Case Report - (2022) Volume 13, Issue 3
Anton syndrome due to bilateral posterior cerebral artery stroke
with polyneuropathy in a patient with uncontrolled diabetes
mellitus
Krishnendu Choudhury*,
Swapan Sarkar,
Subhadeep Basu and
Supratim Ghosh
Department of Medicine and Neurology, Jagannath Gupta Institute of Medical Science, West Bengal, India
*Correspondence:
Krishnendu Choudhury, Department of Medicine and Neurology, Jagannath Gupta Institute of Medical Science, West Bengal,
India,
Email:
Received: 22-Dec-2021, Manuscript No. ipjnn-21-12133;
Editor assigned: 24-Dec-2021, Pre QC No. P-12133;
Reviewed: 22-Mar-2022, QC No. Q-12133;
Revised: 24-Mar-2022, Manuscript No. R-12133;
Published:
31-Mar-2022
Abstract
Anton syndrome comprises of visual loss from cortical damage with
patients not perceiving their own blindness in the absence of psychiatric
illness or underlying cognitive impairment. Most commonly it results
from bilateral posterior cerebral artery stroke.
In 1920, Meyer first reported occipital lobe infarction and postulated
compression of branches of the posterior cerebral artery as the causal
factor for Anton syndrome.
Joseph Babinski (1857-1932) used the term “anosognosia” for the
first time, to describe the unawareness of the deficit in patients with
hemiplegia.
We present an elderly man with uncontrolled diabetes mellitus
who was admitted with symptoms of sudden blurring of vision and
repeated fall but he denied having visual loss. On evaluation he was
found to have bilateral posterior cerebral artery ischemic stroke with
hemorrhagic conversion leading to cortical blindness as well as distal
demyelinating motor sensory polyneuropathy.
Keywords
Anton syndrome; Hemiplegia; Motor sensory
polyneuropathy.
Introduction
An elderly diabetic and hypertensive male of age 61 was
brought to our hospital by his relatives who declared that
the patient was complaining of dizziness for previous 2
days and fell several times while moving but denied having
any impairment of his vision [1-3].
Case Report
On physical examination, blood pressure was 176/100
mm Hg.
On neurological examination, his higher functions
were not significantly altered but his insight of illness was
impaired so that he confabulated while asked about his
visual impairment. He could not visually recognize any of
his relatives. He also could recognize the examining doctor
by his conversation. He was unaware of his blindness and
was confabulating about his surroundings when asked
about.
His speech was fluent with normal comprehension and
repetition.
Results
Cranial nerves: Absence of visual perceptions with
normal pupillary light reaction.
Motor system: Decreased power in lower limbs with
decreased knee and ankle jerks bilaterally.
Babinski sign+bilaterally
Sensory system examination revealed diminished
vibration and position sensation in both lower limbs
without any impairment of pain sensation.
His gait was high stepping but couldn't walk without
support.
Investigations: Routine CBC wnl.
FBS, PPBS: 180 and 350 mg /dl.
Serum cholesterol was 230 mg/dl, LDL 175 mg/dl.
