Maria Mitsogianni1, Ioannis Vasileiadis1, Maria Parisi1, Georgios Tzanis1, Efstathia Kampisiouli1, Zoi Psaroudaki2, Efstathia Perivolioti2, Kimon Fountoulis2, Christina Routsi1, Serafeim Nanas1* and Sotirios Tsiodras3
1First Critical Care Department, National and Kapodistrian University of Athens, Evangelismos Hospital, Athens, Greece
2Department of Clinical Microbiology, Evangelismos Hospital, Athens, Greece
3Fourth Department of Internal Medicine, National and Kapodistrian University of Athens, Attikon University Hospital, Athens, Greece
- *Corresponding Author:
- Prof. Serafeim Nanas
First Critical Care Department
National and Kapodistrian University of Athens
Evangelismos Hospital, Ypsilantou 45-47
106 75, Athens, Greece
Tel: +306973036448
Fax: +302132043385
E-mail: a.icusn@gmail.com
Received Date: November 23, 2015; Accepted Date: January 25, 2016; Published Date: January 31, 2016
Keywords
Bloodstream infection; Central venous catheter bundle; Hand hygiene; Education intervention
Abbreviation
BSI: Blood Stream Infection; CVC: Central Venous Catheter; CLABSI: Central Line-Associated Blood Stream Infection; ICU: Intensive Care Unit; COPD: Chronic Obstructive Pulmonary Disease; APACHE II: Acute Physiology and Chronic Health Evaluation II; SAPS III: Simplified Acute Physiology Score III; SOFA: Sequential Organ Failure Assessment
Introduction
Bloodstream infection (BSI) is a major cause of morbidity and mortality worldwide and is associated with prolonged hospital stay and additional health care costs [1-4].
Compared to the general hospital population, critically ill patients are at increased risk of BSI because of underlying comorbid conditions [5,6], prior receipt of antimicrobial therapy and widespread use of invasive devices such as central venous catheters (CVCs). The presence of the latter is a common predisposing factor for BSI (central line associated bloodstream infection - CLABSI) [7]. The risk varies depending on ward-type, institution and geographical region [8].
Specific strategies have been shown to significantly reduce the rate of CLABSIs in intensive care units (ICUs) [9] and have been adopted in the Centers for Disease Control and Prevention (CDC) and other guidelines [10-12]: full barrier technique during CVC insertion, skin antisepsis with chlorhexidine, catheter site selection with avoidance of the femoral vein, preinsertion hand hygiene and early removal of unnecessary catheters. Behavioral interventions that improve the compliance of the personnel also seem to play a significant role [13]. The efficacy of these measures has been confirmed in several large scale studies in the recent years [14-18], whereas the goal of a zero CLABSI rate has not been achieved.
Moreover, hand hygiene is generally regarded as an effective way to reduce health-care infection rates - and consequently BSI rates - caused by cross-transmission of pathogens [19]. Based on the World Health Organization initiative [20], several campaigns aiming at promoting hand hygiene in healthcare have been introduced in the last years [21]. However, compliance between healthcare workers still remains low [22].
The objective of the present study is to evaluate the impact of a series of technical and educational interventions consisting of CLABSI prevention measures and a hand hygiene promotion program on the rates of BSI in an ICU.
Methods
Study design
This prospective interventional study was conducted in the 30- bed intensive care unit (ICU) of Evangelismos hospital, a 1000- bed tertiary care hospital in Athens, over a 17-month period (October 2010 to February 2012).
All adult patients admitted to the ICU for more than 48 hours were eligible to participate in the study. The exclusion criteria were ICU hospitalization in the previous three months, brain death, pregnancy and microbiologically confirmed sepsis at the admission point.
Data collected included demographics, preexisting medical conditions, severity scores on admission, days of antimicrobial therapy, days of central venous catheterization as well as number of catheter-insertions during the ICU stay. All episodes of bacteraemia were recorded. The patients were followed until acquiring a BSI, until discharge from the ICU or for a maximum of 30 days.
