Keywords
Neuropathic pain; Nociceptive pain; Mononeuropathy
Introduction
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage [1]. Broadly pain is classified in three types nociceptive pain, inflammatory pain, associated with tissue damage and infiltration of immune cells, and neuropathic pain associated with damage or dysfunction in the nervous system or by its abnormal function. Neuropathic pain, in distinction to nociceptive pain, is burning, electric, tingling and shooting in nature and continuous or paroxysmal. Nociceptive pain is caused by the stimulation of peripheral of A-delta and C-polymodal pain receptors, by algogenic substances (e.g., histamine bradykinin, substance P, etc.) while neuropathic pain is produced by damage to the peripheral or central nervous systems. Neuropathic pain results from damage of primary afferent neuron, spinal cord injury, and central nervous system. When the nerves that carry messages to the brain and spinal cord from the peripheral body parts are damaged, referred as Peripheral Neuropathy (PN). The feature of neuropathic pain is chronic allodynia (pain from a stimulus that ordinarily does not elicit a painful response e.g., light touch) and hyperalgesia (increased sensitivity to a normally painful stimuli). Hyperalgesia occurs as Primary, caused by sensitization of C-fibers, occurs immediately within the area of the injury and Secondary, caused by sensitization of dorsal horn neurons, occurs in the undamaged area surrounding the injury. Certain disease condition like chronic diabetes, cancer, AIDS, Leprosy, Cervical protrusion and foraminotomy are at high risk to get PN [2]. Chronic ethanol consumption leads to neuropathic pain [3]. From the behavioral point of view, neuropathic pain is associated with hypersensitive pain behavior, including allodynia (pain due to non-noxious stimulus) and hyperalgesia (enhanced pain due to noxious stimuli). Neuropathic pain results from the increased neuronal expression and/or activation of ion channels and receptors that initiate and mediate the abnormal generation of action potentials and synaptic transmission in pain.
Types of neuropathy
? Mononeuropathy
? Polyneuropathy
Known causes of acquired neuropathies include:
o Diabetes
o Several rare inherited diseases.
o Alcoholism
o Poor nutrition or vitamin deficiency
o Cancer and chemotherapy
o Immune system
o Certain medications
o Kidney or thyroid disease
o Infections such as Lyme disease, shingles, or AIDS
? Hereditary neuropathies
? Idiopathic neuropathies
Neuropathic pain is not based on a single pathophysiological process and is often refractory to treat with analgesics such as, opiates and nonsteroidal anti-inflammatory drugs. The defense mechanisms involve pain signal transduction from the nociceptorsperipheral nervous system-spinal dorsal horns-thalamus-cortex and the pain control system from the cortex-periaqueductal grey matternucleus raphe magnus-spinal dorsal horn. In normal individual the transduction system and the pain management is under control but in PN imbalance between these two results in the neuropathy in persons. In PN the lesions can be located at various locations in the body such as peripheral nerve, dorsal root ganglion or dorsal root or PN may be due to compression, inflammation, ischemia, trauma, deficit nutritions or any degenerative disorder [4].
Treatment of Neuropathic Pain
Untimely recognition and insistent management of neuropathic pain may be vital to successful outcome. Several treatment options are offered by an interdisciplinary management team includes systemic medication, physical modalities (e.g., Physical rehabilitation), psychological modalities (e.g., behavior modification, relaxation training), invasive procedures (e.g., Triggerpoint injections, epidural steroids, sympathetic blocks), spinal cord stimulators, intrathecal morphine pump systems and various surgical techniques (e.g., dorsal root entry zone lesions, cordotomy and sympathectomy). But while offering these options caution is warranted as it may produce deaffrentation and exacerbate the underlying neuropathic mechanisms. So the mainstay for the management of NP is the tricyclic anti-depressants, anticonvulsants, local anaesthetics, corticosteroids, substance-p depletors, autonomic drugs and NMDA-antagonists.
Tricyclic antidepressants (TCAs)
TCA have been successfully used in the management of NP since last 25 years. Amitriptyline and Nortriptyline exerts their effect through the interactions with serotonin or norepinephrine neurotransmitter system [5]. But the use of anti-depressant is slowed down because of frequent side effects like hallucinations, dizziness, lightheadedness, dependence and abusability [6].
