Case Series - (2022) Volume 10, Issue 1
Acute Appendicitis in Pregnancy: Thirty Three Cases
Alaarabiou A*,
Rabbani K,
Louzi A and
Finech B
Department of Visceral Surgery, University hospital Centre Mohammed VI, Marrakech, Morocco
*Correspondence:
Alaarabiou A, Department of Visceral Surgery, University hospital Centre Mohammed VI, Marrakech,
Morocco,
Tel: 21265678904,
Email:
Received: 03-Oct-2019, Manuscript No. IPJUS-19-2667;
Editor assigned: 09-Oct-2019, Pre QC No. IPJUS-19-2667 (PQ);
Reviewed: 23-Oct-2019, QC No. IPJUS-19-2667;
Revised: 28-Jun-2022, Manuscript No. IPJUS-19-2667 (R);
Published:
26-Jul-2022
Abstract
Acute appendicitis is the most common nonobstetric
surgical emergency during pregnancy. Its occurrence during
pregnancy exposes it to additional diagnostic difficulties and
transforms the current pregnancy into a pregnancy at risk.
Our series includes 33 cases of acute appendicitis and
pregnancy. The objective of the study is to describe the
characteristics of acute appendicitis in pregnant women. In
terms of epidemiology most studies find a predominance of
primary patients with acute appendicitis, in our study it was
more the multipares. The age of onset of acute appendicitis
is between 18 and 44 years of age so there is a larger
proportion of onset in the second trimester of
pregnancy. Despite the many possible tables, the most
constant sign of examination at any stage of pregnancy
remains the pain caused at the level of the right iliac fossa
and this despite the migration of the appendix. Biology is
only an additional diagnostic tool that does not alone affirm
or deny the diagnosis. Ultrasound may specify, correct or
support a suspected diagnosis. The scanner is not without
danger, but its high performance may, in case of
questionable clinical presentation, be of valuable help.
During the operation any hypoxia, hypotension,
hypertension, acidosis, hypo or hyperventilation should be
avoided. Coelioscopy adds other risks related to
pneumoperitin. Coelioscopic surgery during pregnancy and
in particular appendicectomy has many advantages over
laparotomy and seems to be safe for more and more
advanced stages of pregnancy. The use of tocolytic agents
must be case-specific, its indications are not consensual and
their effectiveness in prophylactic measurement is not
demonstrated. In our context, there is no place for
coelioscopic surgery for appendectomy during pregnancy
and laparotomy takes its place. Appendicitis and pregnancy
are a high-risk maternal-fetal association whose prognosis
depends on the early diagnosis and therapeutic
management.
Keywords
Appendicitis; Pregnancy; Diagnosis; Treatment
Introduction
Acute appendicitis is the most common nonobstetric surgical
emergency during pregnancy [1]. Its occurrence during
pregnancy exposes it to additional diagnostic difficulties and
transforms the current pregnancy into a pregnancy at risk [2].
The aim of this work was to describe the characteristic of acute
appendicitis in the pregnant woman in term of clinical,
biological, radiological diagnosis, treatment and prognosis [3].
Case Presentation
It is a descriptive retrospective study of 33 cases of pregnant
women operated on for acute appendicitis at any developmental
stage, collected at the visceral surgery department of university
hospital Mohammed VI in Marrakech (Morocco) [4]. Over a
period of 5 years from January 2012 to December 2016 [5].
During the study period, 3751 women received an
appendectomy at the department of visceral surgery [7]. Acute
appendicitis occurred in pregnant women once for 113
appendicites, or 0.8% [8]. The average age of our patients was
24.6 years, with extremes ranging from 18 to 44 years [9]. The
average gesture in our series was 3.2 while the average parity
was 2.3. There were 18 multiparous and 15 primiparas
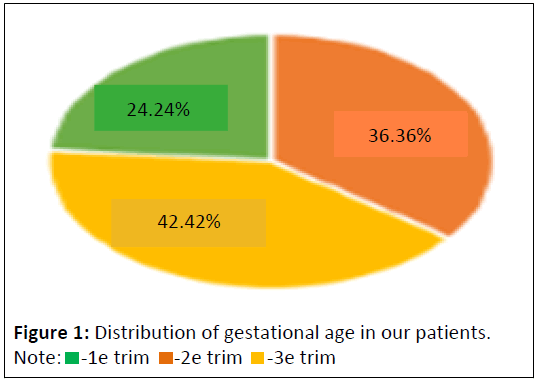
[10]. Gestational age was in the first trimester in 36.36% of cases
(n=12) and in the second trimester in 42.42% (n=14) and in the
third trimester in 24.24% (n=8) (Figure 1) [11].
