Keywords
COVID-19; Australia; New Zealand; Indonesia; Response
Background
At the end of 2019, a new pneumonia disease caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-20) was first spreading in Wuhan, China, and has continued to spread throughout the world [1]. On 11 March 2020, the World Health Organization (WHO) declared COVID-19 to be a pandemic. It is also understood that COVID-19 is a serious public health threat of the decade [2]. According to the WHO report [3], more than 80 million COVID-19 cases and more than 1.9 million deaths were reported by 12 January 2021. The epidemiological situation is variable across regions: Americas (38 861 668 cumulative cases and 910 741 deaths), Europe (28 797 583 cumulative cases and 626 804 deaths), South-East Asia (12 257 684 cumulative cases and 187 786 deaths), Eastern Mediterranean (5 149 132 cumulative cases and 124 836 deaths), Africa (215 878 cumulative cases and 47 905 deaths), Western Pacific (1 184 662 cumulative deaths and 21 119 deaths) [4]. Overall, the Americas region continues to be the region with the heaviest COVID-19 burden. The Europe region is the second most affected region and accounts for 10% and 6% of newly reported cases and deaths respectively. On the contrary, the cumulative cases in the Western Pacific Region are the lowest, accounting for 1% of global cases and 1% of all deaths [5].
We think that it is important to analyze this variable pattern of the pandemic across countries in order to better understand the epidemic and the response to it. The gaps in understanding and controlling COVID-19 between high-burden and low-burden countries were identified by analyzing their response and different epidemic situation. We will be using three countries in the Indo-pacific region which have different epidemic patterns: Indonesia had 882 418 cases and 25 484 deaths as of 12 January 2021 (the first case was reported on 2 March 2020), Australia had 28 669 cases and 909 deaths as of 12 January 2021 (the first case was reported on 25 January 2020), and New Zealand had 2 246 cases and 25 deaths (the first case was reported on 28 February 2020). The objective of this paper is to analyze the epidemic of COVID-19 and explain the variable expression of the epidemics in Australia, New Zealand and Indonesia.
Methods
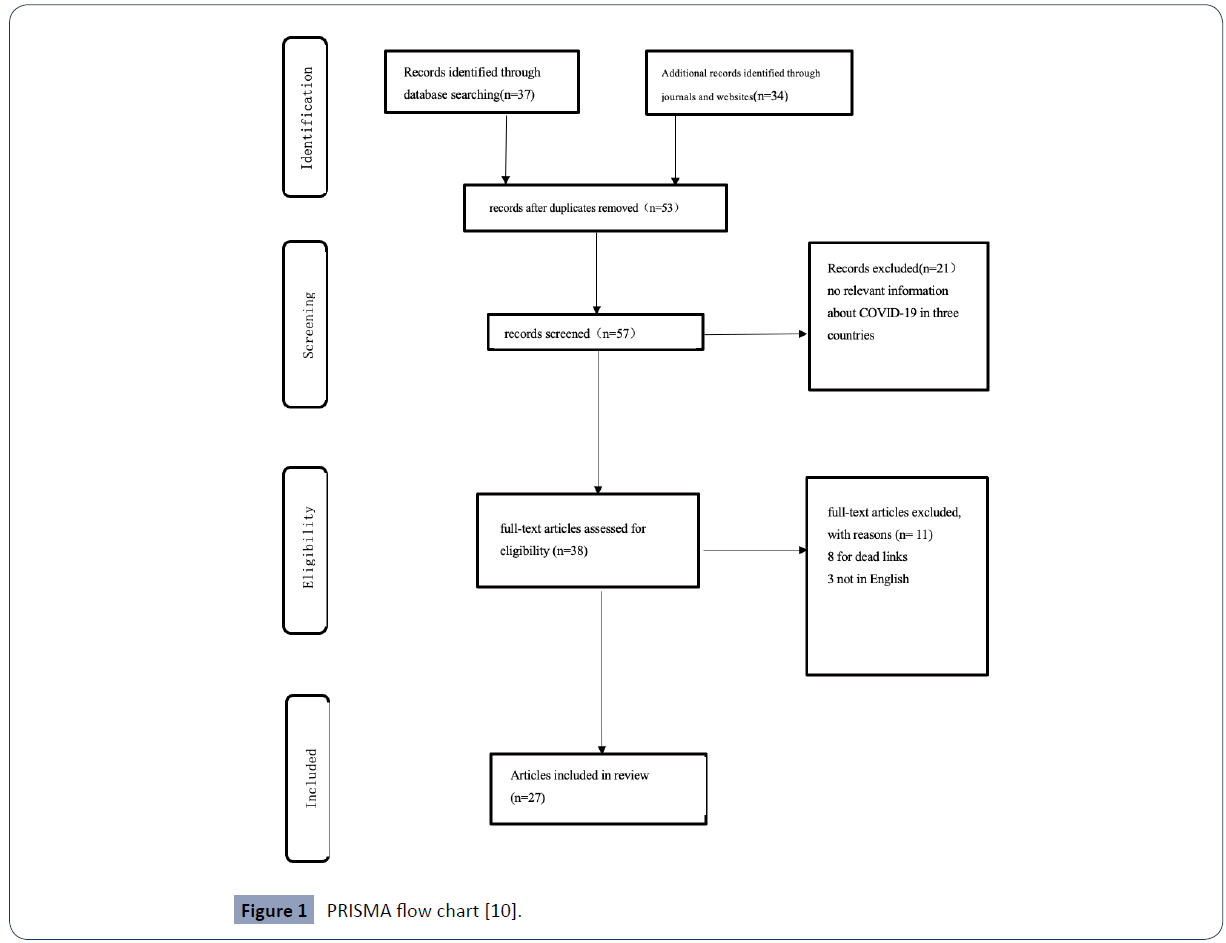
We used a mixed-methods study design, including a quantitative method to analyze the epidemics in Australia, New Zealand and Indonesia and a scoping review to identify the factors that may explain the heterogeneity of the epidemic in these countries [6]. The procedures of screening and selection of eligible studies were presented using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis [PRISMA] flow diagram.
