Keywords
Bariatric surgery infection; Urinary tract infection; Prevention
Introduction
Urinary tract infections (UTI) are common, accounting for 40% of all hospital infections and affecting about 1.7 million patients annually [1]. Previous studies have shown that up to 80% of UTIs are associated with catheters. Also, Intensive Care Unit (ICU) represents 16.9% of all post-discharge complications in Bariatric Surgery (BS) patients [2]. In this sense, previous studies have analyzed that the cases of postoperative UTI occurrence are greater than 50% [2]. Thus, it is imperative to identify the main risk factors for UTI that could be addressed in an attempt to decrease the rate of this postoperative morbidity [2-6]. In this context, the association between the use of urinary catheters and UTI is already well described [2]. Catheters allow direct access to pathogens for the urinary tract [7,8]. A crystalline biofilm has been shown to form in the internal catheter itself [9]. The biofilm is highly resistant to the innate and adaptive immune system, and continues to seed urine with bacteria, which increases antibiotic resistance and the patient's immune response [10]. In this context, E. coli is the primary causative agent in over 90% of outpatients diagnosed with UTI, followed by K. pnuemoniae, P. aeruginosa, P. mirabilis, C. koseri and E. faecalis [2]. Therefore, the present study aimed to analyze the incidence of urinary tract infections in patients undergoing BS, as well as whether any patient received prophylactic antibiotic measurements and whether this measure was effective in preventing infections. It has been hypothesized that revision procedures are significantly associated with increased UTI rate after BS.
Methods
Study design
Following literary search criteria with the use of the MeSH Terms that were cited in the item on "Search strategies", a total of 34 clinical studies that were submitted to the eligibility analysis were checked, and after that, 26 studies were selected, following the rules of systematic review-PRISMA (Transparent reporting of systematic reviews and meta-analyzes-https://www.prismastatement.org/).
Search strategy and information sources
The search strategy was performed in PubMed, Embase, Ovid and Cochrane Library, Web of Science, ScienceDirect Journals (Elsevier), Scopus (Elsevier), OneFile (Gale) followed the following steps: search for MeSH Terms: Bariatric surgery. Infection. Urinary tract infection. Prevention - use of boolean "and" between mesh terms and "or" among historical findings.
Risk of bias
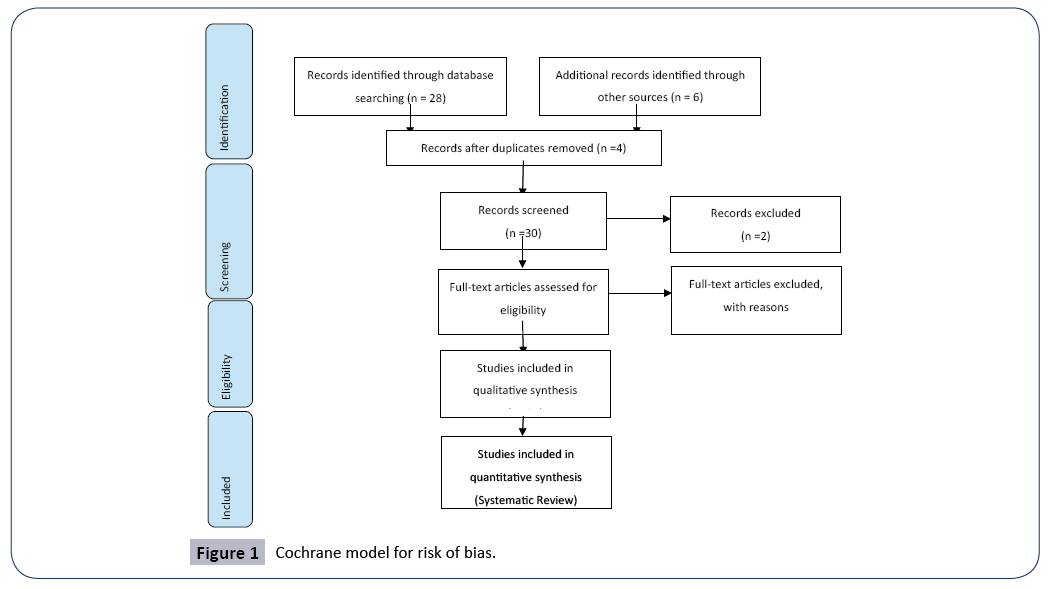
According to the Cochrane model for risk of bias in the present study, the overall assessment resulted in 5 studies with high bias risk and 3 studies with uncertain risk. In addition, there was an absence of funding source in 2 studies and four studies did not disclose the information on the declaration of conflict of interest (Figure 1).