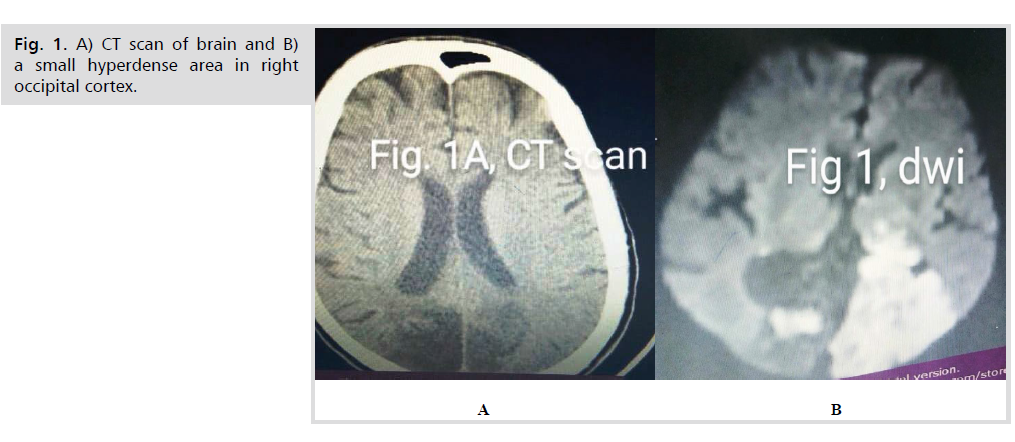
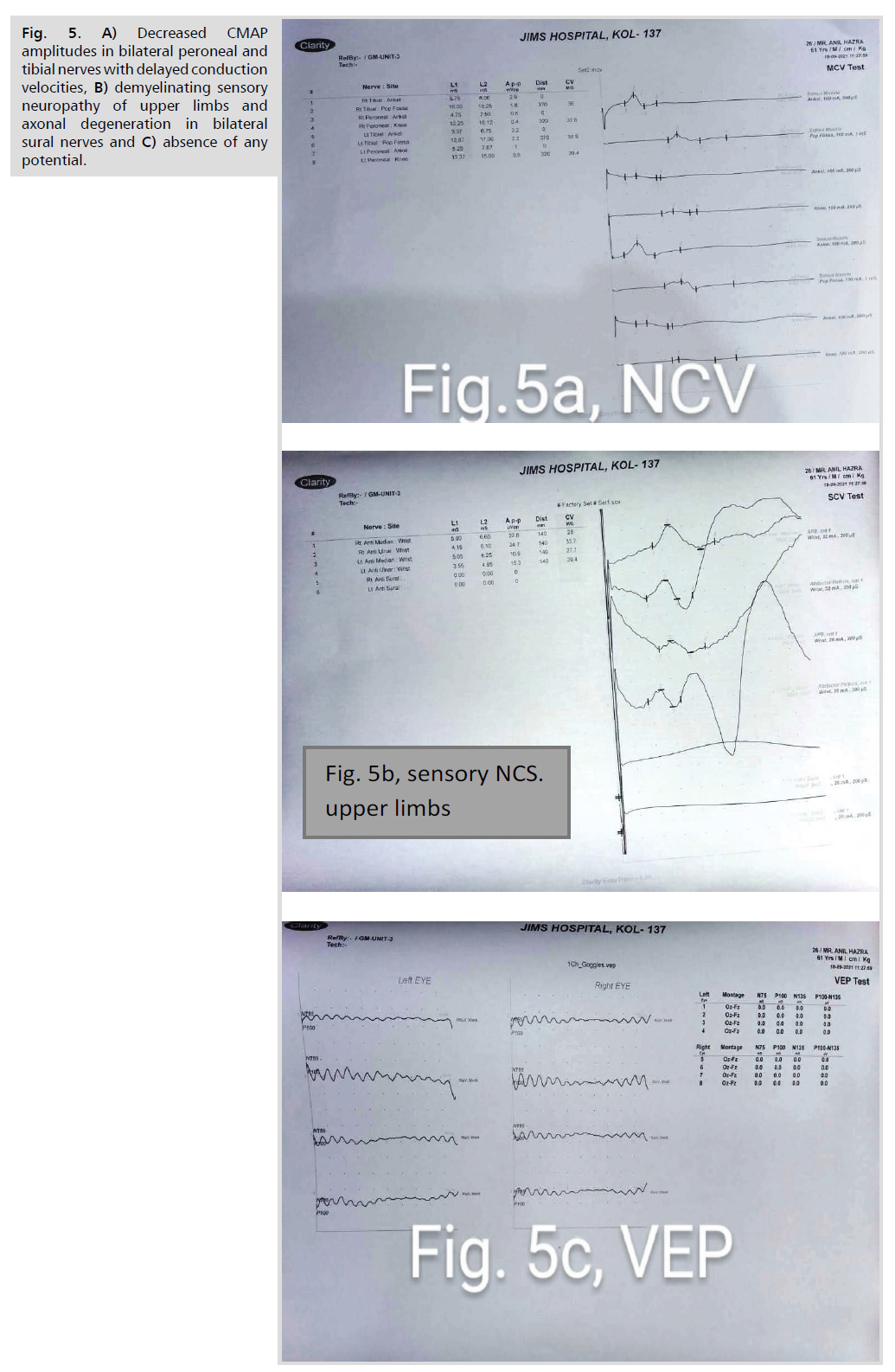
CT brain (Fig. 1A): Hypodense lesions in bilateral
occipital cortices, with a small hyperdense area in right
occipital cortex.
