Xiaosheng Lu1,2*, Meijing Huang3, Jinmin Zhao4, Hao Peng5, Jichen He6, Wen Wei1, Tingyang Li1, Hui Li1 and Wei Li1
1Department of Orthopaedics, The People’s Hospital of Baise, Baise 533000, Guangxi Zhuang Autonomous Region, PR China
2Southwest Affiliated Hospital of Youjiang Medical University for Nationalities, Baise 533000, Guangxi Zhuang Autonomous Region, PR China
3National Health School of Baise, Baise 533000, Guangxi Zhuang Autonomous Region, PR China
4The First Affiliated Hospital of Guangxi Medical University, Nanning 530021, Guangxi Zhuang Autonomous Region, PR China
5Department of Orthopaedics, The People’s Hospital of Wuhan University, Wuhan 430060, Hubei, PR China
6The Graduate School of Guangxi Medical University, Nanning 530021, Guangxi Zhuang Autonomous Region, PR China
*Corresponding Author:
Xiaosheng Lu
Department of Orthopaedics, The People’s Hospital of Baise, Baise 533000, Guangxi Zhuang Autonomous Region, PR China
Tel: 8613006911077
E-mail: suguoshengv@sina.com
Received date: 27 August 2016; Accepted date: 26 September 2016; Published date: 30 September 2016
Citation: Lu X, Huang M, Zhao J, et al. A Retrospective Study of Improved System of Micro-Endoscopic Discectomy for the Lumbar Spinal Canal Stenosis. Ann Clin Lab Res. 2016, 4: 3. doi: 10.21767/2386-5180.1000122
Keywords
Micro-endoscope, Minimally invasive surgery, Lumbar stenosis
Introduction
Lumbar stenosis is a common and complicated disease. Although traditional decompression surgery is well suggested, it can easily lead to spinal instability and scarring from hematology because of the destruction of the posterior spinal structures [1]. It can maintain the stability of spinal biomechanics on the premise of full decompression [2]. Therefore, it has drawn great attention by an increasing number of spine surgeons. The MED (micro-endoscopic discectomy) was first applied to lumbar disc herniation by Smith and Foly in 1997. It is easily accepted by patients because it causes less pain and has the advantages of small incision, high-resolution [3]. It has also been recognized by more and more specialists for its full decompression, less trauma, spinal stability and rapid recovery [4-6]. With the development of minimally invasive surgery, the application of microsurgery in spine surgery is increasing [7,8]. In recent years, a major breakthrough in the treatment of lumbar stenosis has been made. However, there is rare comparative retrospective study between MED and traditional discectomy. We performed this retrospective study to compare these two methods, which treated 300 cases with lumbar stenosis from June 2004 to May 2011. We aim to offer a better surgical solution for lumbar spinal stenosis.
Materials and Methods
Ethical statement
All study procedures were reviewed and approved by the institutional ethics review board at the people’s hospital of Baise and conducted according to the principles expressed in the declaration of Helsinki. Informed consent was exempted by the board due to the retrospective nature of this research. Patient records/information were anonymized and deidentified prior to analysis.
The Patients
All symptoms of those patients met the following conditions. First of all, the main symptom is nerve intermittent claudication less than 500 meters accompanying intractable pain. Secondly, the imaging (CT or MRI) shows lumbar spinal sagittal diameter <10 mm, lateral recess <2 mm, it is lateral recess stenosis which conform to the clinical symptoms and physical signs. What’s more, this study eliminates lumbar diseases such as congenital stenosis or instability and spondylolisthesis. Last but not least, there is discharge or recurrent attacks after 3 months of conservative treatment. The patients were divided into two groups, the improved MED group A and the traditional group B. All of them were examined by X-ray, CT, MRI and proved to be lumbar stenosis.
There were 80 males and 68 females in group A, the average age was 46 ± 10.2 years old?33 to 80 years old). The average duration of the disease was 49 ± 13.8 months (7 months to 28 years). All cases were caused by degenerative disease. 120 cases were combined with lumbar disc herniation. The clinical manifestations were low back pain and intermittent claudication of varying degrees. 23 cases combined with cauda equina symptom. 103 cases involved one-segment spinal stenosis, including 14 cases in L3/4, 43 cases in L4/5 and 46 cases in L5/S1. 38 cases involved two segments, including 16 cases in L3/4 and L4/5 and 22 cases in L4/5 and L5/S1. 7 cases had spinal stenosis from L3/4 to L5/S1. 34 cases had hypertension and 9 cases had diabetes mellitus.