We conducted our search in the following databases: PubMed, Google Scholar, Medline, Scopus. We applied the following keywords: [coronavirus OR COVID-19 OR SARS-CoV-2] and [Indonesia OR Australia OR New Zealand] and [response OR strategy OR interventions OR risks] [Title/Abstract]. We included papers published from January 2020 to January 2021.
Eligibility criteria
Articles that met the following criteria were included: (1) Australia’s strategy in response to COVID-19; (2) New Zealand’s strategy in response to COVID-19; (3) Indonesia’s strategy in response to COVID-19; (4) COVID-19 risks in Australia; (5) COVID-19 risks in New Zealand; and (6) COVID-19 risks in Indonesia. We also used Google search engine in order to broaden the scope and search for more information. The review includes all papers based on qualitative, quantitative, and mixed studies. The review is limited to papers published in English.
Article selection and data extraction
Articles that meet the inclusion criteria are selected using the above inclusion criteria. Finally, we extracted data from the selected articles on the following: national information, research types, key findings, and conclusions. All retrieved studies were initially imported into the Endnote library to assist in removing the duplicates.
A three-stage screening process was used to eliminate non-relevant articles at the stage of title, abstract, and full text-screening. Finally, the full texts of all relevant studies found to meet the inclusion criteria were retained for the final synthesis [7].
Data were extracted from eligible articles using a customized data extraction Microsoft excel spread sheet format. The format contained the name of the first author, year of publication, title of the article, study design, study location [country], and key findings of the article. The review findings were mapped and interpreted in line with the review objectives. We used a comparative framework to compare and contrast the response to COVID-19 in the three countries [8]. A narrative synthesis was employed.
Results
The table below presents the data on the total number of confirmed cases and deaths, hospitalization rate, death rate, the number of people tested per million among the three countries. As of 12 January 2021 (Table 1), the number of total cases is 882 418 in Indonesia, 28 669 in Australia and 2 246 in New Zealand. The number of total deaths is 25 484 in Indonesia, 909 in Australia and 25 in New Zealand. There were: 3 208 cases, 93 deaths and 29 833 tests per 1 000 000 in Indonesia; 1117 cases, 305 deaths and 479 969 tests per 1 000 000 in Australia; and, 449 cases, 5 deaths and 29 833 tests per 1 000 000 in New Zealand. The case fatality rate of New Zealand is relatively low with 0.2%. The testing rate is relatively higher in Australia (479 969 per 1 000 000) than in New Zealand (291 293 per 1 000 000) [9-17].
| |
Total cases |
Total cases per
1 000 000 |
Total deaths |
Total deaths per
1 000 000 |
Hospitalization rate |
Case Fatality rate |
Total tests |
Tests per
1 000 000 |
| Australia |
28 669 |
1 117 |
909 |
35 |
9.6% |
3.1% |
12 327 753 |
479 969 |
| New Zealand |
2 246 |
449 |
25 |
5 |
5.9% |
0.2% |
1 457 076 |
291 293 |
| Indonesia |
882 418 |
3 208 |
25 484 |
93 |
5.0% |
2.9% |
8 206 401 |
29 833 |
Source from: Australian Government Department of Health report [9].
Table 1 COVID-19 in Australia, New Zealand, Indonesia, 12 January 2021.
| Country |
Overall strategy |
community engagement |
Health system capacity |
Public-health capacity |
Strategies for border closure |
| Australia |
Three-step framework |
Keep 1.5m social distance in public; Maintain good hand hygiene?mandatory mask order in VIC, NSW,QLD |
Current health capacity was under control.
increase ICU beds and ventilators? |
Tests can be done in private and public sector laboratories; 479 969 tests per 1 million; not well in quarantine and contact tracing |
Border closed to visitors since 20 March.
All arrivals need to be quarantined for 14 days. |
| New Zealand |
Four-level alert system |
Keep 1.5m social distancing.
Keep basic hand hygiene.
Keep good contact tracing of community.
Adopt stricter protection measures for the elderly |
Hospitals and ICUs are well under capacity? Conduct training of medical personnel? |
The capacity is under control; conduct 291 293 per 1million tests. |
Border closed to visitors since 19 March.
All arrivals need to be quarantined for 14 days. |
| Indonesia |
Suppress COVID-19 but keep some economic open |
Wash hands with soap; People with symptoms wear masks.
Keep 1-2M social distance. |
a shortage of workforce? medical staff are under great pressure ?the capacity of hospitals and ICUs is low |
designate 48 laboratories nationwide for COVID-19 diagnosis; most laboratories have not yet been put into use.
only conduct 29 833 tests per 1 million: not well in contact tracing |
Indonesia's border closure policy began on 2 April 2020.
All arrivals need to be quarantined for 14 days. People with special visas can enter the border after submitting a health certificate. |
Table 2 Summarize the review and findings [11-17].
