Research - (2023) Volume 14, Issue 2
Addictions and psychiatric disorders in patients followed at the Doctor Joseph Guislain Neuropsychiatric Centre in Lubumbashi, series of 112 cases and review of the literature
Ntalaja Kabuayi Philippe MD1,2*,
Célèbre Mualaba MD3*,
Bondish Kambaja Munya MD2,
Grégoire Kamanga MD2,
Joseph Tshitoko MD2,
Dalida Kibokela Ndembe MD2 and
Massar Diagne Phd4
1Doctor Joseph Guislain Neuropsychiatric Centre of Lubumbashi, Democratic Republic of Congo
2Department of Neurology, NeuropsychoPathological Centre of Kinshasa, Democratic Republic of Congo
3Department of Neurosurgery, Fann University Hospital, Dakar, Senegal
4Department of Neurology, Fann University Hospital, Dakar, Senegal
*Correspondence:
Ntalaja Kabuayi Philippe MD, Doctor Joseph Guislain Neuropsychiatric Centre of Lubumbashi,
Democratic Republic of Congo,
Email:
Célèbre Mualaba MD, Department of Neurosurgery, Fann University Hospital, Dakar,
Senegal,
Email:
Received: 22-Feb-2023, Manuscript No. ipjnn-23-13525;
Editor assigned: 02-Mar-2023, Pre QC No. P-13525;
Reviewed: 16-Mar-2023, QC No. Q-13525;
Revised: 22-Mar-2023, Manuscript No. R-13525;
Published:
30-Mar-2023
Abstract
The impact of addictions and their consequences has become a mental health and, beyond that, a public health problem throughout the world and developing countries are no exception. It is even more worrying because it is exacerbated by the increase in poverty, youth unemployment and the attraction of the consumption habits of rich countries. It therefore seemed appropriate to carry out this preliminary study to take stock of the situation in hospitals before extending our analysis to the general population and suggesting ways of dealing with the problem of the interaction between addiction and psychiatric pathology. The results of this study highlight this intertwining of addiction and mental pathology based on recent neurobiological knowledge that classifies addictions as a mental pathology and not as a lifestyle choice or vice. Moreover, the notion of a dual pathology suggests the imperative need for multidisciplinary management of addictions, which are everyone's business, given that their neurobiological and environmental underpinnings are common to many of us, and that the desire and difficulty of abstinence and its maintenance are deeply human.
Keywords
Addiction; Psychoactive substances; Psychiatric disorders
and Withdrawal
Introduction
The term addiction is of Latin etymology, ad-dicere "to
say to". In Roman civilization, slaves had no proper name
and were said to their Pater familias. The term addiction
expresses an absence of independence and freedom, and
therefore slavery. It is therefore the process by which
a behavior that can both produce pleasure and ward off
or alleviate a feeling of internal discomfort is employed
in a way characterized by the repeated impossibility of
controlling this behaviour and its continuation despite the
knowledge of its negative consequences [1].
The term "addiction" is not used as a diagnostic term
in the DSM-5, nor in the ICD- 1016. In many countries,
it is common practice, including among clinicians, to use
the term addiction to describe serious problems related
to repeated compulsive substance use, but the term is
not included in official terminologies due to its uncertain
definition and negative connotation.
Addictive behaviours involve substances (tobacco,
alcohol), behaviours (shopping, sex, food, work) and
objects (internet). Throughout this article we will focus
more on substance-related addictive behaviours while
briefly presenting other causes.
A distinction must be made between:
• What falls under addictive behaviours
• The complications of addictive behaviour (somatic,
psychiatric, social)
• Co-morbidities in cases of harmful use and/or
dependence
Addictive behaviours evolve according to the way they
are consumed, from simple use to abuse to dependence [2].
Use: Consumption of psychoactive substances that
does not lead to somatic complications or harm and is not
a pathological problem
Abuse (DSM) or harmful use (ICD) of psychoactive
substances: Repeated consumption leading to damage
in the somatic, psycho-affective or social domains (either
for the subject himself or herself, or for his or her own
environment or distant environment)
Dependence: The impossibility of abstaining from
consumption (Existence of a tolerance, Existence of a
withdrawal syndrome)
In the general population there is a strong association
between psychiatric disorders and addictive disorders,
mainly for states of DEPENDENCE (mood disorders,
anxiety disorders, post-traumatic disorders, personality
disorders [2].
The existence in the same subject of an addictive
disorder and another psychopathological disorder is
commonly referred to as "Dual Pathology". It is linked to
neurobiological and environmental phenomena a+ssociated
with addictive behaviours with or without substances.
It should be noted that this use is more frequent in
patients with behavioral disorders, either because the use
preceded the disorders, as is the case for most users, or
because the use is a co-morbidity of the psychiatric disorder.
The demand for care and treatment is all the lower as
the number of disorders increases or worsens: the higher
the number of psychiatric disorders and the more severe
the symptoms, the less care is sought. We must also take
into account the association between the risk factor of
deserialization and criminal acts (rape, etc.) or somatic
disorders (HIV).
The consumption of alcohol, tobacco, illicit substances
(cannabis, heroin, cocaine, synthetic products) , as well
as deviant behaviours such as excessive gambling, eating
disorders and compulsive shopping, represent major
mental health problems in particular and public health
problems in general, both in terms of the number of people
they affect and the social, health, environmental and legal
problems they cause.
Approximately 207,400 deaths related to illicit drug
use are estimated to have occurred worldwide in 2014,
more than a third of which are related to overdoses [3].
A study carried out in the French population in
June 2013 showed that alcohol was the substance most
frequently experimented with by students, ahead of tobacco
and cannabis with 91.3%, 65.2% and 42.8% respectively.
Tobacco was used daily by 18.4% of students [4].
Alcohol and tobacco consumption, as well as the
initiation of cannabis at an early age, can cause a lot of
health and social damage in the short and long term. It
is therefore a real mental health problem both for normal
people and for patients with psychiatric conditions.
According to the United Nations Office on Drugs and
Crime (UNODC), it is estimated that one in 20 adults
used at least one drug in 2014. This represents 250 million
people aged 15-64. The scale of the global problem becomes
more apparent when one considers that more than one in
ten drug users are problematic users, suffering from drug
use disorders or addiction [5].
From a neurobiological point of view, studies have
shown that addictive behaviours can have irreversible
consequences on the development of young people's brains, which go through different stages of maturation between
the ages of 15 and 25. This maturation process is weakened
by the use of psychoactive substances which can lead to
brain disorders resulting in psychiatric pathologies [6].
The use of certain psychoactive substances (PAS)
is widespread among adolescents and young adults, in
particular alcohol, tobacco and cannabis, which are among
the most common substances of abuse in many countries
of the world.
The use of psychoactive substances (PAS) has
particularly harmful effects on adolescents and young
adults. It remains high in Europe, particularly in France,
and in Anglo-Saxon countries, but an increasing trend in
developing countries like ours has been noted [6].
In Ghana, cannabis abuse is estimated to be over 13%
among people aged 15-65 years (3.8% worldwide) [7].
Moreover, co-morbidity between addictive disorders
and psychiatric disorders is also more frequent than the
simple co-occurrence of independent disorders would
suggest. The hypothesis of self-medication of psychiatric
symptoms by the use of psychoactive products has been
put forward.