Group B included 82 males and 70 females, the average was 48 ± 12.4 years old (34 to 82 years old). The average duration of the disease was 50 ± 14.4 months (9 months to 26 years). Degeneration is the cause for all cases. 123 cases combined with lumbar disc herniation. The clinical manifestations were low back pain and intermittent claudication of varying degrees. 25 cases combined with cauda equina symptom. 106 cases had one-segment spinal stenosis, including 16 cases in L3/4, 47 cases in L4/5 and 43 cases in L5/S1. 40 cases had two segments, including 22 cases in L3/4 and L4/5, 18 cases in L4/5 and L5/S1. 6 cases involved from L3/4 to L5/S1. 36 cases complicated with hypertension and 7 cases had diabetes mellitus.
It showed that the lumbar spinal and the lateral recess stenosis, dural and nerve root compression were caused by the following factors such as lumbar small joint hyperplasia and cohesion, yellow ligament hypertrophy, lumbar disc herniation. It can be diagnosed by X-ray, CT or MRI imaging. There was no significant difference between the two groups in terms of the general information such as sex ratio, duration, segment stenosis, the average age and complications (P>0.05) (Table 1).
| Group |
Gender |
Age (x ± s, years) |
Duration (x ± s, months) |
Spinal Stenosis (segments, numbers) |
Complication (diseases, numbers) |
| |
Male |
Female |
One |
Two |
Three |
Hypertension |
DM |
| A (148) |
80 |
68 |
46.5 ± 5.33 |
48 ± 23 |
103 |
38 |
7 |
34 |
9 |
| B (152) |
82 |
70 |
47.1 ± 5.21 |
49 ± 19 |
106 |
40 |
6 |
36 |
7 |
| P value |
0.9852 |
0.3249 |
0.6814 |
|
|
|
|
|
Table 1: Comparison of two groups of patients before treatment
Operation Methods
Anesthesia, position and orientation
The patient is set up in bow and prone position, therefore the abdomen could be hung up after epidural anesthesia. Carm X-ray machine was used for accurate position during the whole procedure.
Surgical method
Similar to the report by Li et al. [9], the improved system was applied in group A. Firstly, for improved working channel of MED, it has 360° rotational camera system and up-down adjustable fixing device, the button is designed with a 40° curve to expand operative vision field. Secondly, the new system changed the traditional straight chisel into 2.6 mm diameter curved one, more effective deal with the hypertrophied lamina and the proliferated small joints. Thirdly, using the self-invented L-shaped reverse curette for calcified lumbar disc. The handle length was 32 cm, the convex side was upward and the surface was smooth, the concave side was downward and the edge was sharp. With combination with the mobile MED devices it can be freely to tilt or sway. 1.6 cm to 2.6 cm length longitudinal incision was made 1 cm beside the targeted vertebral segment. For multiple segments, after making the posterior mid-line incision, both side of the vertebral segment inserted guide wires. In order inserting the expanding pipe and working channel to the lamina. Drilling a bone window carefully and removing the lower edge of upper lamina. For complicated cases with serious hypertrophied lamina and the proliferated small joints, firstly should use the micro curved chisel to make it thinner and then open the bone window from the lamina with the bone forceps. Removing the yellow ligament completely, expanding gradually the range of decompression, the working channel should be appropriate tilted outward to accommodate the lamina. By adjusting the work channel, all the soft tissues and osteoarthritis of lateral recess should be removed thoroughly to achieve full decompression of the nerve roots on both sides. Lumbar disc should be excised and the central tube should be enlarged if combined with lumbar disc herniation. The standard of decompression was that the limited nerve root can move inward around 1 cm [10]. Besides, the dura and nerve root can move 3 mm to 4 mm freely. The probe can be inserted into the nerve root site along the nerve root.
In group B, 6 cm to 15 cm length longitudinal incision was made along the mid-line of the spinous process. Separating the soft tissues and exposing the targeted up and down vertebral lamina. Removing all or half of the lamina and gradually exposing the yellow ligament and dural sac. Checking and confirming the cause of the stenosis, then carefully cutting out the yellow ligament, hyperplasia of the articular facets, calcification of the posterior longitudinal ligament and herniated disc to make the nerve root moving freely and release the compression of the dural sac as well. Decompression standard is the same with group A.
Clinical evaluation and standard
The postoperative efficacy of those two groups was determined by Nakai standards [11].
