Abstract
Postsurgical critical care unit patients are known to experience complications from systemic inflammatory response syndrome. The majority of cerebral palsy patients who receive posterior spinal fusion for neuromuscular scoliosis exhibit SIRS in the intensive care unit, according to our observations. Literature on the effects of intraoperative causes of postoperative SIRS and subsequent effects in these individuals is scarce. The goal of the study was to better understand the risk factors for SIRS in children undergoing PSF for neuromuscular scoliosis. Children who had PSF for neuromuscular scoliosis were included in this retrospective, case-control study. Patients with tracheotomy, osteogenesis imperfecta, and idiopathic scoliosis were eliminated. Depending on whether SIRS had been identified in the intensive care unit, the subjects were split into two study groups. To pinpoint factors, descriptive statistical analysis was employed. In order to further assess the independent and substantial influence of these parameters on SIRS, a regression analysis was utilised. The demographic and other preoperative characteristics did not significantly differ. However, the SIRS group received considerably more blood products overall than the non-SIRS group. When compared to the non-SIRS group, the percentage of patients who remained intubated was higher in the SIRS group. According to the regression model, patients who were not extubated had a 7.467-fold higher chance of developing SIRS than those who had been extubated. Patients who were not extubated at the conclusion of PSF surgery have a considerably greater incidence of SIRS. Additional prospective studies are required to examine the elements that hinder extubation. These individuals following their operation Cerebral palsy patients undergoing posterior spinal fusion for neuromuscular scoliosis frequently have serious comorbidities include seizures, chronic lung disease, poor nutrition, and recurrent UTIs.
Keywords
Scoliosis; Neuromuscular; Systemic inflammatory response
syndrome; Spinal fusion; Postoperative extubation; Children
INTRODUCTION
Preoperative optimisation has significantly improved in the
last ten years in terms of lung function, diet, and seizure
control. When compared to PSF for idiopathic scoliosis,
postoperative morbidity in this cohort remains significant
despite advancements in anaesthetic management and
surgical technique. Children with neuromuscular scoliosis
who undergo posterior spinal fusion often have severe
blood loss as a result of poor nutrition that causes a lack
of coagulation factors and abnormalities in the vascular
con nective tissue. As a result, large volume transfusions
are frequently used in intraoperative fluid control. of
blood products and crystalloids. With the restriction of
crystalloid, balanced transfusion of blood products with
a larger ratio of fresh frozen plasma, packed red blood
cells, and the use of anti-fibrinolytic to prevent excessive
blood loss, transfusion practises have improved recently.
While these actions have improved the intraoperative
course, nothing is known about how they may affect the
morbidity and death rates in the immediate postoperative
course [1]. A systemic inflammatory response syndrome
is characterised by two or more of the disorders listed
below: tachycardia is characterised by a mean heart rate
that is more than two standard deviations above the agerelated
average, a mean respiratory rate that is more than
two standard deviations above the age-related average, or
mechanical tachycardia. Leukocyte counts that are raised or
decreased for age-immature neutrophils and ventilation for
an acute pulmonary process [2]. After cardiac surgery and
in children who have emergency intestinal procedures, the
diagnosis of SIRS and its effects on the postoperative course
have been thoroughly characterised. Patients who undergo
major surgery are more likely to develop SIRS at this time
due to the interaction of substantial fluid shifts, blood
transfusions, and surgical tissue stress [3]. In the community
of patients with neuromuscular spine fusion admitted to the
paediatric critical care unit, we have observed an increase
in the diagnosis of SIRS. In this study, the incidence of
SIRS throughout the postoperative period was investigated
in relation to preoperative patient characteristics and
intraoperative anaesthetic care. We sought to look back
and assess the effect on length of stay in the PICU of fluid
management, transfusion practises, the choice to extubate,
and the development of SIRS [4]. A mean respiratory rate
that is more than two standard deviations over the ageappropriate
norm; a leukocyte count that is high or low
for the age; or a percentage of immature neutrophils [5].
To fully understand the influence of the intraoperative
and preoperative factors over the incidence of SIRS in the
ICU, the time for SIRS diagnosis was restricted to 48 hours
[6]. Categorical variables were expressed as a percentage
of an outcome in a group, while continuous variables
were expressed as means standard deviation [7]. The
preoperative, intraoperative, and postoperative differences
between the SIRS and non-SIRS groups were compared
using a univariate approach. To assess statistical significance
between the two groups, the chi-square contingency test
was used for categorical data and the t-test for continuous
variables [8]. Prior to transformation, continuous variables
with wide distributions were converted raw means were
calculated and displayed in the findings, but no p values
were obtained from the analysis. Additionally, a logistic
regression analysis was performed to find risk factors that
contribute on their own to SIRS development [9]. The
regression model comprised variables that were significant
in univariate analysis or important to the SIRS outcome.
