Guive Sharifi1, Tahereh Gahdiri2,3*, Gelareh Vakilzadeh4 and Davide Nasi5
1Department of Neurosurgery, Loghman e Hakim Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
2Department of Neuroscience, Faculty of Advanced Medical Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
3Neuroscience Research Center, Tabriz, Iran
4Shefa Neuroscience Research Center, Khatamolanbia Hospital, Tehran, Iran
5Department of Neurosurgery, Institute for Scientific and Care Research "ASMN" of Reggio Emilia, Reggio Emilia, Italy
*Corresponding Author:
Dr. Tahereh Ghadiri
Department of Neuroscience, Faculty
of Advanced Medical Sciences, Tabriz
University of Medical Sciences, Tabriz, Iran
Tel: +98 41 33355789
E-mail: ghadirit@tbzmed.ac.ir, ghadiri21980@yahoo.com
Received Date: September 05, 2017 Accepted Date: October 03, 2017 Published Date:October 09, 2017
Citation: Sharifi G, Gahdiri T, Vakilzadeh G, Nasi D (2017) An Idiopathic Huge Trapped Temporal Horn: Surgical Strategy and Review of Literature. J Neurol Neurosci. Vol.8 No. S4: 229 doi: 10.21767/2171-6625.1000229
Keywords
Trapped temporal horn; Idiopathic; Ventriculo-cisternostomy; Subduro-peritonal shunt
Introduction
Temporal horn entrapment is a very rare kind of isolated focal non-communicating hydrocephalus caused by obstruction at the trigone of the lateral ventricle, which seals off the temporal horn from the rest of the ventricular system [1-3]. Since, outflow of cerebro-spinal fluid (CSF) is blocked due to an obstruction, continues secretion of CSF leads to progressive dilation of the temporal horn following effusion [4]. The dilated temporal horn compresses over the surrounding structures and results in numerous neurologic problems [5,6]. Information of all reported patients with temporal horn entrapment has been summarized in the Table 1 [1-27].
| Author, year |
Sex |
Age |
Side |
Cause |
Treatment |
| Cairns [4] |
M |
NR |
NR |
Penetrating wound |
Coagulation of plexus choroideus,ventriculostomy into 3rd ventricle |
| M |
19 y |
NR |
Penetrating wound |
Resection of plexus choroideus |
| NR |
7 m |
NR |
Subependymal hemorrhage suspected |
None, diagnosed at autopsy |
| Smith [24] |
NR |
NR |
R |
Grade II WHO astrocytoma |
NR |
| NR |
NR |
R |
Mass of unspecified origin |
NR |
| NR |
R |
R |
Meningioma |
NR |
| Maurice-Williams [16] |
F |
23 y |
R |
Recurrent glioma |
Direct communication to the atrium |
| F |
35 y |
R |
Tuberculous meningitis |
Ventriculo-atrial shunt |
| F |
30 y |
L |
Removal of arteriovenous malformation
(AVM) |
Ventriculo-peritoneal shunt |
| Ofori-Kwakye [18] |
F |
35 y |
R |
Cryptococcal meningoencephalitis |
External ventricular shunt |
| Schlitt [21] |
F |
33 y |
L |
Neurosarcoidosis |
Drainage of trapped temporal horn and ventriculo-peritoneal
shunt |
| Yamamoto [29] |
F |
2 y |
L |
Multiple streptococcal brain abscess |
Ventriculo-peritoneal
shunt |
| Bruck [3] |
M |
50 y |
L |
Xanthogranuloma of choroid plexus |
Removal |
| Tsugane [26] |
M |
35 y |
R |
Tuberculous meningitis |
External ventricular shunt followed by ventriculo-peritoneal shunt |
| F |
44 y |
R |
streptococcal brain abscess |
External ventricular shunt followed by ventriculo-peritoneal shunt |
| Watanabe [27] |
M |
16 y |
L |
Intraventricular hemorrhage by AVM rupture |
Ventriculo-peritoneal shunt |
| Coria [6] |
F |
70 y |
R |
Intracranial surgery for a giant basilar aneurysm |
Conservative |
| Parrent [20] |
M |
68 y |
R |
Cryptococcal meningitis |
Endoscopic fenestration of the choroidal
Fissure |
| Hamada [8] |
F |
7 m |
L |
Arachnoid cyst |
Endoscopic ventriculo-cyst-cysternostomy |