The other hypothesis is that there are common
vulnerability factors between the use of APS and psychiatric
disorders. This concerns schizophrenic patients, but also
those with mood disorders or personality disorders. Multiple
concordant studies find a higher prevalence of smoking in
schizophrenic patients, but anater dependence on nicotine.
Schizophrenic patients evaluated in a Norwegian study
showed a much higher lifetime use of all illicit substances
than the general population. This was also the case for
patients enrolled in the CATIE study, an American study
of the effectiveness of different pharmacological treatments
for schizophrenia. The prevalence of abuse and dependence
on at least one substance among them was 36%. The type
of substance used was mainly alcohol (87%), followed by
cannabis (44%) and cocaine (36%) [3].
This association between the use of APSs and psychiatric
disorders is bidirectional: use predicts the presence of
a psychiatric disorder and conversely, the presence of a
psychiatric pathology increases the risk of a transition to
APS dependence.
The lack of treatment centres equipped with antiaddiction
drugs explains the absence of epidemiological
data linking addictive behaviour and psychiatric disorders
in our environment. Most of the studies carried out often
only analyse the prevalence of the substances consumed
without establishing a link with psychiatric pathology.
Moreover, this implication is twofold, particularly
for our country, DR Congo, where the majority of the
population is young (adolescents and young adults);
moreover, the initiation of the consumption of APS begins
in adolescence, as do most psychiatric disorders, including
schizophrenia, mood disorders, anxiety disorders, etc.,
generally between the ages of 15 and 25. This is why our
country is particularly interested in the coexistence of psychiatric disorders and the use of APS. This correlation
has an enormous direct and indirect cost on the economy
of the families and the national economy; thus, it seems
relevant to us to approach this subject starting from the
determination of the characteristics of the consumption
of psychoactive substances in the patients followed at the
Neuropsychiatric Centre Dr Joseph Guislain.
Our research has raised questions in our
environment, namely
• What is the rate of SPA use among patients in our
study setting?
• What are the motivations for this consumption?
• What are the main pathologies related to the use of
APS in the patients followed up?
The general objective is to characterise the nature of the
link between psychiatric disorders and addictive behaviours
in order to improve screening and treatment.
In order to do this, we have endeavored to determine
the socio-demographic characteristics of the patients
followed and consuming APS; the degree of consumption
or dependence; the motivations for the consumption of
APS in order to understand the links between psychiatric
pathology and consumption in their chronology and their
intricacy, and finally, if possible, to analyse the link between
the consumption of APS and psychiatric pathologies.
Methodology
We conducted a descriptive cross-sectional study at the
Dr. Joseph Guislain Neuropsychiatric Centre (DJNPC)
in Lubumbashi, DRC, over a period from 1 June 2022 to
31 July 2022. This study involved 111 patients who were
hospitalized and followed up at the CNJG for addiction.
Our sampling was stratified simple random. We included
in the study the medical records of patients with a diagnosis
of addiction who were aged 12 years or older.
We collected the data using a pre-designed form,
which contained our study variables. For each patient we
collected:
• Socio-demographic data (age, gender, marital
status, type of housing, education level, occupation)
sources of income, family economic level, legal
problems)
• Data related to addictive behaviours (substance used,
age of onset, mode of use, withdrawal attempts,
symptoms experienced during withdrawal)
• Data related to the dual pathology (psychiatric
diagnosis, age of first episode, family history,
management, evolution)
We collected the data anonymously, in order to preserve
patient confidentiality.
The data were entered and analysed in Excel 2019 and
Epi info 7.2 and the results generated were presented in
tables and + ures using Word 2019.
Results
Socio-demographic data
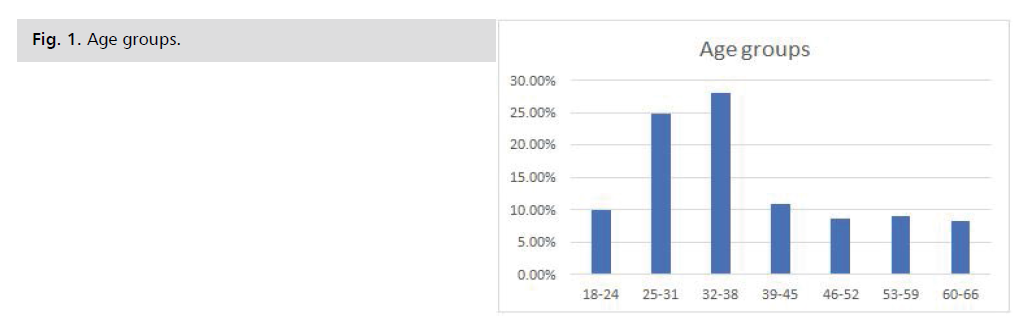
Age: The histogram shows that the most represented
age group was 18 to 45 years old. Median: 32 years; Mode:
35 years; Standard deviation: 11.22 years; Quartile 1: 26
years; Quartile 2: 32 years; Quartile 3: 38.5 years Fig. 1.
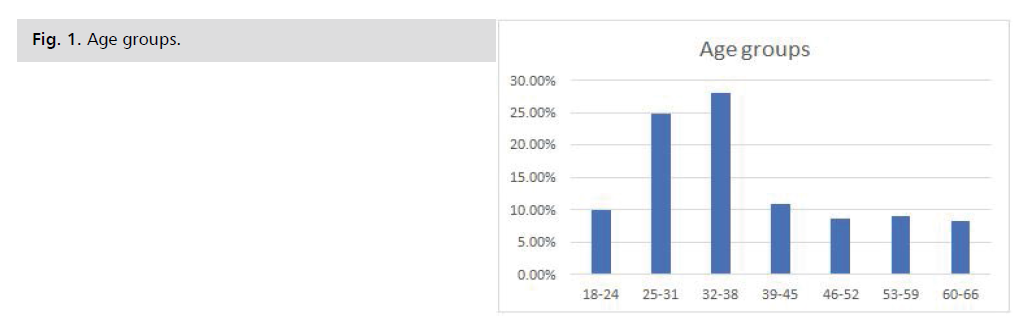
Fig. 1: Age groups.
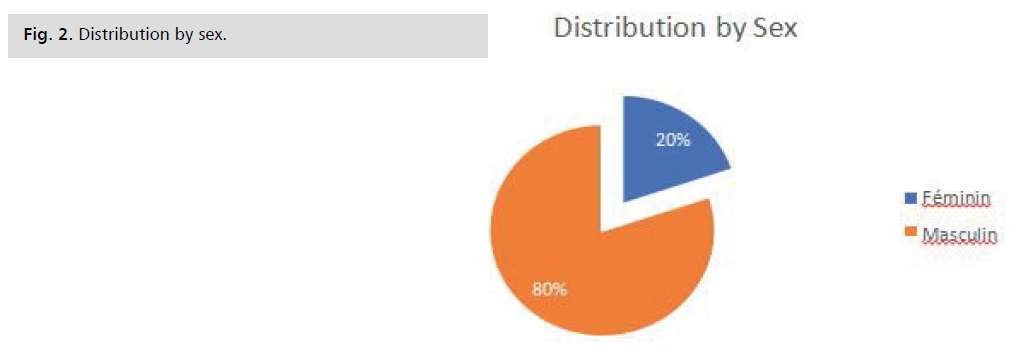
Sex: We can see from this figure that the male sex was
the most represented with 80% of cases and a sex ratio of 4
men to 1 woman Fig. 2.