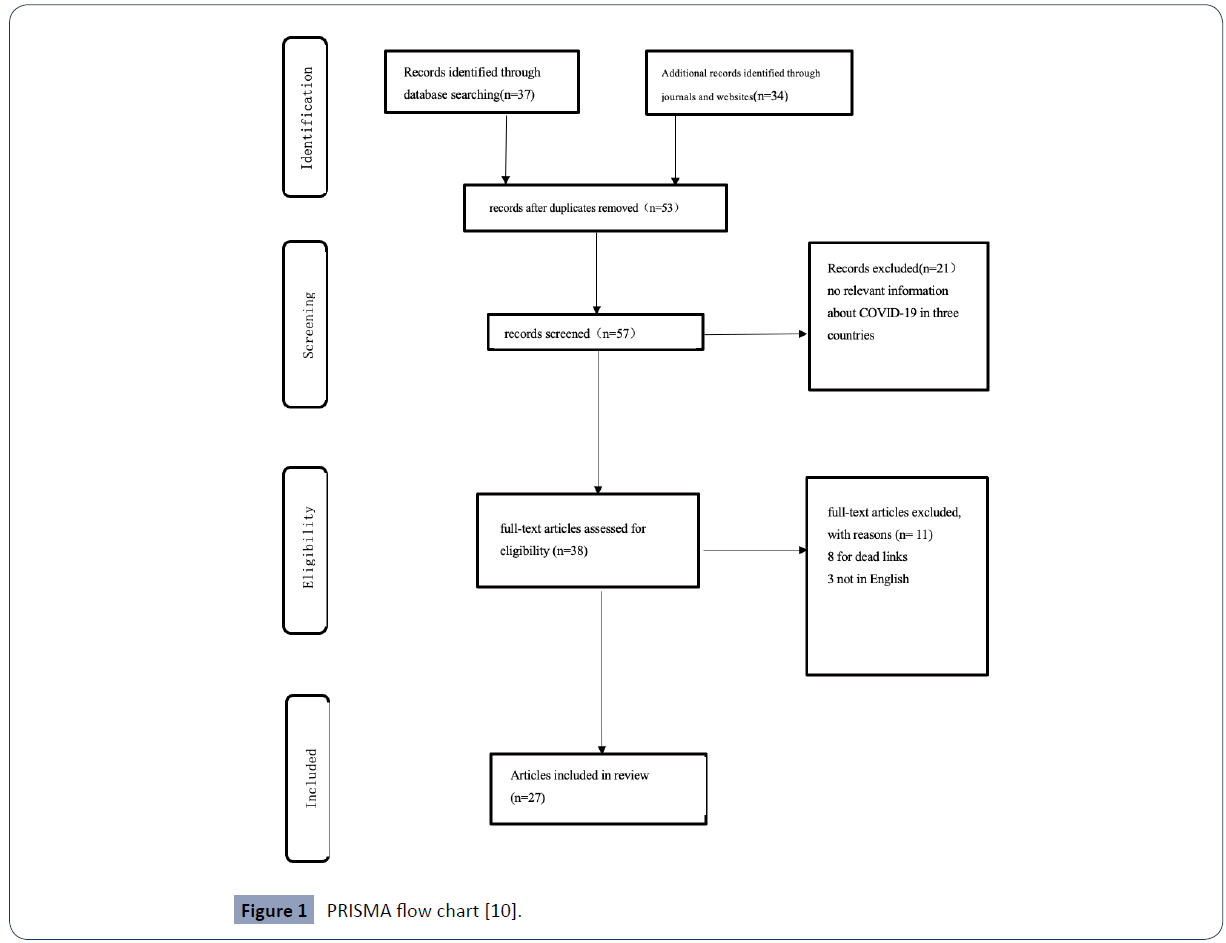
Figure 1 PRISMA flow chart [10].
Characteristics of included studies
The procedures of screening and selection of eligible studies were presented using the PRISMA flow diagram. There were 71 articles in the initial search. After duplicates were removed, a total of 57 articles were left. Eight articles were excluded for dead links and three articles were removed because they were not in English. 27 papers are highly related to analyzing COVID risks or strategies in Indonesia or Australia or New Zealand.
All of the articles were published in 2020. Thirteen articles were describing Indonesia's challenges facing the SARS-CoV-2 and how it responded to it. Out of these, twelve articles mainly criticize Indonesia’s inadequate response to the pandemic. One article describes both Australia's and Indonesia's epidemiological situation. Australia's response to COVID-19 was included in five articles. Four articles provided an in-depth analysis of New Zealand's policies and the reasons why it was successful in the pandemic. The rest of the article introduced the epidemiology of New Zealand and Australia and the success of their responses.
The scoping review identified a number of themes (community engagement, public health capacity, health systems, and governance) that can explain the variability of the epidemic in these three island states. Review findings were included.
Community engagement
Community engagement is the key to containing the COVID-19 epidemic [18]. Social distancing is a common public health measure to slow the spread of infectious diseases from person to person. In Indonesia, people were encouraged to keep a social distancing of 1-2m. Besides, other precautions, such as washing hands with soap and tap water regularly and wear masks, were advocated [19]. However, it is hard to keep social distancing in Indonesia [20].
On the other hand, in New Zealand and Australia, people have been maintaining a social distancing of 1.5m, practice good hand hygiene and wearing masks. Reports showed that more than 80 percent of people complied with the social distance measure. Besides, New Zealand and Australian citizens have a high level of trust in the government [21]. A survey showed that almost 90% of New Zealanders and Australians believe that the government can make the right decision on the COVID-19 pandemic, which also allows New Zealand and Australia to obtain a high degree of community cooperation [22].
People were also self-isolate if they have symptoms of cold or flu in New Zealand. In addition, New Zealand has adopted stricter protection measures for the elderly [23]. The elderly were required to stay at home, and many aged care facilities across the country have restricted visits since mid-March [24].