Anticonvulsants
Phenytoin and carbamazepine are widely used as anticonvulsants. These drugs exert their membrane-stabilizing properties by blocking sodium channels specically and therefore reduce neuronal excitability in nociceptors. Carbamazepine is the drug of choice for the treatment of trigeminal neuralgia due to its potential sodium channel blocking action. Lamotrigine, new anticonvulsant has been tried as add-on treatment with carbamazepine in the treatment of trigeminal neuralgia [7]. Gabapentin, a novel anticonvulsant, the exact mechanism as either an anticonvulsant or an analgesic is unknown but proposed that it block the sub type of calcium channel on the neurons and thus reduces the pain. Venlafaxine hydrochloride, structurally novel antidepressant inhibits neuronal serotonin and norepinephrine re-uptake.
Capsaicin
Capsaicin derived from the chili pepper topically has been found to be beneficial in peripheral neuropathy. Depletion of substance P in the distal nerve endings is the proposed mechanism for its use in neuropathy [8].
Autonomic drugs
Autonomic drugs which include the alpha-2 agonists (Clonidine) and alpha-1 antagonists (prazosin, terazosin). Both are proposed to produce analgesia by actions in the periphery, supraspinal CNS, and in the spinal cord.
NMDA-Receptor antagonists
Role of ionotropic glutamate receptors are well established in the hyperexcitability in peripheral neuropathy which eventually lead to allodynia and hyperalgesia. Drugs capable of modulating the NMDA receptor activity have been studied to alleviate neuropathic pain. Several NMDA receptor channel antagonists, including dextromethorphan, amantadine, memantine, and ketamine have been reported to relieve pain in various neuropathic pain states including phantom limb pain, central neuropathic pain, post herpetic neuralgia, and peripheral neuropathic pain [9]. Pharmacological inhibition of enzyme glutamate carboxypeptidase (hydrolyses N-acetylaspartylglutamate to produce glutamate) leading to decreased glutamate is associated with neuroprotective effects animal models of cisplatin, paclitaxel and bortezomib-induced peripheral neuropathy [10].
Preventive treatments
The preventative treatment available for neuropathy must reduce the incidence or severity. These drugs not only reduce the neurotoxic effect of the chemotherapeutic agent, but also must maintain the anticancer effect. The agent includes drugs, vitamins, minerals, herbal remedies.
Vitamin E: Vitamin E has been investigated for prevention of platinum drugs induced neurotoxicity. Cisplatin causes accumulation of platinum adducts in dorsal root of ganglia, and vitamin E may reduce that neurotoxicity via its antioxidant property. Some studies have shown that this antioxidant may protect nerves from the damage caused by cisplatin and paclitaxel and also protects against the microtubule dysfunction that caused by platinum drugs [11].
Amifostine: Amifostine is an organic thiophosphate and it has been studied primarily in cisplatin induced neuropathic pain that is thought to exert its neuroprotective function as a free radical scavenger. It is also effective as neuroprotectant in cisplatin and paclitaxel induced neuropathic pain [12].
Glutathione: Glutathione is primarily used in Cisplatin induced neuropathic pain (CIPN) [13]. Glutathione also affects the kidneys and may increase the elimination of cisplatin; this may contribute to its neuroprotective effect, but it may also diminish its antitumor activity. The proposed mechanism of glutathione interferes with the accumulation of p53 protein, which is activated by cisplatin [14].
Glutamine: Glutamine, endogenously present non-essential amino acid gets converted to essential amino acid in severe stress condition. It plays a vital role in the synthesis of glutathione in the body [15]. Glutamine has been studied for its protective role in CIPN. Vahdat et al. [16] proposed glutamine to protect against oxidative injury and regulate the nerve growth factor.
Acetyl L-carnitine (ALC): Acetyl L-carnitine may modulate NGF expression; it may also promote regeneration following nerve injury [17]. ALC may block abnormal A-fiber and C-fiber nociceptor firing [18].