Excellent: The signs and symptoms disappeared completely, restoring the original work;
Good: The symptoms and positive signs disappeared basically, but low back pain and lower limb soreness remained after exertion;
Fair: The symptoms and signs were improved significantly, but left sequelae such as mild low back pain or leg discomfort. Those patients cannot be fully engaged in the work and life;
Poor: The improvement of symptoms and signs is not obvious, cannot be engaged in normal work and life.
Statistical Analysis
Data are presented as mean ± standard of deviation, SPSS 11.0 statistical analysis software package are used for statistical analysis. Measurement data between groups and within groups were analyzed using independent sample t-test and paired t-test, chi-square test with count data. For all statistical tests, P<0.05 was considered significant.
Results
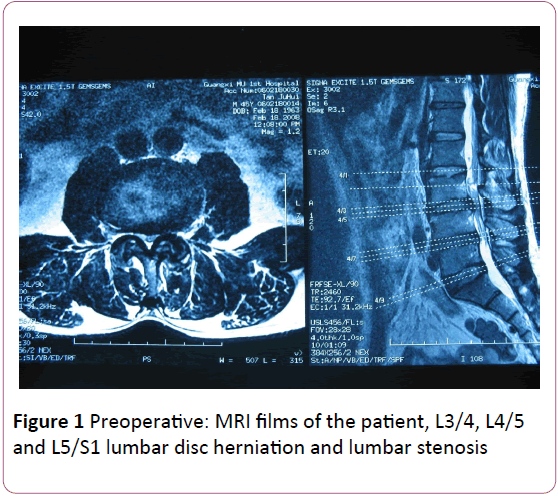
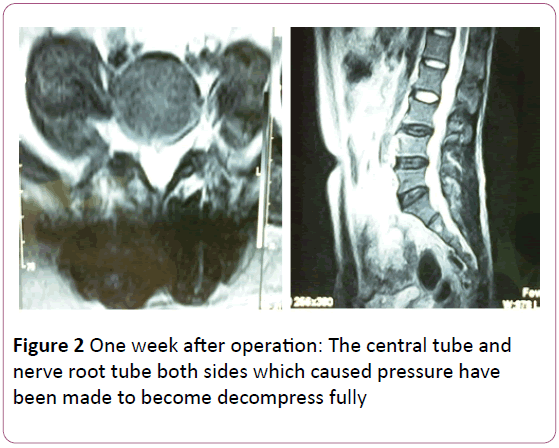
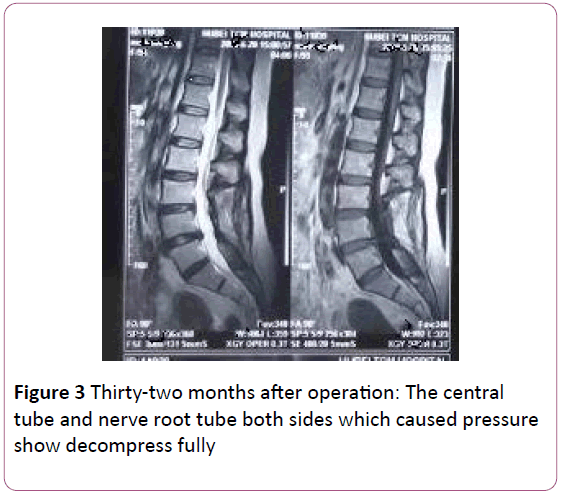
All cases had been successfully operated. The average blood loss during operation in group A was 83.10 ml ± 5.21 ml, while in group B it was 150.13 ml ± 10.23 ml. The hospitalization after operation in group A was 7.2 ± 1.1 d, while in group B, it was 11.9 ± 1.4 d. There were significant differences between two groups (P<0.01) (Table 2). Patients in group A were followed up for 14 to 56 months with an average time of 28 months, while in group B, they were followed up for 13 to 54 months with an average time of 27 months. Example: a typical case (Figures 1-3). There were 5 cases suffering endorachis rupture in each of the two groups, which were healed by corresponding treatment such as patch, fibrin glue closure and gelatin sponge. There were 4 cases suffering from spine instability in group B after 4 years of treatment. And those patients were treated with cumber fusion jointed between GSS pedicle screw fixation. There were no other complications such as operational error, nerve root injury and cauda equina injury. There were no recurrent cases reexamined by imaging. According to the Nakai classification, there were 72 excellent cases, 65 good cases, 9 fair cases and 2 poor cases in group A. The excellent and good rate was 92.6%, while in group B, there were excellent 75 cases, 64 good cases, 10 fair cases and 4 poor cases. The excellent and good rate was 91.4%. There was no significant difference between the two groups (P>0.05) (Table 3).
