Case Report - (2023) Volume 17, Issue 3
Aneurysmal cyst: Case report.
Amal Lachkar*,
Bouzoubaa SM and
Ben Yahya I
Faculty de medicine dentaire, Morocco
*Correspondence:
Amal Lachkar, Faculty de medicine dentaire,
Morocco,
Tel: 0670224743,
Email:
Received: 03-Mar-2023, Manuscript No. Iphsj-23-13541;
Editor assigned: 06-Mar-2023, Pre QC No. Iphsj-23-13541 (PQ);
Reviewed: 20-Mar-2023, QC No. Iphsj-23-13541;
Revised: 25-Mar-2023, Manuscript No. Iphsj-23-13541(R);
Published:
31-Mar-2023, DOI: 10.36648/1791- 809X.17.3.1004
Abstract
The aneurysmal bone cyst (KOA) is a benign cystic lesion of the bones. It is consisted of
blood-filled cavities separated from each other by septa of connective tissue comprising
fibroblasts, giant osteoplastic cells, and a larger trabecular meshwork bone, more or
less abundant. It affects especially the long bones and the rachis. It occurs mainly in
children and young adults, with a slight predominance of women. We report the case
of a KOA in a young 13 year old patient, with accidental radiological discovery. The
purpose of the presentation of this case is to identify the diagnostic, therapeutic and
prognostic features of this lesion which lyses the bone aggressively and can simulate a
variety of aggressive tumors.
Key words
Aneurysmal Bone Cyst; Oral Cavity; Maxillary
Introduction
According to the WHO definition (2002), the aneurysmal bone cyst (KOA) is a benign cystic lesion of the bones consisting of bloodfilled cavities separated from each other by septa of connective tissue containing fibroblasts, osteoplastic giant cells and a more or less abundant reaction trabecular bone [1,2,3]. In 1893, Van Arsdale called this lesion hematoma humerus ossifing [4]. In 1940 Ewing uses the term aneurysmal » to describe this lesion [1]. The term aneurysmal cyst is described for the first time in 1942 by Jaffe and Lichtenstein [ 1, 4] it was not until 1950 that the term aneurysmal bone cyst was used for the first time in the literature [4]. We are reporting the case of a young patient, presenting an aneurysmal bone cyst of the mandible, emphasizing the diagnostic difficulties, and the therapeutic management of this rare entity.
Case report
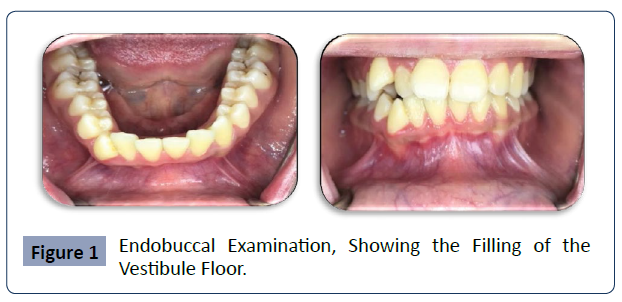
We received in consultation a 13-year-old girl, who was referred by her orthodontist following the fortuitous discovery of a symphysis mandibular image; she presents an apparently good general condition. The exobuccal examination showed no specificity, the palpation of the cervical ganglion areas revealed no lymphadenopathy. At the endobuccal examination (Fig. 1), oral hygiene was correct, with the presence of a swelling sitting on the mandibular symphysis level, filling the bottom of the vestibule. The swelling was well circumscribed and extended from the distal surface of the 32 to the distal surface of the 42. The overlying mucosa was normal in appearance. On palpation the swelling was hard, not painful nor bleeding. Cold vitality tests were positive for the entire incise group, as opposed to canines that had a delayed response, with no persistence of pain after stopping the stimulus (Figure 1).
Figure 1 Endobuccal Examination, Showing the Filling of the Vestibule Floor.