Herbal Treatment of Neuropathy
In view of prominent adverse effects of modern medicine, drugs from natural sources offer safe therapeutic option in the treatment of neuropathy. Range of plants and phytoconstituents extensively studied for the management of neuropathy in rats (Table 1). Several active phytoconstituents like caffeic acid, phenethyl ester [19]; flavonoids like bioflavone, polyphenols [20] with reputable antioxidant and anti-inflammatory activity have been evaluated in the treatment of neuropathic pain. Isolated bioactive moieties from medicinal plant are documented as promising free radical scavengers playing crucial role in amelioration of neuropathy in animals.
| S No |
Plants and phytoconstituents |
References |
| 01 |
Ocimum sanctum |
[21] |
| 02 |
Gingko biloba |
[22,23] |
| 03 |
Cannabis sativa |
[24,25] |
| 04 |
Salvia officinalis |
[26] |
| 05 |
Matricaria chamomilla |
[27] |
| 06 |
Vernonia cinerea |
[28] |
| 07 |
Ghrelin |
[29] |
| 08 |
α-lipoic acid |
[30] |
| 09 |
Glutamate carbopeptidase |
[10] |
| 10 |
Caffeic acid phenethyl ester |
[19] |
| 11 |
Bioflavone, polyphenols |
[20] |
Table 1: Plants and phytoconstituents reported in neuropathic pain.
Animal Models in Neuropathic Pain
Central pain models
Weight-drop model (Allen technique): It is the most widely used model for the induction for spinal cord injury (SCI). SCI can be induced by dropping a fixed weight on the surgically exposed spinal dorsal surface at the lower thoracic-lumbar level [31-33]. SCI results in severe paraplegia and increased complete segmental necrosis [34,35].
Excitotoxic spinal cord injury (ESCI): Intraspinal injection of quisqualic acid (QUIS), AMPA agonist can turn out long lasting spontaneous pain, mechanical allodynia and thermal hyperalgesia and neuronal loss in specific regions of the spinal gray matter in rat [36,37].
Peripheral nerve injury models
Chronic constriction injury model (CCI or Bennett model): CCI is the well established and universally accepted animal model for the induction of neuropathy. In CCI, after thiopental sodium (35 mg/kg i.p.) anesthesia, skin of the lateral surface of the left thigh incised and a cut directly through the biceps femoris muscles to expose the sciatic nerve given. Ischemia can be induced by placing four ligatures (silk 4–0) around the nerve proximal part of the trifurcation at a distance of 1 mm between each ligature. Nociceptive thresholds be measured before and after performing surgery on different days, i.e., days 0, 1, 3, 6, 9, 1, 2, 15, 18, and 21 [1].
Partial sciatic nerve ligation model (PSL or Seltzer model): In PSL/PSNL, half of the left sciatic nerve ligated partially at the upper thigh level nylon suture. Three weeks after PSNL, allodynia and hyperalgesia could be evaluated after day 1.
L5/L6 spinal nerve ligation model (SNL): Allodynia and hyperalgesia developed in SNL model in animals after unilateral ligation of L5 and L6 spinal nerves last for at least 4 months [38] and can be evaluated.
Sciatic cryoneurolysis model (SCN): Freezing of the sciatic nerve as an alternative to complete transections or ligation, induces nerve injury in the SCN model [39,40] which leads to touch allodynia. Advantage of this method is that cryoneurolysis-induced nerve injury may be reversible, may be beneficial to study the effect of transient nerve injury and the healing process [41,42].
Peripheral neuropathy induced by diseases
Diabetic neuropathic pain model (DNP): Many diabetic models are available, e.g., insulin deficient BB rats [43] and NOD mice [44,45], insulin resistant ob/ob and db/db mice [46,47], In addition, inflammatory the Mongolian gerbil [48,49], several chemicallyinduced models [50] can be used. The most commonly used model streptozocin-induced diabetic neuropathy model. Streptozocin kills insulin-secreting islet in rats, a single i.p. injection of streptozocin induces long lasting thermal and mechanical hyperalgesia, and cold and thermal allodynia [51,52].
Cancer pain models
Chemotherapy-induced peripheral neuropathy models: Chemotherapy are the mainstay to treat cancer but are linked with chronic damage of peripheral nerves termed as chemotherapy induced neuropathic pain. Amongst the drugs available for the treatment of cancer, platinum drugs, taxanes, Vinca alkaloids, thalidomide and its analogues [2,53] are associated with neuropathy due to direct injury to peripheral nervous system.
Cisplatin induced neuropathic pain: Administration of cisplatin (1, 2 mg/kg i.p) twice a week for 5 weeks [2,23] (1 ml/kg s.c saline solution given to avoid renal hydration) induce neuropathy in rats due to damage of large myelinated Aδ fibers, at the level of sensory nerves located in the dorsal root ganglia [54]. The symptoms of CINP are paresthesias and numbness, loss of tendon reflexes and a decrease thick fiber mediated sensory qualities such as vibration perception, fine touch perception and proprioception leading to difficulties in motor coordination. Further disabling sensory ataxia may, muscle weakness is developed. CIPN continue to deteriorate up to three to four months after cessation of therapy [55].