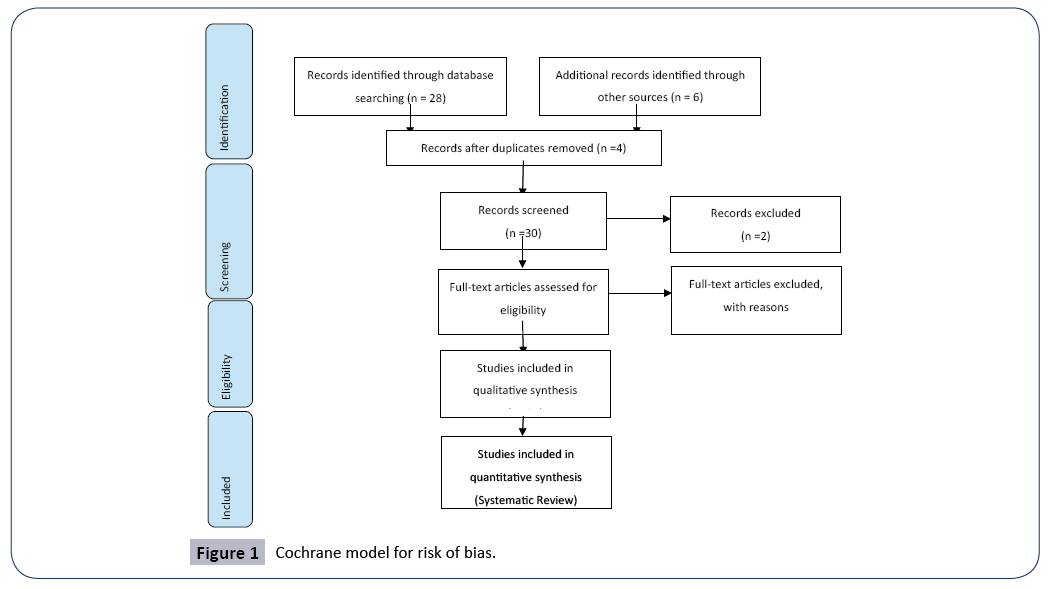
Figure 1: Cochrane model for risk of bias.
Literature Review
A recent analysis revealed that over 90% of the catheterized patients with 100,000 CFU/mL of bacteria had the UTI as their main site of infection, and was asymptomatic [11-13]. Additionally, urinary catheter patients in a site older than 2 days have been shown to be twice as likely to develop the UTI as compared to patients with catheterization of 2 days or less [14]. In addition, a study showed that it is important to design a workflow in which patients are eliminated immediately before going to the BS room, placing urinary catheters only in patients with an expected duration greater than 4 h [14-17]. In addition to urinary catheter use, UTI risk factors identified in previous studies include age, operative time, longer hospital stay and even BMI [18]. There is also evidence that administration of clindamycin as prophylaxis was associated with a significantly increased rate of UTI [19]. In addition, cefazolin covers many gram-positive and some gram-negative bacteria, while clindamycin mainly covers gram-positive bacteria [20]. Because E. coli is a gram-negative bacterium and is the most common cause of urinary tract infections, clindamycin monotherapy can leave patients susceptible to gram-negative organisms [21]. Therefore, American and European guidelines recommend cefazolin prophylaxis [2]. In this context, a study with 1,596 patients included presented a descriptive analysis of the results in relation to obese patients undergoing BS, in terms of infection control. Thus, a care package was designed to control surgical site infection (SSI) rates in patients undergoing BS. The package included smoking cessation, 4% chlorhexidine bath two hours before surgery, cefazolin (2 g) in anesthetic induction associated with continuous infusion of the same drug at a dose of 1 g for a period of two hours, appropriate trichotomy, control glycemic supplemental oxygen, normothermia, intraspinal morphine for pain relief and sterile dressing removal 48 hours after surgery. All patients were followed for 30 days. As a result, 334 (20.9%) underwent open surgery and 1,262 (79.1%) underwent laparoscopic surgery. SSI rates were 0.5% in the group undergoing laparoscopic surgery and 3% in the group undergoing open surgery. The overall incidence of SSI was 1%. Intra-abdominal, respiratory and urinary tract infections occurred in 0.9%, 1.1% and 1.5% of the sample, respectively. Also, higher BMI was associated with a higher incidence of SSI (p=0.001). Among patients with diabetes, 2.2% developed SSI, while the infection rate among non-diabetics was only 0.6%. Therefore, the care package structured by basic evidence-based strategies was able to maintain low SSI rates after BS [1]. In addition, a retrospective study of 694 patients (82.7% female) examined whether preoperative factors and perioperative processes contribute to an increased risk of UTI. The standard protocol was cefazolin antibiotic prophylaxis. Patients with penicillin allergy received clindamycin. Urinary catheters were placed selectively. A univariate and multivariate analysis was performed to determine risk factors for patients who developed an UTI within 30 days postoperatively. As a result, UTI were more common in women (4.9 vs. 1.7%, p=0.12). In the univariate analysis, age, operative time, length of stay, urinary catheter placement, clindamycin prophylaxis, and revision surgery were significantly correlated with UTI. A multivariate logistic regression The model revealed that the risk of UTI increased 5.38 times [95% confidence interval (CI) 2.41-12.05]] with the use of clindamycin, 6.37 times [95% CI 2 .22-18.18] with revision surgery and 1.25 times [95% CI 1.05- 1.49] every 5 years gained in age. Therefore, advanced age, clindamycin prophylaxis, and revision procedures are significantly associated with an increased UTI rate after BS. Several identified variables are modifiable risk factors and targets for a quality improvement initiative to decrease the UTI rate in patients with BS [22]. Another retrospective cohort study with 156,517 patients determined the impact of BS on perioperative complications of posterior lumbar fusion. Patients undergoing posterior lumbar fusion surgery in the state inpatient