| Group |
N |
Blood Loss (ml) |
Hospitalization After Operation (d) |
| A |
148 |
83.10 ± 5.21* |
7.2 ± 1.1* |
| B |
152 |
150.13 ± 10.23 |
11.9 ± 1.4 |
| Note: Compared with the B group?*p<0.05 |
Table 2: Comparison of two groups of surgical indicators
| Group |
N |
Excellent |
Good |
Fair |
Poor |
And Good Rate |
| A |
148 |
72 |
65 |
9 |
2 |
92.6? |
| B |
152 |
75 |
64 |
10 |
4 |
91.4? |
| Note: Compared with the B group: p<0.05 |
Table 3: Evaluated by Nakai classification
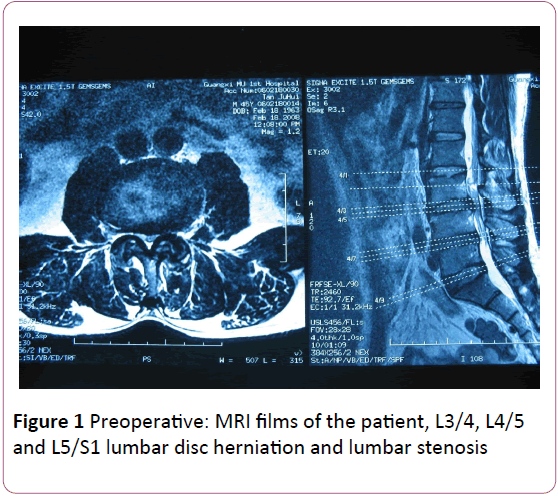
Figure 1: Preoperative: MRI films of the patient, L3/4, L4/5 and L5/S1 lumbar disc herniation and lumbar stenosis
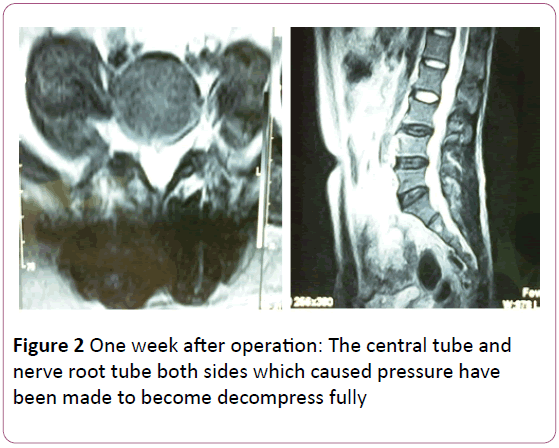
Figure 2: One week after operation: The central tube and nerve root tube both sides which caused pressure have been made to become decompress fully
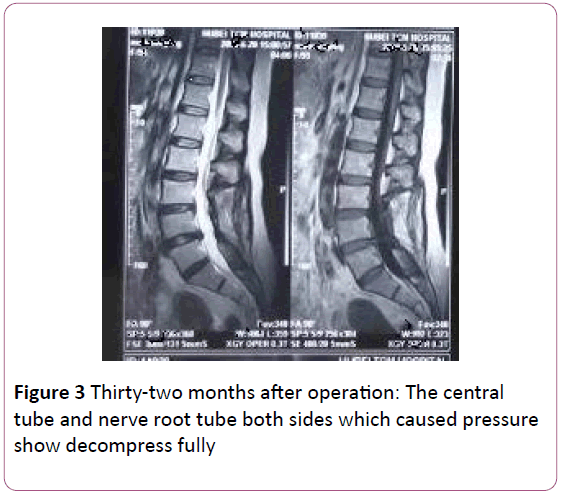
Figure 3: Thirty-two months after operation: The central tube and nerve root tube both sides which caused pressure show decompress fully
Discussion
Lumbar stenosis is a common and multiple illness that leads to low back and leg pain. The patients have to be treated when their disease is associated with nerve root lesions. Traditional surgery can decompress completely, but there are some shortcomings such as larger trauma, slow recovery and potential instability of lumbar. Because of the important role of the spinal posterior structure which maintains the stability of the spine [12], and there is no or less damage to blood supply of paraspinal and nerve, the minimally invasive techniques of spinal has been widely drawn attention.