Results
Abdominal pain was the main symptom and the first
symptom to
appear in all patients [12]. It was mainly located in the right
iliac fossa [13]. Vomiting was an associated symptom in 3 cases,
nausea in 5 cases, fever in 21 cases, only one patient had urinary
burns and another had uterine contractions but no metrorrhagia
or cervical abnormalities [14]. Abdominal defence was present in 3 patients (9.09%), a defence or sensitivity of the right iliac
fossa in 22 cases (66.66%) and a defence or sensitivity of the
right flank in 6 cases (18.18%) and a mass of the right iliac fossa
in 2 cases (6.06%) [15].
Biologically, the leukocyte count was performed in all of our
patients with hyperleukocytosis (>10,000) in 9 of them (27.27%)
[16]. CRP was performed in 23 patients (69.69%), and was
elevated (>5) in all patients [17]. urine cytobacteriological
examination was performed 16 times (48.48%), with no germs
[18]. Abdominal and obstetric ultrasound were performed in all
patients and and was suggestive of acute appendicitis in 19
patients (57.57%) and appendicular abscesses in 11 patients
(33.33%) while the appearance of appendicular peritonitis was
noted in 3 patients (9.09%) [19]. The fetus was alive in all patients and there was no associated pathology (Figure 2) [20].
Figure 2: Abdominal ultrasound results of patients in our series (numbers).
All patients received pain medication combined with
antibiotic therapy. Tocolysis was initiated at induction of
anesthesia, continued in preoperative and postoperative mode
for 24 hours based on progesterone in the first trimester, and
nifedipine in the second and third trimesters.
Our patients were operated on by laparotomy with Mac
Burney incision in 30 cases (90.90%), and a median incision
straddling the umbilicus in 3 cases (9.09%). The appendix was in
the lateral-internal caecal position in 78.8% of the cases and
retro caecal in 21.2% of the cases. Surgery consisted of an
appendectomy in 100% of cases, with peritoneal flushing and
drainage in the case of abscesses or peritonitis in 14 cases
(42.42%).The anatomopathological study was in favour of acute
appendicitis with no signs of malignancy in all patients in our
series, it also revealed appendicular mucocele in 1 patient
(3.03%), which was re-performed for hemaicolectomy after
delivery. The average hospital postoperative stay was 4.7 days.
Maternal mortality was nil. Maternal morbidity was represented
by 4 cases of parietal suppuration (12.12%). One case of
abortion was reported in a patient pregnant and operated for
peritonitis. Fetal death was observed in a pregnant woman in
the 3rd trimester (3.03%).
Discussion
Surgical indications for nonobstetric pathologies concern 0.2%
to 2% of pregnancies. The most frequent etiologies are acute
appendicitis, acute cholecystitis, and surgery of the annexes. For
some, the high level of progesterone during pregnancy would
promote acute appendicitis by decreasing intestinal mobility.Prevalence of acute appendicitis during pregnancy varies
between studies, ranging from 1/1440 to 1/1783 pregnancies.
Most of the studies are now dominated by primary patients
with acute appendicitis. This is due to the average age of onset
of acute appendicitis, which, as in the general population, is
between 24 and 30 years of age, whereas many women are still
only primitive. These studies show a higher proportion of the
second trimester of pregnancy: 48%-51%. This data is affected
by several means: the lower prevalence in the first trimester of
pregnancy is explained by the fact that most studies are carried
out by obstetricians and thus exclude women who have acute
appendicitis at the beginning of pregnancy and who are
managed in digestive surgery. Similarly, acute appendicitis at the
end of pregnancy often results in fetal extraction before
appendectomy. Series that include acute appendicitis during
pregnancy exclude these cases. The results found in our series
coincide with these data for the trimester of occurrence, but we
found a slight predominance among the multiparous.