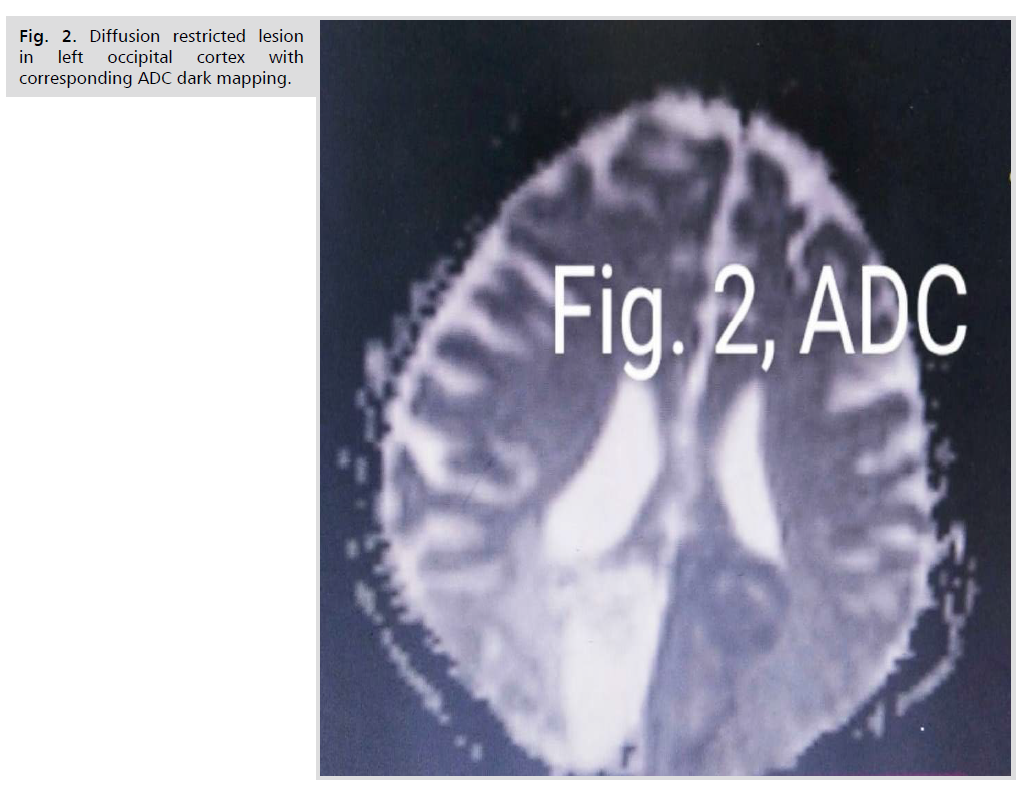
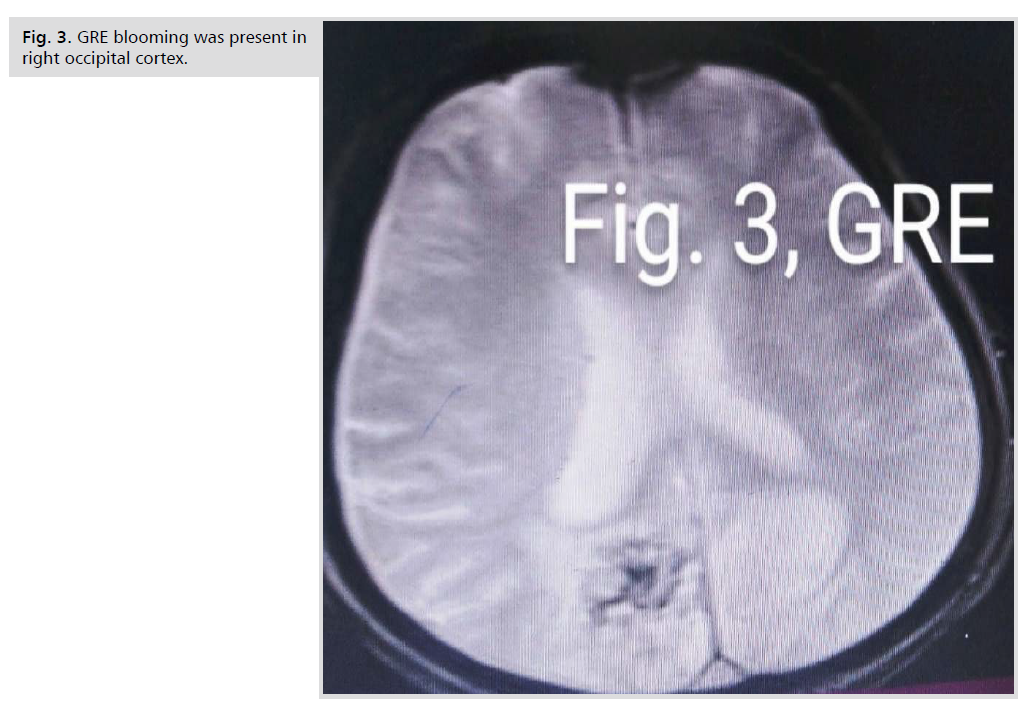
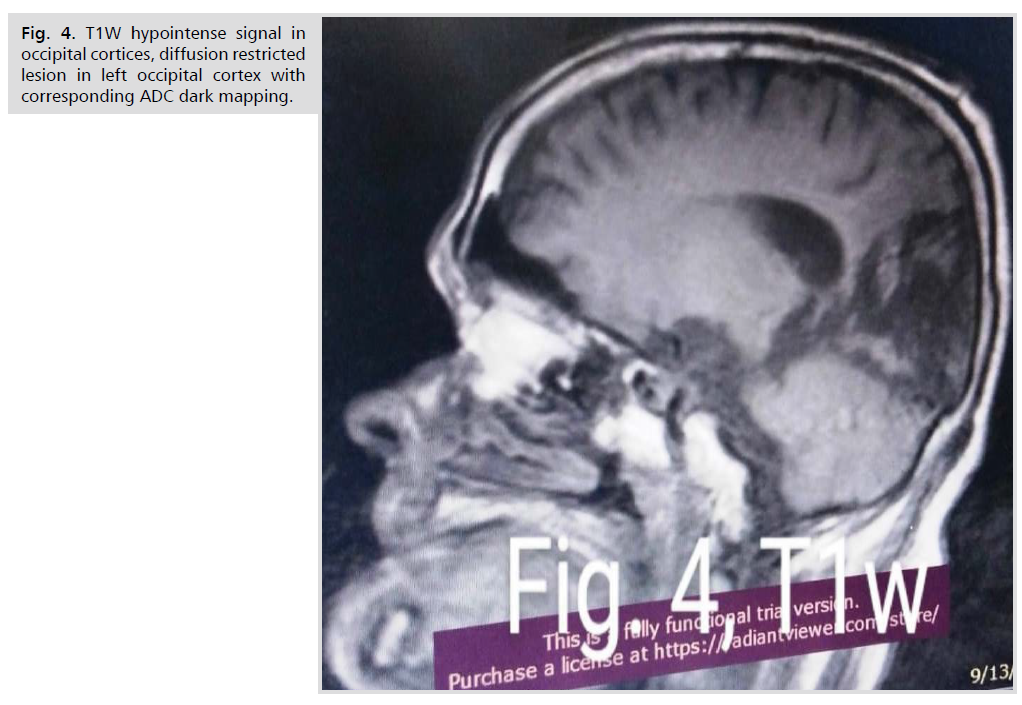
MRI brain (Fig. 1-4.): T1W hypointense signal in
occipital cortices, diffusion restricted lesion in left occipital cortex with corresponding ADC dark mapping. GRE
blooming was present in right occipital cortex.
