Keywords
Antimicrobial; Egerton; Fungal; Kenya; Mushroom; Njoro
Introduction
Microorganisms make a group of organisms some of which cannot be seen with unaided eye [1]. Bacteria occur a wide range of shapes, ranging from spheres to rods and spirals and they are a few micrometres in length while fungi are said to be macroscopic [2]. The ability of microorganisms to survive in varied habitats such as on earth, growing in soil, acidic hot springs, radioactive waste [3] water, deep in the earth’s crust, as well as in organic matter and the live bodies of plants and animals allows them to be the most populous organisms on earth. For example, there are about 40 million bacterial cells in a gram of soil and a million bacterial cells in a millilitre of fresh water [4]. Totally, there are approximately five nonillions bacteria on earth, forming much of the world’s biomass [5].
Previously, there has been a mix up in classification of microorganisms. A case in point is bacteria were regarded as plants belonging to the class Schizomycetes [6]. However, with the rise of sophisticated techniques coupled with advanced cellular analysis, classification of microorganisms has been ironed out. Fungi are now considered eukaryotes while bacteria are prokaryotes. Unlike cells of animals and other eukaryotes, bacterial cells do not contain a nucleus and rarely harbour membrane-bound organelles [3]. Although the term bacteria traditionally included all prokaryotes, the scientific classification changed after the discovery in the 1990s that prokaryotes consist of two very different groups of organisms that evolved independently from an ancient common ancestor. These evolutionary domains are called Bacteria and Archaea [7].
In the human body, there are approximately ten times as many bacterial and fungal cells in as there are human cells in the body [8]. Majority of these organisms are found on the skin and as gut flora. Their pathogenicity is reduced by the protective effects of the immune system while us some are normal microflora helping the body in various metabolic activities. However, a few species of fungi and bacteria are pathogenic and cause infectious diseases [9].
Currently, the world is witnessing heightened antimicrobial drug resistance. According to Adams (2014) emergence of resistance often reflects evolutionary processes that take place during antibacterial drug therapy. The antimicrobial treatment may select for bacteria strains with physiological or genetically enhanced capacity to survive high doses of antibacterial [10]. Under certain conditions, it may result in preferential growth of resistant bacteria while growth of susceptible bacteria is inhibited by the drug [11]. For example, antibacterial selection within whole bacterial population for strains having previously acquired antibacterial resistant genes was demonstrated in 1943 Laria-Delbruck experiment. Survival of fungi and bacteria often results from inheritable resistance [12].
Antimicrobial resistance is probably the biggest threat to human existence on planet earth today. The use of convectional synthetic drugs in offering remedy to the existing human, animal and plants disease therapy has proved not to be very fruitful [13]. The pathogens are increasingly sharpening their tools to ensure they resist any such drug that finds its way in the market. As a result, the use of naturally produced antimicrobial has gained allot of popularity the reason this study was conceived [14]. The study aimed at isolating Erwinia spp. and Ralstonia solanacearum from infected plants and subjecting the isolates to mushroom and fungal metabolites. In addition, other bacteria that cause disease in humans and animals were also tested.
Materials and Methods
The study area
The study was conducted at Egerton, main campus, Njoro located 25 km southwest of the town of Nakuru, approximately 182 Km by road Northwest of Nairobi and at an altitude of 2.250 above sea level. It receives an annual rainfall of over 1000 mm and the temperatures range between 14-16°C. The soils are well drained, sandy, clay loam with a thick humid top [15].
Collection of plant samples
The infected plant samples were collected from Egerton University’s horticulture farm (Plate 1 and 2). These includd symptomatic potatoes for potato wilt and carrots for soft rot disease.

Figure 1: Infected carrots by Erwinia spp.
Figure 2: Infected potato plants by Ralstonia spp.
Isolation of Erwinia and Ralstonia spp.
The bacteria were isolated separately following a method described by [16]. About 1 g of the infected plant tissues were separately place in a motor and the tissues macerated using a pistil followed by addition of 9 g of distilled water. Serial dilution was carried out up to 10−9. Using a micropipette, 0.01 ml of the diluent was spread on nutrient agar medium using spread plate technique followed by characterization using biochemical tests.