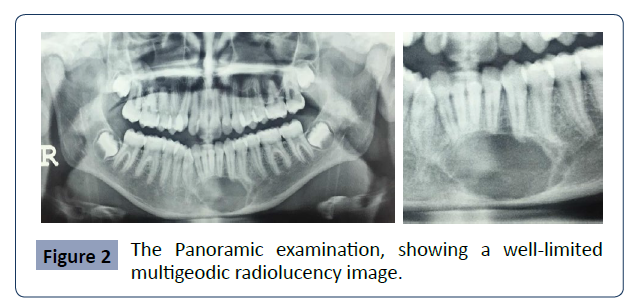
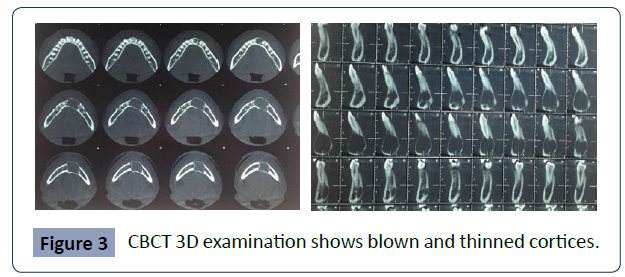
The panoramic X-ray showed a well-defined radiolucency image, surrounded by a peripheral border extending from 34 to 43, and from the basilar rim to 1/3 apical of the incisive-canine mandibular group, with several geodes and respecting the continuity of the basilar rim, without resorption nor displacement of the adjacent teeth (fig 2). The cone beam examination showed a blistering and thinning of the vestibular and lingual cortical without rupture, it was a lesion formed of a principal clear radio geode of greater diameter, and of some small geodes (fig 3). Figure 2: the panoramic examination, showing a well-limited multigeodic radiolucency image. Figure 3: CBCT 3D examination shows blown and thinned cortices (Figure 2 & 3).
Figure 2 The Panoramic examination, showing a well-limited multigeodic radiolucency image.
Figure 3 CBCT 3D examination shows blown and thinned cortices.
The puncture was negative, which led to the diagnosis of a full tumor. The diagnoses mentioned were those of ameloblastoma, myxoma, giant-cell central granuloma, and ossifying fibroma, or an aneurysmal bone cyst, or a solitary bone cyst or a keratocyst.
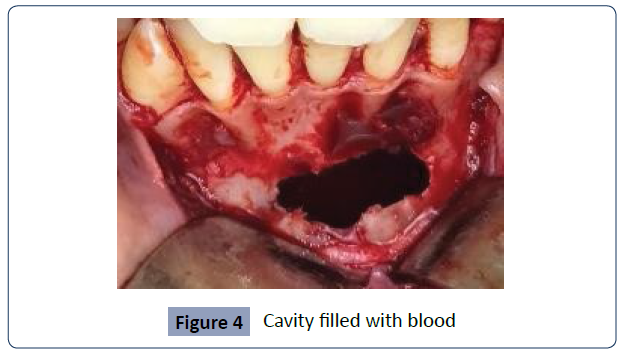
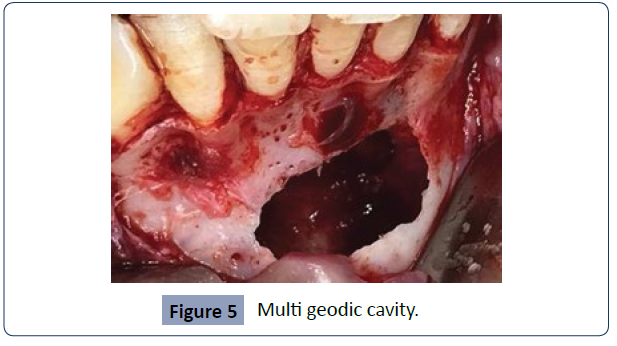
The treatment consisted in the realization of a cystic enucleation, under local anaesthesia, the elimination of the vestibular cortex, allowed to find a bone cavity, without cystic pouch, filled with a bright red blood (figure 4, 5). After aspiration of this fluid, fine fibrous tissue was found, then removed, and sent for anatomopathological examination (Figure 4-6).
Figure 4 Cavity filled with blood
Figure 5 Multi geodic cavity.
Figure 6 Performed for all the teeth plunging within
the bone cavity.
At the end an apical resection was performed for all the teeth plunging within the bone cavity. Postoperative: Amoxicillin 2g daily, combined with short-course corticosteroids has been prescribed. Pathological examination concluded the diagnosis of aneurysmal bone cyst.