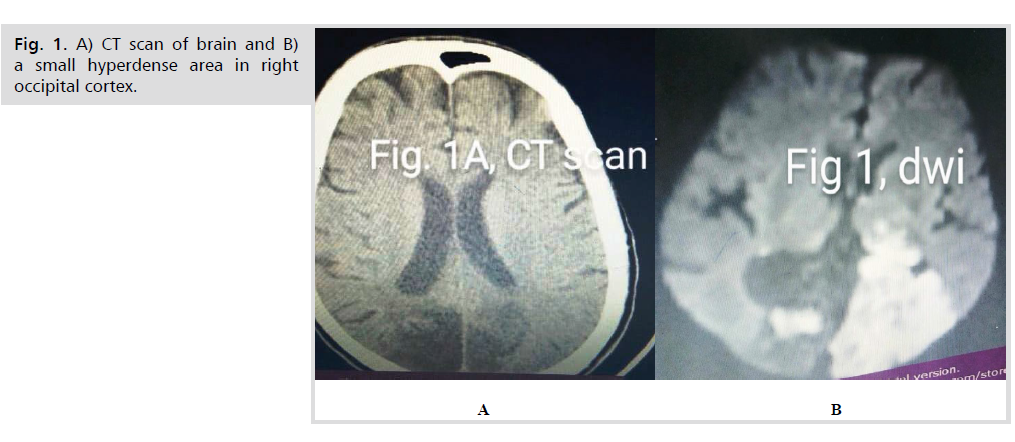
Fig 1: A) CT scan of brain and B) a small hyperdense area in right occipital cortex.
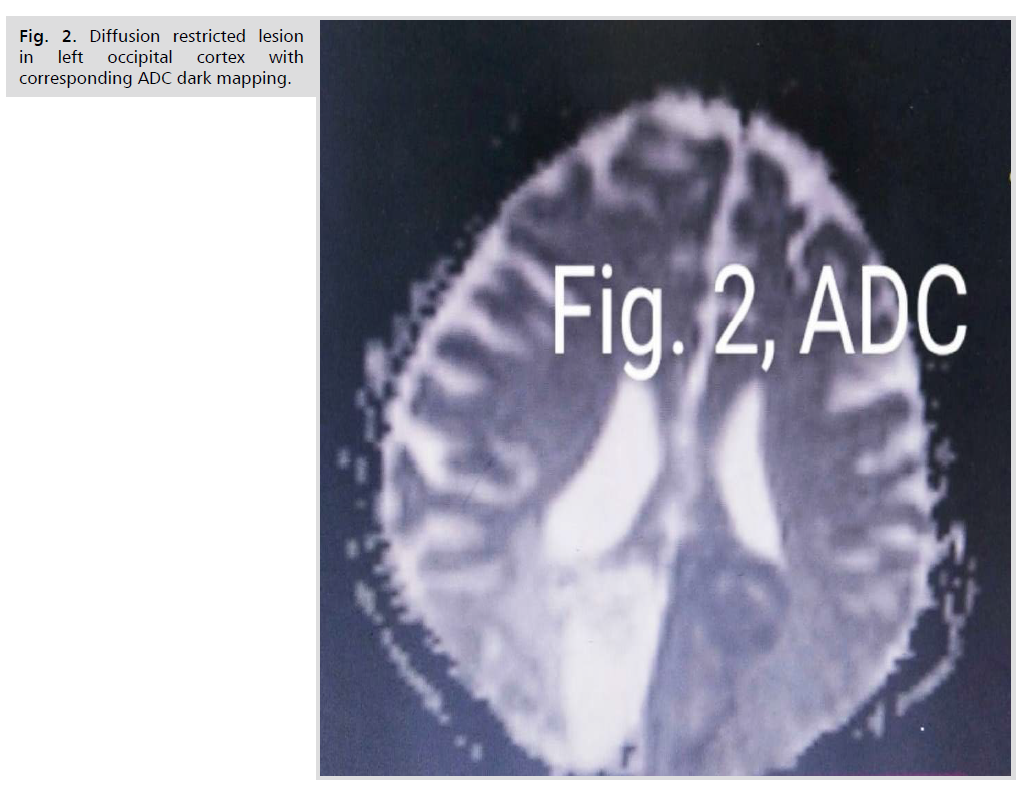
Fig 2: Diffusion restricted lesion in left occipital cortex with corresponding ADC dark mapping.