Preparation of mushroom and fungal crude methanol extract
The fruiting bodies of the mushrooms and fungi were dried under shade (Plate 3 and 4). The dried fruiting bodies were cut into small pieces using scalpels and crushed using a pistil and a motor. Separately, 50.0 g of mushroom and fungal powder was placed in Erlenmeyer flasks, onto which 95% methanol had been placed. The flasks were covered with aluminium foil and allowed to stand for seven days for extraction. The mixture was filtered through Whatman filter paper no. 1 and the filtrate concentrated in a rotary evaporator. The methanol was evaporated and the extract was collected and dried. To eliminate the antagonistic effect of methanol, 1ml of methanol extract was mixed with 20 ml of ethyl acetate and shaken vigorously .To this mixture, 30 ml of sodium bicarbonate was added to remove the weak acids followed by filtration using Whatman filter paper no. 1 [17]. In addition bacteria Staphylococcus aureus (ATCC 25923), Enterococcus faecalis (ATCC 29212), Escherichia coli (ATCC 25922), Pseudomonas aeruginosa (ATCC 27853), Streptococcus pneumoniae (ATCC 49617), Proteus vulgaris (ATCC 49990) and fungi Candida albicans, Aspergillus niger (ATCC 1015), Fusarium oxysporum (ATCC 16608) and Ustilago maydis (ATCC 14826), Microsporum gypseum (ATCC 15621), Malassezia furfur (ATCC 14423), were also included in the study.
Plate 3: Mushroom (Agaricus bisporus).
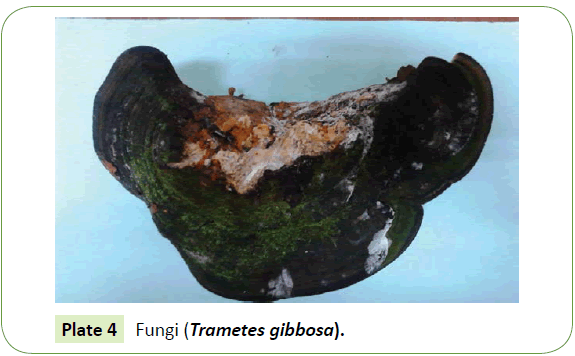
Plate 4: Fungi (Trametes gibbosa).
Assay for antibacterial activity
The antimicrobial assay was performed by Karby Bauer’s agar disc diffusion methods. The surface of the Muller Hinton Agar was separately swabbed with cultures of the test pathogens. Filter paper discs measuring 6.0 mm diameter were cut from Whatman No. 1 filter paper using a cork borer. The discs were sterilized in a dry heat oven before saturation with different concentrations (10 μ-50 μ) of the mushroom and fungal extracts by immersion [18]. The discs were aseptically placed over the swabbed surface and the plates were incubated for 24-48 hr at 37°C. Antimicrobial activities were determined by measuring the diameter of zone of inhibition.
Data analysis
The data was analysed using Statistical Package for Social Sciences Software (SPSS) version 17.0 software. The comparison of inhibition zones of the extracts on the pathogens were compared using one way ANOVA. In addition, comparison of the inhibition activities of mushroom and fungal extracts was carried out using T-tests.
Results
Isolation of Erwinia and Ralstonia spp
A total of 88 Erwinia and Ralstonia spp. were obtained. The Erwinia spp. colonies were white, smooth and with entire edges (Table 1). On the other hand, Rastonia spp. presented themselves on culture media as pinkish red centered colonies. The biochemical reactions of the isolates were typical of Erwinia spp. and Ralstonia spp.
| Pathogen |
Cultural characteristics |
Biochemical characteristics |
| |
|
KOH |
Id |
Ct |
Sh |
Kov |
Cu |
Gr |
| Erwinia spp. |
white, smooth colonies with entire edges |
+ |
+ |
+ |
+ |
- |
+ |
- |
| Ralstonia spp. |
pinkish red centered colonies |
+ |
- |
+ |
- |
+ |
+ |
- |
KOH; Potassium hydroxide test, Id; Indole test, Ct; catalase test, Sh; starch hydrolyses, Kov;
Kovacs oxidase test, Cu; Citrate utilization, Gr; Gram reaction.
Table 1: Cultural and biochemical characteristics of Erwiniaand Ralstonia spp.