The clinical diagnosis of acute appendicitis during pregnancy
presents varying difficulties depending on gestational age. In the
first trimester, the semiology of appendicitis is no different from
that observed in the non-pregnant woman. Abdominal pain is
the most common sign. It has been found in all patients in our
series, 96% of the 720 cases studied, with different opinions as
to its location. The frequency of spontaneous localization of pain
in the right iliac fossa varies significantly among authors. Other
more or less frequent locations of pain: Epigastric, periumbilical,
right hypochondrium 32%, 20%. This pain may lead to discussion
of a threat of early abortion or urinary tract infection, hence the
interest of the obstetric examination and urine
cytobacteriological examination. In our study, these two tests
were normal outside of uterine contractions in a patient
(3.03%). The other functional signs of appendicitis (nausea,
vomiting, and constipation) are common during pregnancy at
this gestational age, which takes away any diagnostic interest. In
our study 3 patients had vomiting (9.09%) and 5 patients had
nausea? During the last two trimesters of pregnancy, the
diagnosis of appendicitis becomes more difficult because of a
change in the ratio of the appendix and the uterus. The
appendix is pushed up and out and reaches the costal rim on the
8th. Pain is located in the right flank or hypochondrium. It may
be accompanied by uterine contractions suggesting a threat of
late abortion or premature delivery.
The blood count is difficult to interpret because of the
physiological hyperleucocytosis of pregnancy, while the CRP may
be normal. These two tests are therefore of little interest in the
diagnosis of appendicitis during pregnancy.
Abdominal-pelvic ultrasound confirms diagnosis when it
visualizes an incompressible appendix greater than 7 mm in
diameter, aperitif with a parietal thickness of more than 3 mm
and sometimes a presence of liquid in the appendicular light.
Performed by a trained operator, ultrasound has a sensitivity of
100% and a specificity of 96 % at this gestational age. Its interest
is also to eliminate an associated annexial or obstetrical
pathology, to document the pregnancy by specifying gestational
age and fetal vitality. In our patients, ultrasound was an excellent
contribution, confirming the diagnosis of appendicitis in all cases. We therefore recommend ultrasound because of the
availability of machines, the performance of the examination in
gynecological pathology and the absence of irradiation.
Computed tomography remains the gold standard for imaging in
non-pregnant patients, but to be avoided in pregnant women
for fear of increasing the risk of developing childhood cancers,
and the possibility of interfering with organogenesis, especially
between the 2nd and 15th of gestational age. This has led to the
increased use of magnetic resonance imaging for the diagnosis
of appendicitis during pregnancy, especially when ultrasound
results are inconclusive.
We don’t have experience with coelioscopy in the diagnosis of
acute appendicitis. It allows a diagnostic approach in that it
visualizes the appendix and specifies its location. It avoids white
laparotomy and can diagnose other causes of abdominal pain
such as extra-uterine pregnancy. It is contraindicated beyond the
20th week due to the risk of uterine wound and fetal risk related
to abdominal hyperpressure which would lead to a reduction in
uterine blood flowplacental. However, some authors believe
that coelioscopy is possible in the 2nd trimester and even
beyond by exploiting the free space between the previously
identified uterine floor and the xiphoid appendix.
Complications of acute appendicitis during pregnancy are the
same as outside pregnancy. In the first trimester, all
complications of appendicitis can be seen. On this date, the still
pelvic uterus does not suppress neighboring organs that can
form adhesions around the appendectular focal point and
isolate it from the peritoneal cavity making an appendular
plastron. The development of the appendicular crisis may also
be towards diffuse acute peritonitis. In the last two trimesters,
there is nothing to prevent the spread of appendicular infection.
In fact, uterine contractions hinder the formation of adhesions
and the partitioning of the infection; high steroid levels decrease
inflammatory response and increased pelvic vascularization
facilitates the spread of infection. All of these reasons explain
the more rapid evolution towards peritonitis in the third
trimester.
According to the latest recommendations, antibiotic
prophylaxis is recommended. It reduces the risk of parietal
infection and deep abscess. She has to start preoperative, then
continue per- and postoperative. The duration of administration
and the type of antibiotic still need to be assessed. Regarding
curative antibiotic therapy, most authors agree that it should
only be indicated in the case of complicated acute appendicitis
(perforated, gangrenes, abcess, with or without peritonitis).