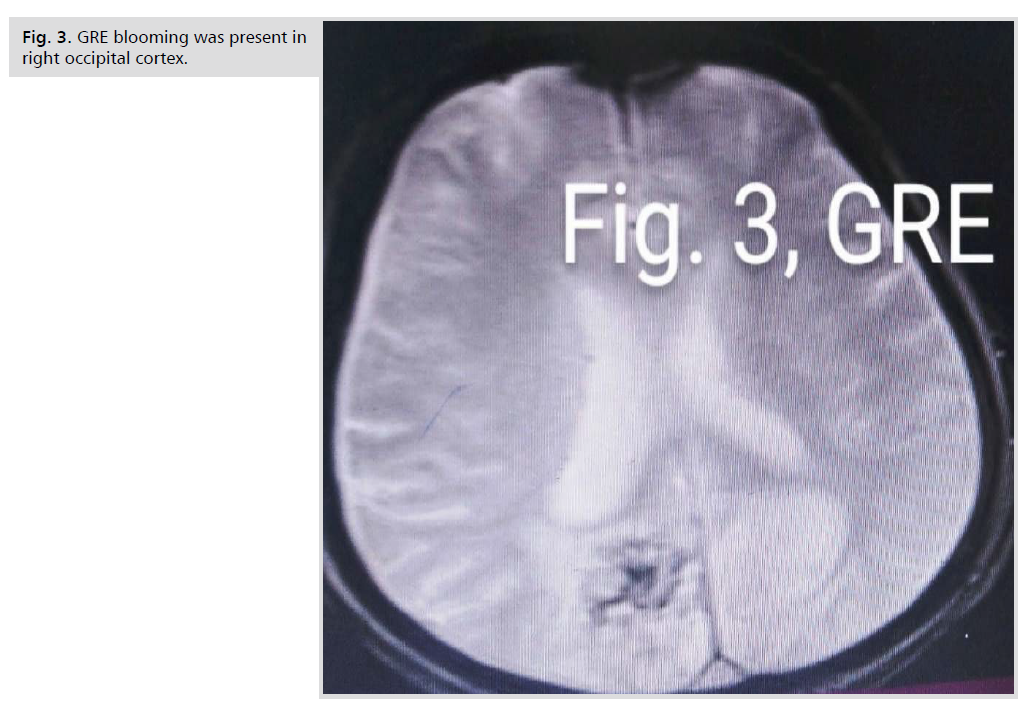
Fig 3: GRE blooming was present in right occipital cortex.