Paclitaxel induced neuropathic pain: Chemotherapeutic dose of paclitaxel are associated with common side effects i.e., mylosuppression, kidney damage and peripheral neurotoxicity [56-59]. Dysfunction of axons and Schwann cells by low doses of paclitaxel produce pain hypersensitivity including allodynia and hyperalgesia [60,61]. Symptoms include numbness, paresthesias and a burning pain in the hands and feet. Disruption of microtubule structure leading to impairment of axoplasmic transport causes neuropathy. Paclitaxel (0.5, 1, 2 mg/kg i.p) on alternate days for 21 days [2,56] induces neuropathic pain in rats. The neurotoxicity produced by paclitaxel is dose dependant painful sensory neuropathy characterized by symptoms includes hyperalgesia, allodynia to thermal and mechanical stimuli, spontaneous pain, weakness, numbness, tingling, burning in distal extremities [62].
Evaluation of Neuropathy in Animal Models
Heat hyperalgesia
The nociceptive activity assessed in terms of paw withdrawal latency in the Hargreaves apparatus (Figure 1) [63]. The apparatus consists of a rectangular glass surface with Plexiglas walls on four sides. The temperature of the glass plate maintained at 52.5 ± 0.5°C with the help of thermocouples attached to the bottom of the chamber. The rats are allowed to acclimate for the period of 10 m. Thereafter, a radiant heat source, consisting of a high intensity bulb (12 V, 50 W), located 20 mm below the glass floor, and projecting through a small round aperture of 5 mm diameter, directly targeted at the hind paw of the rat. Paw withdrawal latency recorded using digital counter, the time interval between the application of the heat beam and the first overt behavioral sign of nociception as described earlier. The cutoff time set at 15 s. Following the treatment with each agent, the rat was then tested in Hargreaves apparatus and three readings were taken at intervals of 10 m each.
Figure 1: Hargreaves apparatus.
Cold-allodynia
In cold allodynia [64] assessment of neuropathic pain done by immersing paw in cold water maintained temperature at 4 ± 1°C. The paw of rat is submerged gently in water and the time taken by rat to withdraw its paw from cold water recorded [65,66] with a cutoff 20 sec maintained throughout the experiment.
Mechanical hyperalgesia (Randall sellitto)
Mechanical Hyperalgesia assessed in rats by using Randall sellitto (Figure 2) [67] paw pressure instrument (UGO Basile Biological Research apparatus, Italy). Rats allowed to stabilize on device and to test stimulus. The nociceptive threshold measured in grams after applying increasing pressure on the paw. The paw of the rat placed under the tip and progressive pressure applied until rat vocalized. The paw withdrawal threshold measured with a maximum cutoff pressure of 450 g.

Figure 2: Randall selitto.
Tactile mechanical allodynia (Von Frey Hair)
Mechanical allodynia (non-noxious mechanical stimuli) was assessed by Von Frey hair (Figure 3) [68]. Rats placed individually on elevated maze (1 cm2 perforations) in a clear plastic cage and adapted to the testing environment for at least 15 m. Briefly, calibrated nylon filaments (Von Frey Hair) of bending forces (g), to be applied from below the mesh floor to the plantar surface of the left hind paw with sufficient force to cause slight bending against paw and hold for 1 sec. Gradual stimulation applied to five times in an interval of 4-5 s. Withdrawal of the left hind limb robustly or immediately to be considered as a positive response.

Figure 3: Von Frey hair apparatus.
Tactile mechanical hyperalgesia (Pin prick)
In the pin prick method [69], the surface of the injured hind paw touched with the point of the bent 18 gauge needle (at 90° angle to the syringe) at an intensity sufficient to produce a reflex withdrawal response. The paw withdrawal (lifting) duration should be recorded in seconds [53] with cutoff time of 20 sec maintained throughout the experiment.