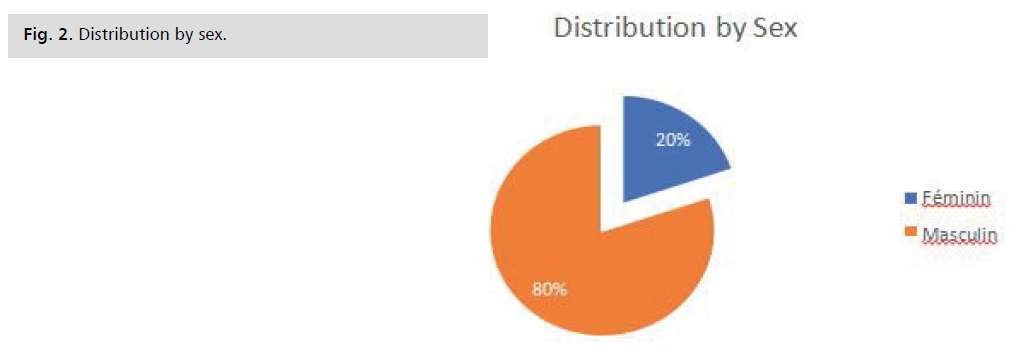
Fig. 2: Distribution by sex.
Marital status: According to this table, Single was the
most represented marital status with 66.67%, followed by
Married with 18.92%; Divorced: 9.01% and Widowed
was the least present with 5.41% Tab. 1.
| Civil Status |
Workforce |
Percentage |
| Single |
74 |
66,67% |
| Married |
21 |
18,92% |
| Divorced |
10 |
9,01% |
| Widower |
6 |
5,41% |
| Grand Total |
111 |
100,00% |
Tab. 1. Marital status.
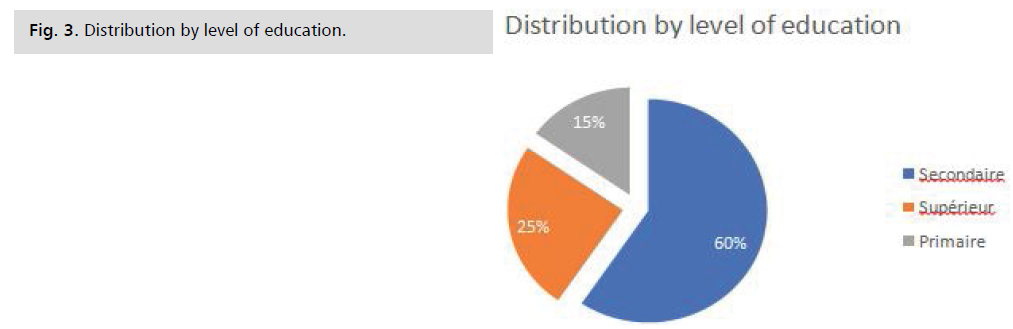
Level of education: This graph illustrates that the
most frequent level of education was Secondary with 60%
followed by Higher 25% and Primary 15% Fig. 3.
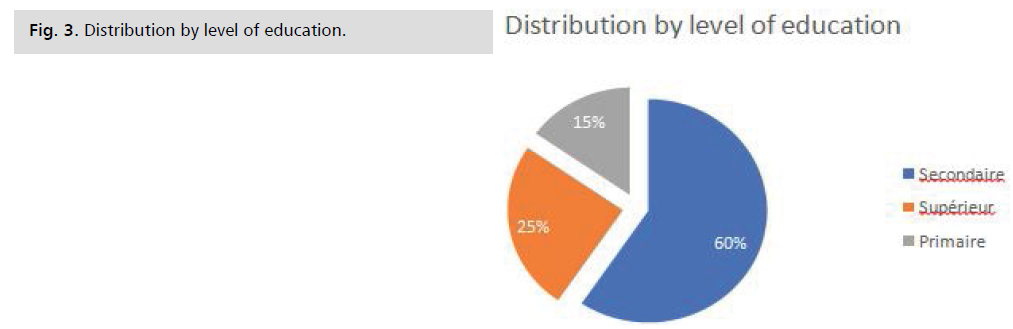
Fig. 3: Distribution by level of education.
Economic level Family: Most of the patients had a
medium income level 53.15%, followed by low income
patients 35.14% and high income patients came last
11.71% Tab. 2.
| Economic level |
Workforce |
Percentage |
| Medium |
59 |
53,15% |
| Low |
39 |
35,14% |
| High |
13 |
11,71% |
| Grand Total |
111 |
100,00% |
Tab. 2. Economic level family.
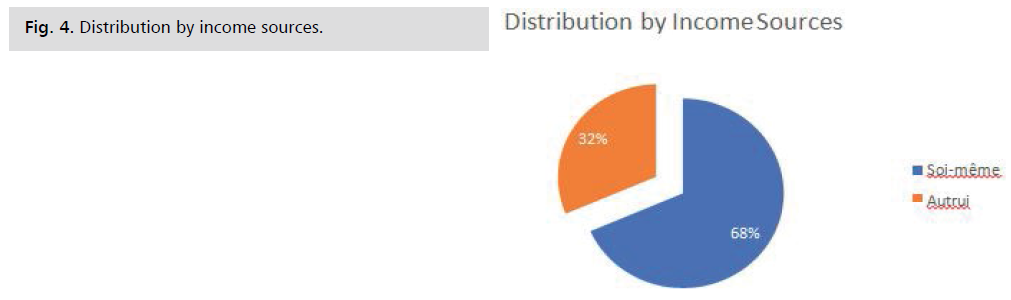
Source of income: We find that among the inpatients,
68% had other people as their source of income; only 32%
had themselves as their source of income Fig. 4.
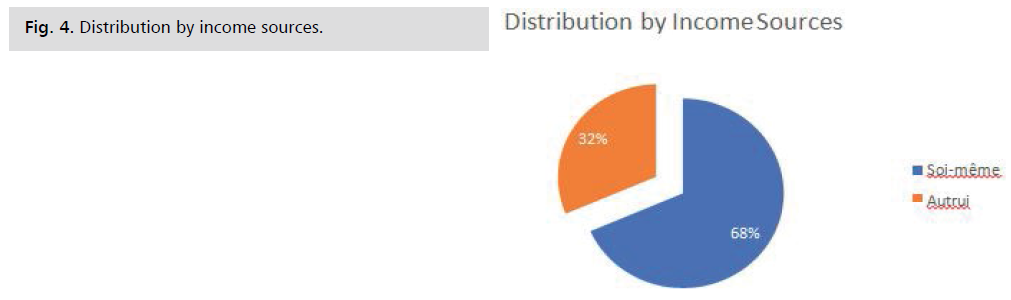
Fig. 4: Distribution by income sources.
