviations, medians and
interquartile ranges were used as appropriate in describing the
continuous type variables. Binary logistic regression was used to
determine associated factors of anemia. Odds ratio with its
respective 95% confidence interval were used to measure
strength of association after Hosmer_Lemeshow goodness of fit
were checked.
Results and Discussion
Socio-demographic and housing characteristics
All participants were Muslim in religion and Somali in
ethnicity. With regard to age, the median value is 23 years (IQR:
20, 25) with the majority (50.25%) residing in the age group of
20-24 years (Table 1).
| Characteristics |
Frequency |
Percent |
| Community |
| Agro-pastoralists |
147 |
36.8 |
| Pastoralists |
253 |
63.2 |
| Age (in years) |
| 15-19 |
66 |
16.5 |
| 20-24 |
201 |
50.25 |
| 25-45 |
133 |
33.25 |
| Educational level of women |
| Uneducated |
292 |
73 |
| Educated |
108 |
27 |
| Educational level of HH head |
| Uneducated |
284 |
71 |
| Educated |
116 |
29 |
| Water source |
| Pipe water |
108 |
27 |
| Tube well/borehole |
31 |
7.8 |
| Dug well |
259 |
64.8 |
| Rain water |
1 |
0.2 |
| Tank truck |
1 |
0.2 |
| Toilet facility type |
| Open field |
213 |
53.2 |
| Composing latrine |
101 |
25.2 |
| Hanging toilet |
81 |
20.2 |
| Bucket toilet/pit latrines/flush toilet |
5 |
1.2 |
| Food security |
| Secure |
80 |
20 |
| Insecure |
320 |
80 |
Table 1: Socio-demographic and housing characteristic of study participants.
Nutrition and illness related characteristics
One hundred thirty (32.5%) of the study participants had a
BMI less than 18.5 kg/m2 (chronically energy deficient); whereas
only eight had a BMI greater than or equal to 25 kg/m2 (over
weight) (Table 2). With regard to history of illness in the last two
weeks, there were 2.5% of the participants reported malaria,
3.5% diarrhea, 9.5% fever and 11.2% cough. Nearly half, 46.75% of the participants have only two meals per day whereas a
round one fifth, 21.5% of the participants have only one
meal per day. Moreover, nearly two third (66.2%) of the
participants have no snacks between meals.
| Characteristics |
Frequency |
Percent |
| BMI |
| Under weight |
130 |
32.5 |
| Normal |
262 |
65.5 |
| Over weight |
8 |
2 |
| Meals per day |
| One |
86 |
21.5 |
| Two |
187 |
46.75 |
| Three |
127 |
31.75 |
| Have snacks between meals |
| Yes |
135 |
33.75 |
| No |
265 |
66.25 |
| MUAC (cm) |
| ≥ 23 |
314 |
78.5 |
| 21-23 |
38 |
9.5 |
| <21 |
48 |
12 |
| Cough |
| Yes |
45 |
11.2 |
| No |
355 |
88.8 |
| Diarrhea |
| Yes |
14 |
3.5 |
| No |
386 |
96.5 |
| Fever |
| Yes |
38 |
9.5 |
| No |
362 |
90.5 |
| Malaria |
| Yes |
10 |
2.5 |
| No |
390 |
97.5 |
Table 2: Nutrition and illness related characteristics of the study participants.
Dietary intakes of the study participants
Out of 16 food groups, the number of food groups consumed
by the study participants ranged 4 to 9 with the median of 5
(IQR: 5, 9). Besides, largest percentage observed that is around
half, 54.75% consumed 5 food groups followed by nearly one
fourth, 25.25% consumed nine food groups. In general, nearly
three fourth of the participants consumed at most eight (half) of
the total food groups [10].
Almost all of the participants consumed oil and fat (oil); cereal
(sorghum, wheat, maize, teff, barley, and rice); spice, condiment
and beverage (salt/iodized salt) and sweets (sugar) based foods.