Discussion: The aneurysmal bone cyst is a primary or secondary benign tumor, consisting of an intraosseous cavity, uni or multilocular, with a thematic content, not bordered by an endothelium [5]. It behaves locally in an aggressive manner because of its rapid growth and of its osteolytic capacity [6, 7]. In 2018 WHO classified the aneurysmal cyst, a group of giant cell and bone cysts, as a subunit of bone tumors and associated lesions [8]. The aneurysmal bone cyst often sits in the metaphysis of the long bones 50% and the spine 20% [2]. Its development in the maxillae is rare, 1.9% of the aneurysmal cysts are located in the maxilla, it represents 1.5% of non-odontogenic cysts [4, 9, 10]. It mainly affects children and young adults, between the 2nd and 3rd decades, with a slight predominance of women [5, 10, 11]. The aneurysmal bone cyst has a mandibular/ maxillary predominance: the rates vary from 2: 1 to 11: 9 [12], the preferred seats are the horizontal limb (40%), the ramus (30%), the mandibular Angle (19%), and the condyles (2%) [4, 7]. The symphysis region is generally respected [5], whereas it is the affected region for the reported case.
Etiopathogenesis is uncertain and controversial [6, 8]. KOAs are most commonly found in high venous bone and high bone marrow [3, 5, 9]. Several theories have been discussed, whether it is a neoplasm, an abnormal development, an Arteriovenous malformation [6], a genetic predisposition, a chronic infection, an abnormality Arteriovenous, degenerative lesion or sub periosteal intraosseous hematoma [2,3,6]. Some authors, such as Struthers and Shears, consider the aneurysmal bone cyst as a lesion secondary to trauma followed by the development of a sub periosteal hematoma [1,4,7], whereas our patient has not reported any history of trauma even minimal. Some researchers have demonstrated that a chromosomal translocation (q22; p13) is a cytogenic abnormality that can lead to the development of a primary KOA [2, 12]. Clinically, the aneurysmal bone cyst has a variable symptomatology. It may be asymptomatic for incidental discovery [10, 12], as in the case reported, as it may be symptomatic, mainly pain [5,7,12], bone expansion [2, 12], mobility and tooth displacement [6,7] the appearance of a pathological fracture [5]. The radiographic aspect is not characteristic [6], one can find a radio-clear image, uni-geodic [2, 11], or multi geodic in honeycomb or bubble of soap, as the reported case. Computed tomography allows to assess the extent of bone lysis [13], and to show bone expansion, sometimes with blown and thinned cortices [5], which has been noted for the reported case, sometimes even cortical rupture and periosteal reaction [7].
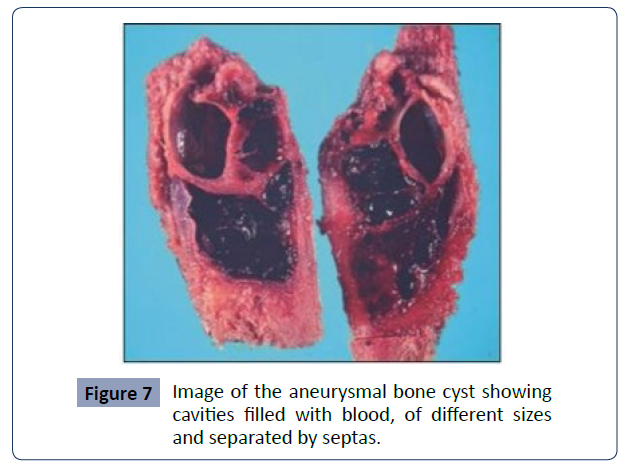
Macroscopically, KAO is considered a pseudo cyst because of the absence of an epithelial wall [4]. Microscopically, there are cavities of variable size filled with blood, separated by the connective tissue, by trabecular bone or osteoid tissue, many giant cells osteoplastic [4, 7, 11, 12] (Figure 7).
Figure 7 Image of the aneurysmal bone cyst showing cavities filled with blood, of different sizes and separated by septas.
The aneurysmal bone cysts are clinically and histologically divided into three types [9] vascular (95% of cases) is characterized by an expanding lesion, rapid growth leading to cortical perforation and invasion of soft tissue [4,9] it presents histologically a sparse stroma, numerous sinusoids gorged with blood and caves. Bleeding can occur during surgery and extensive bone destruction with soft tissue spread is also evident [12], Solid type(5%); which can be in the form of a small asymptomatic lesion noticed for the first time as a radiolucency on a routine X-ray or a slight swelling [4,9], few blood vessels and caves [12], this type lends confusion with: the repairer giant cell granuloma / brown tumor [11] Histologically this dense stroma, lean sinusoids few blood vessels and caves, bone expansion and heavy bleeding during surgery [12], a mixed type, has both vascular and solid-type features, probably representing a transition phase of the lesion [4,9,12].