Health system capacity
The higher case fatality rate in Indonesia is due to the extremely limited medical resources [25]. According to the latest data from the Indonesian Ministry of Health, Indonesia has only 309 100 hospital beds, most of which are located on the island of Java [26]. Besides, there are fewer than 6 000 intensive care unit (ICU) beds nationwide. This means that Indonesia has only 2.7 ICU beds per 100 000 people, one of the countries with the lowest rate of hospital beds in Asia [17]. At the same time, mechanical ventilators are not widely used in rural areas [27]. Besides the medical workforce was under significant pressure. The staff needs to conduct long-time and intensive work. Many mild cases could not be treated effectively and turned into severe cases, causing more deaths in Indonesia [15].
Adequate medical resources have kept the hospitalization rate and case fatality rate at a lower level in New Zealand and Australia. Australia has 191 intensive care units and 2 378 intensive care beds [9.4 per 100 000 people]. Australia added 4 258 intensive care beds and 2 631 invasive ventilators after the onset of the pandemic. This may require an additional 4 092 senior doctors and 42 720 registered ICU nurses [28]. In New Zealand, there are approximately 4.6 intensive care beds per 100 000 people [29]. By July 2020, 552 intensive care unit beds were available in New Zealand. Hospitals and intensive care units across the country have carried out a lot of work to prepare for the influx of patients [30]. There were many aspects to this plan; many units have rearranged their roster, formed new teams including ICU and non-ICU staff, formulated new agreements, and conducted hours of meetings and teaching activities to the professional staff [31].
Indonesia has only 4.27 doctors per 10 000 people and 24.1 nurses per 10 000 people while 32.7 doctors per 10 000 and 15.5 nurses per 10 000 in Australia and 35.9 per 10 000 and 124.5 nurses in New Zealand [32]. The medical staff in Indonesia experienced long working hours, overcrowded hospitals, lack of personal protective equipment [33].
Public health capacity
The testing rate for coronavirus in Indonesia was extremely low. In Indonesia, tests for coronavirus were usually performed in people who have symptoms. Patients who do not meet the eligibility criteria for free testing have to pay, costs ranging from 1.5 million rupees to 2.5 million rupees per test- which made it more difficult for many people to get access to tests [34]. Therefore, a mass of asymptomatic or mildly symptomatic cases cannot be detected in Indonesia.
Another reason for low testing is that Indonesia's health infrastructure, especially health laboratories, has been one of the weakest components of the health system [35]. The spread of COVID-19 has exposed the gaps in these health infrastructures. Currently, the Ministry of Health of Indonesia only designated 48 laboratories nationwide for COVID-19 diagnosis [36]. This means that 12 of the 34 provinces in Indonesia do not have COVID-19 diagnostic laboratory facilities. Of the 44 laboratories contacted, 36 (82%) responded to the survey; 11 were surveillance laboratories and 25 were non-surveillance laboratories. At the time of the investigation, only 13 laboratories tested SARS-CoV-2 specimens: seven out of 11 monitoring laboratories, and six out of 25 non-monitoring laboratories [16]. The investigation report showed that the laboratory lacked reagents and equipment, especially the limited workforce. Due to the lack of equipment and materials, most laboratories have not yet been put into use. In terms of equipment, in 36 COVID-19 diagnostic laboratories, there are 38 real-time polymerase chain reaction (RT-PCR) machines [37]. The daily testing capacity of 44 diagnostic laboratories is 2 544 specimens.The detection rate of COVID-19 was one of the lowest in the world. Besides, contact tracing in Indonesia seemed to be a huge gap because of insufficient staff, inadequate cooperation, and disease stigma. Among confirmed or suspected cases, only 53.7% received contact tracing [38].
On the other hand, Australia’s testing capacity is sufficient to meet possible needs. PCR testing is widely carried out in private and public sector laboratories [39]. New Zealand testing laboratories have been working hard to provide SARS-CoV-2 testing for the New Zealand public. New Zealand was expected to conduct at least 30 000 tests per week, including mandatory boundary tests. New Zealand used digital software for contact tracking, which reduces the possibility of recording errors and improves the efficiency of tracing [40].
The higher number of cases in Australia is due to the failure of hotel quarantine in Victoria, which has led to the second wave in Australia [41]. Approximately 90% of confirmed cases in Victoria can be traced back to quarantine hotels. More catastrophically, Australia failed to track contacts after the outbreak of the second wave. As of January 12, there were 28,689 cases, but the unknown contact cases accounted for 15.4% which reflected that the contact tracing was not adequate [30]. On the other hand, the surveillance and contract tracing system were overwhelmed, with thousands of cases diagnosed every day during the peak period [42].
Border closure
Closing the border is a common measure taken by most countries to cope with the increasingly fiercepandemic [43]. Evidence suggested that the Indonesian government responds to COVID-19 slowly [44]. Until the first confirmed cases on 2 March, the Indonesian government had no obvious signs that it was accelerating its response to COVID-19 and Indonesia's border closure policy began on 2 April 2020 which indicated it had missed key points to prevent COVID-19 from an outbreak [45]. The death rate from COVID-19 in Indonesia ranked second in the world. Although the number of coronavirus cases and virus-related deaths continued to rise, the government has been reluctant to implement lockdowns across the country to reduce mortality and prevalence [46]. Although the national police have ordered the closure of large-scale religious activities as well as sports and entertainment activities. However, Jakarta, which has the highest death rate, has not officially imposed a curfew [47].
