Keywords
Hemoptysis; Hirudo medicinalis; Fibroscopy examination; Byparasitological examination
Introduction
Leeches (Hirudo medicinalis) have been used in medicine for thousands of years to treat a wide range of ailments. Nowadays, leeches are used successfully for only a few conditions, notably in the field of reconstructive or microsurgery. However, they can act like parasite and infest human which cause wide range of symptoms. The species of human importance (order: Gnathobdellida; family: Hirudinidae) are divided into land leeches and aquatic leeches. Aquatic leeches enter the human body through orifices and occur worldwide. Human infestation with land leeches is more common than with aquatic leeches, but the latter more commonly cause dangerous infestations [1]. Aquatic leeches live in fresh water and have weak jaws because they do not require attachment to the skin for feeding purposes but to the mucosa. Infestation is rare. Most cases occur in low-income countries where access to safe water is a problem [2]. Some cases have been reported from Europe [3]. Aquatic leeches enter the human body during swimming or drinking by attaching to the conjunctiva, mucousmembranes of the nose, larynx, pharynx, esophagus, urethra, vagina, or anus, or else. In this paper we report an unusual case of upper airways obstruction by leech infestation and we review some similar cases in the literature.
Case Report
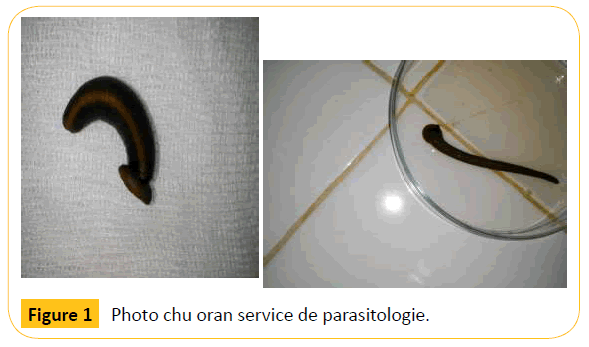
M.A a 64-year-old male patient, from Saida city, with emphysema history and smoker, wasreferred from the Saidahospital to the department of pneumology of the EHU Oran for exploration of hemoptysis. At admission the patient presented abundant hemoptysis, dysphonia, pain and sensation of something in the throat. The patient was hemodynamically stable without fever. Theinitial ortholyringique, cardiaque, radiologic exploration, complete blood countand coagulation tests were normal. In the fibroscopique examination there was a bleeding from his vocal cords and a live dark brown mass could be seen on the pharyngeal surface. The removal of the parasite was impossibleso local anesthesia was instaured using xylocaine in order to paralyze the parasite. After fibrscopy the patient expelled the parasite and it was brought to the parasitology and medical mycology department of the CHU Oranand identified as themedicinal leech Hirudo medicinalisn (Figure 1). Retrospective history showed that the patient has a farm in rural area, nearby there is stream of fresh water and he usually drinks this water. He has history with leech infestation in the past, he used traditional treatment by ingestion of chewing tobacco but this time this treatment was not effective. Bleeding ceased soon after the leech was expelled and discharged without any problem on the next day. Follow-up one week later revealed no further symptoms.
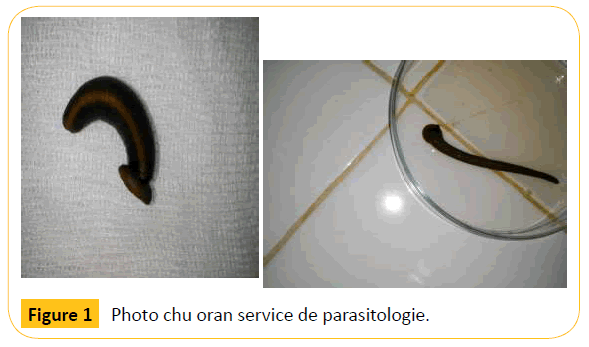
Figure 1: Photo chu oran service de parasitologie.
Discussion
Leeches belong to the Annelida phylum and Hirudinea class. Most of leeches are hematophagous, which makes them predominantly blood suckers that feed on blood from vertebrate and invertebrate animals. Almost 700 species of leeches have been described. Among them, 100 species are marine, 90 terrestrial and the rest of them live in freshwater.