The study was divided in two periods: a baseline observation period (October 2010 - April 2011) and an intervention period (May 2011 - February 2012). The study protocol was approved by the Ethical Committee of the hospital.
Interventions
We introduced a CVC insertion and maintenance bundle consisting of:
Full barrier precautions during the insertion including donning of sterile gloves, sterile gown, cap and mask by the physician inserting the catheter, large sterile draping of the patient, skin antisepsis with 2 % chlorhexidine preparation and avoidance of the femoral site when possible. Compliance with best practices was ensured by a checklist which had to be filled by the physician at every new insertion.
Regular inspection of the insertion site for signs of infection and replace of the dressing when dump or soiled or routinely once per week.
Moreover, we implemented a series of measures in order to promote hand hygiene among healthcare workers:
Indications for hand hygiene were posted at strategic locations throughout the ICU.
Healthcare workers were informed about the necessity of hand hygiene in a lecture.
In order to further support our measures, a booklet of standards regarding central line care and hand hygiene according to recommended guidelines was distributed to the personnel.
Definitions
A BSI was considered to be ICU-related if it was detected at least 48 hours after admission. Both primary and secondary BSIs were considered in the analysis. Cultures of common skin contaminants were not included in the analysis, unless the microorganism was isolated in two different samples. An antimicrobial day was defined as a day for which any amount of an antimicrobial agent was administered to an individual patient.
Microbiological methods
Blood cultures were obtained when indicated by the treating physician in case of clinical suspicion of infection. All specimens were processed using standard methods at the microbiological laboratory of the hospital. Detection of microorganisms was performed by the automatic blood culture system BD BACTECTM 9000 Series.
Statistical analysis
The data analysis was performed using SPSS for Windows Version 19.0. Continuous variables are expressed as mean (standard deviation - SD) and categorical variables as counts and percentages.
Variables were compared using the independent-sample t-test or Pearson chi square test, as appropriate. Risks were compared using odds ratios (OD) with corresponding 95 % confidence intervals (CI). All tests were two-tailed, and p-values less than 0.05 were considered to indicate statistical significance.
Outcome measures
The primary endpoint of the study was the acquisition of bacteraemia. The BSI rate was expressed as the number of BSIs per 1000 patient days.
Results
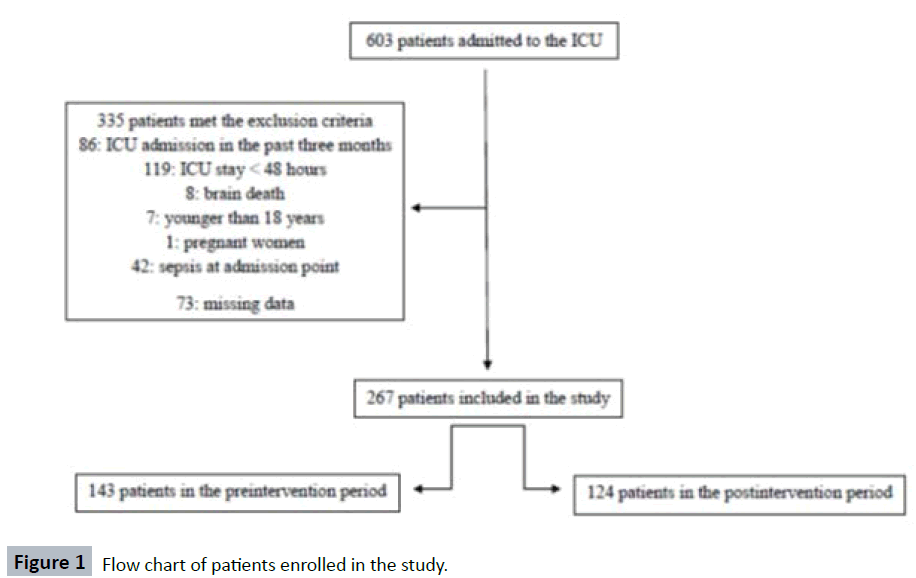
As shown in Figure 1, a total of 603 patients were admitted to the ICU during the study period, of which 267 were eligible for enrolment in the study (143 in the baseline and 124 in the intervention period) and were included in further analysis.