Profession: This table shows that Military was the
most frequent occupation with 28.83%, followed by
Unemployed with 27.93%; Student with 6.31%; Biker
and Teacher were represented at 4.50%; Engineer and
State Agent represented 3.60%. And the rest were other
professions with 20.73% Tab. 3.
| Profession |
Workforce |
Percentage |
| Military |
32 |
28,83% |
| Unemployed |
31 |
27,93% |
| Student |
7 |
6,31% |
| Biker |
5 |
4,50% |
| Teacher |
5 |
4,50% |
| Trader |
4 |
3,60% |
| Engineer |
4 |
3,60% |
| State agent |
3 |
2,70% |
| Lawyer |
2 |
1,80% |
| Commercial agent |
2 |
1,80% |
| Financial |
2 |
1,80% |
| Mason |
1 |
0,90% |
| Professor |
1 |
0,90% |
| Mason's helper |
1 |
0,90% |
| Administrative |
1 |
0,90% |
| Driver |
1 |
0,90% |
| Hairdresser |
1 |
0,90% |
| Trainee doctor |
1 |
0,90% |
| Cabin boy |
1 |
0,90% |
| Painter |
1 |
0,90% |
| Nurse |
1 |
0,90% |
| Student |
1 |
0,90% |
| Cashier |
1 |
0,90% |
| Journalist |
1 |
0,90% |
| Contractor |
1 |
0,90% |
| Grand Total |
111 |
100,00% |
Tab. 3. Profession.
Legal problems: Of the patients followed up, 74.77%
had never experienced any legal problems; 18.02% had
experienced problems without incarceration and 7.21%
with incarceration Tab. 4.
| Legal problems |
Workforce |
Percentage |
| Never |
83 |
74,77% |
| Yes, without incarceration |
20 |
18,02% |
| Yes with incarceration |
8 |
7,21% |
| Grand Total |
111 |
100,00% |
Tab. 4. Legal problems.
Data related to addictive behavior
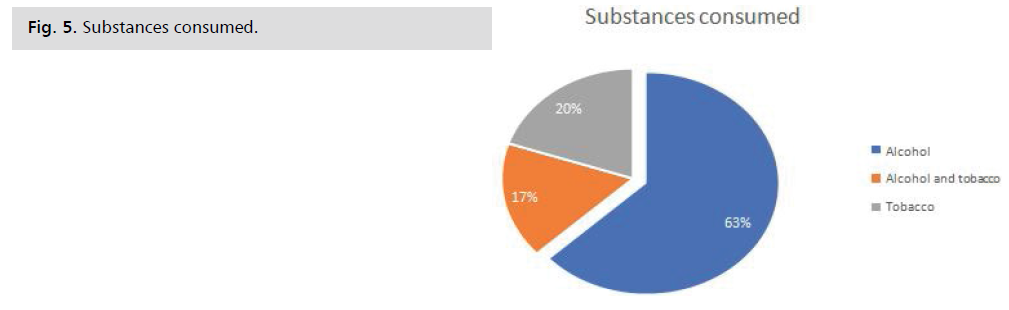
Substances consumed: This graph shows that Alcohol
was the most consumed substance with 63%; followed by Tobacco with 20% and the combination of Alcohol and
Tobacco with 17% Fig. 5.
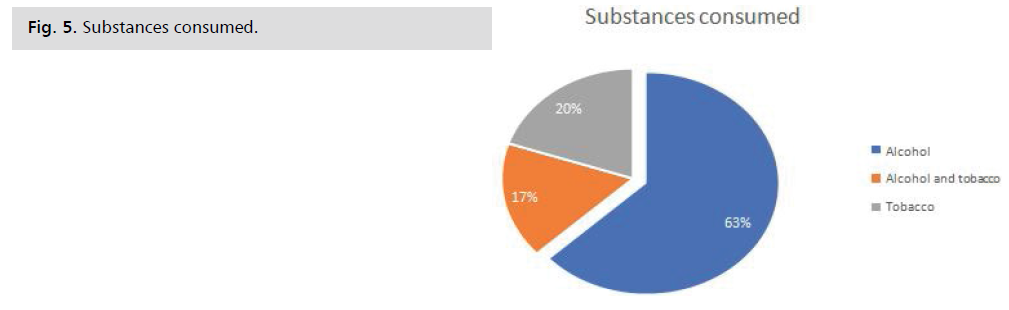
Fig. 5: Substances consumed.
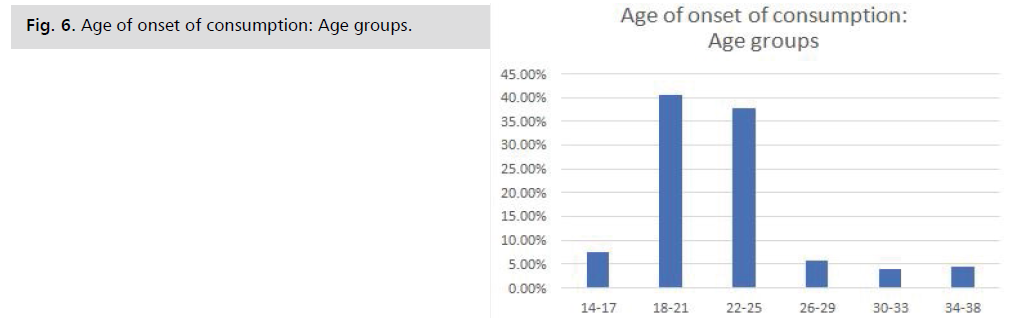
Age of onset: This histogram shows that the most
represented age group was 18 to 21 years with 40.56%;
followed by 22 to 25 years with 37.73%; 14 to 17 years
with 7.56%; 26 to 29 years with 5.66%; 34 to 38 years
with 4.56%; the least represented was 30 to 33 years
with 3.93%. Central tendency values: Mean: 21 years;
Median: 21 years; Mode: 18
years; Standard deviation: 4.01; Quartile 1: 18 years;
Quartile 2: 21 years; Quartile 3:
22.5 years Fig. 6.
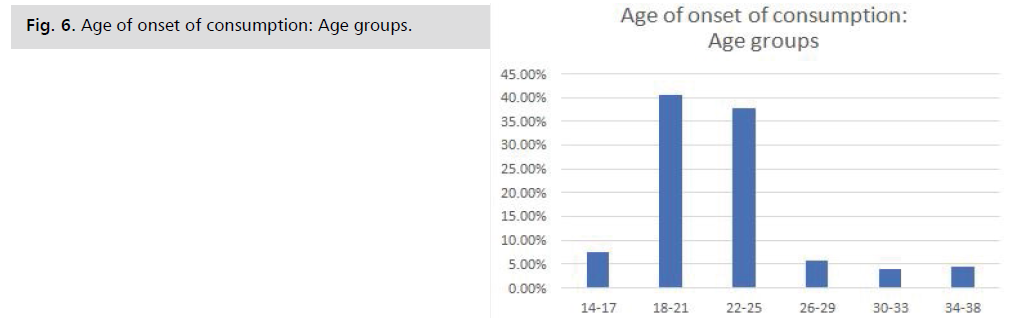
Fig. 6: Age of onset of consumption: Age groups.
Motivations for consumption: The most frequent
consumption motivation was relaxation and pleasure with
35.14%; followed by stress reduction with 32.43%; social
conformity with 14.41%, coping with a situation with
11.71% and the least frequent was to fill boredom with
6.31% Tab. 5.
| Motivations for consumption |
Workforce |
Percentage |
| Relaxation and fun |
39 |
35,14% |
| Stress reduction |
36 |
32,43% |
| Social compliance |
16 |
14,41% |
| Coping with a situation |
13 |
11,71% |
| Filling the boredom |
7 |
6,31% |
| Grand Total |
111 |
100,00% |
Tab. 5. Motivations for consumption.