databases of New York, Florida, North Carolina, Nebraska, Utah, and California comprised the patient sample. Thirty-day medical complications, surgical complications (nerve injury, infection, revision), death, readmission, and length of hospital stay were the results of the study. Patients were analyzed using the codes of the International Classification of Diseases, Ninth Revision. Patients were categorized into three groups: Group 1: history of BS and obesity, Group 2: severe obesity, body mass index (BMI)>40 (severe obesity) and Group 3: normal weight, BMI <25. Multivariate logistic and linear regressions were performed to compare complications and hospitalization, respectively, between BS and groups with severe obesity and groups with BS and non-obese while controlling for confounders. There were 590 patients with BS, 5,791 severely obese and 150,136 nonobese. Comparing BS with severe obesity, BS had significantly lower rates of respiratory failure (odds ratio [OR] 0.59, p=0.019), urinary tract infection (OR 0.64, p=0.031), acute renal failure (OR 0.39, p=0.007), general medical complications (OR 0.59, p<0.001) and infection (OR 0.65, p=0.025). Comparing BS with nonobese, there were no significant differences in medical complications; However, BS had significantly higher rates of infection (OR 2.70, p<0.001), reoperation (OR 2.05, p=0.045) and readmission (OR 1.89, p<0.001). Therefore, BS before elective posterior lumbar fusion reduces the risk of medical complications and infection. However, these patients still have an increased risk of infection, revision surgery, and readmission compared with patients with normal BMI. Surgeons may consider referral to BS for severely obese patients before undergoing spinal surgery [23]. In addition, a study of 19,616 patients compared early patient morbidity and mortality after BS in cases with and without resident involvement, using the American College of Surgeons National Surgical Quality Improvement Program database. These patients were divided into three groups based on the resident's involvement in his surgery. The effect of resident involvement and postgraduate level on 30-day morbidity and mortality was investigated using composite results, including cardiac events (acute myocardial infarction or cardiac arrest requiring cardiopulmonary resuscitation), pulmonary events (pneumonia, prolonged intubation or reintubation/unplanned), wound (superficial surgical site infection, deep surgical site infection, space-organ infection or dehiscence), septic events (sepsis and septic shock), coagulation events (pulmonary embolism and deep vein thrombosis) and renal events (urinary tract infection and kidney injury requiring dialysis). Length of stay, unplanned return to the operating room and 30-day mortality were also investigated. About 8960 (45.7%) procedures were performed with resident involvement, with 5406 (36.7%) of these cases involving senior residents. Operations involving a senior resident were more likely to have postoperative cardiac events (p<0.006), pulmonary events (p=0.03), wound events (p=0.01), septic events (p<0.002), renal events (p ≤ 0.01), prolonged operative time (p<0.0001) and prolonged length of stay (p<0.0001) than those involving no junior or resident level residents. Therefore, although BS involving senior-level residents has statistically more significant morbidity outcomes, these morbidity outcomes are more related to perioperative care than to intraoperative resident involvement. This suggests that more emphasis on progressive perioperative responsibility may be required to match operational supervision [24]. In this sense, although emerging data show that obesity is a risk factor for infectious diseases, no study has investigated the relationship of BS with the risk of infectious diseases in obese adults. Thus, a self-controlled case series analysis was performed using data from the State Emergency Department Database and the State Internal Patient Database from 3 US states (California, Florida, and Nebraska) from 2005 to 2011. We included obese adults undergoing BS as a weight reduction instrument. Primary outcomes were visited the emergency department (ED) or hospitalization for skin and soft tissue infection (STI), respiratory infection, intra-abdominal infection or UTI.