Leeches are parasites that vary in color and range in length from a few millimeters to half a meter; they are cylindrical or leaf - like in shape, depending on the contraction of their bodies, Leech bodies are composed of 34 segment [4]
A leech has two suckers, one at each end. The mouth is located on the small sucker and has three jaws with sharp teeth that make a Y-shaped incision in the flesh [2].
In tropical regions, leech bites on the skin are a common event. However, serious consequences of leech bite injury to the internal viscera are uncommon. If they do occur, they can cause significant morbidity and may even be fatal [1]. The clinical symptoms are variable depending on location. Internal attachment of leeches in different areas of human body such as nose [5], pharynx [6], larynx [4], vagina [7], bronchi, eyes and rectum have been reported in several cases.
After the contaminated water is drunk, the leech may adhere to anywhere along the upper aero digestive tract. Possible areas are the nasal cavity oropharynx and hypopharynx, larynx, trachea, and esophagus
From that location they secrete a cocktail of anticoagulant substances among them hirudin, which inhibits coagulation of the blood and start to suck blood, leeches ingest blood averaging 890% of their weight, for these reasons they can cause severe anemia. They grow rapidly through blood sucking and may stay where they are for some weeks.
Leech endoparasitism described worldwide, and for the pharyngolaryngeal localization cases came from Africa (morocco, Ethiopia), India and Middle East (Turkey, Iran, Syria, Yemen) and one case from developed country Spain (Table 1). Our case is the first case described from Algeria in decades.
| Country (area) |
Age/Gender |
Mode of contamination |
Symptoms |
Complications |
Duration |
Diagnostic |
Removal |
Leech (lengh(cm)) |
Evolution |
References |
| Morocco |
17 m/M |
Swimming
15 |
Hematemesis
Pallor
Fever 38°C
POLYPNEIQUE
Cough |
Respiratory distress
ANEMIA |
One week |
Fibroscopy One week
endoscopy |
forceps |
5/1.5 |
discharged |
[8] |
| Yemen |
60/M |
Drinking
2 months |
Progressive hoarseness, blood stained sputum, mild throat pain
Hemoptysis |
|
One month |
Indirect laryngoscopy –
One month |
Spontaneously expelled |
5.5/1 |
discharged |
[9] |
| India |
48/M |
Drinking |
Cyanotic
Severe breathlessness
Difficulty of speaking
Inspiratory stidor with bilateral decreased air |
|
3 hours |
Indirect laryngoscopy
3hours |
Direct laryngoscopy
Attached to the forceps |
5/0.5 |
discharged |
[10] |
| Turkey |
7/M |
|
spitting blood
inspiratory stridor |
|
|
Indirect laryngoscopy |
Direct laryngoscpy
General anesthesia
forceps |
|
discharged |
[4] |
| 35/M |
|
spitting blood |
|
3 months |
Indirect laryngoscopy |
Direct laryngoscopy
local anaesthesia |
5 |
|
|
| 8/F |
|
spitting blood,
difficulty in breathing
inspiratory stridor |
|
|
Indirect laryngoscopy |
Direct laryngoscpy
General anesthesia
forceps |
4 |
|
|
| 42/M |
|
spitting blood, dysphagia
feeling of a foreign body in the throat |
|
2 weeks |
Indirect laryngoscopy
2 weeks |
Direct laryngoscopy
local anaesthesia
forceps |
|
|
|
| Syria |
6/M |
Drinking |
Cough; hemoptysis; sensation of suffocation; stridor |
Severe respiratory distress
Cachectic
Cyanotic
pale |
3 hours |
Indirect mirror laryngoscopy
3 hours
One month |
General anesthesia forceps |
7 |
discharged |
[11] |
| Morocco |
38 /F |
Drinking |
Toux, hemoptysis, dyspnea, aphonie |
|
10 days |
Fibroscopy |
Laryngoscpie direct
forceps |
4cm |
discharged |
[12] |
| Spain |
34/M |
drinking |
a foreign
body sensation in his throat
hemoptysis
dysphagia
recurrend hemoptysis dysphagia melena and progessive nocturnal dyspnea |
|
