Karan Raheja1,*, Amitabh Goel2, Arun Kumar3, Ashish Prakash4 and Himanshu Sehgal4
1Department of Pediatric Intensivist Care (PICU Head), Yashoda Hospital, Ghaziabad, India
2Department of Neurosurgery, Yashoda Hospital, Ghaziabad, India
3PICU Director, Senior Pediatric Consultant, Yashoda Hospital, Ghaziabad, India
4Department of Pediatrics and Senior Neonatologist, Yashoda Hospital, Ghaziabad, India
*Corresponding Author:
Dr. Karan Raheja
Pediatric Intensivist (PICU Head)
Yashoda Hospital, Ghaziabad, India
Tel: 9899311517
E-mail: aquariankaran@ymail.com
Received Date: May 31, 2017 Accepted Date: June 16, 2017 Published Date: June 20, 2017
Citation: Raheja K, Goel A, Kumar A, et al. Acute Post-traumatic Pediatric Dural Venous Sinus Thrombosis: A Case Report. J Neurol Neurosci. 2017, 8:3.
Keywords
Anti-coagulation; Dural sinus thrombosis; Head trauma; Pediatrics; Superior saggital sinus thrombosis
Introduction
DST mainly involves following- sagittal sinus (70-80%), transverse, sigmoid sinuses (70%), and may extend to the cerebral veins. PDST is a dreadful condition, which cannot be easily diagnosed until we suspect on clinical grounds. The signs and symptoms are extremely varied and nonspecific, ranging in severity from mild headache to progressive neurological deficit, deterioration of consciousness, progressive coma and death related to intracranial hemorrhagic infarction and increased intracranial pressure [1-4]. The estimated annual incidence is 1.5 to 3 cases per million in adults and 6.7% per million in children [4]. Depressed skull fracture, epidural or subdural hematomas can also cause PCST [5-9]. Other than above mentioned causes, post-craniotomy, head and neck infections, cranial tumors, deep venous thrombosis, severe dehydration, inflammatory bowel diseases, connective tissue disorders (CTD), sarcoidosis, nephrotic syndrome, lumbar puncture, parenteral injections, and neonatal asphyxia have been reported as the causes of DST [4,6,10-13]. Recent retrospective studies on safety and outcome of systemic anticoagulation therapy (ACT), showed anticoagulation is safe in pediatric population especially in the absence of initial intracranial hemorrhage, and non-treatment was associated with short term complications like-thrombus propagation, intracranial hypertension, coma and headache [14]. Long-term neurological sequelae include developmental delay, sensorimotor and visual deficits and epilepsy [15-18].
Case Report
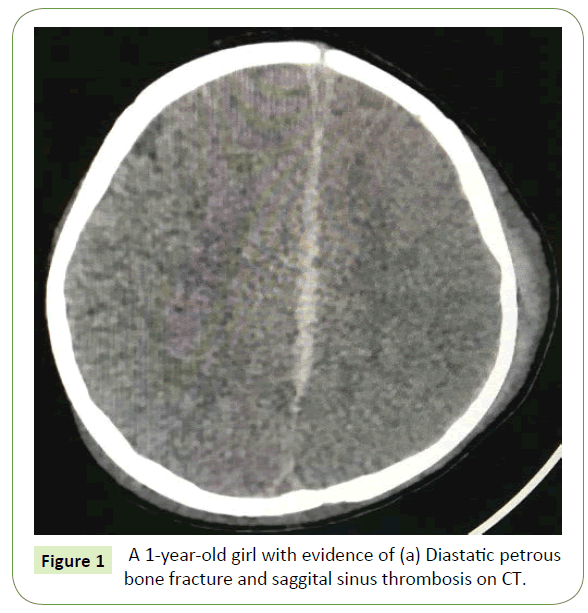