Discussion
Among 56277 obese adults who underwent BS compared to preoperative months 13-24 as reference period, the risk of hospital visit or hospitalization from 0 to 12 months postoperatively decreased significantly for STI (OR 0.85 [95% CI, 0.76-0.95]) and respiratory infection (OR, 0.82 [95% CI, 0.75-0.90]) and remained significantly low in the postoperative period of 13 at 24 months (OR, 0.77 [95% CI, 0.68-0.86] and 0.75 [95% CI, 0.68-0.82], respectively). On the other hand, the risk increased significantly in the postoperative period from 0 to 12 months for intra abdominal infection (OR, 2.09 [95% CI, 1.78-2.46]) and UTI (OR, 1, 93 [95% CI, 1.74-2.15)]) and remained high in the postoperative period of 13 to 24 months (OR, 1.29 [95% CI, 1.09-1.54] and 1, 31 [95% CI, 1.17-1.47], respectively). Therefore, a divergent risk pattern was found in the risk of 4 common infectious diseases after BS. The risk of STI and respiratory infection decreased after BS, while the risk of intra-abdominal infection and UTI increased [25]. One study determined the rate of SSI, UTI and venous thromboembolism (VTE) in BS patients. In addition, the association of these infections with patient factors and their effects on postoperative outcomes was investigated. Patients over 18 years with body mass index (BMI) ≥ 35 undergoing BS were identified using the American College of Surgeons National Surgical Quality Improvement Program database (2005-2012). Patients were grouped into two categories: patients with infection versus no indication and baseline characteristics and outcomes, including 30-day mortality, reoperation, and the average length of hospital stay. 98,553 patients were identified, 2,809 (2.9%) developed at least one type of infection. SSI was the most common (1.8%), followed by UTI (0.7%) and VTE (0.4%). The rate of these infections decreased significantly from 4.6% in 2005-2006 to 2.5% in 2012 (p<0.001). Laparoscopic gastric banding was associated with lower infection rates (1.3%) and open gastric circulation with the highest (8.0%). Patients with infections had significantly higher rates of hospital mortality (0.8 vs. 0.1%, p<0.001) and LOS (3.9 vs. 2.1 days, p<0.001). The presence of a resident surgeon from 7 to 11 years after graduation was associated with significantly increased chances of infection (1.86, 1.50-2.31, p<0.001). Therefore, there was a strong correlation between the three types of infections after BS [26].
Conclusion
Clindamycin monotherapy may leave patients susceptible to gram-negative organisms. Therefore, American and European guidelines recommend cefazolin prophylaxis. The care package structured by basic evidence-based strategies has been able to maintain low rates of urinary tract infections following bariatric surgery. In addition, bariatric surgery before posterior lumbar fusion reduces the risk of medical complications and infection. It was also found that the risk of STI and respiratory infection decreased after bariatric surgery, while the risk of intraabdominal infection and UTI increased.
25256
References
- Helmen ZM, Helm MC, Helm JH, Nielsen A, Kindel T, et al. (2018). Predictors of Postoperative Urinary Tract Infection After Bariatric Surgery. Obes Surg 28:1950-1954. doi: 10.1007/s11695-017-3095-6.
- Klevens RM, Edwards JR, Richards CL (2002). Estimating health care-associated infections and deaths in U.S. hospitals, Public Health Rep 122:160–6. https://doi.org/10.1177/ 003335490712200205.
- Saint S (2008). Clinical and economic consequences of nosocomial catheter-related bacteruria. Am J Infect Control 28:68–75. https://doi.org/10.1016/S0196-6553(00)90015-4.
- Weber DJ, Sickbert-Bennett EE, Gould CV (2011). Incidence of catheter-associated and non-catheter-associated urinary tract infections in a healthcare system. Infect Control Hosp Epidemiol 32:822–823. https://doi.org/10.1086/661107.
- Chen SY, Stem M, Schweitzer MA (2015). Assessment of postdischarge complications after bariatric surgery: a National Surgical Quality Improvement Program analysis. Surgery 158:777–86. https://doi.org/10.1016/j.surg.2015.04.028.
- Foxman B (2014). Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin N Am 28:1–13. https://doi.org/10.1016/j.idc.2013.09.003.