1 week |
transnasal laryngoscopy
1 week |
local anesthesia failed
under general
anesthesia, the microlaryngoscopic extraction |
Theromyzontessulatum
5cm |
|
[3] |
| Turkey |
5/F |
Drinking |
Vomiting fresh blood
Epistaxis, Pallor
Tachycardie
fever |
anemia |
3 days |
Laryngoscopy |
Local anesthesia |
Limnatisnilotica
3.7/0.7 |
discharged |
[13] |
| Turkey |
8/F |
Drinking |
several days
hemoptysis
subfebrile |
|
|
|
forceps |
Limnatislinotica
5/1 |
discharged |
[6] |
| Iran |
73/M |
Drinking |
intermittent hemoptysis,
dysphagia,dyspnea
stridor |
|
|
fiberoptic laryngoscopy |
4 ml lidocaine |
|
discharged |
[14] |
| |
|
|
|
|
|
|
|
|
|
|
| Iran |
41/F |
Drinking |
Respiratory distress
Tachypnea, stridor, feeling something in the throat vomiting nausea |
|
|
laryngoscopy |
General anesthesia
Lidocaine
forceps |
|
discharged |
[15] |
| Morocco |
71/F |
Drinking |
hemoptysis |
anemia |
8 days |
Expelled from the nose |
|
7/1.5 |
discharged |
[16] |
| Ethiopia |
7/M |
Drinking |
Blood stained saliva, shortness of breath |
Anemia |
14 days |
Laryngoscopy |
Forceps
General anesthesia |
6 |
discharged |
[2] |
| |
|
|
|
|
|
|
|
|
|
|
| Iran |
64/M |
Drinking
8 |
Hemoptysis ,sensation of foreign body, dysphonia, mild respiratory distress |
|
|
Indirect laryngoscopy |
General annsethesia
Rigide laryngoscopy
forceps |
5.5 |
discharged |
[17] |
Service de parasitologie et mycology chu OranprBenmansour.
Table 1: Literature review about laryngeal leech infestation
| Country (area) |
Age/Gender |
Mode of contamination |
Symptoms |
Complications |
Duration |
Diagnostic |
Removal |
Leech (lengh(cm)) |
Evolution |
References |
| Morocco |
17 m/M |
Swimming
15 |
Hematemesis
Pallor
Fever 38°C
POLYPNEIQUE
Cough |
Respiratory distress
ANEMIA |
One week |
Fibroscopy One week
endoscopy |
forceps |
5/1.5 |
discharged |
[8] |
| Yemen |
60/M |
Drinking
2 months |
Progressive hoarseness, blood stained sputum, mild throat pain
Hemoptysis |
|
One month |
Indirect laryngoscopy –
One month |
Spontaneously expelled |
5.5/1 |
discharged |
[9] |
| India |
48/M |
Drinking |
Cyanotic
Severe breathlessness
Difficulty of speaking
Inspiratory stidor with bilateral decreased air |
|
3 hours |
Indirect laryngoscopy
3hours |
Direct laryngoscopy
Attached to the forceps |
5/0.5 |
discharged |
[10] |
| Turkey |
7/M |
|
spitting blood
inspiratory stridor |
|
|
Indirect laryngoscopy |
Direct laryngoscpy
General anesthesia
forceps |
|
discharged |
[4] |
| 35/M |
|
spitting blood |
|
3 months |
Indirect laryngoscopy |
Direct laryngoscopy
local anaesthesia |
5 |
|
|
| 8/F |
|
spitting blood,
difficulty in breathing
inspiratory stridor |
|
|
Indirect laryngoscopy |
Direct laryngoscpy
General anesthesia
forceps |
4 |
|
|
| 42/M |
|
spitting blood, dysphagia
feeling of a foreign body in the throat |
|
2 weeks |
Indirect laryngoscopy
2 weeks |
Direct laryngoscopy
local anaesthesia
forceps |
|
|
|
| Syria |
6/M |
Drinking |
Cough; hemoptysis; sensation of suffocation; stridor |
Severe respiratory distress
Cachectic
Cyanotic
pale |
3 hours |
Indirect mirror laryngoscopy
3 hours
One month |
General anesthesia forceps |
7 |
discharged |
[11] |
| Morocco |
38 /F |
Drinking |
Toux, hemoptysis, dyspnea, aphonie |
|
10 days |
Fibroscopy |
Laryngoscpie direct
forceps |
4cm |
discharged |
[12] |
| Spain |
34/M |
drinking |
a foreign
body sensation in his throat
hemoptysis
dysphagia
recurrend hemoptysis dysphagia melena and progessive nocturnal dyspnea |
|
1 week |
transnasal laryngoscopy
1 week |
local anesthesia failed
under general
anesthesia, the microlaryngoscopic extraction |
Theromyzontessulatum
5cm |
|
[3] |
| Turkey |
5/F |
Drinking |
Vomiting fresh blood
Epistaxis, Pallor
Tachycardie
fever |