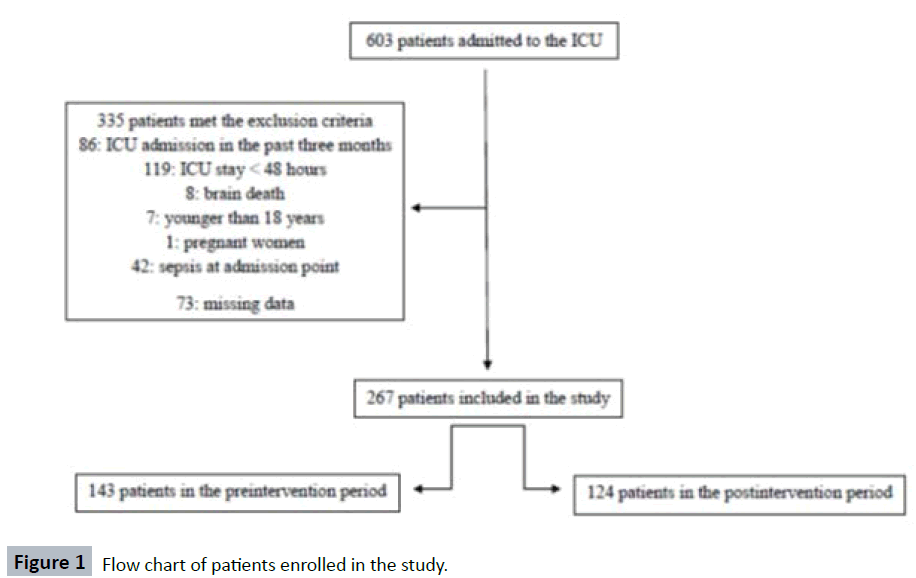
Figure 1: Flow chart of patients enrolled in the study.
Their main demographic and clinical characteristics are summarized in Table 1. Overall, the study groups were similar in both periods. An exception to this is the higher SOFA gravity score in the intervention period (p = 0.017), indicating a larger extent of organ failure in this group of patients. Nevertheless, such a difference in the two populations was not confirmed by the APACHE II (p = 0.438, death prediction: p = 0.244) or SAPS III (p = 0.493, death prediction p = 0.693) severity scores.
Table 1: Patient demographic data and clinical characteristics.
| |
Preintervention (n=143) |
Postintervention (n=124) |
p value |
| Patient-days |
2379 |
2037 |
|
| Male, n %) |
90 (62.9) |
89 (71.8) |
0.126 |
| Age, years, mean (SD) |
56.8 (18.6) |
56.5 (19.7) |
0.906 |
| Length of stay, days, mean (SD) |
16.6 (9.8) |
16.4 (10.9) |
0.869 |
| ICU-Mortality, n (%) |
46 (32.2) |
38 (30.6) |
0.789 |
| Severity scores on admission, mean (SD) |
|
|
|
| SOFA |
6.4 (2.9) |
7.4 (3.7) |
0.017 |
| APACHE II |
15.0 (6.0) |
15.6 (6.8) |
0.438 |
| APACHE II death prediction |
23.9 (15.7) |
26.2 (16.6) |
0.244 |
| SAPS III |
57.6 (15.0) |
56.2 (18.4) |
0.493 |
| SAPS III death prediction |
33.1 (22.9) |
32.0 (23.5) |
0.693 |
| Type of admission, n (%) |
|
|
|
| Medical |
76 (53.1) |
52 (41.9) |
0.067 |
| Elective surgery |