| Maurya [17] |
F |
25 y |
L |
Intraventricular hydatid cyst |
Removal |
| Lyngdoh [15] |
M |
12 y |
L |
Intraventricular meningioma |
Removal |
| F |
15 y |
L |
Intraventricular meningioma |
Removal |
| Berhouma [1] |
M |
60 y |
L |
Intraventricular meningioma |
Removal |
| F |
42 y |
R |
Neurosarcoidosis |
Temporal tip lobectomy |
| Singh [23] |
F |
35 y |
R |
Neurosarcoidosis |
Endoscopic removal |
| F |
35 y |
R |
Neurosarcoidosis |
Removal |
| Hervey-Jumper [10] |
M |
47 y |
L |
Ependymoma in the left atrium |
Fronto-temporal shunt |
| F |
70 y |
R |
B-cell CNS lymphoma |
Fronto-temporal shunt |
| F |
69 y |
R |
Glioblastoma multiforme |
Fronto-temporal shunt |
| Chen [5] |
M |
41 y |
R |
Meningioma |
Temporal horn to prepontine cistern shunt |
| Kamali [12] |
F |
25 y |
L |
Intraventricular hydatid cyst |
Removal |
| |
|
|
Intraventricular hydatid cyst |
Cyst’s marsupialization |
| Krähenbühl [13] |
M |
15 y |
MH |
Postnatal CNS infection (haemophilus influenza) |
Endoscopic temporal ventriculocisternostomy
followed by ventriculo-peritoneal shunt |
| F |
10 m |
R |
After resection of xanthogranulomatous lesion
(Systemic juvenile xanthogranulomatosis) |
Endoscopic temporal ventriculocisternostomy |
| F |
66 y |
L |
After resection of anaplastic glioma |
Endoscopic temporal ventriculocisternostomy |
| F |
15 y |
R |
After resection of CNS ganglioneuroblastoma |
Endoscopic temporal ventriculocisternostomy |
| Iaccarino [22] |
M |
50 y |
L+R |
Septed temporal horns |
Bitemporal horn-peritoneal shunt |
| Sharma [11] |
F |
22 y |
R |
tuberculous meningitis with
ventriculitis |
Ventriculo-peritoneal
shunt |
| Spallone [25] |
M |
58 y |
L |
Post operative local scarring
(from previous surgery or infection) |
internal temporal-to-frontal shunt followed by
ventriculo-peritoneal
shunt |
| Paredes [19] |
F |
20 y |
L |
Intracranical hemorrhage due to rupture of an AVM |
Ventriculo-cisternostomy |
| F |
5 y |
L |
Intraventricular tumor
(choroid plexus
Carcinoma) |
Ventriculo-cisternostomy
Followed by A closed external ventricular drain (EVD) |
| M |
66 y |
R |
after operation of metastatic intraparenchymal carcinoma |
Ventriculo-cisternostomy |
| M |
73 y |
R |
Tuberculoma mass at right atrium secondary to an atypical mycobacterium |
Removal |
| Ellis [7] |
M |
7 y |
L |
Arachnoid cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| M |
4 m |
L |
Epandymal/Arachnoid cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| M |
2 y |
L |
subepandymal cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| M |
4 y |
L |
Arachnoid cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| M |
26 y |
L |
Cyctic anaplastic astrocytoma |
Cyst fenestration via Endoscopic transoccipital horn approach |
| M |
35 y |
NR |
Postinfectious cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| M |
54 y |
L |
Postinfectious cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| M |
3 y |
R |
Arachnoid cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| M |
5 y |
R |
Archnoid cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| F |
5 y |
R |
Archnoid cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| F |
10 y |
R |
Archnoid cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| F |
5 m |
R |
Archnoid cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| F |
11 y |
L |
Archnoid cyst |
Cyst fenestration via Endoscopic transoccipital horn approach |
| Bohl [2] |
M |
57 y |
R |
Glioblastoma, Post operative edema |
Temporal horn EVD |
| NR |
NR |
NR |
Neoplasm |
External ventricular drain |
| NR |
NR |
NR |
Neoplasm |