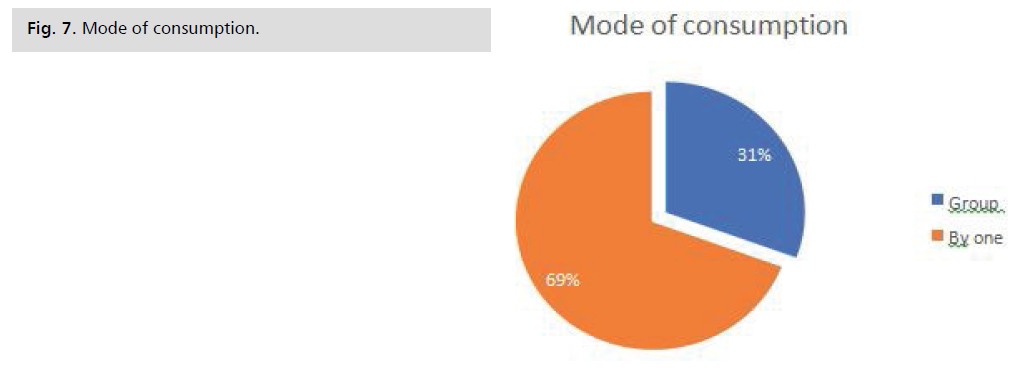
Mode of consumption: This graph shows that most
patients used APS alone (69%). Group use was represented
by only 31% Fig. 7.
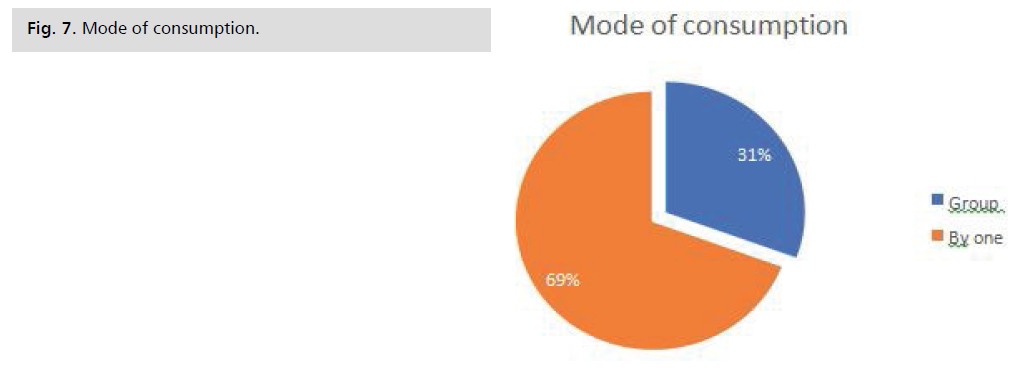
Fig. 7: Mode of consumption.
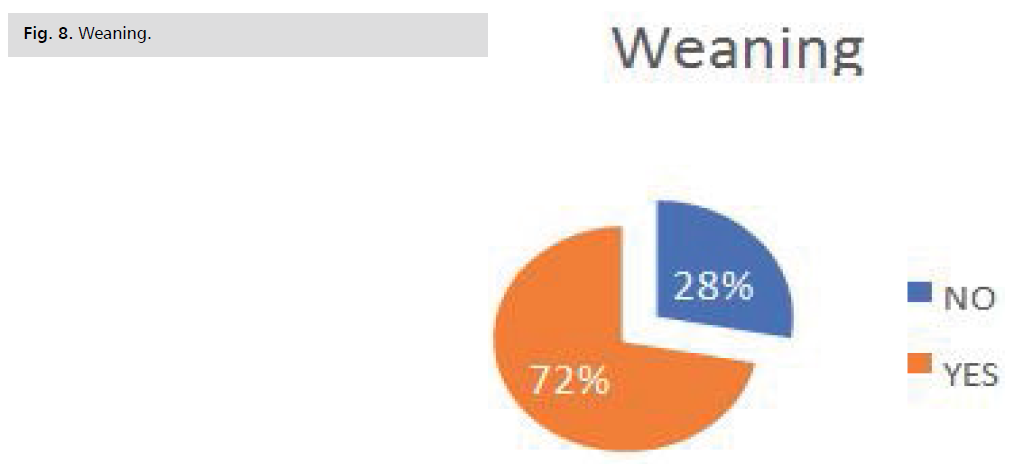
Weaning: This table shows that Anxiety was the
most experienced symptom with 23.42% followed by
Nervousness with 21.62%; Convulsions with 9.91%;
Trembling of the extremities, Confusion and Hallucinations were represented at 8.11%; Profuse sweating with 6.31%;
Nightmares with 4.50%; Insomnia with 3.60%; Vomiting
with 2.70%; Palpitations with 1.80%; Hyperthermia and
Tachycardia with 0.90% Fig. 8, Tab. 6.
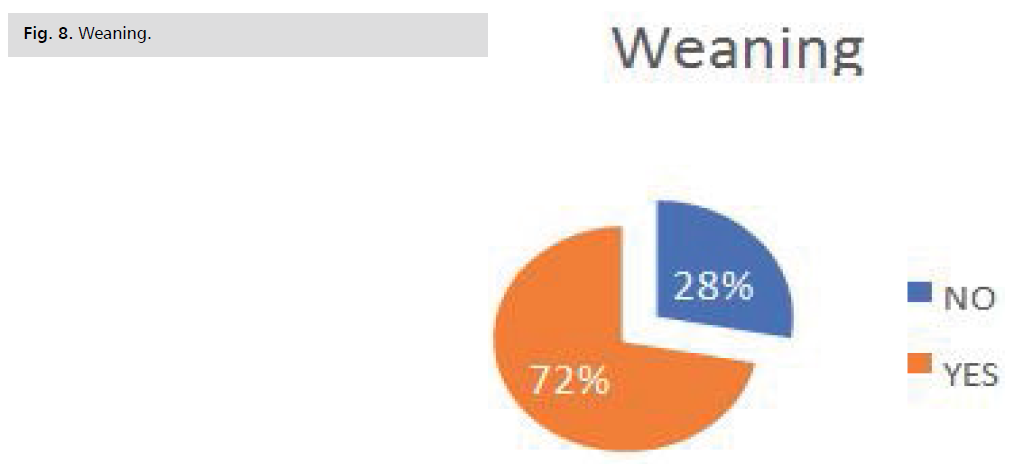
Fig. 8: Weaning.
| Symptoms experienced after weaning |
Workforce |
Percentage |
| Anxiety |
26 |
23,42% |
| Nervousness |
24 |
21,62% |
| Convulsions |
11 |
9,91% |
| Trembling of the extremities |
9 |
8,11% |
| Confusions |
9 |
8,11% |
| Hallucinations |
9 |
8,11% |
| Profuse sweating |
7 |
6,31% |
| Nightmares |
5 |
4,50% |
| Insomnia |
4 |
3,60% |
| Vomiting |
3 |
2,70% |
| Palpitations |
2 |
1,80% |
| Hyperthermia |
1 |
0,90% |
| Tachycardia |
1 |
0,90% |
| Grand Total |
111 |
100,00% |
Tab. 6. Weaning.
Somatic complications related to the use of APS: This
table shows that weight loss was the most common somatic
complication with 27.03%; followed by no complication
with 24.32%; then bloody sputum with 14.41%; lower
limb or generalised oedema and liver cirrhosis with 8.11%;
chronic cough and digestive bleeding accounted for 7.21%.