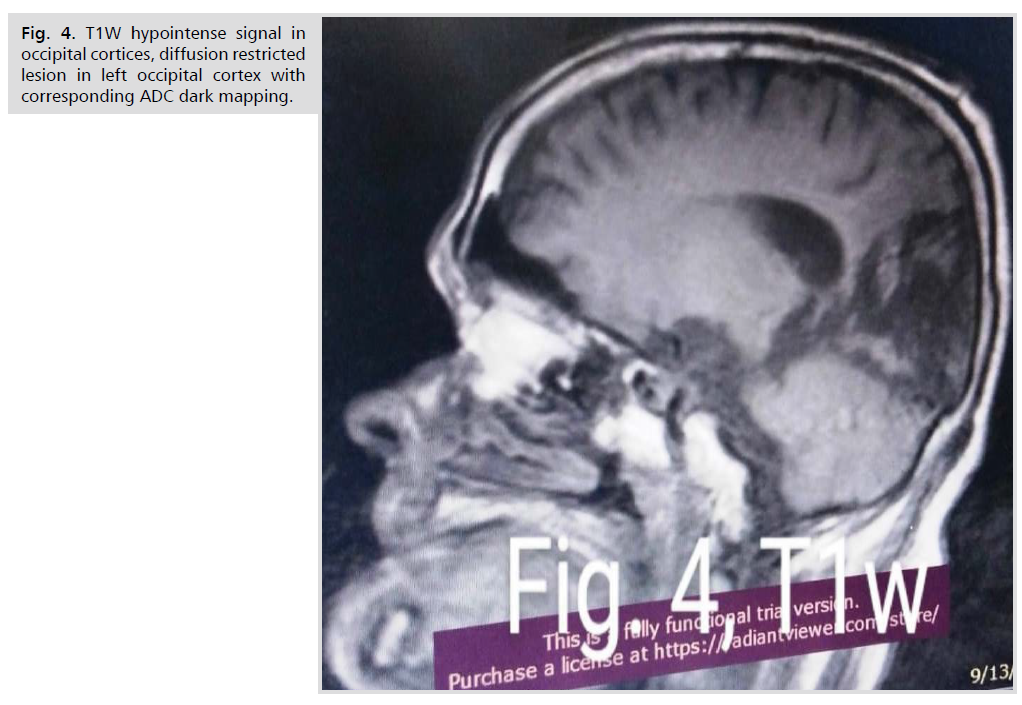
Fig 4: T1W hypointense signal in occipital cortices, diffusion restricted lesion in left occipital cortex with corresponding ADC dark mapping.
NCV (Fig. 5A.): Decreased CMAP amplitudes in
bilateral peroneal and tibial nerves with delayed conduction
velocities.
Sensory NCS (Fig. 5B.): Demyelinating sensory
neuropathy of upper limbs and axonal degeneration in
bilateral sural nerves.
VEP (Fig. 5C.): Absence of any potential.
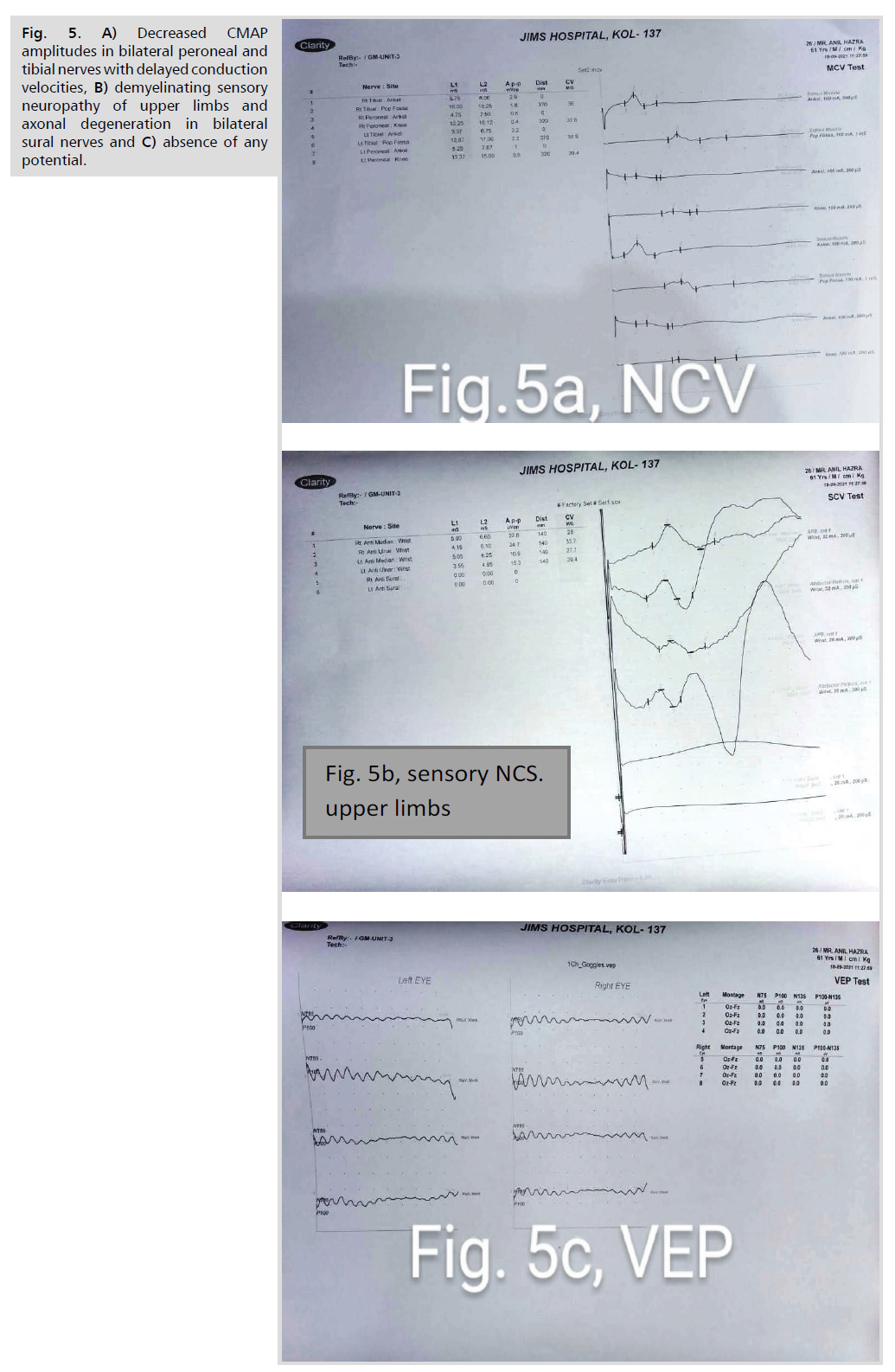
Fig 5: A) Decreased CMAP amplitudes in bilateral peroneal and tibial nerves with delayed conduction velocities, B) demyelinating sensory neuropathy of upper limbs and axonal degeneration in bilateral sural nerves and C) absence of any potential.
Provisionally diagnosed as Anton syndrome with
bilateral occipital lobe stroke (bilateral homonymous hemianopia) and visual anosognosia [4,5].
Treatment: Antihypertensives, inj insulin and oral
hypoglycemics, physiotherapy and counseling. After
about 10 days, he did not have confabulation and verbally
admitted his visual loss.
Discussion
Bilateral posterior cerebral artery stroke presenting
with visual anosognosia with denial of blindness in this
hypertensive, diabetic patient was diagnostic of Anton
syndrome.
He also had distal symmetric axonal polyneuropathy