Majority of the study participants 91.5% consumed other
vegetables (tomato, onion, garlic, potato whereas small
percentage, 33.0% consumed dark green leafy vegetables based
foods. Nearly equal percent, 36.0% and 36.25% of participants
consumed vitamin A rich fruits and other fruits respectively.
Smallest observed percentage, 28.0% was corresponding to
consumption of egg. No report was obtained with regard to
consumption of white roots and tuber; vitamin A rich vegetable
and tubers; organ meat; flesh meat; fish and sea food; legumes,
nuts and seeds; and milk and milk products (Table 3).
| Food group |
Frequency |
Percent |
| Cereal (sorghum, wheat, maize, teff, barley, rice) |
| Yes |
400 |
100 |
| No |
0 |
0 |
| Dark green leafy vegetables |
| Yes |
132 |
33 |
| No |
268 |
67 |
| Other vegetables (tomato, onion, garlic, potato) |
| Yes |
366 |
91.5 |
| No |
34 |
8.5 |
| Vitamin A rich fruits (mango, papaya) |
| Yes |
144 |
36 |
| No |
256 |
64 |
| Other fruits (orange, avocado, guava, banana) |
| Yes |
145 |
36.25 |
| No |
255 |
63.75 |
| Eggs |
| Yes |
112 |
28 |
| No |
288 |
72 |
| Oil and fat (oil) |
| Yes |
400 |
100 |
| No |
0 |
0 |
| Sweets (sugar) |
| Yes |
399 |
99.75 |
| No |
1 |
0.25 |
| Spice, condiment and beverage (salt/iodized salt) |
| Yes |
399 |
99.75 |
No |
1 |
0.25 |
Table 3: Dietary diversity of foods eaten within 24 hours.
Prevalence of anemia
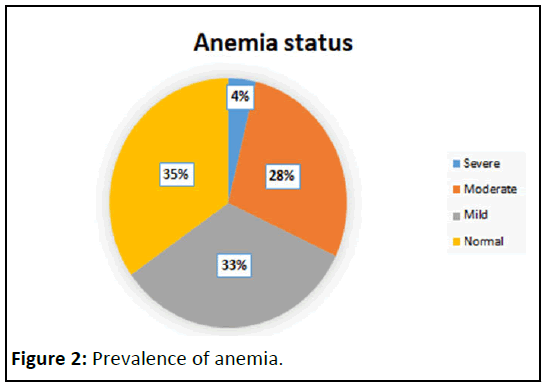
Prevalence of anemia is 65.2% (95% CI: 60.35, 69.91) where
33.2%, 28.25% and 3.75% were mildly, moderately and severely
anemic respectively (Figure 2). Variation of prevalence of
anemia by some characteristics was observed. Of these type of
community (pastoral vs. agro-pastoral), educational status of the
women, type of water supply source, household food insecurity,
body mass index and type of toilet facility were some (Table 4).
The prevalence of anemia is very much high, 89.3% (5.9%
severe, 42.7% moderate and 40.7% mild) in pastoralist
community as compared to 23.8% (0.0% severe, 3.4% moderate
and 20.4% mild) agro-pastoralist. Furthermore, large percent,
71.9% (4.4% severe, 31.9% moderate and 35.6% mild) of women
from food insecure household were anemic relative to 38.75%
(1.25% severe, 13.75% moderate and 23.75% mild) of women
from food secure.