Comparing the methods of improved system of MED with traditional discectomy for lumbar stenosis, MED is a combination of traditional discectomy and endoscopic techniques. Clearer surgical field can guarantee complete fenestration, nerve root channels to expand, and the separation of adhesions around the nerve root for operative field amplification due to the advanced video recording system [8,10]. Dural sac and nerve root can be fully decompressed. It can resect hypertrophic ligament in medial edge of the facet and expand the nerve root canal with the advantages of minimally invasive, good curative effect [13]. As Li et al. [9] reported, using a modified endoscope and special designed instruments could reduce decompression of the spinal canal. There were no serious complications. The results were satisfied and expanded the surgical indications by MED for lumbar stenosis. Xu et al. [14] also reported that using mobile micro-endoscopic discectomy technique for lumbar disc herniation and canal stenosis can be much easier to reduce decompression and provides good results. We made the fullest use of combination advantages of the improved system. The excellent and good rate was 92.6% in group A which was close to the reports in domestic and abroad. There was no lumbar instability in group A and 4 cases were suffered from spine instability in group B after treatment of 4 years. And those patients were treated with lumber fusion jointed between GSS pedicle screw fixation, which suggests that excessive iatrogenic injury may accelerate the degenerative lumbar instability. MED is a kind of "minimally invasive approach ", called "separation of eye and hand". It needs to be operated within a narrow channel, because its vision position is limited. So that the surgeons should have the operating experience of open surgery and minimally invasive surgery and be well-known of the spinal local anatomical knowledge [15]. It takes a long time to practice and accumulate experience to master skilled techniques. Qi et al. [16] pointed out that the operation key points of MED technique is the working channel and position of opening window which should be aligned with the disc herniation, avoid spinal hemorrhage, and use strict hemostasis to prevent surgical field becoming unclear. At the same time, it’s much important to prevent the omission of lesions due to limited vision. The efficacy of minimally invasive surgery is close to classic surgery for retaining the complex of lamina, spinouts’ process and interspinous ligament [17,18]. Compared with traditional surgery, the MED has the advantages of fewer traumas, less bleeding, shorter hospitalization time, and fewer complications and less impact on the stability of the spine.
The most common complications of surgery for lumbar stenosis are dural rupture, nerve root injury, infection, fixed position error. The following points should be paid attention to. Firstly, according to the medical history, clinical symptoms and imaging examination results, the cases should be selected strictly. Secondly, in order to avoid positioning error, it’s of significant importance to read X-ray carefully and repeatedly adjusting the position during the procedure. Thirdly, it is easier to start from the narrower side which the patients’ symptoms are usually more serious. Before removing the yellow ligament, it is important to cut the homolateral lamina and related osteoarthritis structure to achieve decompression. It can help avoiding the damage of endorachis and nerve root. Fourthly, it should be extremely careful and gentle when separating the yellow ligaments from endorachis to avoid the rupture. If occurred, endorachis reparation is needed during treatment. For difficult cases, biological proteins glue and gelatin sponge filling should be used and the end of the bed should be elevated after surgery. Liu et al. [19] calculated that iatrogenic cause could account for 76.9% of all the dural accidental injuries. Totally 10 cases occurred endorachis rupture from the two groups, which may be caused by incomplete separation of the yellow ligament from endorachis or the operating methods were not careful enough. Fifthly, it is effective to start from the site of herniated disc, then gently stripping and revealing outward, separating and protecting the vein plexus. By application of gelatin sponge, thrombin, brain cotton piece with adrenaline, bone wax and bipolar of electricity to achieve stopping bleeding completely. By repeated saline flushing it can also help to prevent adhesion and postoperative infection, reduce inflammatory mediators and bone debris. If it is difficult to enter the spinal canal, bleeding is serious and difficult to stop, vision is not ideal, decompression is not satisfying, nerve or endorachis injury is hard to handle, it is necessary to turn back to the traditional open surgery. There were 3 cases in group B treated with open surgery and ended with success. Finally, the critical surgical technique is removing tissue completely which damaged the normal morphology and slip space of nerve root [20]. Probing the nerve root freely after decompression to confirm the operation effect. The dural membrane should be with no pressure and no summon up. Both of the two groups have followed the above principles and achieved satisfactory results.
This study shows that improved system compared with traditional discectomy for lumbar stenosis not only could obtain the same satisfactory results of therapy, but also overcome the defects of traditional surgery, which can be one of the ideal minimal invasive operations.
Conclusion
The curative effects of improved system of microendoscopic discectomy (MED) and traditional discectomy for the treatment of lumbar stenosis are satisfactory, but the improved system of MED can overcome the disadvantages of traditional discectomy, less cost and faster heal, which can be one of the ideal minimal invasive operations.