They recommend the use of a 3rd or 2nd generation
cephalosporin associated with metronidazole or ampicillin
associated with metronidazole. It shall be maintained and
adapted to the antibiogram taken from the collection of the
peritoneal fluid up to a period greater than 48 hours. For
uncomplicated forms, it can be stopped in immediate
postoperative mode depending on the clinical course.
If the indication of tocolysis is not discussed before a table of
threat of premature delivery, prophylactic, pre and/or
postoperative tocolysis is controversial: Desire, on the one hand
to avoid at all costs a threat of premature delivery and on the
other hand, fear of adverse effects. For many authors, it is indicated only for curative purposes. Some recommend
systematic preoperative prophylaxis. Others recommend
systematic postoperative tocolysis before fetal viability although
its effectiveness is not demonstrated. For many, this is a matter
of personal conviction, given the lack of conclusive studies for
fetal benefit. In our context, prophylactic tocolysis for 48 hours is
systematic. Calcium blockers are used as first-line inhibitors. If
they fail, they go to beta-optics.
All patients were operated on by laparotomy. The technique
for the treatment of acute appendicitis and appendicular
peritonitis doesn’t present any particularity in pregnant women.
The Pathway first depends on the stage of pregnancy, clinical
presentation and whether or not a diagnostic doubt or
associated pathology is present. At the beginning of pregnancy:
The classic right lateral first path with incision at the Mac Burney
point is the most commonly practiced. In the event of a
diagnostic doubt, a paramedic pathway will be possible. In the
last two trimesters: The incision must be higher, located in the
right flank. These high incisions allow resolving the operating
difficulties related to the migrations of the cecum in the 2nd and
3rd trimesters. For some authors, the appendicular region would
be better exposed by a mid-umbilical incision in the 2nd trimester and a Jalaguier incision in the 3rd trimester. However,
in the diffuse appendicular peritonites, the median incision
straddling the umbilicus allows for a quick start and a thorough
exploration of the abdominal cavity as we did in the 3 observed
cases. Coelioscopy reduces uterine manipulation in relation to
the need to explore and in appendicular peritonites, preserves
the abdominal parietal capital and allows a better abdominal
toilet. The appendectomy is performed either intraperitoneally
or transparietal after the appendicitis is removed by a slightly
enlarged suprapubic incision. Coelioscopy, which is
contraindicated in case of scar abdomen due to the risk of
adhesions, would reduce the length of hospitalization and doses
of anaesthetic products without increasing morbidity.
The maternal-fetal prognosis is a function of the severity of
the condition and the delay in treatment. No maternal deaths
were noted in our work as in other series. This is due, to the
early diagnosis and treatment. Fetal death observed in a case of
peritonitis with appendicular perforation diagnosed and treated
4 days after admission. Fetal mortality is more than 35% in
appendicular peritonitis and ranges from 1% to 8% in women
with uncomplicated acute appendicitis. We noted a premature
delivery that was not related to the appendicular condition.
Prematurity and spontaneous delivery is the main fetal risks. The
rate of threat of premature delivery fluctuates between 6.4%
and 22%, the rate of prematurity from 0 to 20% according to the
authors 4.8% .This risk would be higher in the 3rd trimester.
Conclusion
Acute appendicitis in pregnant women is a rare and relatively
difficult diagnosis. In the first trimester, diagnosis is easy,
treatment simple and prognosis generally good. In the last 2
trimesters, diagnostic difficulties are responsible for severe
forms and aggressive surgical treatment. Pelvic ultrasound and
urine cytobacteriological examination should be systematic for
abdominal pain in pregnant women. Diagnostic doubt requires surgical exploration. The primary risk factor for maternal-fetal
mortality is management time, related to the rate of
appendicular perforation. Surgery during pregnancy must be
performed according to a codified protocol. Maternal and fetal
mortality have been reduced due to advances (antibiotic
therapy, surgical techniques, intensive perioperative
monitoring).
Competing Interests
The authors declare no competing interests.
REFERENCES
- To WW, Ngai CS, Ma HK (1995) Pregnancies complicated by acute appendicitis. Australian New Zealand J Surg 65: 799-803.