The least frequent somatic complication was recurrent
anaemia with 3.60% Tab. 7.
| Somatic complications |
Workforce |
Percentage |
| Weight loss |
30 |
27,03% |
| No |
27 |
24,32% |
| Bloody sputum |
16 |
14,41% |
| Edema of the lower limbs or generalized |
9 |
8,11% |
| Cirrhosis of the liver |
9 |
8,11% |
| Chronic cough |
8 |
7,21% |
| Digestive bleeding |
8 |
7,21% |
| Recurrent anaemia |
4 |
3,60% |
| Grand Total |
111 |
100,00% |
Tab. 7. Somatic complications related to the use of APS.
Data related to psychiatric pathology
Psychiatric diagnosis: Chronic psychotic disorder was
the most frequent diagnosis with 52.25%, followed by
mood disorder with 21.62%, acute psychotic disorder with
17.12%, personality disorder with 5.41%, anxiety disorder
with 2.70% and sleep disorder with 0.90% Tab. 8.
| Psychiatric diagnosis |
Workforce |
Percentage |
| Chronic psychotic disorder |
58 |
52,25% |
| Mood disorder |
24 |
21,62% |
| Acute psychotic disorder |
19 |
17,12% |
| Personality disorder |
6 |
5,41% |
| Anxiety disorder |
3 |
2,70% |
| Sleep disorder |
1 |
0,90% |
| Grand Total |
111 |
100,00% |
Tab. 8. Psychiatric diagnosis.
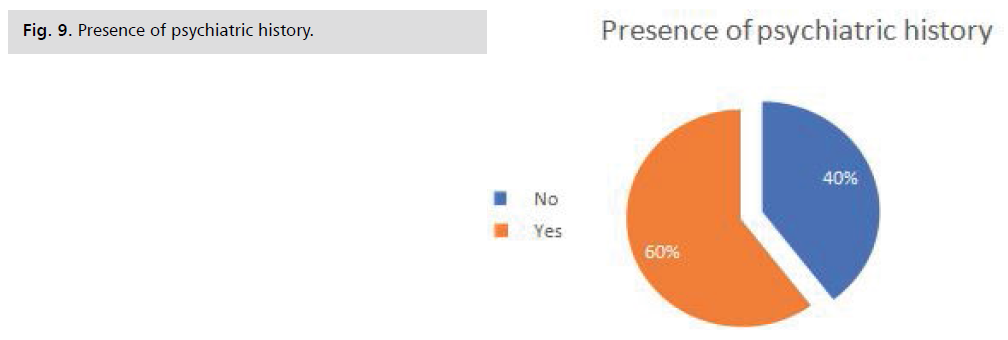
Presence of a family history: This graph shows that
most of the patients had a family history of psychiatric illness (69%). The absence of psychiatric history in the
family was 31% Fig. 9.
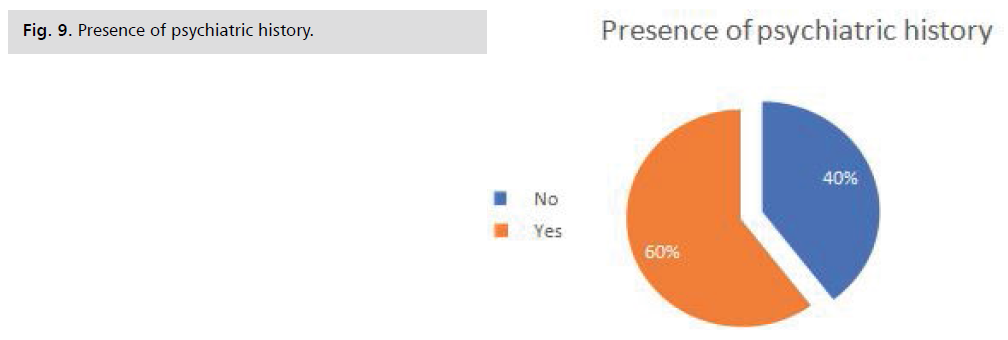
Fig. 9: Presence of psychiatric history.
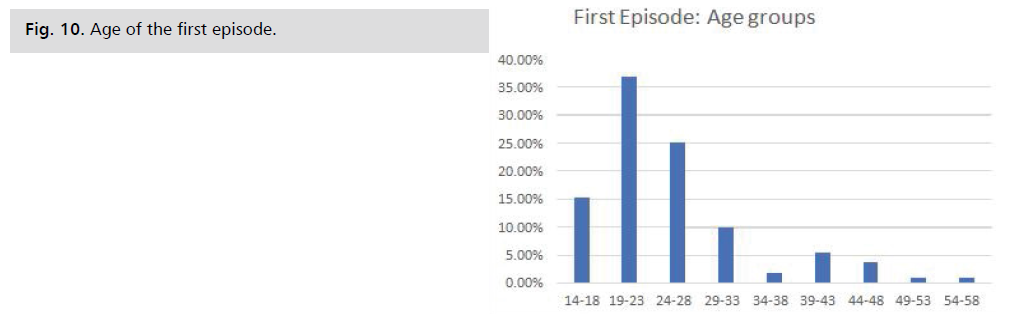
Age of the first episode: This histogram shows that
the most represented age group was 19 to 23 years with
36.94%; followed by 24 to 28 years with 25.23%; 14 to
17 years with 15.32%; 29 to 33 years with 9.91%; 39 to
43 years with 5.41%; 44 to 48 years with 3.60%; 34 to 38
years with 1.80%. The least represented classes were: 49
1, 80%. Central tendencies: Mean: 25 years; Median: 23
years; Mode: 18 years; Standard deviation: 8.16; Quartile
1: 21 years; Quartile 2: 23 years; Quartile 3: 28 years Fig. 10.
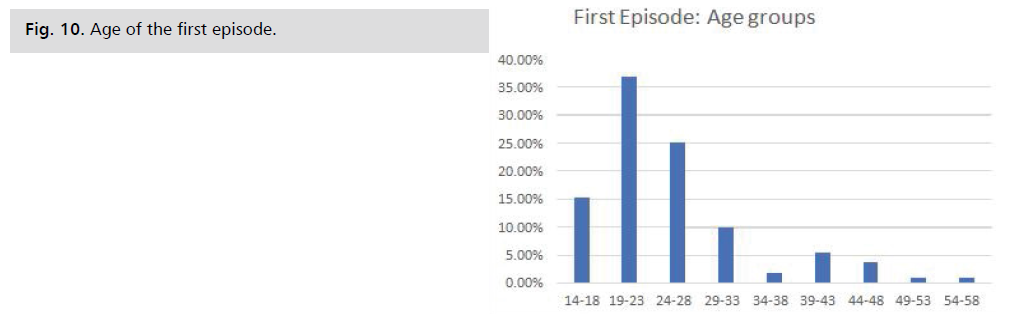
Fig. 10: Age of the first episode.