The SPSS statistical software system was used for the
statistical analysis, which was deemed significant [10].
MATERIAL AND METHODS
1. Study design: The study design could be retrospective
or prospective, depending on the availability of data
and the research objectives. A retrospective study
would involve reviewing medical records and data
from a previous period, while a prospective study
would involve collecting new data from participants.
2. Participant selection: Participants would include
young individuals with developmental disabilities who
have undergone scoliosis surgery and subsequently
experienced postpartum SIRS. The inclusion criteria
would specify the age range, type of developmental
disability, and history of scoliosis surgery.
3. Data collection: Relevant data would be collected
from medical records and patient charts. This
would include demographic information, details of
the scoliosis surgery, postoperative complications,
presence of postpartum SIRS, and any other relevant variables.
4. Risk assessment: Statistical analysis would be
conducted to assess the association between scoliosis
surgery and postpartum SIRS in young individuals
with developmental disabilities. This may involve
calculating odds ratios, relative risks, or conducting
regression analysis to control for potential confounding
factors.
5. Ethical considerations: Ethical approval would be
obtained from the appropriate research ethics board
or committee to ensure participant privacy, informed
consent, and compliance with ethical guidelines.
RESULTS
Invariable analysis of variables between SIRS and
non-SIRS. After the electronic medical records of the
intraoperative anesthesia and intensive care documentation
were reviewed, a total of 77 patients met the criteria and
were included in the study. The patients were divided into
2 groups based on the incidence of SIRS in the intensive
care unit. We had 34 patients in the SIRS group and 43
patients in the non-SIRS group [Fig.1].
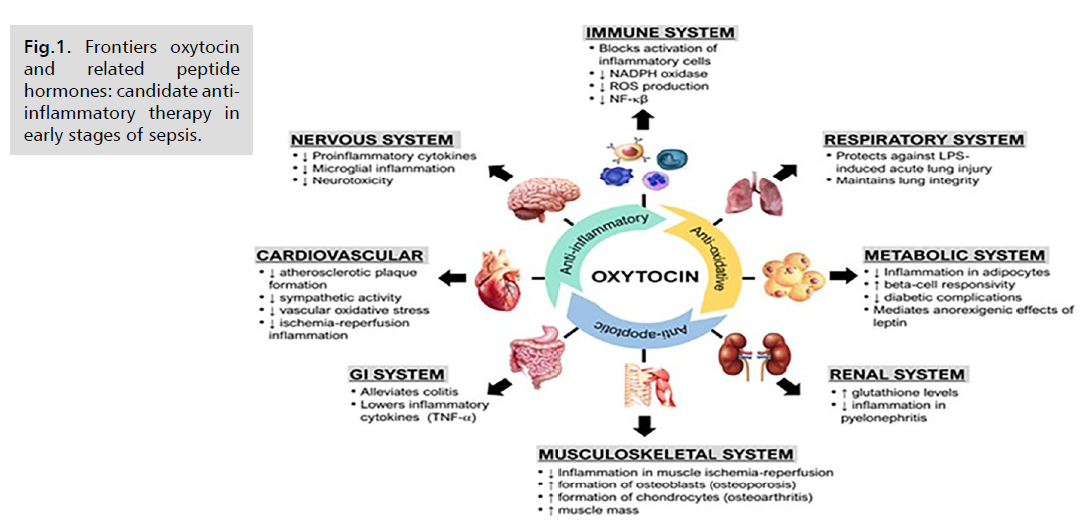
Fig.1. Frontiers oxytocin
and related peptide
hormones: candidate antiinflammatory
therapy in
early stages of sepsis.
The SIRS and non-SIRS groups had similar demographic
and clinical conditions preoperatively. No significant
differences were found in terms of degree of scoliosis, type
of surgery, feed status, and seizures or on medication for
suspected seizures [Tab.1.].