[Crossref][Google Scholar][Pubmed]
- Mazze RI, Kallen B (1989) Reproductive outcome after anesthesia and operationduring pregnancy: A Registry study of 5405 cases. Am J Obstetr Gynecol 161: 1178-1185.
[Crossref][Google Scholar][Pubmed]
- Mazze RI, Kallen B (1991) Appendectomy during pregnancy: A Swedish registry study of 778 cases. Obstetrics Gynecology 77: 835-840.
[Google Scholar][Pubmed]
- Zahra LF, Badsi S, Benaouicha N, Zraidi N, Lakhdar A, et al. (2022) Appendicular peritonitis during pregnancy: A Case Report. Sch Int J Obstet Gynec 5: 84-88.
[Google Scholar]
- Tamir IL, Bongard FS, Klein SR (1990) Acute appendicitis in the pregnant patient. Ame J Surg 160: 571-576.
[Crossref][Google Scholar][Pubmed]
- Nouira M, Jerbi M, Sahraoui W, Mellouli R, Sakhri J, et al. (1999) Appendicite aigue chez la femme enceinte : A propos de 18 cas. Rev Fr Gynecol Obstet 94: 486-491.
[Google Scholar]
- Tamirel P, Kessler N, Blayac PM, Lesmik A, Gallix B, et al. Imagerie de l’appendicite. Échographie, scanne rouriendu tout. J Radiol 83: 1952-1960. [Crossref][Google Scholar][Pubmed]
- Lim HK, Bae SH, Seo GS. Diagnosis of acute appendicitis in pregnant women: Value of sonography. AJR 1992; 159: 539-542.
[Crossref][Google Scholar][Pubmed]
- Batallan A, Benifla JC, Panel P, Dorin S, Darai E, et al. (1999) Chirurgie laparoscopique au deuxieme trimestre de la grossesse : Indication, technique et retentissement fœtal. A propos de 9 observations et revue de la literature. Ann Chir 53: 285-290.
[Google Scholar]
- Marret H, Laffon H, De Calan L, Bourlier LP, Lansac J, et al. (2000) Urgences chirurgicales au cours de la grossesse. Encycl Med Chir, Gynecologie Obstetrique 5-049-D10 13.
[Google Scholar]
- Barnes SL, Shane MD, Shoemann MB, Bernard AC, Boulanger BR, et al. (2004) Laparoscopic appendectomy after 30 weeks pregnancy: Report of two cases and description of technique. Am Surg 70: 733-736.
[Google Scholar][Pubmed]
- Adloff M, Schloegel M (1989) Appendicitis. Encycl Med Chir. Stomach intestine. 9066 a 10, 10-1989. 10.
- Berthet-Badetti L, Tanti MC, Boimond H (1997) Appendicite aiguë au troisieme trimestre de la grossesse. Rev Fr Gynecol Obstet 92: 205-207.
[Google Scholar]
- Leroy JL (1981) Acute appendicitis during pregnancy-puerperality: Difficulties in diagnosis and treatment. Med Chir Dig 10: 143-147.
- Maisonnette F, Dubayle G, Aubard Y, Baudet JH (1999) Acute appendicitis in the last two trimesters of pregnancy. Rev Fr Gynecol Obstet 94: 66-69.
[Google Scholar]
- Borie F, Philippe C (2011) Appendicite aigue. EMC (Elsevier Masson SAS, Paris) Gastoentérologie 9-066.
[Google Scholar]
- Hunt MG, Martin JN Jr, Martin RW, Meeks GR, Wiser WL, et al. (1989) Perinatal aspects of abdominal surgery for nonobstetric disease. American J Perinatology 6: 412-417.
[Crossref][Google Scholar][Pubmed]
- Hee P, Viktrup L (1999) The diagnosis of appendicitis during pregnancy and maternal and fetal outcome after appendectomy. Int J Gynecol Obstetrics 65: 129-135.
[Crossref][Google Scholar][Pubmed]
Citation: Rabbani K, Alaarabiou A, Louzi A, Finech B (2022) Acute Appendicitis in Pregnancy: Thirty Three Cases. J Univer Surg Vol: 10 No: 1.






 -1e trim
-1e trim  -2e trim
-2e trim  -3e trim
-3e trim