External ventricular drain |
| NR |
NR |
NR |
Neoplasm |
External ventricular drain |
| NR |
NR |
NR |
Neoplasm |
External ventricular drain |
| NR |
NR |
NR |
Neoplasm |
External ventricular drain |
| NR |
NR |
NR |
Neoplasm |
External ventricular drain |
| NR |
NR |
NR |
Neoplasm |
External ventricular drain |
| NR |
NR |
NR |
Neoplasm |
External ventricular drain |
| NR |
NR |
NR |
Neoplasm |
External ventricular drain |
| NR |
NR |
NR |
congenital hydrocephalus |
External ventricular drain |
| M |
53 y |
R |
Intraventricular
Hemorrhage, |
Temporal horn EVD (tEVD) subsequently right ventriculoperitoneal shunt |
| NR |
NR |
NR |
Hemorrhage |
External ventricular drain |
| NR |
NR |
NR |
Hemorrhage |
External ventricular drain |
| NR |
NR |
NR |
Hemorrhage |
External ventricular drain |
| NR |
NR |
NR |
Hemorrhage |
External ventricular drain |
| NR |
NR |
NR |
Hemorrhage |
External ventricular drain |
| F |
63 y |
R |
Post operation (evacuation of the intraventricular abscess) |
tEVD |
| NR |
NR |
NR |
congenital hydrocephalus |
External ventricular drain |
| NR |
NR |
NR |
Subdural hematoma |
NR |
| Hana [9] |
M |
60 y |
NR |
Glioblastoma |
combining ventriculo-peritoneal shunt followed by ventriculo-cisternostomy with stent placement |
| Present case |
M |
16 y |
L |
Idiopathic |
Ventriculo-cisternostomy followed by subduro-peritoneal shunt |
NR: Not Reported; M: Male; F: Female; M: Month; Y: Year; L: Left; R: Right; MH: Multiloculated Hydrocephalus, WHO: World Health Organization; CNS: Central Nervous System; AVM: Arteriovenous Malformation; EVD: External Ventricular Drainage; Tevd: Temporal Horn External Ventricular Drainage; VAS: Ventriculo-Atrial Shunt
Table 1: Summary of reported cases from 1947 to 2017.
Etiologically, trapped temporal horn could be outcome of various brain pathologies [2,3,5,6,17,20-22]. Despite description of various surgical approaches from ventriculo-cisternostomy to shunting, there is no standard surgical treatment for this rare condition. To the best of our knowledge, we present the first case of idiopathic unilateral trapped temporal horn.
Case Report
A 16-year-old right-handed adolescent presented with 3 months history of headache along with cranial asymmetry bulging on the left side and mild stuttering. He was alert and motor and sensory systems as well as all cranial nerves were normal on examination. Pupils were equal and normally reacting to light in both eyes. Muscles forces and contour at both sides were symmetrical.
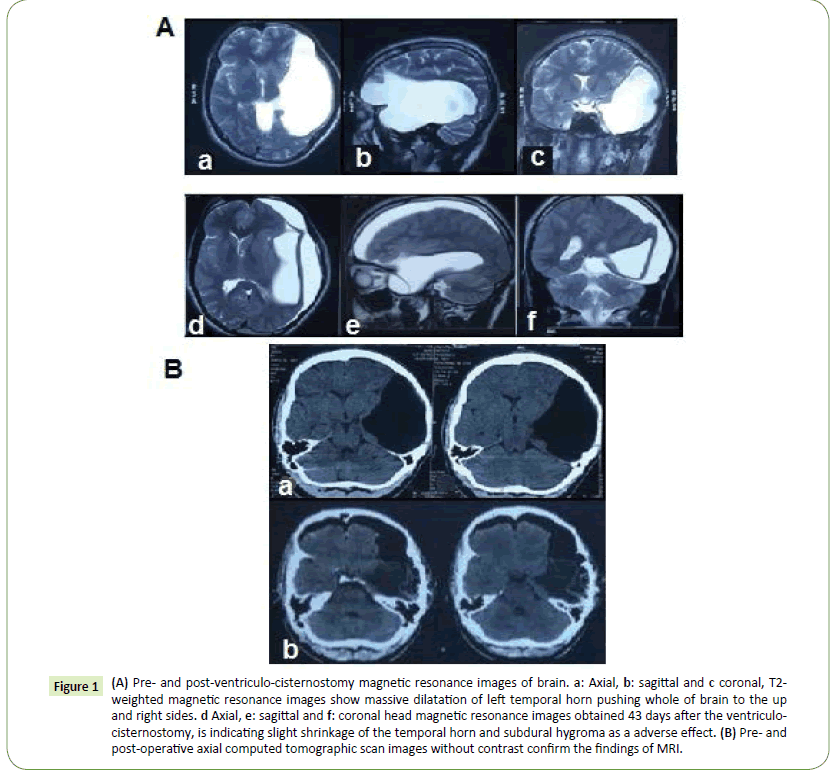
Upon admission, in the computerized tomography (CT), a large left temporo-parietal cystic lesion causing obvious mass effect and midline shift was detected which suggesting subarachnoid cyst as primary diagnosis. In the contrast magnetic resonance imaging (MRI) and Gadolinium-enhanced MRI entrapped temporal lobe was considered due to asymmetric extraordinary enlargement of the temporal horn of the left lateral ventricle (Figures 1A and 1B). Due to the risk of cerebral herniation and/or collapse of frontal horn, in the case of significant midline shift (over 5 mm) surgical intervention is indicated [28]. We did not find a septum between the trapped horn and the atrium of the lateral ventricle to fenestrate endoscopically. With regard to clear evidence of a thinned wall between the temporal horn and basal CSF pathways, in this case of focal obstructive hydrocephalus we adopted a microscopic transtemporal ventriculo-cysto-cisternostomy aiming to avoid a permanent shunt with its subsequent risks of infection and malfunction.