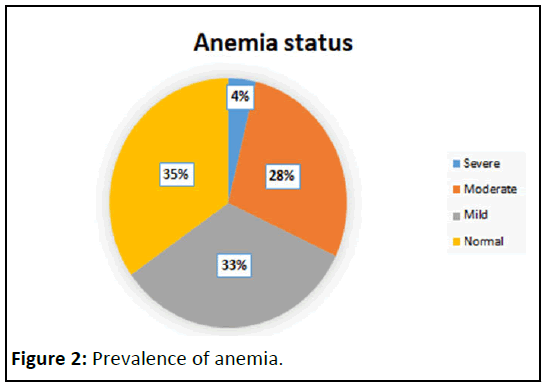
Figure 2: Prevalence of anemia.
| Characteristics |
Anemic (%) |
Non-anemic (%) |
| Severe |
Moderate |
Mild |
| Age of women |
| 15-19 |
3 |
31.8 |
33.3 |
31.8 |
| 20-24 |
4.5 |
28.4 |
35.3 |
31.8 |
| 25-45 |
3 |
26.3 |
30.1 |
40.6 |
| Educational status of the woman |
| Uneducated |
4.8 |
35.3 |
36.6 |
23.3 |
| Educated |
0.9 |
9.3 |
24.1 |
65.7 |
| Piped water supply source |
| Yes |
0 |
3.7 |
22.2 |
74.1 |
| Noa |
5.1 |
37.3 |
37.3 |
20.2 |
| Food security |
| Secure |
1.25 |
13.75 |
23.75 |
61.25 |
| Insecure |
4.4 |
31.9 |
35.6 |
28.1 |
| Community |
| Agro-pastoral |
0 |
3.4 |
20.4 |
76.2 |
| Pastoral |
5.9 |
42.7 |
40.7 |
10.7 |
| BMI |
| Over/under weight |
7.25 |
47.8 |
30.4 |
14.5 |
| Normal |
1.9 |
17.9 |
34.7 |
45.4 |
| Open field toilet type |
| Yes |
5.6 |
40.4 |
41.8 |
12.2 |
| Nob |
1.6 |
14.4 |
23.5 |
60.4 |
| Illness* |
| Yes |
1.3 |
12 |
33.3 |
53.3 |
| No |
4.3 |
32 |
33.2 |
30.5 |
Note: aTubewell/borehole, dug well, rain water or tank truck; bflush toilet, pit latrine, composing latrine, bucket toilet or hanging toilet; *Diarrhea, cough, fever or malaria in the last 14 days
Table 4: Prevalence of anemia by selected characteristics among women in pastoralist and agro-pastoralists.
Associated factors of anemia
All variables considered in simple binary logistic regression
yielded p-values less than 0.25. As a result, all others were
considered in the final model multivariable binary logistic
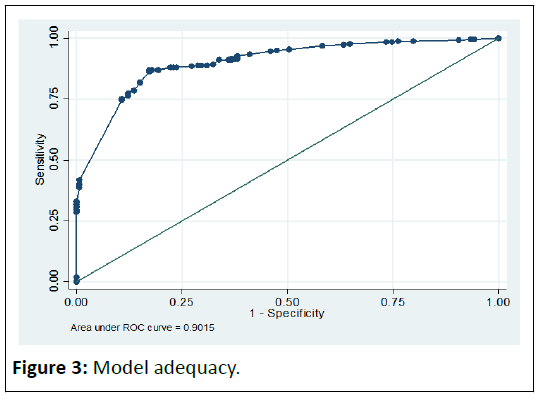
regression. The final model is adequate fit of the data as shown
in the figure below (Figure 3) as well as using
Hosmer_Lemeshow goodness of fit test (P-value=0.4541).
Community type, BMI and toilet type were significantly associated with anemia status at 5% level of significance from
the final model variables (Figure 3).
The likelihood of being anemic for a woman from pastoral
community is 19.03 (AOR=19.03, 95% CI: 6.59, 54.95) times that
of agro-pastoralists (Table 5). With respect to BMI, those who
are with normal body weight are 79% (AOR=0.21, 95% CI: 0.10,
0.41) times less likely as compared to those with either over
weight or underweight. Besides, those using any kind of toilet
including flush toilet, pit latrine, composing latrine, bucket toilet or hanging toilet were 61% (AOR=0.39, 95% CI: 0.18, 0.82) times
less likely as compared to those using open field.