Compared with Indonesia, Australia and New Zealand announced strong border closure measures to block viruses on 20 March at the beginning of the pandemic [48]. However, New Zealand has implemented stricter border closures than Australia. In February, New Zealand imposed entry restrictions on travelers from multiple COVID-19 hotspots. When New Zealand's cases began to increase significantly in early March, the government completely closed the country on March 23 [49]. Australia’s initial response wanted to keep social distance restrictions but keep the economy open, but New Zealand introduced a new four-stage alert system, whichaimed to eliminate the epidemic in the country [50].
Besides, New Zealand has the advantage of demographic isolation compared with Australia, which is beneficial that there are fewer early travelers from China and other epidemic hotpots. It is located 2 500 miles east of Australia, and its nearest neighbor is the New Caledonia Chain of Islands, 1 200 miles north [51]. Australia is an island country between the Pacific and Indian Oceans with frequent association with hot spots of COVID-19 in Asia, Europe, and North America [52]. So, the time before cases start to appear is longer and the number of cases is relatively low. When New Zealand had its first case on 28 February, community transmission had already occurred in Australia [53].
The practice of non-healthy behavior in Indonesia may cause more cases and deaths due to COVID-19. More than 76% of adult males in Indonesia are smokers, which accounted for the highest percentage in the world [54]. People who smoke are believed to be more susceptible to COVID-19 and are at increased risk of severe respiratory complications because of the high risk of lung inflammation [55,56]. High hospitalization and fatality rate were also associated with its poor air quality. Indonesia’s air quality was considered moderately unsafe [57]. Polluted air is a common cause of acute respiratory diseases [58]. In this polluted environment, smoking and malnourished Indonesian are more likely to get more serious respiratory diseases [59].
Population density is also one of the reasons for the high number of cases and deaths. The population density of Indonesia is 50 times that of Australia (151 per Km2vs.3.2 per Km2) and 10 times that of New Zealand (151 per Km2 vs.15 Km2) [60]. Indonesia’s high population density also means that it could be easier for the virus to spread through close contact and breathing droplets in the air and will cause more people to be infected. Jakarta, the largest city in Indonesia has a population of 9.608 million, and its population density is more than 33 times that of Sydney which is the biggest city in Australia [61].
Multisectoral-factors
In Australia, the Minister of Finance announced the 2020 Budget Strategy which supplemented the preliminary work in response to COVID-19. Supporting public services, fighting the COVID-19 epidemic were the key priorities of the strategy [62]. Australia has implemented programs such as Jobkeeper and Jobseeker [63].These are programs to support businesses and non-profit organizations affected by Covid-19 so as to help more Australians stay at work. Meanwhile, the government has announced a series of measures to help renters, including waiving some rents and tax relief [64].
The New Zealand government has introduced a wage subsidy to protect vulnerable companies. At the same time, for small and medium-sized enterprises, the government has also launched an enterprise financing guarantee scheme to protect jobs and support the economy [42]. Besides, the New Zealand government has introduced an employer wage subsidy scheme to retain the workforce. In the community, reduce the increase of residential rent to protect the rights of tenants [30].
In order to mitigate the social consequences of the epidemic and the blockade, the Indonesian Government had initiated relief measures for the poor and small businesses [15]. The government has issued ration cards and waived some electricity bills [16]. To ease the pressure on small and medium-sized businesses, the government's aid package includes subsidized loans and taxation reduction [44].
Discussion
Australia and New Zealand have demonstrated their resilience in the war against the epidemic of COVID-19 much better than many other high-income countries. This is possible due to good leadership and governance of the response, community engagement, public health systems capacity and multi-sectoral actions. Compared with Indonesia, Australia and New Zealand have implemented a strict border closure policy, practiced stricter public health activities, performed massive testing to slow the spread of COVID-19 and provided sufficient medical services with minimal burden on the health system. Therefore, it is not surprising to find that cases and deaths are low in Australia and New Zealand while they continue to rise in Indonesia.
The strategies and interventions in Australia and New Zealand are also being implemented by other countries around the globe and have also benefited them in the prevention and control of COVID-19. Thailand has performed intensely in responding to this pandemic. As of 21 August, there were only 3 390 confirmed cases and 58 deaths, which was a very low number. The key to Thailand's successful containment of the epidemic lies in the widespread use of testing and ensuring adequate medical services [65]. Meanwhile other Asian countries including China, South Korea, Japan provided fast, effective, and timely responses [66]. China's early response and measures, such as monitoring and early reporting, and large-scale surveillance, have successfully reduced the epidemic in China and the epicenter of Wuhan [67]. Japan succeeded in mitigating the catastrophic harm of COVID-19 in the early stage. Japan’s adequate medical system, good personal hygiene habits, and high citizen compliance are the reasons for successfully reducing the impact of the COVID-19 epidemic [68]. The well-functioning national medical insurance system, sufficient human resources, and infrastructure have allowed South Korea to respond very decisively to the epidemic [69,70].
On the other hand, there are countries which have inadequate response have been hugely affected by the COVID-19 pandemic. The United States is one of the countries which are unsuccessful in their response. The United States has the epidemic with the highest number of confirmed cases in the world. Their slow initial response to the outbreak was to blame. The number of tests in the United States was still far behind other successful countries. According to data provided by "Our World in Data" [71], the number of tests per 1 000 000 in Denmark was twice that of the United States, but the number of confirmed cases was by far less than half that of the United States. The United States is not the only country that has been hit badly by COVID-19 [72]. Countries such as the United Kingdom are also hugely affected by the pandemic despite their high Global Health Security index (GHS index) [73]. The countries with the highest GHS index were the countries that were most affected by COVID-19 [74]. These countries have been hit severely by COVID-19 because they all missed the prime time to control the epidemic- the initial moment. The severity of the epidemic also seems to be more obvious in Brazil and India because of their extreme inequality within the countries in addition to their low level of preparedness for GHS [75].
