Aissa A1*, Yengui H2, Habboul Z2, Khattat N2, Helal KB2, Nouri A3 and Alouini R1
1Department of Imaging, Ibn El Jazzar Hospital, Kairouan, Tunisia
2Departement of Pediatrics, Ibn El Jazzar Hospital, Kairouan, Tunisia
3Departement of Pediatrics Surgery, Fattouma Bourguiba Hospital, Monastir, Tunisia
Corresponding Author:
Aissa A
Department of Imaging
Ibn El Jazzar Hospital
Kairouan, Tunisia
Tel: 77226300
E-mail: amene.aissa@rns.tn
Received date: November 15, 2016; Accepted date: November 25, 2016; Published date: November 30, 2016
Citation: Aissa A, Yengui H, Habboul Z, Khattat N, Helal KB, et al. A Rare Case of a Giant Congenital Pulmonary Hemangioma. Arch Med. 2016, 8:6 doi:10.21767/1989-5216.1000176
Copyright: © 2016 Aissa A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Intrathoracic hemangiomas; Imaging; Newborn
Introduction
Intrathoracic hemangiomas are extremely uncommon. These have previously been described as arising from the diaphragm, bronchus, trachea, and pericardium. They may also arise within the lung itself [1]. We present a unique case of giant congenital pulmonary hemangioma causing respiratory distress in a newborn.
Case Report
Female infant, aged 1 month, admitted for dyspnea and fever. Physical examination revealed the presence of a small tuberous angioma skin of the chest wall. Radiography of the chest showed a poorly systematized pneumonia in the left lung (Figure 1).
Figure 1: Radiography of the chest: a poorly systematized pneumonia in the left lung.
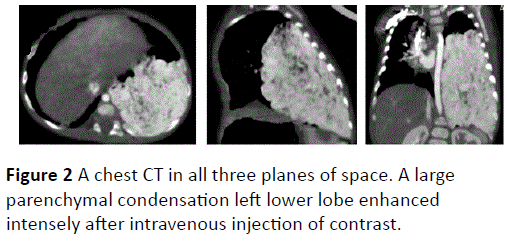
The outcome was negative after antibiotic treatment with worsening dyspnea. Further exploration by a chest CT was performed to rule out pulmonary sequestration. He showed a large parenchymal condensation left lower lobe enhanced intensely (Figure 2). The diagnosis was another location before pulmonary hemangiomatosis angiomatous skin location of the chest wall. The patient was operated. She had a left thoracotomy and intraoperative exploration showed a large hyper-vascularized mass unventilated. The pathological diagnosis was that of pulmonary capillary hemangiomatosis. The postoperative course was unfavorable and the patient had died.
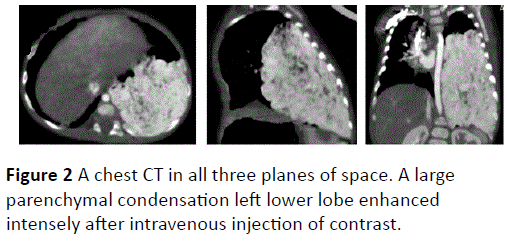
Figure 2: A chest CT in all three planes of space. A large parenchymal condensation left lower lobe enhanced intensely after intravenous injection of contrast.
Discussion
Congenital hemangiomas are less common than the infantile variety. These lesions are most commonly seen on the head, torso, and extremities and have rapidly involuting and non involuting subtypes. A diffuse vascular abnormality reported in children is pulmonary capillary hemangiomatosis. In this condition multiple hemangiomas are found in the lung interstitium and ronchovascular walls [1].
Clinical features also differ among patients. Although two thirds of all patients primarily suffer from signs of dyspnea, hemoptysis is described as first clinical symptomas well [2].
But sometimes it presents considerable diagnostic problems, as it is associated with nonspecific symptoms such as cough and dyspnea. Similarly, there are no characteristic findings on physical examination [3].
Perfusion scanning in patients with PCH usually shows diffusely enhanced perfusion, predominantly in the lower lobes. This corresponds with the regions of lung most affected by the proliferating capillary masses [3]. Our case and observation might be useful in distinguishing pulmonary capillary hemangiomatosis from other histopathologic variants of pulmonary hypertension, such as pulmonary veno-occlusive disease.
Rapidly involuting congenital hemangiomas, including multifocal and visceral hemangiomas, may take weeks to months to involute, favoring a concerted, patient effort at nonoperative management in newborns whose symptoms from the hemangioma are clinically favorable [1].
The use of steroids to promote involution in a neonate is not without potential morbidity with regard to long-term developmental effects. The possibility of treating this hemangioma with angioembolization was considered. Once the patient developed significant respiratory compromise, a surgical approach seemed more definitive than an attempt at angioembolization [1].
Conclusion
Our patient show that familial intrathoracic hemangiomas might occur early in life. The rare disorder was not associated with other life-threatening pathology but with signs of pulmonary hypertension. Thus, the diagnosis should be considered in young children with right heart failure, right ventricular hypertrophy, or pulmonary hypertension. Open lung biopsy was required to confirm the diagnosis. There is no established therapy in infancy.
17920
References
- Capizzani TR, Patel H, Hines MH, Mott RT, Petty JK (2008) A unique case of a giant congenital pulmonary hemangioma in a newborn.J PediatrSurg 43: 574-578.
- Wirbelauer J, Hebestreit H, Marx A, Mark EJ, Speer CP (2011) Familial pulmonary capillary hemangiomatosis early in life.
- Masur Y, Remberger K, Hoefer M (1996) Pulmonary capillary hemangiomatosis as a rare cause of pulmonary hypertension.Pathol Res Pract 192: 290-295.