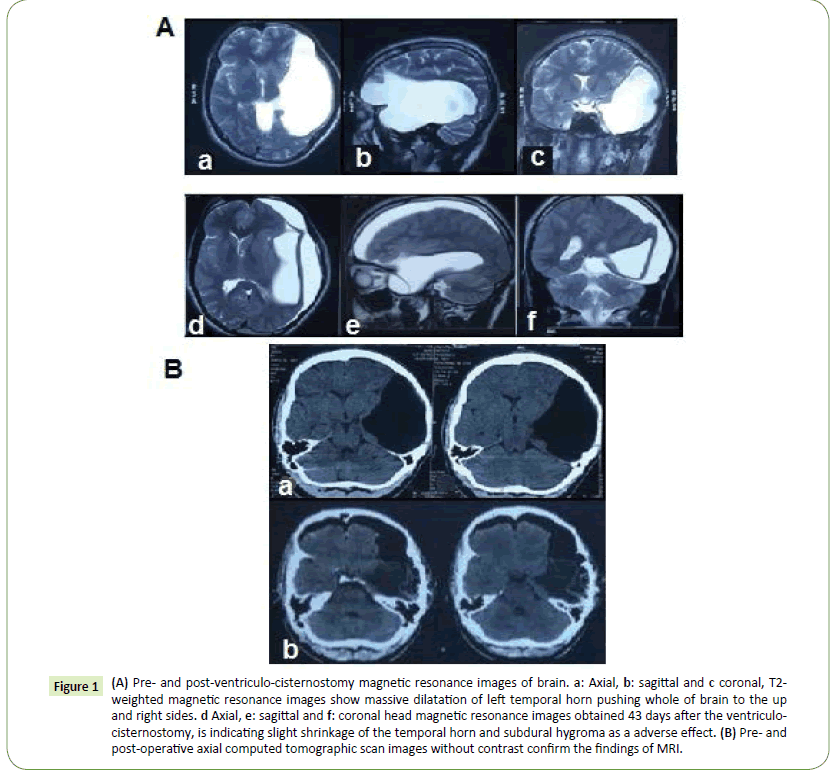
Figure 1: (A) Pre- and post-ventriculo-cisternostomy magnetic resonance images of brain. a: Axial, b: sagittal and c coronal, T2- weighted magnetic resonance images show massive dilatation of left temporal horn pushing whole of brain to the up and right sides. d Axial, e: sagittal and f: coronal head magnetic resonance images obtained 43 days after the ventriculocisternostomy, is indicating slight shrinkage of the temporal horn and subdural hygroma as a adverse effect. (B) Pre- and post-operative axial computed tomographic scan images without contrast confirm the findings of MRI.