Motor co-ordination (grip muscle strength)
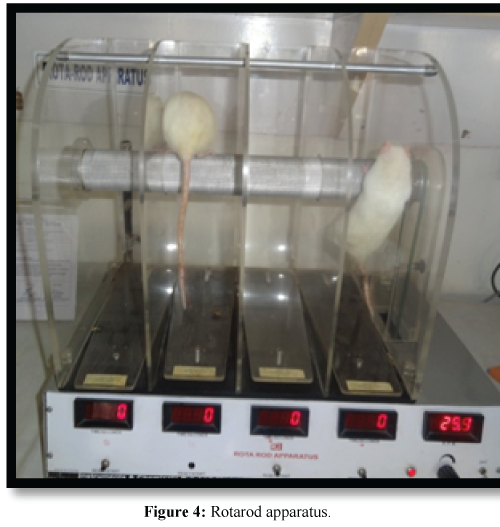
For the measurement of motor co-ordination Rota-rod (Figure 4) [70] can be used. Briefly rats placed for one minute on the rotating rod (20-25 rpm). The time taken for the falling from the roller, during a one minute period to be recorded.
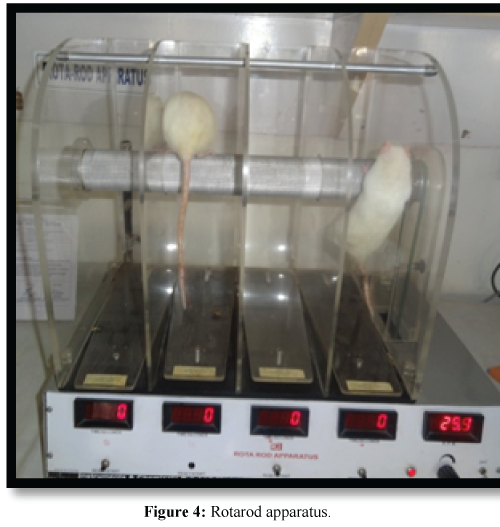
Figure 4: Rotarod apparatus.
Exploratory activity (Locomotor activity)
Photoactometer (Figure 5) test can be used to assess the spontaneous motor activity (exploratory) [53]. Each animal should be observed for a period of 5 min a square closed field arena (30 × 30 × 30 cm) equipped with 6 photocells in outer wall. Interruption of photocell beam (locomotor exploratory action) recorded by means of digital counter.

Figure 5: Actophotometer.
Conclusion
In spite of the significant advancements in neuropathic pain during recent decades, clinical management of patients with this disease remains challenging and the satisfaction of the patients with neuropathic pain is still disappointing. In order to provide better pain control for patients, we must focus on the mechanisms underlying the symptoms of neuropathic pain and as per the necessity of the patient, treatment should be initiated. Mechanism based pharmacotherapy of neuropathic pain would be beneficial to improve the quality of life of patients with neuropathic pain and will improve the approach towards the management of neuropathic pain in patients.
9488
References
- Bennette PN, Brown MJ (2003) Clinical pharmacology. 9th edn. Churchill Living Stone, pp: 319-322.
- Golden JP, Johnson EM (2004) Models of chemotherapy drug-induced peripheral neuropathy. Drug discov today: Dis model 1: 186-191.
- Kandhare AD, Raygude KS, Ghosh P, Ghule AE, Bodhankar SL (2012) Therapeutic role of curcumin in prevention of biochemical and behavioral aberration induced by alcoholic neuropathy in laboratory animals. Neuroscience Letters 511: 18-22.
- Carter GT, Galer BS (2001) Advances in the management of neuropathic pain. Phys Med Rehabil Clin N Am 12: 447-459.
- Hammack JE, Michalak JC, Loprinzi CL, Sloan JA, Novotny PJ, et al. (2002) Phase III evaluation of nortriptyline for alleviation of symptoms of cis-platinum-induced peripheral neuropathy. Pain 98: 195-203.
- Cruccu G (2007) Treatment of painful neuropathy. Curr Opin Neurol 20: 531-535.
- Spina E, Perugi G (2004) Antiepileptic drugs: indications other than epilepsy. Epileptic Disord 6: 57-75.
- Low PA, Opfer-Gehrking TL, Dyck PJ, Litchy WJ, O’Brien PC (1995) Double-blind, placebo-controlled study of the application of capsaicin cream in chronic distal painful polyneuropathy. Pain 62: 163-168.
- Pascual D, Goicoechea C, Burgos E, Martín MI (2010) Antinociceptive effect of three common analgesic drugs on peripheral neuropathy induced by paclitaxel in rats. Pharmacol Biochem Behav 95: 331-337.