anemia |
3 days |
Laryngoscopy |
Local anesthesia |
Limnatisnilotica
3.7/0.7 |
discharged |
[13] |
| Turkey |
8/F |
Drinking |
several days
hemoptysis
subfebrile |
|
|
|
forceps |
Limnatislinotica
5/1 |
discharged |
[6] |
| Iran |
73/M |
Drinking |
intermittent hemoptysis,
dysphagia,dyspnea
stridor |
|
|
fiberoptic laryngoscopy |
4 ml lidocaine |
|
discharged |
[14] |
| |
|
|
|
|
|
|
|
|
|
|
| Iran |
41/F |
Drinking |
Respiratory distress
Tachypnea, stridor, feeling something in the throat vomiting nausea |
|
|
laryngoscopy |
General anesthesia
Lidocaine
forceps |
|
discharged |
[15] |
| Morocco |
71/F |
Drinking |
hemoptysis |
anemia |
8 days |
Expelled from the nose |
|
7/1.5 |
discharged |
[16] |
| Ethiopia |
7/M |
Drinking |
Blood stained saliva, shortness of breath |
Anemia |
14 days |
Laryngoscopy |
Forceps
General anesthesia |
6 |
discharged |
[2] |
| |
|
|
|
|
|
|
|
|
|
|
| Iran |
64/M |
Drinking
8 |
Hemoptysis ,sensation of foreign body, dysphonia, mild respiratory distress |
|
|
Indirect laryngoscopy |
General annsethesia
Rigide laryngoscopy
forceps |
5.5 |
discharged |
[17] |
Service de parasitologie et mycology chu OranprBenmansour.
Table 1: Literature review about laryngeal leech infestation
Aquatic leeches are common in Algeria where two species have been described Hirudo medicinalis and Limnatis nilotica. In the past leeches infestation were a major cause of morbidity and mortality for animals, and even cases of human infestation were described in French soldiers, travels and gerlach’s series [8-10]. At present, the situation is unclear rarely described maybe because of adequate safe water supply and/or the use of traditional medication by the local population to remove the leech.
We also performed literature review about pharyngolaryngeal leeches infestation from 1999 to 2015. There are 17 cases reported in the literature (Table 1). The age distribution of patients is ranged from 17 months to 73 years. The male are more affected than female (11 vs 5).
The major symptoms reported are the result of bleeding such as hemoptysis, hematemesis and blood in sputum sometimes associated with symptom of obstruction (dysphonia, cough, sensation of something in the throat, dyspnea, and even suffocation) and fever in children. Any delay of diagnostic can lead to lethal complications such as severe anemia and suffocation.
The symptoms may be misdiagnosed as asthma, laryngitis, tuberculosis, hookwormand malignancies [11].
The diagnostic of leech infestation was done by laryngoscopy or fibroscopy. And in some cases until the patient spontaneously expelled the leech [9] and only in few reports diagnostic was suspected on the medical history of the patient.
All patients have a contact with exposed water; the mode of contamination is more likely drinking than swimming (Table 1)
Removal of leeches from the larynx is difficult, can be performed by direct laryngoscope with the patient under general or local anesthesia and the parasite is extracted with forceps, in fortunate cases the leech was spontaneously expelled by the patient [9], after application of xylocaine in our case or attached to the forceps [10].
In four reports patients consulted only when they failed to remove the leech with traditional medicine (ingestion of chewing tobacco as our patient, dehydratation….). The application of traditional medications may lead to dislodging of the leech deeper and may result in suffocation to death [2].
The length of leeches ranged from to 3.7 to 7 cm. Only 4 reports identified the leech to species level Myxobdella Africana in 6 cases from Kenya, Limnatis linoticain 2 cases from turkey and Theromyzon tessulatum in one cases from Spain [3,6,13-21].