Link between addiction and psychiatric
pathology
Substance use and psychiatric disorder: We note
from this table that most psychiatric disorders were
present in patients consuming only alcohol, and were
moderately present in those consuming only tobacco. The
psychiatric disorders frequently found in the three types of
consumption were chronic psychotic disorder (52.25%),
followed by mood disorder (21.62%), chronic psychotic disorder (19.82%), acute psychotic disorder with (17.12%),
personality disorder with (5.41%), anxiety disorder with
(2.70%) and sleep disorder with (0.90%) Tab. 9.
| Substance Use and Psychiatric Disorder |
Workforce |
Percentage |
| Alcohol |
70 |
63,06% |
| Chronic psychotic disorder |
37 |
33,33% |
| Mood disorder |
13 |
11,71% |
| Acute psychotic disorder |
11 |
9,91% |
| Personality disorder |
5 |
4,50% |
| Anxiety disorder |
3 |
2,70% |
| Sleep disorder |
1 |
0,90% |
| Tobacco |
22 |
19,82% |
| Chronic psychotic disorder |
12 |
10,81% |
| Mood disorder |
7 |
6,31% |
| Acute psychotic disorder |
2 |
1,80% |
| Personality disorder |
1 |
0,90% |
| Alcohol and Tobacco |
19 |
17,12% |
| Chronic psychotic disorder |
9 |
8,11% |
| Acute psychotic disorder |
6 |
5,41% |
| Mood disorder |
4 |
3,60% |
| Grand Total |
111 |
100,00% |
Tab. 9. Substance use and psychiatric disorder.
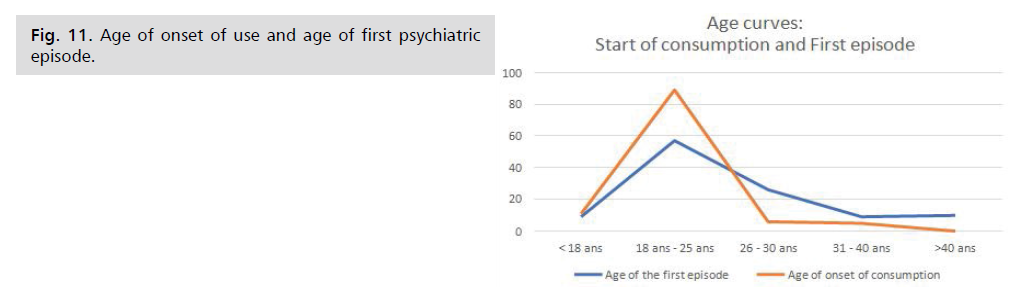
Age of onset of use and age of first psychiatric
episode: This graph shows the evolution of the age of onset of the first psychiatric episode and the age of onset of use
according to age groups. It can be seen that the onset of
APS use was between the ages of 18 and 30, with a peak
between 18 and 25. The first psychiatric episode often
appeared between the ages of 18 and 40, peaking between
18 and 30 and stabilising around 40. The ages of onset of psychiatric pathology and the onset of PSA use overlapped
significantly Fig. 11.
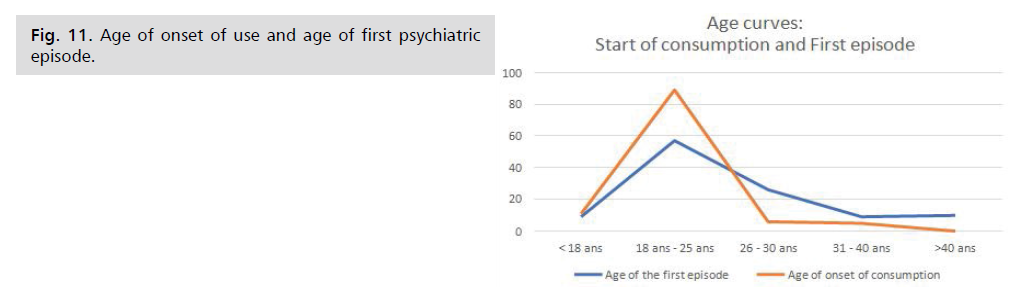
Fig. 11: Age of onset of use and age of first psychiatric episode.
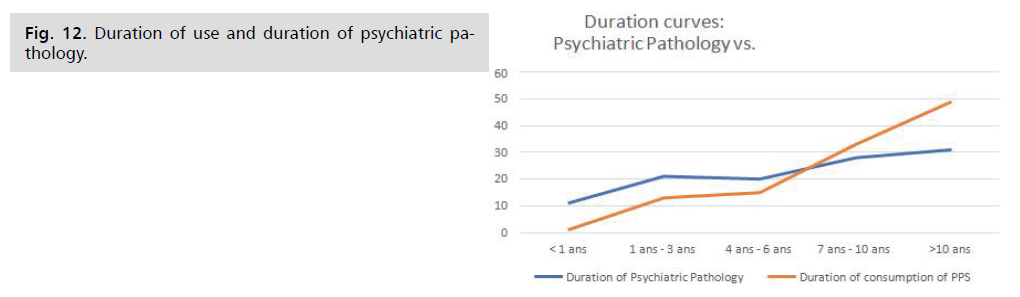
Duration of use and duration of psychiatric
pathology: This graph shows the evolution of the duration
of psychiatric pathology and consumption Fig. 12.
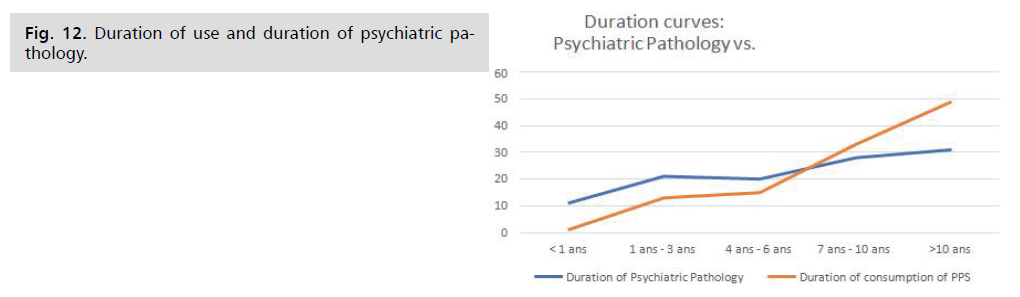
Fig. 12: Duration of use and duration of psychiatric pathology.
Discussion
It seems to us that patients hospitalised for mental health
problems related to the use of psychoactive substances had
particular socio-demographic and addiction characteristics.
In particular, they had more difficulty in stopping using
these substances and seemed less interested in the activities
offered during their hospitalization.
Characteristics of addiction
Thus, our results show a predominantly male sample
with an average age of 21 years, which is in line with the
data in the literature [8]. The patients are characterized by
average precariousness. Alcohol use is high.
It is true that the inactivity of these patients is a factor
in addiction, but alcoholisation can also be a consequence
of inactivity. In fact, 10 to 20% of accidents at work are
linked to alcohol consumption and many patients with an
alcohol-related disorder are on disability (road accident,
depression, chronic pathologies) [8]. Similarly, people
who are unemployed are 2.4 times more likely to be binge
drinkers than those who are employed and 2.7 times more
likely to be alcohol dependent [9].
Only one third of the sample had pursued higher
education - a lower score than that reported in a French
study which reported 43.6% of 30-34 year olds having
successfully completed higher education [6].
Young people aged 14 to 17 who left school early or had
a chaotic school career that led them to short or vocational
courses are almost twice as likely to use APS regularly as
young people still in mainstream education [10]. More
than one patient in two has already had to deal with the
law, mainly for traffic offences.
The preliminary results of our study allow us to better
analyse the factors associated with the excessive use of
APS: being a middle-aged, inactive, single man, with little
education and a history of trouble with the law seems to
be the most at risk of using APS and becoming an addict.
It can therefore help us to target at-risk populations before
implementing policies to improve health status and reduce
avoidable mortality.