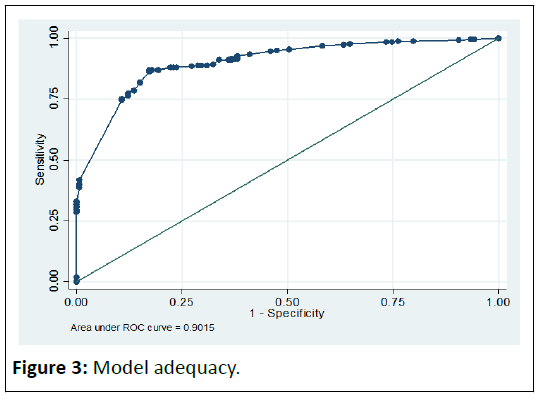
Figure 3: Model adequacy.
| Variables |
COR (95% CI) |
AOR (95% CI) |
| Piped water supply source |
| Yes |
0.09 (0.05, 0.15) |
1.50 (0.56, 3.98) |
| Noa |
1 |
1 |
| Food security |
| Secured |
1 |
1 |
| Unsecured |
4.04 (2.42, 6.74) |
1.29 (0.56, 2.94) |
| Education of women |
| Un educated |
1 |
1 |
| educated |
0.16 (0.10, 0.25) |
0.83 (0.38, 1.83) |
| Community |
| Agro-pastoral |
1 |
1 |
| Pastoral |
26.78 (15.44, 46.46) |
19.03 (6.59, 54.95) |
| BMI |
| Over/under weight |
1 |
1 |
| Normal |
0.20 (0.12, 0.34) |
0.21 (0.10, 0.41) |
| Open field toilet type |
| Yes |
1 |
1 |
| Nob |
0.09 (0.05, 0.15) |
0.39 (0.18, 0.82) |
| Illness* |
| Yes |
0.38 (0.23, 0.63) |
1.53 (0.74, 3.16) |
| No |
1 |
1 |
Note: aTubewell/borehole, dug well, rain water or tank truck; bflush toilet, pit latrine, composing latrine, bucket toilet or hanging toilet; *Diarrhea, cough, fever or malaria in the last 14 days
Table 5: Factors associated with anemia
WHO considers anemia prevalence over 40% in a population
to be a major public health problem, anemia prevalence
between 20% and 40% is considered a medium-level public
health problem, and between 5 to less than 20% is considered a
mild public health problem. In this study, community type was
found to be a significant determinant of anemia. Those women
from pastoral community were ninety times (95% CI: 6.59,
54.95) more likely to develop anemia than whose women from
agro-pastoral community [11].
According to this study, odds of developed anemia in women
with normal body mass indicate was reduced by 21 percent (95%
CI: 0.10, 0.41) as compare with over or under weight. A study
conducted in Bangladesh found that stunted children and
women with low BMI have significantly increased odds of
developing anemia, as reflected by the adjusted ORs of 1.76
(95% CI: 1.10-2.83) and 1.81 (95% CI: 1.11-3.48), respectively.
This result was also supported by study conducted in northern
Tanzania. The finding showed, overweight (BMI of 25-<30 kg/m2)
and obesity (BMI ≥ 30 kg/m2) were observed in 20.2%(95% CI
18.1%-22.6%) and 11.2% (95% CI 9.6-13.1) of the women,
respectively.
However, a study conducted in found no association between
hematological characteristics and BMI. The data showed that
only 13.4% of obese women and 17.1% of the women with
normal weight had IDA (odds ratio=0.75; 95% confidence
interval: 0.39-1.49, P>0.05). The study also revealed, a women
who didn’t use open field toilet type the risk to develop anemia
is reduced by 39 percent (95% CI: 0.18, 0.82). This finding was
also supported by study conducted in Rwanda.
Conclusion
The result showed the risk of anemia was higher among
underweight women and women living in households without
toilet facilities. This may be women from households without
toilet facilities may be susceptible to infection by hookworms
and parasites and this may support our findings that lack of
toilet facilities in household or community increases the risk of
anemia. Anemia is a major public health problem in the study
area. More efforts should be invested to transform pastoral to
agro-pastoral in order to benefit nutritionally.