- Carozzi VA, Chiorazzi A, Canta A, Lapidus RG, Slusher BS, et al. (2010) Glutamate carboxypeptidase inhibition reduces the severity of chemotherapy-induced peripheral neurotoxicity in rat. Neurotox Res 17: 380-391.
- Pace A, Antonella S, Mauro P, Vittoria M, Umberto P, et al. (2003) Neuroprotective effect of vitamin E supplementation in patients treated with cisplatin chemotherapy. Journal of Clinical Oncology 21: 927-931.
- Moore DH, Donnelly J, McGuire WP, Almadrones L, Cella DF, et al. (2003) Limited Access Trial Using Amifostine for Protection Against Cisplatin-and Three-Hour Paclitaxel-Induced Neurotoxicity: A Phase II Study of the Gynecologic Oncology Group. J Clin Oncol 21: 4207-4213.
- Cascinu S, Cordella L, Del Ferro E, Fronzoni M, Catalano G (1995) Neuroprotective effect of reduced glutathione on cisplatin-based chemotherapy in advanced gastric cancer: a randomized double-blind placebo-controlled trial. J Clin Oncol 13: 26-32.
- Park SA, Choi KS, Bang JH, Huh K, Kim SU (2000) Cisplatin-induced apoptotic cell death in mouse hybrid neurons is blocked by antioxidants through suppression of cisplatin-mediated accumulation of p53 but not of Fas/Fas ligand. J Neurochem 75: 946-953.
- Savarese DM, Savy G, Vahdat L, Wischmeyer PE, Corey B (2003) Prevention of chemotherapy and radiation toxicity with glutamine. Cancer Treat Rev 29: 501-513.
- Vahdat L, Papadopoulos K, Lange D, Leuin S, Kaufman E, et al. (2001) Reduction of paclitaxel-induced peripheral neuropathy with glutamine. Clin Cancer Res 7: 1192-1197.
- Flatters SJ, Xiao WH, Bennett GJ (2006) Acetyl-L-carnitine prevents and reduces paclitaxel-induced painful peripheral neuropathy. Neurosci Lett 397: 219-223.
- Xiao WH, Bennett GJ (2008) Chemotherapy-evoked neuropathic pain: Abnormal spontaneous discharge in A-fiber and C-fiber primary afferent neurons and its suppression by acetyl-L-carnitine. Pain 135: 262-270.
- Ozyurt B, Gulec M, Ozyurt H, Ekici F, Atis O, et al. (2006) The effect of antioxidant caffeic acid phenethyl ester (CAPE) on some enzyme activities in cisplatin-induced neurotoxicity in rats. Eur J Gen Med 3: 167-172.
- Lee JS, Kim YT, Jeon EK, Won HS, Cho YS, et al. (2012) Effect of green tea extracts on oxaliplatin-induced peripheral neuropathy in rats. BMC Complement Altern Med 12: 124.
- Kaur G, Jaggi AS, Singh N (2010) Exploring the potential effect of Ocimum sanctum in vincristine-induced neuropathic pain in rats. J Brachial Plex Peripher Nerve Inj 5: 3.
- Ozturk G, Anlar O, Erdogan E, Kosem M, Ozbek H, et al. (2004) The effect of Ginkgo extract EGb761 in cisplatin-induced peripheral neuropathy in mice. Toxicol Appl Pharmacol 196: 169-175.
- Park HJ, Lee HG, Kim YS, Lee JY, Jeon JP, et al. (2012) Ginkgo biloba Extract Attenuates Hyperalgesia in a Rat Model of Vincristine-Induced Peripheral Neuropathy. Anesth Anal 115: 1228-1233.
- Bridges D, Ahmad K, Rice AS (2001) The synthetic cannabinoid WIN55, 212-2 attenuates hyperalgesia and allodynia in a rat model of neuropathic pain. Br J Pharmacol 133: 586-594.
- Bridges D, Thompson SW, Rice AS (2001) Mechanisms of neuropathic pain. Br J Anaesth 87: 12-26.
- Abad ANA, Nouri MHK, Tavakkoli F (2011) Effect of Salvia officinalis Hydroalcoholic Extract on Vincristine-induced Neuropathy in Mice. Chinese J Nat Med 9: 354-358.