A 1-year-old girl with no past medical or surgical history who was transported to us from some hospital following fall from height (2nd floor), where child was intubated in view of poor GCS and later shifted to Yashoda Hospital, Ghaziabad. Child was shifted to PICU where she was ventilated and ct brain was done which showed Hyperdensity in falx and small subdural haemorrhage in left pareital region. Child was started on anti-edema measures- 3% Nacl along with other supportive management. On day 2 of PICU child was extubated in view of better sensorium. Postextubation child remained haemodynamically stable and was doing well. But on day 3 of PICU child had fall in GCS so was intubated and ventilated. Urgent CT and MRV head was done which showed- Fracture in bilateral pareital bone, left temporal bone with longitudinal fracture of petrous with collection in mastoid and middle ear with thin subdural haemorrhage underlying the fractures and loss of flow void with filling defect in middle part of superior saggital sinus- suggestive of thrombosis. Child was immediately started on Inj Heparin infusion at 10 I.U/ kg/hr with targeting ApTT between 60 to 80. Child's was continued on management for raised ICP in form of antiedema measures. Child's condition gradually improved and child was extubated on day 6 of PICU. Post- extubation child remained haemodynamically stable with GCS- 15/15. Repeat MRV done showed recanalization of saggital sinus. On day 8 of PICU stay patient was shifted tio HDU where physiotherapy and other symptomatic management was continued. Child condition gradually improved as she was able to move her hemiparetic limbs. She was shifted to s/c low molecular weight heparin(LMWH) and was sent home on day-10 of hospital stay with advice to follow up in the OPD weekly till next 6 weeks along with continuation of LMWH therapy.
Initial imaging studies
A 1-year-old girl with evidence of (a) Diastatic petrous bone fracture and (b) saggital sinus thrombosis on CT (Figure 1).
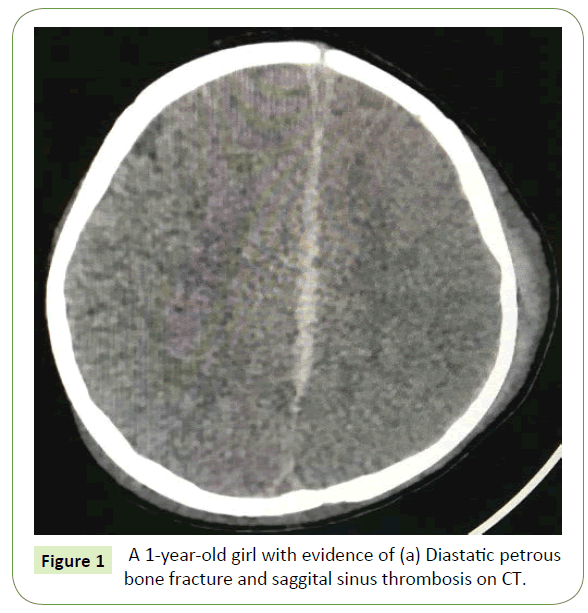
Figure 1: A 1-year-old girl with evidence of (a) Diastatic petrous bone fracture and saggital sinus thrombosis on CT.
Hospital course
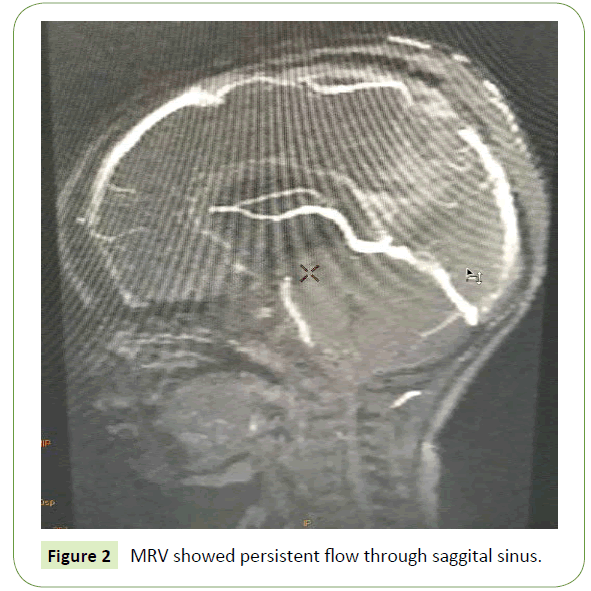
The coagulation profile of patient, Protein S, C and D-Dimers were in the normal limits, so she started on intravenous heparin at 10 I.U/kg/hr and APTT was monitored (Target around-60) along with any changes in neurologic status. Till day 5 of hospital stay patient remained haemodynamically stable and repeat MRV (Figure 2) demonstrated persistent flow of the saggital sinus. As the patient's condition improved so the patient was shifted to LMWH (enoxaparin).