Antibacterial activities of mushroom and fungal extracts
The zone of inhibition of mushroom extract on Erwinia spp. ranged from 18 ± 0.1 mm to 12 ± 9.2 mm, Ralstonia spp. (14 ± 0.3-11 ± 0.1), Enterococcus faecalis (15 ± 0.3-09 ± 0.2), Staphylococcus aureus (16 ± 0.1-08 ± 0.2), Streptococcus pneumoniae (14 ± 0.3-10 ± 0.1), Escherichia coli (22 ± 0.2-10 ± 0.2), Pseudomonas aeruginosa (20 ± 0.2 - 10 ± 0.1) and Proteus vulgaris (23 ± 0.2-12 ± 0.1) (Table 2). From the fungal extracts the ranges were Erwinia spp. (24 ± 0.2-15 ± 0.1), Ralstonia spp. (22 ± 0.2-16 ± 0.2), Escherichia coli (23 ± 0.2-14 ± 0.1), Pseudomonas aeruginosa (24 ± 0.1-17 ± 0.2) and Proteus vulgaris (25 ± 0.3-16 ± 0.3). There was no significant difference in inhibition of the bacterial growth by mushroom extracts (F=1.92, P=0.09). However, there was significant growth inhibition of the bacteria by fungal extracts (F=12, P=0.00001). In addition, there was no significant difference in bacterial growth inhibition between mushroom and fungal extracts (P=0.089).
| Extract |
Con. |
Zone of inhibition (mm) |
| |
(µg/ml) |
|
|
| |
|
Er |
Ral |
Ef |
Sa |
Sp |
Ec |
Pa |
Pv |
| Mushroom |
10 |
12±0.2 |
11±0.1 |
09±0.2 |
08±0.2 |
10±0.1 |
10±0.2 |
10±0.1 |
12±0.1 |
| |
20 |
15±0.3 |
11±0.3 |
10±0.1 |
12±0.1 |
11±0.2 |
13±0.1 |
11±0.2 |
15±0.1 |
| |
30 |
17±0.3 |
13±0.3 |
13±0.2 |
14±0.3 |
12±0.1 |
18±0.1 |
13±0.3 |
16±0.3 |
| |
40 |
17±0.2 |
14±0.2 |
14±0.1 |
14±0.2 |
13±0.3 |
20±0.2 |
18±0.1 |
19±0.2 |
| |
50 |
18±0.1 |
14±0.3 |
15±0.3 |
16±0.1 |
14±0.3 |
22±0.2 |
20±0.2 |
23±0.2 |
| Fungi |
10 |
15±0.1 |
16±0.2 |
0±0.2 |
0±0.2 |
0±0.1 |
14±0.1 |
17±0.2 |
16±0.3 |
| |
20 |
18±0.2 |
20±0.3 |
0±0.1 |
0±0.1 |
0±0.1 |
15±0.2 |
18±0.3 |
18±0.1 |
| |
30 |
19±0.2 |
20±0.1 |
0±0.3 |
0±0.1 |
0±0.2 |
17±0.3 |
18±0.1 |
19±0.3 |
| |
40 |
20±0.3 |
21±0.1 |
0±0.2 |
0±0.2 |
0±0.1 |
19±0.1 |
20±0.2 |
20±0.1 |
| |
50 |
24±0.2 |
22±0.2 |
0±0.1 |
0±0.3 |
0±0.3 |
23±0.2 |
24±0.1 |
25±0.3 |
Er; Erwinia spp., Ral; Ralstonia spp., Ef; Enterococcus faecalis, Sa; Staphylococcus aureus,
Sp; Streptococcus pneumoniae,Ec; Escherichia coli, Pa; Pseudomonas aeruginosa,Pv;
Proteus vulgaris
Table 2: Antibacterial activities of mushroom and fungal extracts.
Antifungal activities of mushroom and fungal extracts
The growth inhibition of Candinda albicans by mushroom extracts ranged from (18 ± 0.3-11 ± 0.2), Aspergillus niger (20 ± 0.3-13 ± 0.2), Fusarium oxysporum (16 ± 0.1-08 ± 0.3), Microsporum gypseum (19 ± 0.3-10 ± 0.1), Malassezia furfur (19 ± 0.2-09 ± 0.3) and Ustilago maydis (21 ± 0.2-11 ± 0.3) (Table 3). However, the growth inhibition of the fungal pathogens fungal extracts ranges were Candinda albicans (210.1 ± 12 ± 0.2), Aspergillus niger (20 ± 0.3-14 ± 0.2), Fusarium oxysporum (21 ± 0.1-15 ± 0.3), Microsporum gypseum (22 ± 0.2-14 ± 0.3), Malassezia furfur (20 ± 0.3-10 ± 0.2) and Ustilago maydis (22 ± 0.2-13 ± 0.1). There was no significant difference in growth inhibition of the fungi by mushroom extracts (F=1.44, P=0.24). Contrastingly, there was significant difference in growth inhibition of the fungal pathogens by the fungal extracts (F=2.88, P=0.025) and also in the inhibition of the fungal pathogens by mushroom and fungal extracts (0.0022).