- Abad ANA, Nouri MHK, Gharjanie A, Tavakoli F (2011) Effect of Matricaria chamomilla Hydroalcoholic Extract on Cisplatin-induced Neuropathy in Mice. Chinese J Nat Med 9: 126-131.
- Thiagarajan VRK, Shanmugam P, Krishnan UM, Muthuraman A (2012) Ameliorative effect of Vernonia cinerea in vincristine-induced painful neuropathy in rats. Toxicol Ind health 30: 794-805.
- Garcia JM, Cata JP, Dougherty PM, Smith RG (2008) Ghrelin prevents cisplatin-induced mechanical hyperalgesia and cachexia. Endocrinology 149: 455-460.
- Gedlicka C, Kornek GV, Schmid K, Scheithauer W (2003) Amelioration of docetaxel/cisplatin induced polyneuropathy by alpha-lipoic acid. Ann Oncol 14: 339-340.
- Allen AR (1911) Surgery of experimental lesion of spinal cord equivalent to crush injury of fracture dislocation of spinal column a preliminary report.Journal of the American Medical Association57: 878-880.
- Balentine JD (1978) Pathology of experimental spinal cord trauma. I. The necrotic lesion as a function of vascular injury. Laboratory investigation; a journal of technical methods and pathology 39: 236-253.
- Greenberg J, McKeever PE, Balentine JD (1978) Lysosomal activity in experimental spinal cord trauma: an ultrastructural cytochemical evaluation. Surgical neurol9: 361-364.
- Ford RW (1983) A reproducible spinal cord injury model in the cat. J Neurosurg 59: 268-275.
- Anderson TE (1982) A controlled pneumatic technique for experimental spinal cord contusion. J Neurosci Methods 6: 327-333.
- Yezierski RP, Park SH (1993) The mechanosensitivity of spinal sensory neurons following intraspinal injections of quisqualic acid in the rat. Neurosci Lett 157: 115-119.
- Blumenkopf B Lipman JJ (1991) Studies in autotomy: its pathophysiology and usefulness as a model of chronic pain. Pain 45: 203-209.
- Kim SH, Chung JM (1992) An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat.Pain50: 355-363.
- DeLeo JA, Coombs DW, Willenbring S, Colburn RW, Fromm C, et al. (1994) Characterization of a neuropathic pain model: sciatic cryoneurolysis in the rat. Pain 56: 9-16.
- Wagner R, DeLeo JA, Coombs DW, Willenbring S, Fromm C (1993) Spinal dynorphin immunoreactivity increases bilaterally in a neuropathic pain model. Brain Res 629: 323-326.
- Willenbring S, Beauprie IG, DeLeo JA (1995) Sciatic cryoneurolysis in rats: a model of sympathetically independent pain. Part 1: Effects of sympathectomy. Anesth Analg 81: 544-548.
- Willenbring S, DeLeo JA, Coombs DW (1995) Sciatic cryoneurolysis in rats: a model of sympathetically independent pain. Part 2: Adrenergic pharmacology.Anesthesia & Analgesia81: 549-554.
- Sima AA (1980) Peripheral neuropathy in the spontaneously diabetic BB-Wistar-rat. An ultrastructural study. Acta Neuropathol 51: 223-227.
- Mosseri R, Waner T, Shefi M, Shafrir E, Meyerovitch J (2000) Gluconeogenesis in non-obese diabetic (NOD) mice: in vivo effects of vanadate treatment on hepatic glucose-6-phosphatase and phosphoenolpyruvate carboxykinase.Metabolism49: 321-325.
- Pieper GM, Mizoguchi H, Ohsawa M, Kamei J, Nagase H, et al. (2000) Decreased opioid-induced antinociception but unaltered G-protein activation in the genetic-diabetic NOD mouse.EJP401: 375-379.
- Meyerovitch J, Rothenberg P, Shechter Y, Bonner-Weir S, Kahn CR (1991) Vanadate normalizes hyperglycemia in two mouse models of non-insulin-dependent diabetes mellitus. J Clin Invest 87: 1286-1294.
- Kamei J, Sodeyama M, Ohsawa M, Kimura M, Tanaka SI (1997) Modulation by serum glucose levels on morphine-induced antinociceptive effect in C57BL/KsJ-db/db mice.Life sciences 62: PL1-PL6.
- Vincent AL, Rodrick GE, Sodeman WA Jr (1979) The pathology of the Mongolian Gerbil (Meriones unguiculatus): a review. Lab Anim Sci 29: 645-651.