in lower limbs with some associated demyelination
suggested by NCV study. This was most likely related to
his uncontrolled diabetes mellitus for prolonged period.
Conclusion
Cerebrovascular disease is the most common cause of
Anton's syndrome, and can be a potential complication
of uncontrolled diabetes mellitus. Any patient with diabetic cerebrovascular stroke should also be evaluated for
associated polyneuropathy.
Conflict of Interest
The authors declare no competing interests.
Acknowledgements
None.
REFERENCES
- Gopalokrishnan CV, Shrivastava A, Easwar HV, et al. Primary Ewing's sarcoma of the spine presenting as acute paraplegia. J Pediatr Neurosci. 2012;7(1):64-66.
Google Scholar, Crossref, Indexed at
- Kim JS. Posterior Cerebral Artery Disease. Stroke. 2022;pp:347-367.e6.
Crossref, Indexed at
- Nannoni S, Michel P. Thalamic and Other Posterior Cerebral Artery Stroke Syndromes. Post Circul Stroke. 2021;pp:67-84.
Google Scholar
- Kumral E, Zirek O. Major neurocognitive disorder followıng isolated hippocampal ischemıc lesions. J Neurol Sci. 2017;372:496-500.
Google Scholar, Crossref, Indexed at
- Kumral E, Bayulkem G, Ataç C, et al. Spectrum of superficial posterior cerebral artery territory infarcts. Eur J Neurol. 2004;11(4):237-246.
Google Scholar, Crossref, Indexed at