Ethical Consideration
Ethical approval was obtained from the Institutional review
committee of the college of natural science, Addis Ababa
University and Ministry of health at regional level. Permission to
conduct the study in the villages was obtained from area chiefs
and the dates for data collection were communicated to the
chief before visiting the community. Oral informed consent was
obtained from the participants after the purpose of the study, her right to withdraw at any time and confidentiality had been
explained to her.
Funding
This work was supported by our financially.
Consent for Publication
Not applicable.
Availability of Data
All relevant data are within the paper.
Acknowledgement
We would like to express our sincere gratitude to those
individuals and institutions who contributed in a special way in
this study. Of these, the first was EHNRI for providing Hem cue
(photometer), Microcuvetts and Lancet. Second, Jig-jiga
university for supporting financially, and the Ethiopian Somali
Regional State Health bureau for providing Ferrous sulphate,
Lancet and all cooperation and support letters required. Thirdly,
we would like to acknowledge data collectors; community
leaders in different kebeles for giving me permission to work
with their community; and finally, all women who agreed to
participate in the study and answered all the questions.
References
- Rad HA, Sefidgar SAA, Tamadoni A, Sedaghat S, Bakouei F, et al. (2019) Obesity and iron-deficiency anemia in women of reproductive age in northern Iran. J Educ Health Promot 8: 115.
[Crossref] [Google Scholar] [PubMed]
- Allen LH. Anemia and iron deficiency: Effects on pregnancy outcome. Am J Clin Nutr 71: 1280S-1284S.
[Crossref] [Google Scholar] PubMed]
- Macro ORC (2006) Ethiopia demographic and health survey 2005. Cent Statist Agen Add Aba 12: 15-28.
[Google Scholar]
- Coates J, Swindale A, Blinsky P (2007) Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide: version 3. Washington D.C: FDNJ Technical Assistance Project, Academy for Educational Development, 2007.
[Google Scholar]
- Habyarimana F, Zewotir T, Ramroop S (2014) Spatial distribution and analysis of risk factors associated with Anemia among women of reproductive age: Case of 2014 Rwanda demographic and health survey data. Open Pub Healt J 11: 123-132.
[Google Scholar]
- Holmes MD, Dalal S, Volmink J, Adebamowo CA, Njelekela M, et al. (2003) Non-communicable diseases in sub-Saharan Africa: What we know now. PLoS Med 7: e1000244.
[Crossref] [Google Scholar] [PubMed]
- Kennedy G, Ballard T, Dop M (2013) Guidelines for measuring household and individual dietary diversity. Rome; Italy: Nutrition and consumer protection division, Food and Agriculture Organization (FAO) of the United Nations.
- Msemo OA, Bygbjerg IC, Moller SL (2018) Prevalence and risk factors of preconception anemia: A community based cross sectional study of rural women of reproductive age in northeastern Tanzania. PLoS One 13: e0208413.
[Crossref] [Google Scholar] [PubMed]
- Rahman MS, Mushfiquee M, Masud MS, Howlader T (2019) Association between malnutrition and anemia in under-five children and women of reproductive age: Evidence from Bangladesh Demographic and Health Survey 2011. PLoS One 14: e0219170.
[Crossref] [Google Scholar] [PubMed]
- Ray Yip, Ramakrishnan U (2002) Experiences and Challenges in Developing Countries. PLoS One 132: 827S-830S.
[Google Scholar] [PubMed]
- World Health Organization (2001) Haemoglobin concentrations for the diagnosis of anemia and assessment of severity. Vitamin and mineral nutrition information system. Geneva: World Health Organization.
Citation: Kedir M, Nebi TD, Bereka S (2023) Sedentary Lifestyle in the Elderly and Its Association with the Development of Cerebrovascular Disease.
Health Sci J. Vol. 17 No. 5: 1024.