Preoperative diagnosis is difficult [3], due to clinical similarity, and radiological with: traumatic bone cyst, giant cell tumor, hyperparathyroidism [3]. If anatomopathological examination allows a giant cell granuloma to be rejected [10], the difference with the solitary bone cyst is due to the presence of bone partitions and dental resorption, which facilitate the diagnosis towards a KOA [14]. To eliminate brown tumors, it is recommended to study the serum levels of calcium, phosphate and alkaline phosphatase [7]. The main diagnostic challenge for KOA is the possibility of an erroneous diagnosis of osteosarcoma on both histological and radiological evaluation [11]. The treatment of KOA depends on the extent of the lesion [2, 3] ranging from the Wait and see [12] approach, to the simple curettage of blocks resection and bone grafting. In multigame cases divided by bone septa, complete curettage may be difficult; the irrigation of the cavity with diluted hydrogen peroxide allows the identification of the origin of the bleeding, the control of bone bleeding and encourages additional curettage [15]. Recurrence is high, ranging from 26% to 56% [1], regular monitoring of the patient is required with periodic imaging until complete bone repair [6].
To Conclude, KOA is a pseudo-cystic lesion with rapid and aggressive local evolution. Radiological imaging is inconclusive, making diagnosis difficult and may lead to error. After complete curettage, the prognosis is generally good.
References
- Mark J, Kransdorfand Donald E (1995) Sweet Aneurysmal Bone Cyst: Concept, Controversy, Clinical Presentation, and Imaging AJR 164:573-580.
Indexed at, Google Scholar, Crossref
- Aadithya B (2014) Aneurysmal Bone Cyst of the Jaws: Clinic pathological Study. J Maxillofac Oral Surg 13:458-463.
Indexed at, Google Scholar
- Sheth (2010) Maxillary aneurysmal bone cyst: Report of a rare case 307 J Ind Soc of pedodontics and preventive dentistry 28.
Google Scholar
- Pelo (2009) Aneurysmal Bone Cyst located in the Mandibular Condyle. Head and face medicine 58.
Indexed at, Google Scholar
- AssiniEyogho S (2011) Kisne osseux aneurysmal bimaxillaire: presentation d’un cas Med Buccale Chir Buccal 17: 45-50.
Google Scholar
- Tang I P (2009) Aneurysmal bone cyst of the maxilla. Singapore Med J 50: e326.
Google Scholar
- Lopez-Arcas-Calleja JM, Cebrian-Carretero JL, González-Martín J, Burgueno M (2007) Aneurysmal bone cyst of the mandible: Case presentation and review of the literature. Med Oral Patol Oral Cir Bucal 12: E401-3.
Indexed at, Google Scholar, Crossref
- Paul M (2018) Speight Takashi Takata. New tumour entities in the 4th edition of the World Health Organization Classification of Head and Neck tumours: odontogenic and maxillofacial bone tumours. Virchow’s Arch 472:331-339.
Indexed at, Google Scholar, Crossref
- Arora SS (2012) Aneurysmal bone cyst of maxilla existing concurrently with a giant cell granuloma of mandible: A case report of an unusual presentation. J Ind soc pedod and prev den 30.
Indexed at, Google Scholar
- Derruau S et al. (2017) Kyste osseux aneurysmal mandibular:un diagnostic qui reste difficile 65 eme Congres de la SFCO.
Crossref
- Oganavşa R B (2015) Bone Cysts Lesions: Histopathological Spectrum and Diagnostic Challenges. Turkish J Pathology 31:95-103.
Google Scholar
- Debnath SC, Adhyapok AK, Hazarika K, Malik K, Vatsyayan A (2016) Aneurysmal bone cyst of maxillary alveolus: A rare case report. Contemp Clin Dent 7:111-1113.
Indexed at, Google Scholar, Crossref
- Slama A (2007) coll Le kyste osseux aneurysmal de la mandible. Med Buccale Chir Buccale 13: 139-142.
Google Scholar
- Bouzoubaa S (2012) Le kyste osseux solitaire: a propos d’un cas Clinique. Med Buccale Chir Buccale 18:371-375.
Google Scholar
- Motamedi MHK, Behroozian A, Azizi T, Nazhvani AD, Motahary P et al. (2014) Assessment of 120 maxillofacial aneurysmal bone cysts: A nationwide quest to understand this enigma. J Oral Maxillofacial Surg.
Indexed at, Google Scholar, Crossref
Citation: Lachkar A, Bouzoubaa SM, Yahya
IB (2023) Aneurysmal cyst: Case report.
Health Sci J. Vol. 17 No. 3: 1004.