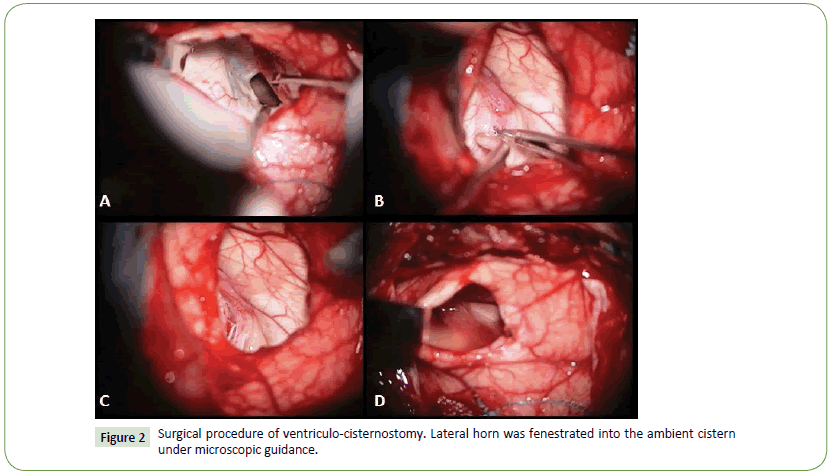
Using functional MRI (fMRI) prior to surgery eloquent cortex was detected to avoid during transgress in order to reach the cyst, especially language areas including the Broca's and the Wernicke's areas. The middle temporal gyrus, safe and non-eloquent, was selected as ideal ventriculo-cisternostomy site after radiologic analysis. Based on neuroimaging review, only possible rout to reach the cistern was the choroidal fissure (Figures 2 and 3).
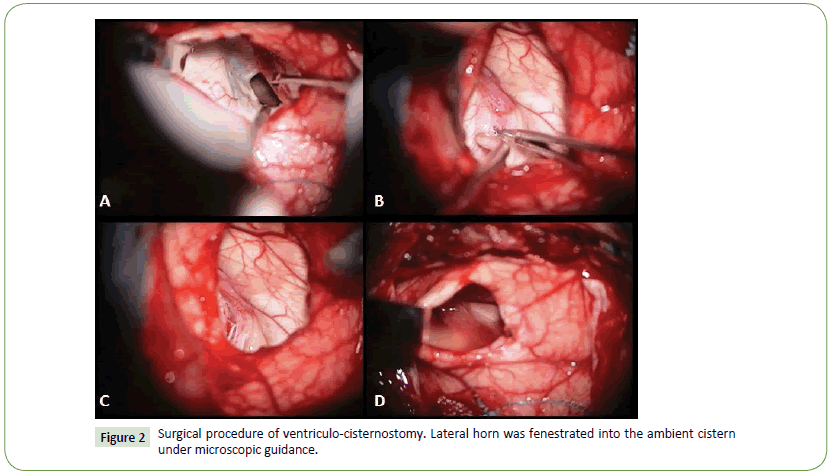
Figure 2: Surgical procedure of ventriculo-cisternostomy. Lateral horn was fenestrated into the ambient cistern under microscopic guidance.
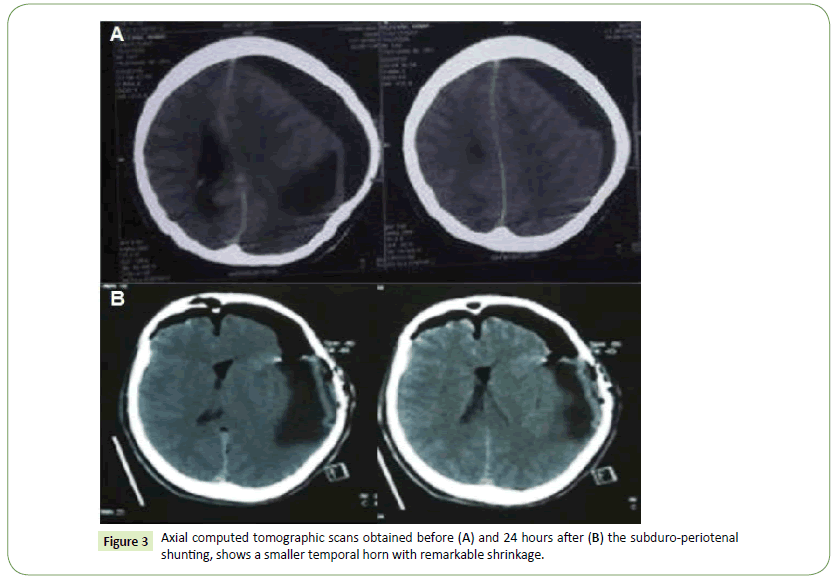
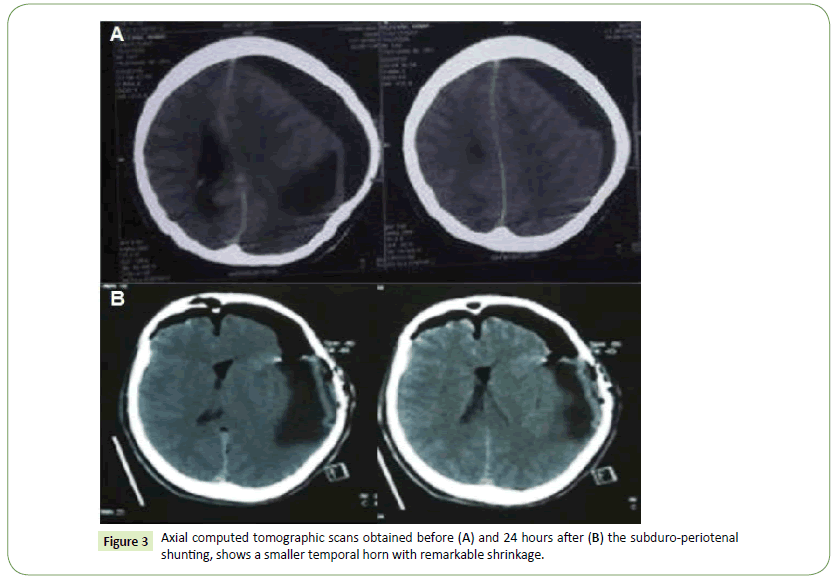
Figure 3: Axial computed tomographic scans obtained before (A) and 24 hours after (B) the subduro-periotenal shunting, shows a smaller temporal horn with remarkable shrinkage.