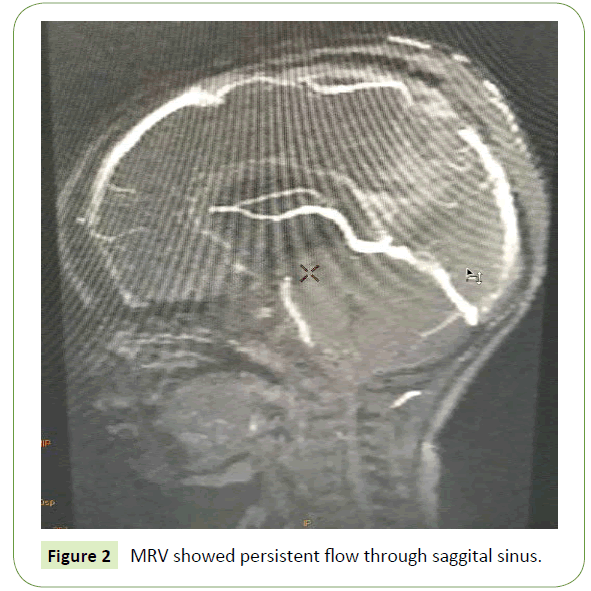
Figure 1: MRV showed persistent flow through saggital sinus.
Discussion
Overall incidence of PDST is 0.67 per 100,000 children per year. Children commonly presents with lethargy, focal neurologic signs, papilledema and headache [19-21]. PDST usually affects a single sinus, the superficial sagittal (47.5%) or transverse sinuses (12%) of cases, respectively; in the same study, two sinuses were involved in 30% of the cases [22]. Many risk factors are associated with PCST, among them, head trauma are very few in number. PDST can also occur without skull fracture but mostly cases involve bone fracture next to that particular thrombosed sinus [23,24]. Age is an important factor to consider PDST if suspected mostly after head trauma. Age should be considered while using diagnositic imagingnfor PDST. CT is commonly used to evaluate for possible intracranial hemorrhage and fractures after head trauma, suspected thrombosis requires further studies to confirm the diagnosis if time permits. CT scan has 84% accuracy to diagnose PDST in children [20] for this reason, MRV is useful tool to rule out PDST in case of suspicion.
Per published DST guidelines [25], in our patient other etiology was rulled out. Many published case reports, [14,26,27] where patients were managed without any intervention, our patient was managed medically with IV heparin and later to subcutaneous LMWH, also our patient had superior saggital sinus thrombosis which has not been reported in such a younger child as PDST and no case reports have used I.V heparin for 5 days. However to decide the usage AC therapy in a head trauma patient with a petrous bone fracture can be dangerous, a recent update in management of pediatric DST which recommend the use of AC therapy even if there is setting of nonsignificant intracranial hemorrhage [25]. In one of case reviewed, after head injury pediatric DST, the patient was managed initially with IV heparin for 1 full day, and later shifted to LMWH [28]. Similarly to that case we started I.V Heparin therapy which was continued for 5 days and later shifted to LMWH. The reversibility and daily handling of heparin therapy in comparison to other anticoagulants makes it a best choice for AC therapy. This treatment option was also easy to administer by the family, and allowed the patient to be treated as an outpatient with weekly coagulation studies. During reevaluation after 2 weeks of enoxaparin child is doing well and has started recovering from hemiparesis too.