22 (15.4) |
24 (19.4) |
0.392 |
| Emergency surgery |
24 (16.8) |
21 (16.9) |
0.974 |
| Trauma, non-surgical |
20 (14.0) |
28 (22.6) |
0.068 |
| Comorbid conditions, n (%) |
|
|
|
| Diabetes mellitus |
22 (15.4) |
22 (17.7) |
0.605 |
| Cancer |
27 (18.9) |
18 (14.5) |
0.342 |
| COPD |
8 (5.6) |
9 (7.3) |
0.579 |
| Immunosuppression |
10 (7.0) |
11 (8.9) |
0.570 |
| Chronic heart failure |
7 (4.9) |
4 (3.2) |
0.494 |
| Chronic renal failure |
3 (2.1) |
5 (4.0) |
0.355 |
| Total antimicrobial days, mean (SD) |
16.3 (10.0) |
15.6 (11.1) |
0.568 |
| CVC-days, mean (SD) |
|
|
|
| Internal jugular / subclavian |
15.1 (9.8) |
15.4 (11.3) |
0.808 |
| Femoral |
1.8 (3.9) |
2.0 (4.7) |
0.679 |
| No of CVC-insertions, mean (SD) |
|
|
|
| Internal jugular / subclavian |
2.2 (1.7) |
1.8 (1.5) |
0.065 |
| Femoral |
0.4 (0.7) |
0.3 (0.7) |
0.599 |
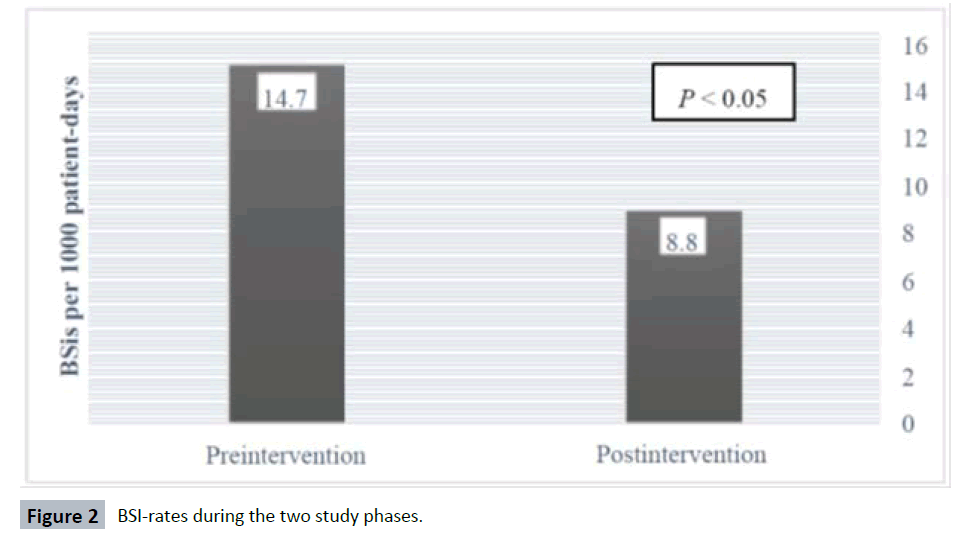
The distribution of BSI rates during the study period is illustrated in Figure 2. Bacteraemic incidents occurred in 35 out of 143 patients in the baseline period (24.5 %, 14.7 incidents per 1000 patient-days) as well as in 18 out of 124 patients in the intervention period (14.5 %, 8.8 incidents per 1000-patient days), indicating a statistically significant lower incidence of BSI after implementing the intervention (p = 0.042, OR 1.9, CI 1.02 - 3.58). The type of isolated microorganisms can be seen in Table 2.