After the removal the evolution is favorable and all patient discharged, in some cases blood transfusion or iron supplement were required to correct the anemia.
Conclusion
Leeches endoparasitism should be included in the differential diagnosis of patients with hemoptysis and or signs of airways obstruction, especially in patients with a history of contact with unfiltered water where aquatic leeches are commonly found.
Cases such as this should be considered as emergencies, and all measures should be taken to avoid complications and death. Therefore, to prevent leech infestation in endemic regions, local people are advised to be informed more effectively about the necessity to use safe water.
7581
References
- Heukelbach J, Hengge UR (2009) Bed bugs, leeches and hookworm larvae in the skin. Clin Dermatol27:285-290.
- Mekonnen D (2013) Leech infestation: The unsual cause of upper airways obstruction. RthiopnJ Health Sci23: 1.
- Kuehnemund M, Bootz F (2006)Rare living hypopharyngeal foreign body. Head Neck 28:1046-1048.
- Kaygusuz I, Yalcin S, Keles E (2001) Leeches in the larynx. Eur Arch Otolaryngol 258:455-457.
- Ghimire A, Acharya A (2008)Unusual cause of unilateral epi-staxis: nasal leech infestation. JNMA J Nepal Med Assoc47:38-40.
- Bulent A, Ilknur O, Beray S, Tulin C, Ulku T, et al. (2010) An unusual cause of hemoptysis in a child: live leech in the posterior pharynx. Trop Biomed27:208-210.
- Hailemariam B (1995)Post-menopausal vaginal bleeding due to vaginal wall leech infestation. Ethiop Med J33:183-185.
- Iraqi M R, Squali FZ (1999) Hématémèseet obstruction des voiesrespiratoires dues à la sangsue. Archives de pédiatrie6:479-480.
- Al-Hadrani DC, Faucon F, Fingerhut A (2000) Hoarseness due to leech ingestion. The Journal of Laryngology and Otology 14: 145–146.
- Pandey CK, Sharma R, Baronia, Agarwal A, Singh N (2000)Anunsual cause of respiratory distress: live leech in the larynx. Anest Anal 90:1227-1228.
- Mohammad Y, Rostum M, Dubaybo BA (2002) Laryngeal hirudiniasis: an unusual cause of airway obstruction and hemoptysis. PediatrPulmonol 33:224-226.
- Amara B,Aakka M, Elhord S,Elbouzidi R, Rahimi H, et al. (2006) Une cause inhabituelled’hémoptysie : la sangsue. Rev PneumolClin62: 252-254.
- Agin H, Ayhan FY, Gulfidan G, Cevik D, Derebasi H (2008)Severe anemia due to the pharyngeal leech Lim-natisnilo-tica in a child. Turkiyeparazitolderg 32:247-248.
- Rahimi-Rad MH, Alizadeh E, Samarei R (2011) Aquatic leech as a rare cause of respiratory distress and hemoptysis. Pneumologia60:85-86.
- Vegari S, Ghaffarlou M, Davarimajd L, EJ Golzari (2012) Globus sensation due to a mobile foreign body in 41-year-old female.Journal of cardiovascular and thoracic research 4: 29-30.
- Hanim FZ,Bourkadi JE,Cherkaoui FZ,Soualhi M,Zahraoui R,(2012) Cause inhabituelle d’hémoptysie : la sangsue. Revue de Pneumologie clinique 68: 327-328.
- Rajati M, Irani S, Khadivi E, Bakhshaee M (2014) An Unusual Cause of Dysphonia with Hemoptysis: A Laryngeal Live Leech . Iranian Journal of Otorhinolaryngology26:181-183.
- Gerlach A, Gerlach Z (1975) Leeches in the respiratory system.LaryngolRhinolOtol 54:123–132.
- Morel (1948)Les sangsues pathogens. Le Chasseur Français N°620 Juin 1948 Page 133.
- VitalMA (1938) observation de sangsue dans la tracheeartere-Bronchotomie-guerison.Encyclograpie des sciencemedicale 28-30.
- Cundall DB, Whitehead SM, Hechtel F (1986)Severeanaemia and death due to the pharyngeal leech Myxobdellaafri-cana.Trans R Soc Trop Med Hyg 80:940-944.