- Saint S, Chenoweth CE (2003). Biofilms and catheter-associated urinary tract infections. Infect Dis Clin N Am 17:411-432. https:// doi.org/10.1016/S0891-5520(03)00011-4.
- Trautner BW, Hull RA, Darouiche RO (2005). Prevention of catheterassociated urinary tract infection. Curr Opin Infect Dis 18:37–41. https://doi.org/10.1097/00001432-200502000- 00007.
- Jacobsen SM, Stickler DJ, Mobley HLT (2008). Complication catheter-associated urinary tract infections due to Escherichia coli and Proteus mirabilis. Clin Microbiol Rev 21:26–59. https://doi.org/10.1128/CMR.00019-07.
- Tambyah PA, Maki DG (2000). Catheter-associated urinary tract infection is rarely symptomatic: a prospective study of 1497 catheterized patients. Arch Intern Med 160:678–682.
- Wald HL, Ma A, Bratzler DW (2008). Indwelling urinary catheter use in the postoperative period: analysis of the national surgical infection prevention project data. Arch Surg 142:551–557.
- Alvarez AP, Demzik AL, Alvi HM, (2016). Risk factors for postoperative urinary tract infections in patients undergoing total joint arthroplasty. Adv Orthop 1:5. https://doi.org/10.1155/2016/7268985.
- Mitchell BG, Ferguson JK, Anderson M (2016). Length of stay and mortality associated with healthcare-associated urinary tract infections: a multi-state model. J Hosp Infect 93:92–99. https:// doi.org/10.1016/j.jhin.2016.01.012.
- Semins MJ, Shore AD, Makary MA, et al. The impact of obesity on urinary tract infection risk. Urology. 2012;79(2):266–9. https://doi. org/10.1016/j.urology.2011.09.040.
- Bratzler DW, Dellinger EP, Olsen KM (2013). Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health-Syst Pharm 70:195–283. https://doi.org/10.2146/ajhp120568.
- Smith BP, Fox N, Fakhro A (2012). BSCIP^ ping antibiotic prophylaxis guidelines in trauma. J Trauma Acute Care Surg 73: 452–456. https://doi.org/10.1097/TA.0b013e31825ff670.
- Campagna JD, Bond MC, Schabelman E (2012). The use of cephalosporins in penicillin-allergic patients: a literature review. J Emerg Med 42:612–20. https://doi.org/10.1016/j.jemermed. 2011.05.035.
- Bernstein IL, Gruchalla RS, Lee RE (1999). Disease management of drug hypersensitivity: a practice parameter. Ann Allergy Asthma Immunol 83:665–700.
- Sogn DD, Evens R, Shepherd GM (1992). Results of the National Institute of Allergy and Infectious Diseases collaborative clinical trial to test the predictive value of skin testing with major and minor penicillin derivatives in hospitalized patients. Arch Intern Med 152:1025–1032. https://doi.org/10.1001/archinte.1992. 00400170105020.
- Wall GC, Peters L, Leaders C (2004). Pharmacist-managed service providing penicillin allergy skin tests. Am J Health Syst Pharm 61:1271–5.
- Elm EV, Altman DG, Egger M (2007). For the STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. PLoS Med 4:296. https://dx.doi.org/10.1371/journal.pmed.0040296.
- Ferraz ÁAB, Vasconcelos CFM, Santa-Cruz F, Aquino MAR, Buenos-Aires VGSiqueira LT (2019). Surgical site infection in bariatric surgery: results of a care bundle. Rev Col Bras Cir 46:e2252. doi: 10.1590/0100-6991e-20192252.
- Jain D, Berven SH, Carter J, Zhang AL, Deviren V (2018). Bariatric surgery before elective posterior lumbar fusion is associated with reduced medical complications and infection. Spine J 18:1526-1532. doi: 10.1016/j.spinee.2018.01.023.
- Haskins IN, Kudsi J, Hayes K, Amdur RL, Lin PP (2018).The effect of resident involvement on bariatric surgical outcomes: an ACS-NSQIP analysis. J Surg Res 223:224-229. doi: 10.1016/j.jss.2017.11.038.
- Goto T, Hirayama A, Faridi MK, Camargo CA Jr, Hasegawa K (2017). Association of Bariatric Surgery With Risk of Infectious Diseases: A Self-Controlled Case Series Analysis. Clin Infect Dis 65:1349-1355. doi: 10.1093/cid/cix541.
- Lidor AO, Moran-Atkin E, Stem M, Magnuson TH, Steele KE (2014). Hospital-acquired conditions after bariatric surgery: we can predict, but can we prevent? Surg Endosc 28:3285-3292. doi: 10.1007/s00464-014-3602.