- Shafrir E, Spielman S, Nachliel I, Khamaisi M, Bar-On H, et al. (2001) Treatment of diabetes with vanadium salts: general overview and amelioration of nutritionally induced diabetes in the Psammomys obesus gerbil. Diabetes/metabolism research and reviews17: 55-66.
- Lee JH, Cox DJ, Mook DG, McCarty RC (1990) Effect of hyperglycemia on pain threshold in alloxan-diabetic rats. Pain 40: 105-107.
- Forman LJ, Estilow S, Lewis M, Vasilenko P (1986) Streptozocin diabetes alters immunoreactive beta-endorphin levels and pain perception after 8 wk in female rats.Diabetes35: 1309-1313.
- Courteix C, Eschalier A, Lavarenne J (1993) Streptozocin-induced diabetic rats: behavioural evidence for a model of chronic pain. Pain 53: 81-88.
- Muthuraman A, Singh N, Jaggi AS (2011) Protective effect of Acorus calamus L. in rat model of vincristine induced painful neuropathy: An evidence of anti-inflammatory and anti-oxidative activity. Food Chem Toxicol 49: 2557-2563.
- Dougherty PM, Cata JP, Cordella JV, Burton A, Weng HR (2004) Taxol-induced sensory disturbance is characterized by preferential impairment of myelinated fiber function in cancer patients. Pain 109: 132-142.
- Hilkens PH, ven den Bent MJ (1997) Chemotherapy-induced peripheral neuropathy. J Peripher Nerv Syst 2: 350-361.
- Flatters SJ, Bennett GJ (2004) Ethosuximide reverses paclitaxel- and vincristine-induced painful peripheral neuropathy. Pain 109: 150-161.
- Authier N, Balayssac D, Marchand F, Ling B, Zangarelli A, et al. (2009) Animal models of chemotherapy-evoked painful peripheral neuropathies. Neurotherapeutics6: 620-629.
- Rowinsky EK, Eisenhauer EA, Chaudhry V, Arbuck SG, Donehower RC (1993) Clinical toxicities encountered with paclitaxel (Taxol). Semin Oncol 20: 1-15.
- Cliffer KD, Siuciak JA, Carson SR, Radley HE, Park JS, et al. (1998) Physiological characterization of taxol-induced large-fiber sensory neuropathy in the rat. Ann Neurol 43: 46-55.
- Flatters SJ, Bennett GJ (2006) Studies of peripheral sensory nerves in paclitaxel-induced painful peripheral neuropathy: evidence for mitochondrial dysfunction. Pain 122: 245-257.
- Polomano RC, Mannes AJ, Clark US, Bennett GJ (2001) A painful peripheral neuropathy in the rat produced by the chemotherapeutic drug, paclitaxel. Pain 94: 293-304.
- Kaley TJ, Deangelis LM (2009) Therapy of chemotherapy-induced peripheral neuropathy. Br J Haematol 145: 3-14.
- Hargreaves K, Dubner R, Brown F, Flores C, Joris J (1988) A new and sensitive method for measuring thermal nociception in cutaneous hyperalgesia. Pain 32: 77-88.
- Yoon C, Wook YY, Sik NH, Ho KS, Mo CJ (1994) Behavioral signs of ongoing pain and cold allodynia in a rat model of neuropathic pain. Pain 59: 369-376.
- Kumar A, Meena S, Kalonia H, Gupta A, Kumar P (2011) Effect of nitric oxide in protective effect of melatonin against chronic constriction sciatic nerve injury induced neuropathic pain in rats. Indian J Exp Biol 49: 664-671.
- Naik AK, Tandan SK, Kumar D, Dudhgaonkar SP (2006) Nitric oxide and its modulators in chronic constriction injury-induced neuropathic pain in rats. Eur J Pharmacol 530: 59-69.
- Randall LO, Selitto JJ (1957) A method for measurement of analgesic activity on inflamed tissue. Arch Int Pharmacodyn Ther 111: 409-419.
- Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL (1994) Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 53: 55-63.
- Erichsen HK, Blackburn-Munro G (2002) Pharmacological characterisation of the spared nerve injury model of neuropathic pain. Pain 98: 151-161.
- Jones BJ, Roberts DJ (1968) The quantiative measurement of motor inco-ordination in naive mice using an acelerating rotarod. J Pharm Pharmacol 20: 302-304.