A pilot cohort study of 22 pediatric patients of DST used various AC (LMWH, heparin and warfarin) regimens and had no reported deaths or intracranial hemorrhage [29]. One of the prospective study showed that conservative therapy was associated with increase in venous thrombi in comparison to AC therapy [30]. In a multicenter European registry of pediatric DST, AC therapy was used in 250 (65%) patients; 1 patient died after AC therapy, 7 (5%) who were managed conservatively died secondary to edema-induced herniation [22]. These findings make a useful argument to use AC therapy in such cases rather them managing conservatively.
In the literature reviewed prognosis of PDST mostly depends on how the patient presenting symptoms were and child's underlying condition. Coma, seizure and venous infarcts were considered as poor predictor for outcome [20]. ALso it has been reported that without use of ACT in any form, itself is a independent risk factor for recurrent CST [22].
Conclusion
Acute PDST is a rare etiology, as its day to day management is not mentioned clearly. Our case report had post head injury DST in a 1-year-old girl, who was treated safely with AC therapy, and had symptomatic along with radiological improvement within 5 days of therapy. I.V heparin therapy may help reduce mortality, morbidity and hospitalization time in comparison to conservative management. Further study trials are required to fully assess the efficacy and efficiency of this therapy in pediatric population.
19675
References
- Brors D, Schafers M, Schick B, Dazert S, Draf W, et al. (2001) Sigmoid and transverse sinus thrombosis after closed head injury presenting with unilateral hearing loss. Neuroradiology 43: 144-146.
- De Bruijn SF, De Haan RJ, Stam J (2001) Clinical features and prognostic factors of cerebral venous sinus thrombosis in a prospective series of 59 patients for The Cerebral Venous Sinus Thrombosis Study Group. J Neurol Neurosurg Psychiatry 70: 105-108.
- Kuehnen J, Schwartz A, Neff W, Hennerici M (1998) Cranial nerve syndrome in thrombosis of the transverse/sigmoid sinuses. Brain 121: 381–388, 1998
- Stam J (2005) Thrombosis of the cerebral veins and sinuses. N Engl J Med 352: 1791-1798.
- Meltzer H, LoSasso B, Sobo EJ (2000) Depressed occipital skull fracture with associated sagittal sinus occlusion. J Trauma 49: 981.
- Owler BK, Besser M (2005) Extradural hematoma causing venous sinus obstruction and pseudotumor cerebri syndrome. Childs Nerv Syst 21: 262-264.
- Tamimi A, Abu-Elrub M, Shudifat A, Saleh Q, Kharazi K, et al. (2005) Superior sagittal sinus thrombosis associated with raised intracranial pressure in closed head injury with depressed skull fracture. Pediatr Neurosurg 41: 237-240
- Uzan M, Ciplak N, Dashti SG, Bozkus H, Erdincler P, et al. (1998) Depressed skull fracture overlying superior sagittal sinus as a cause of benign intracranial hypertension: Case report. J Neurosurg 88: 598-600.
- Yokota H, Eguchi T, Nobayashi M, Nishioka T, Nishimura F, et al. (2006) Persistent intracranial hypertension caused by superior sagittal sinus stenosis following depressed skull fracture. A Case report and review of the literature. J Neurosurg 104: 849-852.
- Cruz BA, Santos LA, Damasceno RP, Ribeiro LS, Xavier GA Jr, et al. (2001) Dural sinus thrombosis in childhood systemic lupus erythematosus. J Rheumatol 28: 2140-2141.
- Renowden S (2004) Cerebral venous sinus thrombosis. Eur Radiol 14: 215-226.
- Taha JM, Crone KR, Berger TS, Becket WW, Prenger EC (1993) Sigmoid sinus thrombosis after closed head injury in children. Neurosurgery 32: 541-545.