Patient was placed supine with the head turned to the right side and fixed with a 3-pin Mayfield headholder. After general anesthesia through endotracheal intubation a temporal mini- craniotomy was made. We started with a gradual decompression to avoid possible remote hemorrhage associated with rapid decompression of huge arachnoid cyst. Therefore, an angiocatheter was inserted into the trapped horn and waited 10 minutes to achieve a normal intracranial pressure. After curvilinear incision on dura, 1.5 cm corticotomy on non-eloquent cortex was performed. Evacuation of CSF led to cortical deflation around corticotomy. Since, the only way to access any cisternal point was choroidal fissure, choroidal fissure was dissected under microscopic magnification. Within procedure, compression of ambient cistern made some difficulties in the opening of cistern. Additionally, throughout dissection it was needed being careful about anterior choridal artery and posterior cerebral artery up to crural cistern in front of a capacious CSF space. After establishing good in and outflow of liquid, dura closed, bone flap replaced and wound was closed.
Early post operation course was uneventful excluding to a course of two seizures which were controlled well by sodium valporate. After a few weeks the patient complained of severe headache which starting and aggregating at night in favor of the presence of high intracranial pressure.
A post-operative MRI imaging showed a reduction of trapped horn and the presence of a subdural hygroma in left frontotemporo- parietal areas. Despite our primary decision, persistent annoying headache forced us to implant a shunt. Surgical drainage of the subdural collection was performed with a subduro-peritoneal shunt connecting the left subdural hygroma to the peritoneal space (Figure 3). A month after shunting, subdural hygroma had gradually disappeared and cortex became thicker (Supplementary Figures 1 and 2). Finally, patient was headache free.
Discussion
Since first description of the term ‘entrapment of temporal horn’ by cairn et al in 1947 [3], several cases with different characteristics had been reported (Table 1).
Based on published data, penetrating wounds (n=2), primary or secondary neoplasms (n=17), intracranial hemorrhages (n=10), meningitis and brain abscess (n=9), cystic lesions (n=17, subepandymal, epandymal, arachnoid cysts, intraventricular hydatic cyst etc.), neurosarcoidosis (n=4), benign brain tumors, xanthogranulomatosis (n=2), ventriculitis, postoperative obstruction due to manipulations across or around the foramen of Monro (n=9) and congenital hydrocephalus (n=2) constitute main reasons of this condition [1-27]. Obviously, there is no case with idiopathic etiology among all reported cases. From Table 1, malignant masses as well as cystic lesions take most important part in the etiology of trapped horn. In spite of, these well described etiologies, present case has not any previous history and definite predisposing factor. To our knowledge based on published images of previous cases, this idiopathic case seems be the largest entrapped temporal horn up to the present time.
According to the literature review, removal of obstructing mass (n=8, intraventricular hydatic cyst and etc.), cyst fenestration via endoscopic transoccipital horn approach (n=13, archnoid cysts), endoscopic temporal ventriculo-cisternostomy (n=10) and shunt (n=16) are most common surgical treatments which have been utilized for managing this entity (Table 1). Ventriculoperitoneal shunt was most frequently method applied in 11 cases. Among existing surgical approaches, temporal to frontal horn shunt [18], temporal to prepontine cistern shunt, and temporal horn ventriculo-cisternostomy have been described as less invasive procedures [29].