| Extract |
Conc. |
Zone of inhibition (mm) |
| (µg/ml) |
| |
|
Ca |
An |
Fo |
Mg |
Mf |
Um |
| Mushroom |
10 |
11±0.2 |
13±0.2 |
08±0.3 |
10±0.1 |
09±0.3 |
11±0.3 |
| |
20 |
14±0.1 |
15±0.1 |
09±0.2 |
12±0.1 |
11±0.1 |
14±0.2 |
| |
30 |
15±0.2 |
16±0.1 |
12±9.2 |
13±0.3 |
14±0.3 |
15±0.1 |
| |
40 |
18±0.2 |
19±0.3 |
13±0.1 |
15±0.2 |
15±0.2 |
19±0.2 |
| |
50 |
18±0.3 |
20±0.3 |
16±0.1 |
19±0.3 |
19±0.2 |
21±0.2 |
| Fungi |
10 |
12±0.2 |
14±0.2 |
15±0.3 |
14±0.3 |
10±0.2 |
13±0.1 |
| |
20 |
15±-.2 |
16±0.3 |
17±0.1 |
15±0.2 |
13±0.1 |
16±0.2 |
| |
30 |
18±0.1 |
18±0.3 |
18±0.1 |
17±0.3 |
14±0.2 |
18±0.1 |
| |
40 |
19±-.3 |
19±0.1 |
20±0.3 |
18±0.1 |
16±0.2 |
19±0.3 |
| |
50 |
21±-.1 |
20±0.3 |
21±0.1 |
22±0.2 |
20±0.3 |
22±0.2 |
Conc.; concentration, Ca; Candindaalbicans, An; Aspergillusniger, Fo; Fusariumoxysporum,
Mg; Microsporumgypseum, Mf; Malassezia furfur and Um; Ustilagomaydis
Table 3: Antifungal activities of mushroom and fungal extracts.
Discussion
The cultural and biochemical characteristics of Erwinia and Ralstonia spp. obtained in this study are typical of the species (Table 1). Similar results were obtained in a previous study [18]. The similarity in the results could have resulted from the use of standard methods in isolating the bacteria. Besides, upon purification of the cultures by sub culturing, same results should be obtained [19].
A similar study with this one on antimicrobial activities of mushroom and fungal extracts carried got results that differed with the ones obtained in this study (Table 2). According to Li, et al. [20], antimicrobial activities of mushrooms and fungal extracts are greatly influenced by their habitat [21] which could have led to the difference in results. The lack of significant difference in the size of inhibition between the bacterial pathogens could have arisen from the similar biochemical pathways utilized by the bacteria [22]. The antifungal metabolites extracted in this study were not effective in inhibiting growth among Gram positive bacteria which agrees with a previous study carried out elsewhere [23].
The results of the current study show that both mushroom and fungal extracts are antagonistic against bacterial and fungal pathogens (Table 3). This partly agrees with a previous study by Ola, et al. [23]. According to Ola, et al. [24] the growth curves in living organisms and the stage at which antimicrobial metabolites are harvested influence the spectrum of antimicrobial activities of the isolates [14]. Additionally, similarity in the growth environment may also contribute to production of the same metabolites [25].
Conclusions and Recommendations
Mushrooms and fungi produce antimicrobial metabolites that can be exploited in treating diseases that affect man and his plants and animals. This study established that the extracted antifungal did not inhibit growth in gram positive bacteria. There is need to carry further study to establish the chemical composition of the antimicrobials.
Acknowledgements
The authors would want to thank Egerton University for giving them a working space in the Department of Biological Sciences.
Conflict of Interest
The authors declare no conflict of interest.
19071
References
- Willem M (2015)Microbial biofilms and the human intestinal microbiome. NPJ Biofilms Microbiomes 1: 15005.
- Huttenhower C, Gevers D, Knight R, Abubucker S, Badger JH, et al. (2012) Structure, function and diversity of the healthy human microbiome. Nat 486: 207-214.
- Sommer F, Bäckhed F (2013) The gut microbiota-masters of host development and physiology. Nat Rev Microbiol 11: 227-238.
- De Vos WM, De Vos EA (2012) Role of the intestinal microbiome in health and disease: from correlation to causation. Nutr Rev 70: S45-S56.
- Douillard FP, Ribbera A, Kant R, Pietilä TE, Järvinen HM (2013) Comparative genomic and functional analysis of 100 Lactobacillus rhamnosus strains and their comparison with strain GG. PLoS Genet 9: e1003683.