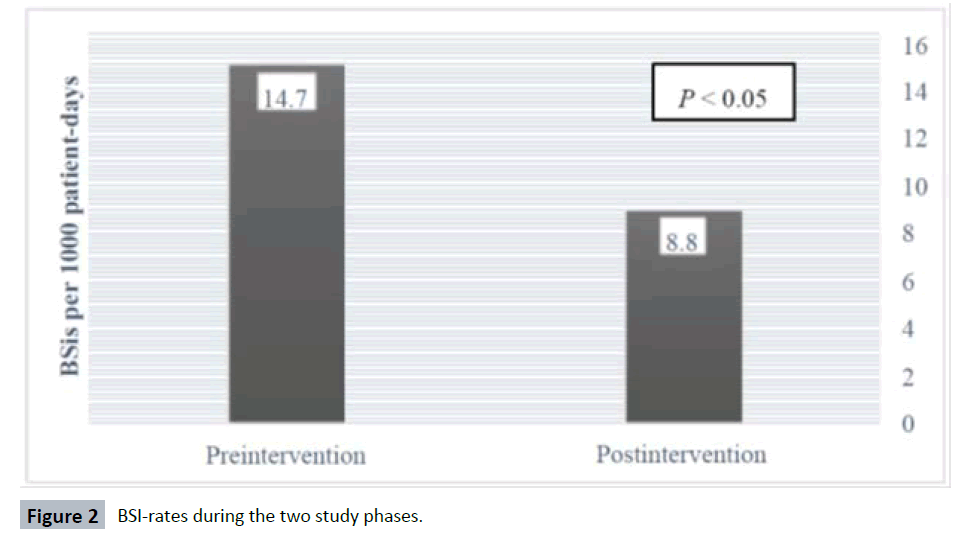
Figure 2: BSI-rates during the two study phases.
Table 2: Type of isolated pathogens.
| Isolated pathogen, n (%) |
Preintervention (n=35) |
Postintervention (n=18) |
| Klebsiella pneumoniae |
12 (34.3) |
7 (38.9) |
| Acinetobacter baumannii |
12 (34.3) |
5 (27.8) |
| Providencia stuartii |
4 (11.4) |
4 (22.2) |
| Pseudomonas aeruginosa |
2 (5.7) |
1 (5.6) |
| Proteus mirabilis |
2 (5.7) |
0 (0.0) |
| Serratia marcesens |
1 (2.9) |
0 (0.0) |
| Staphylococcus aureus |
1 (2.9) |
0 (0.0) |
| Staphylococcus epidermidis |
1 (2.9) |
0 (0.0) |
| Candida albicans |
0 (0.0) |
1 (5.6) |
Days of central line catheterization, number of catheterinsertions, days of antimicrobial therapy and patient mortality did not change significantly during the two study phases, neither in the study population (Table 1) nor in the patients that developed bacteraemia (Table 3).
Table 3: Catheter characteristics and antimicrobial therapy until the acquisition of BSI.
| |
Preintervention (n=35) |
Postintervention (n=18) |
p value |
| CVC-days, mean (SD) |
|
| Internal jugular /Subclavian |
10.0 (5.9) |
11.8 (5.9) |
0.304 |
| Femoral |
1.5 (3.0) |
1.9 (3.2) |
0.656 |
| CVC-insertions, mean (SD) |
|
| Internal jugular /Subclavian |
1.7 (1.4) |
1.7 (0.9) |
0.954 |
| Femoral |
0.4 (0.8) |
0.4 (0.8) |
0.845 |
| Antimicrobial days, mean (SD) |
11.8 (5.8) |
12.4 (5.4) |
0.701 |
Discussion
Main findings
The present study has addressed the effects of changing practice, education and feedback on decreasing BSI rates. Our findings demonstrate that implementation of a CVC-care bundle and a program to improve hand hygiene was associated with a significant reduction in BSIs.
Our study was completed one year after an intervention regarding ventilator-associated pneumonia in the same ICU, which could have already positively affected the working practices of the ICU personnel.