Intracranial expansive process that distort the dura or intracranial vasculature induce headache by the stretching mechanical stress even in the absence of raised intracranial pressure [30]. Beside patient persistent headache, the presence of significant midline shifts due to the risk of cerebral herniation and/or collapse of frontal horn, is the indication for surgical intervention. Choosing suitable surgical technique for management of the present case was critical. In case of obstructive hydrocephalus, shunt placement or implantation of foreign particles should be avoided because of the risk of infection or failure usually necessitating future revisions [18] and in the context of arachnoid cyst the rate of recovery after shunt is not high. Whenever possible, microscopic or endoscopic reconnection to the CSF pathway should be attempted [18]. In the present case, we preferred microsurgical fenestration and reconnection to the CSF pathway via a mini-craniotomy. Regardless to being functional cortex or not, the left-sided location of lesion in the eloquent cortex of language was the most important consideration in the selecting of this approach. Finally, after planning of surgery, patient underwent to ventriculo-cisternostomy. Two months following ventriculo-cisternostomy, because of persistent fluid collection in subdural spaces and recurrence of headache, subduro-peritoneal shunt was performed.
Conclusion
In the present study we introduced a case of idiopathic and massive unilateral trapped temporal suffering from severe headache. Among possible surgical approaches for reconnection of entrapped temporal horn to the CSF pathway via a microsurgical, ventriculo-cysto-cisternostomy had been preferred. In case of unwanted outcomes such as subdural hygroma, a subduroperitoneal shunt would be a suitable choice.
Conflicts of Interest
The authors declare no conflict of interest.
Authors’ Contributions
Guive Sharifi: Patient surgeon and head of surgical team, provider of data and idea of case report
Department of neurosurgery, Loghman e Hakim Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Tahereh Gahdiri: Preparation of manuscript, corresponding author for submission and revision
* Department of Neuroscience, Faculty of Advanced Medical Sciences, Tabriz University of Medical Sciences, Tabriz, Iran AND Neuroscience Research Center, Tabriz, Iran
Gelareh Vakilzadeh: Reviewing of manuscript and preparing images
Shefa Neuroscience Research Center, Khatamolanbia Hospital, Tehran, Iran
Davide Nasi: Reviewing and revising of manuscript
Department of Neurosurgery, Institute for Scientific and Care Research "ASMN" of Reggio Emilia, Reggio Emilia, Italy
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
We would like to thank Prof. Nader-Afshar Fereydoonian for his critical review of the manuscript
Consent
Written consent from the patient has been obtained for publication and teaching.
20773
References
- Berhouma M, Abderrazek K, Krichen W, Jemel H (2009) Apropos of an unusual and menacing presentation of neurosarcoidosis: The space-occupying trapped temporal horn. Clin Neurol Neurosurg 111: 196-199.
- Bohl MA, Almefty KK, Nakaji P (2015) Defining a standardized approach for the bedside insertion of temporal horn external ventricular drains: Procedure development and case series. Neurosurgery 79: 296-304.
- Bruck W, Sander U, Blanckenberg P, Friede RL (1991) Symptomatic xanthogranuloma of choroid plexus with unilateral hydrocephalus. Case report. J Neurosurg 75: 324-327.
- Cairns H, Daniel P, Johnson RT, Northcroft GB (1947) Localized hydrocephalus following penetrating wounds of the ventricle. Br J Surg 55: 187-197.
- Chen CC, Kasper EM, Zinn PO, Warnke PC (2011) Management of entrapped temporal horn by temporal horn to prepontine cistern shunting. World Neurosurg 79: 404-410.
- Coria F, Bahillo ME, Moral BM, Garcia GP, Ortiz Saenz de SantaMaria R (2000) Late-onset isolated gelastic epilepsy secondary to entrapment of the right temporal horn. Neurologia 15: 204-207.
- Ellis JA, McCormick PC, Feldstein NA, Ghatan S (2015) Transoccipital endoscopic fenestration of atrial cysts causing ventricular entrapment. J Neurosurg Pediatr 15: 567-572.
- Hamada H, Nonaka Y, Kusaka Y, Nakazaki H, Abdullah SH, et al. (2006) Huge arachnoid cyst incorporating choroid plexus. Childs Nerv Syst 22: 420-423.