Limitations of the Study
Some limitations exist in the research, such as relatively short time in the study, few selected cases of patients, and some patients were unwilling to return to the hospital for reexamination. Meanwhile, because of the limited funding, the number of selected cases is not enough to attain the representative research results. Therefore, we strongly hope to have more research funding, in order to make the research results more representative.
Acknowledgment
During this topic research process, we got help from many departments and individuals, such as the projects of science and technology, and other personnel not involved in this project research, all of them offered a great support and help in this research. All of members of this research group show our deepest appreciation to them, and wish them good health and everything goes well.
Declaration
There were no conflicts between all of the authors. And the authors did not receive any outside funding or grants in support of their research for or preparation of this work. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity.
Funding
Self-funded plan subject Guangxi Zhuang Autonomous Region Health Department [Gui Wei science and education (2010(11)Z2010489)].
17228
References
- Li QC, Liu XW, Hu HL (2008) The unilateral approach bilateral decompression microendoscopy for lumbar stenosis. Liuzhou Medical 21: 20-23.
- Peng H, Liu SQ, Tao HY (2004) Posterior spinal microsurgical discectomy for lumbar disc herniation. Orthop J Chin 12: 498-500.
- Wang H, Wang HY, An CH (2002) The treatment of microsurgical discectomy surgery for lumbar disc herniation. Orthop J Chin 22: 17-19.
- Perez-Cruet MJ, Foley KT, Isaacs RE (2002) Microendoscopic lumbar discectomy: technical note. Neurosurgery 51(5 Suppl): 129-136.
- Brayda BM, Cinnella P (2000) Posterior endoscopic discectomy (and other procedures). Eur Spine J 9: 24-29.
- Ren H, Hao FH, Zhao CY (2008) The clinical application analysis of posterior microendoscopic. Hebei Medical University 29: 747-748.
- Li B, He CH, Xie XT (2008) Microscope-assisted decompression for degenerative lumbar spinal canal stenosis. Chinese Journal of Spine and Spinal Cord 18: 345-348.
- Peng YQ, Yang L, Jiang H (2003) The operative strategy for the treatment of multi-segmental lumbar disc herniation by MED. Chinese Journal of Spine and Spinal Cord 13: 79-81.
- Li Q, Tan B, Liu XW (2008) Surgical treatment of lumbar vertebral canal stenosis with endoscope and special designed instruments. Chinese Journal of Spine and Spinal Cord 185: 341-344.
- Hu YG (2001) Spine surgery. Beijing: People's Medical Publishing House: 1480.
- Nakai O, Ockawa A, Yamaura L (1991) Long-term roentgenographic and functional changes in patients who were treated wide fenest ration for central lumbar stenosis. J Bone Joint SuryAm 73: 1184-1191.
- Tian HZ, Wang YJ, Li YN (1994) The experimental study of the rear structure excision impact on the stability of lumbar spine. Orthop J Chin 14: 557-560.
- Wang C, Wu XT, Bu XP (2003) Posterior approach microendoscopic surgery in the treatment of lumbar spinal stenosis. J Minim Invasive Surg 3: 288-289.
- Xu BS, Destandau J, Xia Q (2009) Mobile microendoscopic discectomy technique for lumbar disc herniation and canal stenosis. Orthop J Chin 29: 112-116.
- Li LJ, Zhou W, Lu QY (2008) The preliminary report on minimally invasive transforaminal lumbar interbody fusion in the treatment of lower lumbar spine disorders. Chinese Journal of Reparative and Reconstructive Surgery 22: 501-503.
- Qi Q, Bi ZG, Zhao CB (2006) Comparative study of microsurgical lumbar discectomy and microendoscopic discectomy. Orthop J Chin 14: 328-330.
- Zuo JL, Tan J, Zhang LH (2004) The effects of the spinal canal volume and spinal stability on the posterior approaches. Orthop J Chin 12: 1152-1154.
- Kalbarczyk A, Lukes A, Seiler RW (1998) Surgical treatment of lumbar spinal stenosis in the elderly. Acta Neurochir 140: 637-641.
- Liu P, Zeng XB, Liu F (2008) Surgical management of dural injuries and postoperative cerebrospinal fluid fistulas in spinal surgeries. Chinese Journal of Reparative and Reconstructive Surgery 22: 715-718.
- Xiao RC, Li Q,Tang ZH (2008) Treatment of multi-segmental lumbar disc herniation and spinal canal stenosis. Chinese Journal of Reparative and Reconstructive Surgery 22: 404-407.