- Umit H, Asil T, Celik Y Tezel A, Dokmeci G, Tuncbilek N, et al. (2005) Cerebral sinus thrombosis in patients with inflammatory bowel disease: a case report. World J Gastroenterol 11: 5404-5407.
- Moharir MD, Shroff M, Stephens D, Pontigon AM, Chan A, et al. (2010) Anticoagulants in pediatric cerebral sinovenous thrombosis: A safety and outcome study. Ann Neurol 67: 590-599.
- Sébire G, Tabarki B, Saunders DE, Leroy I, Liesner R, et al. (2005) Cerebral venous sinus thrombosis in children: Risk factors, presentation, diagnosis and outcome. Brain 128: 477-489.
- De Veber GA, Mac Gregor D, Curtis R, Mayank S (2000) Neurologic outcome in survivors of childhood arterial ischemic stroke and sinovenous thrombosis. J Child Neurol 15: 316-324.
- Golomb MR, De Veber GA, Mac Gregor DL, Domi T, Whyte H, et al. (2003) Independent walking after neonatal arterial ischemic stroke and sinovenous thrombosis. J Child Neurol 18: 530-536.
- Hetherington R, Tuff L, Anderson P, Miles B, Deveber G (2005) Short-term intellectual outcome after arterial ischemic stroke and sinovenous thrombosis in childhood and infancy. J Child Neurol 20: 553-559.
- Carvalho KS, Bodensteiner JB, Connolly PJ, Garg BP (2001) Cerebral venous thrombosis in children. J Child Neurol 16: 574-580.
- De Veber G, Andrew M, Adams C, Bjornson B, Booth F, et al. (2001) Cerebral sinovenous thrombosis in children. N Engl J Med 345: 417-423.
- Kenet G, Kirkham F, Niederstadt T, Heinecke A, Saunders D, et al. (2007) European Thromboses Study Group. Risk factors for recurrent venous thromboembolism in the European collaborative paediatric database on cerebral venous thrombosis: A multicentre cohort study. Lancet Neurol 6: 595-603.
- Huisman TA, Holzmann D, Martin E, Willi UV (2001) Cerebral venous thrombosis in childhood. Eur Radiol 11: 1760–1765.
- Taha JM, Crone KR, Berger TS, Becket WW, Prenger EC (1993) Sigmoid sinus thrombosis after closed head injury in children. Neurosurgery 32: 541-546.
- Saposnik G, Barinagarrementeria F, Brown RD, Bushnell CD, Cucchiara B, et al. (2011) American Heart Association Stroke Council and the Council on Epidemiology and Prevention. Diagnosis and management of cerebral venous thrombosis a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42: 1158-1192.
- Sousa J, O’Brien D, Bartlett R, Vaz J (2004) Sigmoid sinus thrombosis in a child after closed head injury. Br J Neurosurg 18: 187–188.
- Stiefel D, Eich G, Sacher P (2000) Post-traumatic dural sinus thrombosis in children. Eur J Pediatr Surg 10: 41-44.
- Al-Wala Awad, Ratan Bhardwaj (2008) Acute posttraumatic pediatric cerebral venous thrombosis: Case report and review of literature: A multicenter cohort from the United States. J Child Neurol 23: 26-31.
- deVeber G, Chan A, Monagle P, Marzinotto V, Armstrong D, et al. (1998) Anticoagulation therapy in pediatric patients with sinovenous thrombosis: A cohort study. Arch Neurol 55: 1533-1537.
- Moharir MD, Shroff M, Stephens D, Pontigon AM, Chan A, et al. (2010) Anticoagulants in pediatric cerebral sinovenous thrombosis: A safety and outcome study. Ann Neurol 67: 590-599.
- Wasay M, Dai AI, Ansari M, Shaikh Z, Roach ES (2014) Cerebral venous sinus thrombosis in child Surg Neurol Int 5: 53.