- Hana T, Tanaka S, Shin M, Mukasa A, Kugasawa K, et al. (2015) Neuroendoscopic ventriculocisternostomy with stent placement for trapped temporal horn after the resection of glioblastoma. World Neurosurg 84: e2075-2078.
- Hervey-Jumper SL, Ziewacz JE, Heth JA, Sullivan SE (2009) Frontal-to-temporal horn shunt as treatment for temporal horn entrapment. J Neurosurg 112: 410-413.
- Iaccarino C, Romano A, Ramponi V, Nasi D, Maggi M, et al. (2013) Entrapment of temporal horn: First case of bilateral occurrence and review of literature. Clin Neurol Neurosurg 115: 2207-2212.
- Kamali NI, Huda MF, Srivastava VK (2011) Intraventricular hydatid cyst causing entrapped temporal horn syndrome: Case report and review of literature. Trop Parasitol 1: 113-115.
- Krahenbuhl AK, Baldauf J, Gaab MR, Schroeder HW (2013) Endoscopic temporal ventriculocisternostomy: An option for the treatment of trapped temporal horns. J Neurosurg Pediatr 11: 568-574.
- Kuiper EJa WPV (2001) Trapped third ventricle. Acta Neurochir (Wien) 143: 1169-1172.
- Lyngdoh BT, Giri PJ, Behari S, Banerji D, Chhabra DK, et al. (2007) Intraventricular meningiomas: A surgical challenge. J Clin Neurosci 14: 442-448.
- Maurice-Williams RS, Choksey M (1986) Entrapment of the temporal horn: A form of focal obstructive hydrocephalus. J Neurol Neurosurg Psychiatry 49: 238-242.
- Maurya P, Singh VK, Prasad R, Bhaikhel K, Sharma V, et al. (2007) Intraventricular hydatid cyst causing entrapped temporal horn syndrome: A case report and review of literature. J Pediatric Neurosci 1: 20-22.
- Ofori-Kwakye SK, Wang AM, Morris JH, O'Reilly GV, Fischer EG, et al. (1986) Septation and focal dilatation of ventricles associated with cryptococcal meningoencephalitis. Surg Neurol 25: 253-260.
- Paredes I, Orduna J, Fustero D, Salgado JA, de Diego JM, et al. (2016) Endoscopic temporal ventriculocisternostomy for the management of temporal horn entrapment: report of 4 cases. J Neurosurg pp: 1-6
- Parrent AG (2000) Endoscopically guided fenestration of the choroidal fissure for treatment of trapped temporal horn. J Neurosurg 93: 891-894.
- Schlitt M, Duvall ER, Bonnin J, Morawetz RB (1986) Neurosarcoidosis causing ventricular loculation, hydrocephalus, and death. Surg Neurol 26: 67-71.
- Sharma C, Acharya M, Kumawat BL, Kochar A (2014) Trapped temporal horn of lateral ventricle in tuberculous meningitis. BMJ Case Rep.
- Singh SK, Srivastava C, Ojha BK, Chandra A, Parihar A, et al. (2010) An unusual cause of entrapment of temporal horn: Neurocysticercosis. Neurol India 58: 814-815.
- Smith H, Moody D, Ball M, Laster W, Kelly DL Jr, et al. (1979) The trapped temporal horn: A trap in neuroradiological diagnosis. Neurosurgery 5: 245-249.
- Spallone A, Belvisi D, Marsili L (2015) Entrapment of the temporal horn as a cause of pure wernicke aphasia: Case report. J Neurol Surg Rep 76: e109-112.
- Tsugane R, Shimoda M, Yamaguchi T, Yamamoto I, Sato O (1992) Entrapment of the temporal horn: A form of focal non-communicating hydrocephalus caused by intraventricular block of cerebrospinal fluid flow-report of two cases. Neurol Med Chir (Tokyo) 32: 210-214.
- Watanabe T, Katayama Y (1999) Evaluation by magnetic resonance imaging of the entrapped temporal horn syndrome. J Neurol Neurosurg Psychiatry 66: 113.
- Miller JD (1977) Significance of intracranial hypertension in severe head injury. J Neurosurg 47: 503-516.
- Yamamoto H, Matsukado Y, Nagahiro S (1987) Entrapment of the temporal horn which developed during antibiotic therapy for multiple brain abscess. Shoni No Noshinkei 12: 415-421.
- Manet R (2016) Intracranial hypertension is painless. Acta Neurochir Suppl 122: 275-277.