Inequalities can also explain the epidemic in Indonesia, where women, especially poor women, suffered most. Existing gender inequality puts women at greater risk of contracting the coronavirus. In Indonesia, where men are preferred, women used public transportation more frequently than men because many women do not have their own vehicles [76,77]. When restrictions are relaxed and commuting began to return to normal, it will put female workers at greater risk of infection. Generally speaking, the poor in Indonesia rarely have the opportunity to go to the hospital. However, the proportion of poor women seeking medical care was lower than that of poor men (6.2% and 7%, respectively) [78]. In 2019, the living conditions of female-headed households are worse than those of male-headed households. These women and their families lived in limited clean water, poor sanitation and limited space [79]. This made it difficult or impossible for them to maintain social distance and puts them at risk of COVID-19 infection [80,81].
The blockade of the epidemic has caused countless losses to Australia, and the economy is the first to bear the brunt which led to the worsening of equality [82]. The impact of the unemployment wave was reflected at the end of the income spectrum most. The income of front-line workers was very low, while white-collar workers can work safely at home. Low-income workers in first-line industries were more likely to live in crowded accommodation environments, which increased the risk of transmission [83]. The public health response to the blockade hurts the poor most. Young people who depended on temporary workers lost their livelihoods and their education was interrupted. Women have also suffered disproportionate losses—unemployment, the increasing burden on childcare [84]. People without permanent residency were excluded from public support programs such as Job Seeker and Job Keeper. In order to alleviate these inequalities, Australia has adopted many social protection measures, including reductions in electricity bills and taxation [85].
This study has outlined the common measures of countries that have successfully responded to the epidemic as a window to strengthen the control of the pandemic. It has found the factors that explain the variability of the epidemics by analyzing successful strategies in response to COVID-19. High-burden countries can learn good experiences and methods to successfully curb their epidemics [86-105].
The study has the following potential limitations: (1) all published reports and paper may not be included in the database search; (2) data was only collected until the end of January, but the number of COVID-19 cases was changing quickly; (3) grey literature is not included in the review; and (4) quality assessment was not conducted in this research.
Conclusion
Australia and New Zealand have demonstrated a strong response to COVID-19. Analysis of the measures in these successful countries revealed that some measures have enabled them to control the epidemic: implementation of strict public health response, provision of sufficient medical services, good public communication are key to reduce the spread of the virus, and good governance and social protection measures. These are important lessons countries, such as Indonesia, can learn and adapt them to their context, and be able to control their epidemics.
Declarations
Ethics approval and consent to participate: Not applicable
Consent for publication: Not applicable
Availability of data and materials: The datasets generated and/ or analyzed during the current study are available in the https://covid19.who.int/table
Competing interests: Non-financial competing interests
Funding: Not applicable
Authors' contributions: Not applicable
Acknowledgements: Not applicable
36550
References
- Di Gennaro F, Pizzol D, Marotta C, Antunes M, Racalbuto V, et al. (2020) Coronavirus diseases (COVID-19) current status and future perspectives: a narrative review. Int J Environ Res Public Health 17:2690.
- Kannan S, Ali PSS, Sheeza A, Hemalatha K(2020) COVID-19 (Novel Coronavirus 2019)-recent trends. Eur Rev Med Pharmacol Sci24:2006-2011.
- Peters M, Godfrey C, McInerney P, Soares C, Khalil H, et al. (2015) Methodology for JBI scoping reviews. In: The Joanna Briggs Institute reviewers' manual.
- Dixon-Woods M(2011) Using framework-based synthesis for conducting reviews of qualitative studies. BMC Med 9:39.
- Han E, Tan MMJ, Turk E, Sridhar D, Leung GM, et al. (2020) Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet 396: P1525-1534.
- Moher D, Altman DG, Liberati A, Tetzlaff J (2011) PRISMA statement. Epidemiol 22:128.
- Price DJ, Shearer FM, Meehan MT, McBryde E, Moss R, et al. (2020) Early analysis of the Australian COVID-19 epidemic. Elife 9:58785.
- Shakespeare-Finch J, Bowen-Salter H, Cashin M,Badawi A, Wells R, et al. (2020) COVID-19: an Australian perspective. J Loss Trauma 25:662-672.
- Baker MG, Wilson N, Anglemyer A(2020) Successful elimination of Covid-19 transmission in New Zealand. N Engl J Med 383: 56.
- Olivia S, Gibson J, Nasrudin R(2020) Indonesia in the Time of Covid-19. Bull indones econ stud 56:143-174.
- Suryahadi A, Al Izzati R, Suryadarma D (2020) The impact of COVID-19 outbreak on poverty: An estimation for Indonesia. Jakarta: The SMERU Research Institute.
- Setiati S, Azwar MK(2020) COVID-19 and Indonesia. Acta Med Indones 52:84-89.
- Marston C, Renedo A, Miles S(2020) Community participation is crucial in a pandemic. Lancet 395:1676-1678.
- Yanti B, Wahyudi E, Wahiduddin W, Novika RGH, Arina YMD, et al. (2020) Community knowledge, attitudes, and behavior towards social distancing policy as prevention transmission of COVID-19 in indonesia. J Administrasi Kesehatan Indonesia 8:4-14.
- Russell E (2020) Covid 19 coronavirus: New Zealand rolls out drive-through hubs for testing Covid-19.NZME.
- (2020) Poll: 88% of Kiwis trust Government's coronavirus response, vastly higher than other nations.
- (2020) Coronavirus update: New Zealand close to achieving goal of eradication, record increases seen in India, Pakistan and Russia. News.