Our work also highlights two facts: the main motivation
for consumption is relaxation and pleasure and the other
motive is conformity with the social group.
One proposal would be, for example, to systematically
introduce a specific interview at the beginning of a general
medical consultation, taking into account the DSM-V
criteria and the above characteristics.
Analysis of data on the use of alcohol and tobacco
products also shows that consumption begins in adolescence
at around 14 and a half years of age, in line with the data in
the literature (80% of 17 year olds have already consumed
alcohol in the last 30 days) [9].
Our patients have undertaken an average of one
withdrawal in their lives, stopping their consumption
for a maximum of one and a half years. According to the literature, recidivism is frequent in alcohol-dependent
patients.
The large number of withdrawals and the short periods
of abstinence can be explained by the fact that a certain
number of patients were hospitalised at the request of their
families, or that some were facing difficult family and social
situations (homelessness, somatic symptoms (weight loss,
decompensated liver disease, generalized oedema of the
lower limbs, bloody sputum, psychiatric manifestations
(anxiety, nervousness, convulsions, etc.).
Characteristics of dual pathology
The link between addictions and psychiatric pathologies
is both close and complex: addiction is a determinant
of exposure to dual pathologies before the age of 26. In
this young population, the use of APS was for relaxation,
pleasure and societal conformity. After the age of 26, the
use of APS has a therapeutic motivation to reduce stress
and to cope with difficult situations. Addiction and
psychiatric pathology seem to feed on each other and vice
versa regardless of the precession of one on the other.
The causal link is not fixed, and very often patients
find themselves in a vicious circle. The use of APS can be
explained as a strategy to manage the psycho-trauma: it is
then a question of managing to forget the memories that
arise without warning and to anaesthetize the emotions.
In this case, consumption precedes the disorder. In other
cases, people suffering from psychiatric illnesses use
psychoactive substances to cope with the many symptoms
they cause, particularly in the case of addiction to alcohol
or psychotropic drugs, which alleviate these situations and
enable them to be tolerated [11].
The psychiatric disorders encountered in our series are
distributed as follows: Chronic psychotic disorder 52.25%; Mood disorder 21.62%; Acute psychotic disorder 17.12%;
Personality disorder 5.41%; Anxiety disorder 2.70% and
Sleep disorder 0.90%.
Some substances are more likely to cause addiction and
aggravate existing mental disorders. In our case, alcohol was
correlated with all the above-mentioned disorders. Tobacco
was to a lesser degree and did not seem to be correlated
with anxiety and sleep disorders. The combination of
alcohol and tobacco predisposed to chronic psychotic
disorder, mood disorders and acute psychotic disorder. This
is explained by the fact that the longer a person consumes
a psychoactive substance, the more likely he or she is to
develop an addiction and to suffer from mental health
problems. Prolonged use of psychoactive substances can
also lead to tolerance, which means that the person has
to take higher and higher doses to feel the same effects.
This leads to the risk of overdose and serious mental health
problems or even death.
But the etiopathogenic link between APS and
psychiatric pathology cannot be considered only in a linear
way where one substance induces a psychiatric disorder;
the link is much more complex and involves several factors.
In sum, several variables characterise the link between
addiction and psychiatric pathologies, most of which have
been addressed in this work, but the following factors
should also be taken into account.
Co-morbidity: This is the simultaneous presence
of several mental or physical disorders. Co-morbidity is
common in addiction and psychiatric disorders, such as
depression and anxiety.
Risk factors: Certain risk factors, such as stress, anxiety
and depression, can increase the risk of developing an
addiction.
Coping mechanisms: People with psychiatric
conditions may use addiction as a way of coping with
difficult emotions. However, this can lead to long-term
addiction.
Treatment: It is important to treat the addiction and
psychiatric disorders simultaneously to maximize the
chances of long-term recovery.
Relapse: People who have suffered from addiction and
psychiatric disorders are at increased risk of relapse if one of
the problems is not adequately treated.
Genetic factors: Some people have an increased risk
of developing an addiction or mental illness for genetic
reasons.
Trauma history: People who have experienced
trauma, such as abuse or bereavement, are at greater risk of
developing an addiction or mental illness.
Level of social support: People with a strong social
support network are less likely to develop an addiction or
a mental illness.
Level of education and income: People with a
higher level of education and income have a lower risk of
developing an addiction or a mental illness.
Environmental factors: Some people are more at risk
of developing an addiction or mental illness because of
their living environment, such as lack of family stability or
work-related stress.
Conclusion
Several large-scale epidemiological studies have
consistently found high rates of co- morbidity between
psychiatric disorders and addictive disorders. Moreover,
many studies have shown the negative consequences
of these co-morbid disorders in terms of physical and
psychological health, but also in terms of social situation,
and this at a higher level than in the general population. The
co-occurrence of a severe mental disorder and an addictive
pathology therefore represents a real public health issue.
There is a well-established link between addiction and
certain psychiatric conditions, such as mood disorders
(depression), anxiety and psychotic disorders. Addiction is
often used as a form of temporary "treatment" for these
disorders by patients, but it can also aggravate them in the
long term.
People with psychiatric conditions are also more
likely to develop an addiction because of their emotional
vulnerability. It is important to treat both problems
simultaneously in order to maximize the chances of longterm
recovery.
The difficulties associated with the management
of these co-morbid disorders make access to care more
complicated and are the cause of many therapeutic failures.
Despite an arbitrary institutional divide between addiction
and psychiatric medical structures, the links between
addiction and psychiatric disorders are so strong that
their study and management require these structures to
be coupled and their material and human resources to be
pooled in order to address these issues in a holistic manner.
Their impact on public health is such that it is necessary to
insist on multidisciplinary management. This dynamic has
inspired us to draw up an inventory of epidemiological,
socio-demographic and etiopathogenic knowledge that will
open up avenues for solutions to reduce the impact of these
diseases. However, it is clear that this modest study is only
a beginning.
References
- Goodman A. Addiction: Definition and implications. Br J Addict.1990;85(11):1403-1408.
Google Scholar, Crossref, Indexed at
- Lançon C. Addictive behaviours and processes of change. J Libbey edit. 2013.
- Menecier P, Fernandez L. [Addictive behavior among the elderly]. Presse Medicale Paris Fr 1983. 2012;41(12):1226-1232.
- Badin de Montjoye B, Podevin P, Pharo P. Abstinence from cocaine after long-term addiction. L'encephale. 2011;37(6):404-409.
Google Scholar, Crossref, Indexed at
- Lantheaume S. ACT in the treatment of sexual addiction: About a clinical case. L'encephale. 2017;44(4):387-391.
Google Scholar, Crossref, Indexed at
- Franques P, Auriacombe M, Tignol J. [Addiction and personality]. L'Encephale. 2000;26(1):68-78.
- Karila L, Benyamina A. Addictions. Rev Mal Respir. 2019;36(2):233-240.
- Besson J, Grivel J, Tomei A, et al. [Addiction]. Rev Med Suisse. 2014;10(412-413):13-17.
- Bertolini M. Adolescence and addictions. Rev Med Suisse. 2011;7(309):1794-1798.
- Kommegne T, Denoux P, Bernoussi A, et al. Addictive behavior of street children: Interculturation and resilience. L'encephale. 2013 Dec 17;40(4):315-322.
Google Scholar, Crossref, Indexed at
- Szerman N. Decalogue of dual pathology: addiction and other mental disorders. World Assoc Dual Disord.