- Zarco MF, Vess TJ, Ginsburg GS (2013) The oral microbiome in health and disease and the potential impact on personalized dental medicine. Oral Dis 18: 109-120.
- Johansson ME, Gustafsson JK, Holmén-Larsson J, Jabbar KS, Xia L, et al. (2014) Bacteria penetrate the normally impenetrable inner colon mucus layer in both murine colitis models and patients with ulcerative colitis. Gut 63: 281-291.
- Mounyr B, Moulay S, Saad K (2016) Methods for in vitro evaluating antimicrobial activity: A review.J Pharm Anal 6: 71-79.
- Jyoti PT, Koichi W, Wilhelm H (2016) Diversity of microorganisms in global fermented foods and beverages. Front Microbiol7: 377.
- Akabanda F, Owusu-Kwarteng J, Tano-Debrah K, Glover R, Nielsen LK, et al. (2013) Taxonomic and molecular characterization of lactic acid bacteria and yeasts in nunu, a Ghanaian fermented milk product. Food Microbiol34: 277-283.
- Pathirage KP, Yunman L (2011) Mushrooms as a functional food mediator in Preventing and ameliorating diabetes. FunctNutri Food 4: 161-71.
- Ayesha B, Abdur R, Muhammad J, Musharaf A (2013) Aggressiveness studies of the pathogen of the bacterial blackleg/soft rot of potato. Sarhad J Agric 29: 119-224.
- Zepeda A, Ojeda-Ramírez D, Soto S, Rivero N, Ayala M (2016)Comparison of antibacterial activity of the spent substrate ofPleurotusostreatusand Lentinulaedodes. Afr J Microbiol 5: 234-250.
- Roy DN, Azad AK, Sultana F, Anisuzzaman AS (2016) In-vitro antimicrobial activity of ethyl acetate extract of two common edible mushrooms. J Pharmacol 5: 79-82.
- Amata RL, Otipa MJ, Waiganjo M, Wabule M, Thuranira EG, et al. (2014) Incidence, prevalence and severity of passion fruitfungal diseases in major production regions of Kenya. J ApplBiosci 20: 1146-1152.
- Rashid M, Chowdhury S, Sultana N (2013) In-vitro Screening of some Chemicals and Biocontrol Agents against Erwiniacarotovorasubsp. carotovora, the Causal Agent of Soft Rot of Potato (Solanumtuberosum). The Agri 11: 1-9.
- Bruna P, Josielle A, Rosane M (2016) Effects of carbon sources and time of cultivation on the antimicrobial activities of intra and extracellular extracts of Pleurotuspulmonariuscultured in submerged conditions. Int J CurrMicrobiolApplSci11: 97-105.
- Lukáš H, Matúš K, Jana H, Martin R, Jana P, et al. (2016) Antimicrobial activity of crude ethanolic extracts from some medicinal mushrooms. J microb biotech food sci 5: 60-63.
- Alves MJ, Ferreira IC, Dias J, Teixeira V, Martins A, et al. (2012) A review on antimicrobial activity of mushrooms (Basidiomycetes) extracts and isolated compounds. Plant med 78: 1707-1718.
- Tsungai R, Chenjerayi K, Catherine C, Mudadi AB, Takafira M (2016) Antibacterial properties of wild edible and non-edible mushrooms found in Zimbabwe.Afr J Microbiol Res 977-984.
- Celik GY, Onbasli D, Altinsoy B, Alli H (2014) In vitro antimicrobial and antioxidant properties of Ganodermalucidumextracts grown in Turkey. European J Med Plants 4: 709-722.
- Cristiane UJ, Eliana F, Margô GO, Karnikowski JK (2016) Antimicrobial properties of the mushroom Agaricusblazei – integrative review. Braz J Pharmacog 26: 780-786.
- Thillaimaharan KA, Sharmila K, Thangaraju T, Karthick M, Kalaiselvam M (2016) Studies on antimicrobial and antioxidant properties of oyster mushroom Pleurotusflorida. Int J PharmaSci Res 4: 1540-1545.
- Adams MR (2014) Antimicrobial properties of fungi. Encyclopaedia of Food Microbiology 5: 717-721.
- Mishra VK, Singh G, Passari AK, Yadav VK, Gupta MK, et al. (2016) Distribution and antimicrobial potential of endophytic fungi associated with ethnomedicinal plantMelastomamalabathricum. J EnvBiol37:229-237.