Factors that could have played an independent role to the reduction of BSI like device utilization and antibiotic use remained at the same level during the two study periods, indicating that the observed difference occurred through our intervention. Moreover, although SOFA gravity score at ICU admission has been shown to be independently associated with the acquisition of bacteraemia [23], we observed a higher admission SOFA in the postintervention period. The lower BSI incidence in this phase despite this additional risk factor supports further the effectiveness of our measures.
The prospective character of our study and the large sample size also confirm the reliability of our findings. We applied a program of multifaceted interventions which, although challenged in the recent years [24], are still widely recognized to be more effective than single component ones. The interventions we used are simple and inexpensive and would, therefore, be easily implemented in other ICUs.
Relation to previous findings
Our results support the findings of previous studies demonstrating significant reduction in CLABSI after introducing a series of interventions, as first shown in the landmark study of Berenholtz et al. [9] and then adopted in the CDC guidelines [10]. Based on these guidelines, we introduced an intervention to prevent CLABSI and combined it with a hand hygiene improvement program. By promoting hand hygiene as a means of general infection prevention we were able to affect not only the catheter-related but also the secondary bacteraemia, which has been suggested to be associated with a higher attributable mortality [25].
On the other hand, our findings show that this quality improvement intervention resulting in reduction of BSI was not associated with a better prognosis and are in opposition to the widely accepted reasoning that bacteraemia is a negative prognostic factor for critically ill patients [1-5]. This common belief has already been challenged in previous studies that did not demonstrate excess mortality between bacteraemic patients [26,27], leaving the matter of the clinical significance of BSI still open. However, it has to be pointed out that our study was not designed to control the effect of a BSI preventing intervention on the ICU outcome and, consequently, the role of factors like type of microorganism and antimicrobial treatment on the prognosis has not been evaluated.
Limitations
A limitation of our study is that it is quasi-experimental and conducted at a single medical center. Furthermore, during the study period there was no hospital-wide change in the CVCinsertion technique or in the hand hygiene promotion. The catheters inserted outside the ICU, where the quality of insertion and maintenance could not be controlled, were not removed upon admittance unless there were clinical signs of infection. In addition, our BSI rate may be underestimated given that patients were not followed after discharge from the ICU. Furthermore, by concurrently undertaking a CVC care bundle and a hand hygiene promoting program, we were not able to differentiate at what point each of the two infection preventive strategies is responsible for our final result.
Conclusion
The existing data suggest that BSIs may be preventable to a large extent. Our intervention study supports this evidence by demonstrating a significant decrease in BSI rates after the implementation of a simple series of measures. Nevertheless, there is definitely still room for improvement in this area, as zero risk for infection has yet not been reported.
Conflicts of Interest
None
8760
References
- Pittet D, Tarara D, Wenzel RP (1994) Nosocomial bloodstream infection in critically ill patients. Excess length of stay, extra costs, and attributable mortality.JAMA 271: 1598-1601.
- Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, et al. (2006) Sepsis in European intensive care units: results of the SOAP study.Crit Care Med 34: 344-353.
- Ziegler MJ, Pellegrini DC, Safdar N (2015) Attributable mortality of central line associated bloodstream infection: systematic review and meta-analysis.Infection 43: 29-36.
- Bearman GM, Wenzel RP (2005) Bacteremias: a leading cause of death.Arch Med Res 36: 646-659.
- Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, et al. (2009) International study of the prevalence and outcomes of infection in intensive care units.JAMA 302: 2323-2329.
- Timsit JF, Laupland KB (2012) Update on bloodstream infections in ICUs.CurrOpinCrit Care 18: 479-486.
- McGee DC, Gould MK (2003) Preventing complications of central venous catheterization.N Engl J Med 348: 1123-1133.
- Alberti C, Brun-Buisson C, Burchardi H, Martin C, Goodman S, et al. (2002) Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study.Intensive Care Med 28: 108-121.
- Berenholtz SM, Pronovost PJ, Lipsett PA, Hobson D, Earsing K, et al. (2004) Eliminating catheter-related bloodstream infections in the intensive care unit. Crit Care Med 32: 2014-2020.