The percent of patients with GMFCS Score ≥5 was 85.3%
in the SIRS group, which was higher but not significantly
when compared with the non-SIRS at 69.8% (Table 1;
p=0.091). On the other hand, 17.6% patients in the SIRS
group had intact verbal function comparing with 34.9% in
the non-SIRS group, but the difference was not significant
| Non-Extubated (N=18) |
Extubated (N=59) |
P Value |
|
| Demographic, medical conditions variables: |
|
|
|
| Gender (M/F) |
10-Aug |
23/36 |
0.166 |
| Age |
12.2±2.5 |
13.3±3.2 |
0.203 |
| Weight |
34.6±14.1 |
35.9±11.0 |
0.688 |
| Unit rod surgery % |
61.1% (11) |
52.5% (31) |
0.358 |
| % with Kyphosis |
44.4% (8) |
33.9% (20) |
0.294 |
| GMF Score ≥5 % |
94.4% (17) |
71.2% (42) |
0.035 |
| Verbal % |
16.7% (3) |
30.5% (18) |
0.2 |
| G Tube % |
72.2% (13) |
57.6% (34) |
0.203 |
| Intra-operative variables: |
|
|
|
| Surgery time (Minutes) |
472.4±164.7 |
341.0±121.2 |
0.001 |
| Estimated blood loss (ml/Kg) |
51.8±27.8 |
30.7±21.7 |
0.001 |
| Total blood products (mg/Kg) |
74.8±39.9 |
33.3±23.5 |
<0.001 |
| Total crystalloid (mg/Kg) |
102.0±44.4 |
69.0±28.3 |
0.001 |
| % Received Platelets |
72.2% (13) |
11.9% (7) |
<0.001 |
| PRBC (ml/kg) |
30.8±18.5 (17) |
16.2±11.1 (37) |
0.001 |
| FFP (ml/kg) |
28.6±13.9 (16) |
13.9±8.5 (54) |
<0.001 |
| FFP/PRBC Ratio |
1.1±0.5 (16) |
1.1±0.6 (34) |
0.762 |
| Cell saver (ml/kg) |
18.6±10.5 (14) |
11.0±7.5 (50) |
0.003 |
| Lowest Hgb in OR |
9.3±1.7 |
10.2±1.5 |
0.03 |
| % Vasopressor in OR |
55.6% (10) |
28.8% (17) |
0.038 |
| Post-operative and ICU variables: |
|
|
|
| % Bolus Crystalloid 24 |
77.8% (14) |
49.2% (29) |
0.029 |
| SIRS |
83.3% (15) |
32.2% (19) |
<0.001 |
| % PRBC transfusion POD 1 and/or POD2 |
16.7% (3) |
16.9% (10) |
0.644 |
| % Transfusion 48 hours and discharge |
16.7% (3) |
10.1% (6) |
0.351 |
| Circulatory support with inotropes |
66.7% (12) |
11.9% (7) |
<0.001 |
| Intubated ≥1 day* |
94.4% (17) |
3.4% (2) |
<0.001 |
| ICU >2 days (range:0.5-15 days) |
83.3% (15) |
33.9% (20) |
<0.001 |
| Hospital days >8 (range: 2-85 days) |
72.2% (13) |
42.4% (25) |
0.025 |
| Wound infection at discharge |
11.1% (2) |
5.1% (3) |
0.332 |
Tab.1. Comparison of patient’s
extubated and not extubated in the
operating room.
DISCUSSION
In the context of young individuals with developmental
disabilities who have undergone scoliosis surgery, the risks
associated with postpartum SIRS may be influenced by
several factors. These can include: Surgery-related factors:
The type of scoliosis surgery, its invasiveness, duration, and any complications during or after the procedure can impact
the overall stress on the body and potentially contribute
to an increased risk of postpartum SIRS. Developmental
disabilities: Individuals with developmental disabilities
may have unique physiological and immunological
characteristics that can affect their response to surgery
and subsequent postpartum period. Their underlying
conditions may also contribute to an altered immune
response or predispose them to a higher risk of SIRS.
Postpartum care: The management of the postpartum
period, including monitoring for signs of SIRS, providing
appropriate pain management, and addressing any
complications or infections, are crucial in minimizing the
risk of postpartum SIRS.
CONCLUSION
TIS in children with early-onset scoliosis manifests as
a history of prominent respiratory symptoms, chest
deformity on physical examination, abnormal chest X-ray
and CT findings and changes in pulmonary function. A
potential therapeutic goal for this syndrome is to restore chest function and volume during growth. Although some
patients exhibit good spine growth with growth-friendly
surgery, there is still a subset of patients with poorer lung
outcomes in adulthood. Future research must continue
to focus on classification results based on the specific
diagnoses of EOS patients. Due to the repetitive nature
of prolonged surgery, treatment remains challenging and
complication rates are high. Accordingly, more research
is needed to further reduce complications and improve
outcomes after EOS. Successful treatments that encourage
the growth of the spine and chest will lead to good
outcomes for EOS patients. With the increase of curvature,
EOS patients can lead to structural changes in the chest
cavity, causing severe complications such as restrictive
lung disease, cardiovascular complications and respiratory
failure. However, the treatment of children with EOS is
customized according to specific diseases. Although lack
of treatment has been proved to lead to an increase in
mortality, extensive early and definite fusion may lead to
thoracic insufficiency. Delaying definite surgery and using
increasing instruments may be beneficial to keeping lungs
healthy.