- Megalokonomos M (2020) Australia has recorded fewer than 100 coronavirus deaths - why do other countries differ so much? SBS News.
- Phua J, Faruq MO, Kulkarni AP, Redjeki IS, Detleuxay K, et al. (2020) Critical Care Bed Capacity in Asian Countries and Regions. Crit Care Med 48:654-662.
- Shields L, Hartati LE (2003) Nursing and health care in Indonesia. J Adv Nurs 44:209-216.
- Litton E, Bucci T, Chavan S, Ho YY, Holley A, et al.(2020) Surge capacity of Australian intensive care units associated with COVID-19 admissions. Med J Aust 212: 463-467.
- Summers J, Cheng HY, Lin HH, Barnard LT, Kvalsvig A, et al. (2020) Potential lessons from the Taiwan and New Zealand health responses to the COVID-19 pandemic. The Lancet Regional Health-Western Pacific 4.n
- Udy A (2020) Quapotequisque, in eaconterat arte diem': COVID-19 and Australian and New Zealand intensive care. Crit Care Resusc 2:103.
- Agustina R, Dartanto T, Sitompul R, Susiloretni KA, Achadi EL, et al. (2019) Universal health coverage in Indonesia: concept, progress, and challenges. Lancet 393:75-102.
- Ridley EJ, Freeman-Sanderson A, Haines KJ (2021) Surge capacity for critical care specialised allied health professionals in Australia during COVID-19. Aust Crit Care 2: 191-193.
- Sutarsa IN (2020) Poor and rich Indonesians do not get equal access to COVID-19 tests: this is why it’s a problem.
- Djalante R, Lassa J, Setiamarga D, Mahfud C, Sudjatma A, et al.(2020) Review and analysis of current responses to COVID-19 in Indonesia: Period of January to March 2020. Progress in Disaster Science 6:100091.
- Mahendradhata Y, Trisnantoro L, Listyadewi S, Soewondo P, Marthias T, et al. (2017)The Republic of Indonesia health system review.
- Hendarwan H, Syachroni S, Aryastami NK, Su’udi A, Susilawati MD, et al. (2020) Assessing the COVID-19 diagnostic laboratory capacity in Indonesia in the early phase of the pandemic. WHO South East Asia J Public Health 9:134-140.
- Funk CD, Laferriere C, Ardakani A (2020) A snapshot of the global race for vaccines targeting SARS-CoV-2 and the COVID-19 pandemic. Front pharmacol 11:937.
- Desborough J, Hall SL, de Toca L, Davis S, Roberts L, et al. (2020) Australia’s national COVID-19 primary care response. Med J Aust 3: 104-106.
- Ahmed N, Michelin RA, Xue W, Ruj S, Malaney R, et al. (2020) A survey of covid-19 contact tracing apps. IEEE8:134577-134601.
- (2021) Andrews 'sorry' for hotel quarantine errors as report unable to determine who made private security call.
- Carr A (2020) COVID-19 indigenous peoples and tourism: a view from New Zealand. Tourism Geographies 22:491-502.
- Diseases TLI (2020) COVID-19, a pandemic or not? The Lancet Infectious Diseases 20:383.
- Tosepu R, Gunawan J, Effendy DS, Lestari H, Bahar H, et al. (2020) Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci Total Environ 725:138436.
- Barker A, Souisa H (2020) Coronavirus COVID-19 death rate in Indonesia is the highest in the world. Experts say it's because reported case numbers are too low. News.
- MCBETH J (2020) Indonesia’s high Covid-19 kill rate hides hard facts.
- OM J. (2020) Has New Zealand really done better than Australia in controlling coronavirus?.
- Pannett R (2020) Both New Zealand and Australia Contained Coronavirus, but One Is Set to Pay a Heavier Price.
- Maes K, Closser S, Vorel E, Tesfaye Y (2015) Using community health workers. Ann Anthropol Pract
- Maes K, Closser S, Vorel E, Tesfaye Y (2015) A women’s development army: narratives of community health worker investment and empowerment in rural Ethiopia. Stud Comp Int Dev 50:455-478.
- Satherley D (2020) Coronavirus: Does New Zealand really top the world in COVID-19 testing? Newshub.
- The Union(2020) Indonesia commits to raising tobacco taxes to fund health systems strained by tobacco and COVID-19.
- Teklehaimanot HD, Teklehaimanot A (2013) Human resource development for a community-based health extension program: a case study from Ethiopia. Hum Resour Health 11:39.
- EinhornHSa B (2020) Heavy Smoking Blamed for Indonesia’s 6.6% Coronavirus Death Rate.
- Gramenz J (2020) Indonesia’s child death rate won’t stop COVID-19 restrictions easing.
- Phillips B, Gray M, Biddle N (2020) COVID-19 Job Keeper and Job Seeker impacts on poverty and housing stress under current and alternative economic and policy scenarios.
- Lambropoulos V (2020) Coronavirus, Job keeper and Stand Down under the Fair Work Act 2009 (CTH): A Review of the Law.Australian Business Law Review - Special COVID-19 Edition, Forthcoming.
- Dalglish SL (2020) COVID-19 gives the lie to global health expertise. Lancet 395:1189.
- Burki T (2020) China's successful control of COVID-19. Lancet Infect Dis 20:1240-1241.
- Tashiro A, Shaw R (2020) COVID‐19 pandemic response in Japan: what is behind the initial flattening of the curve? Sustainability 12:5250.
- (2020) Emerging COVID-19 success story: South Korea learned the lessons of MERS.Exemplars in Global Health.
- Lee S, Hwang C, Moon MJ (2020) Policy learning and crisis policy-making: quadruple-loop learning and COVID-19 responses in South Korea. Policy Soc 39:363-381.