- Centers for Disease Control and Prevention (CDC) (2011) Vital signs: central line-associated blood stream infections--United States, 2001, 2008, and 2009.MMWR Morb Mortal Wkly Rep 60: 243-248.
- American Society of Anesthesiologists Task Force on Central Venous Access, Rupp SM, Apfelbaum JL, Blitt C, Caplan RA, et al. (2012) Practice guidelines for central venous access: a report by the American Society of Anesthesiologists Task Force on Central Venous Access.Anesthesiology 116: 539-573.
- O’Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, et al. (2011) Healthcare Infection Control Practices Advisory Committee (HICPAC). Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis 52: 162-193.
- Walz JM, Memtsoudis SG, Heard SO (2010) Prevention of central venous catheter bloodstream infections.J Intensive Care Med 25: 131-138.
- Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, et al. (2006) An intervention to decrease catheter-related bloodstream infections in the ICU.N Engl J Med 355: 2725-2732.
- Palomar M, Álvarez-Lerma F, Riera A, Díaz MT, Torres F, et al. (2013) Impact of a national multimodal intervention to prevent catheter-related bloodstream infection in the ICU: the Spanish experience. Crit Care Med 41: 2364-2372.
- Bion J, Richardson A, Hibbert P, Beer J, Abrusci T, et al. (2013) The Matching Michigan collaboration and writing committee. ‘Matching Mitchigan’: a 2-year stepped interventional programme to minimise central venous catheter-blood stream infections in intensive care units in England. BMJ QualSaf 22: 110-123.
- Miller SE, Maragakis LL (2012) Central line-associated bloodstream infection prevention.CurrOpin Infect Dis 25: 412-422.
- HELICS-ICU working group (2004) Surveillance of Nosocomial Infections in Intensive Care Units. Protocol, version 6.1. Brussels: Scientific Institute of Public Health, IPH/EPI reports D/2004/2505/48.
- Allegranzi B, Pittet D (2009) Role of hand hygiene in healthcare-associated infection prevention.J Hosp Infect 73: 305-315.
- Pittet D, Allegranzi B, Boyce J (2007) World Health Organization World Alliance for Patient Safety First Global Patient Safety Challenge Core Group of Experts (2009) The World Health Organization Guidelines on Hand Hygiene in Health Care and their consensus recommendations. Infect Control HospEpidemiol 30: 611-622.
- Huang GK, Stewardson AJ, Grayson ML (2014) Back to basics: hand hygiene and isolation.CurrOpin Infect Dis 27: 379-389.
- Marra AR, Edmond MB (2012) Hand Hygiene: State-of-the-Art Review With Emphasis on New Technologies and Mechanisms of Surveillance.Curr Infect Dis Rep 14: 585-591.
- Routsi C, Pratikaki M, Sotiropoulou C, Platsouka E, Markaki V, et al. (2007) Application of the sequential organ failure assessment (SOFA) score to bacteremic ICU patients.Infection 35: 240-244.
- Squires J, Sullivan K, Eccles M, Worswick J, Grimshaw JM (2014) Are multifaceted interventions more effective than single-component interventions in changing health-care professionals’ behaviours? An overview of systematic reviews. Implement Sci 9: 152.
- Renaud B, Brun-Buisson C; ICU-Bacteremia Study Group (2001) Outcomes of primary and catheter-related bacteremia. A cohort and case-control study in critically ill patients.Am J RespirCrit Care Med 163: 1584-1590.
- Digiovine B, Chenoweth C, Watts C, Higgins M (1999) The attributable mortality and costs of primary nosocomial bloodstream infections in the intensive care unit.Am J RespirCrit Care Med 160: 976-981.
- Blot SI, Depuydt P, Annemans L, Benoit D, Hoste E, et al. (2005 ) Clinical and economic outcomes in critically ill patients with nosocomial catheter-related bloodstream infections.Clin Infect Dis 41: 1591-1598.