- De Leo S (2020)Covid-19 testing strategies and lockdowns: the European closed curves, analysed by``s kew-normal distributions, the forecasts for the UK, Sweden, and the USA, and the ongoing outbreak in Brazil. med Rxiv.
- Cohen J, Kupferschmidt K(2020) Countries test tactics in ‘war’ against COVID-19. AAAS 367: 1287-1288.
- Chang CL, McAleer M (2020) Alternative global health security indexes for risk analysis of COVID-19. Int J Environ Res Public Health 17:3161.
- Abbey EJ, Khalifa BA, Oduwole MO, Ayeh SK, Nudotor RD, et al. (2020) The Global Health Security Index is not predictive of coronavirus pandemic responses among Organization for Economic Cooperation and Development countries. PloS one 15:0239398.
- Madgavkar A, White O, Krishnan M, Mahajan D, Azcue X (2020) COVID-19 and gender equality: Countering the regressive effects. McKinsey.
- Lambert H, Gupte J, Fletcher H, Hammond L, Lowe N,et al. (2020) COVID-19 as a global challenge: towards an inclusive and sustainable future. Lancet Planet Health 4:312-314.
- Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA(2000) Gender differences in the utilization of health care services. J FamPract 49:147-152.
- Rembis M, Djaya HP (2020) Gender, Disability, and Access to Health Care in Indonesia: Perspectives from Global Disability Studies. Transforming Global Health: Springer pp: 97-111.
- Cyn-Young P, Marie IA (2020) COVID-19 is no excuse to regress on gender equality.Asian Development Bank.
- Cassells R, Duncan A (2020) JobKeeper: The Efficacy of Australia’s First Short-Time Wage Subsidy’. Aust J Labour Econ 23:99-128.
- O’Sullivan D, Rahamathulla M, Pawar M (2020) The impact and implications of COVID-19: An Australian perspective. The International Journal of Community and Social Development 2:134-151.
- Pellicano E, Stears M (2020) The hidden inequalities of COVID-19. SAGE Publications Sage: 1309-1310.
- Pinho-Gomes AC, Peters S, Thompson K, Hockham C, Ripullone K, et al. (2020) Where are the women? Gender inequalities in COVID-19 research authorship. BMJ Glob Health 5: 002922.
- Jaffrey S (2020) Coronavirus Blunders in Indonesia Turn Crisis Into Catastrophe. Carnegie Endowment for International Peace.
- Om J(2020) Has New Zealand really done better than Australia in controlling coronavirus? News.
- Pannett R (2020) Both New Zealand and Australia Contained Coronavirus, but One Is Set to Pay a Heavier Price.The Wall Street Journal.
- NZME (2020) Covid 19 coronavirus: New Zealand rolls out drive-through hubs for testing Covid-19.
- The Conversation (2020) Poor and rich Indonesians do not get equal access to COVID-19 tests: this is why it’s a problem.
- Permitasari N, Satibi S, Kristina SA (2018)National Burden of Cancers Attributable to Secondhand Smoking in Indonesia. Asian Pac J Cancer Prev 19: 1951-1955.
- Setiati S, Azwar MK (2020) COVID-19 and Indonesia. Acta Med Indones 52:84-89.
- Gupta A, Bherwani H, Gautam S, Anjum S, Musugu K, et al. (2020) Air pollution aggravating COVID-19 lethality? Exploration in Asian cities using statistical models. Environment, Development and Sustainability15: 1-10.
- Sasmita NR, Ikhwan M, Suyanto S, Chongsuvivatwong V (2020)Optimal control on a mathematical model to pattern the progression of coronavirus disease 2019 (COVID-19). Glob Health Res Policy 5:38.
- Tosepu R, Gunawan J, Effendy DS, Ahmad OAI, Lestari H, et al. (2020) Correlation between weather and Covid-19 pandemic in Jakarta. Sci Total Environ 725: 138436.
- Eryando T, Sipahutar T, Rahardiantoro S (2020) The Risk Distribution of COVID-19 in Indonesia: A Spatial Analysis. Asia Pac J Public Health 8: 450-452.
- Ravindran B, Hogarth F, Williamson K, Wright R, Kirk M, et al. (2020) High COVID-19 attack rate among attendees of wedding events in Bali. Commun Dis Intell 23: 83.
- Steyn N, Binny RN, Hannah K, Hendy SC, James A, et al. (2020) Estimated inequities in COVID-19 infection fatality rates by ethnicity for Aotearoa New Zealand. N Z Med J 133:28-39.
- Bandyopadhyay G, Meltzer A (2020) let us unite against COVID-19 - a New Zealand perspective. Ir J Psychol Med 37:218-221.
- Litton E, Bucci T, Chavan S, Ho YY, Holley A, et al. (2020) Surge capacity of intensive care units in case of acute increase in demand caused by COVID-19 in Australia. Med J Aust 212:463-467.
- Kidd M (2020) Australia’s primary care COVID-19 response. Aust J Gen Pract49.
- Bilinski A, Emanuel EJ (2020) COVID-19 and Excess All-Cause Mortality in the US and 18 Comparison Countries. JAMA 324:2100-2102.
- Kidd M(2020) Australia’s primary care COVID-19 response. Aust J Gen Pract49.
- Abbas R, Michael K (2020) COVID-19 contact trace app deployments: Learnings from Australia and Singapore. IEEE Consum Electron Mag 9:65-70.
- Jefferies S, French N, Gilkison C, Graham G, Hope V, et al. (2020) COVID-19 in New Zealand and the impact of the national response: a descriptive epidemiological study. The Lancet Public Health 5:612-623.