Research Article - (2022) Volume 0, Issue 0
Approach to patient Management In Critical Condition
Garcerant Campos Isaias1*,
Carmelo Duenas2,
Karen Perales3,
Tafur Delgado Juan E4,
Solano Gustavo Andres5,
Pulgarín Ospina Yohan E6,
Salcedo Gamarra Maria7,
Parodi González Yuli8,
Castro Ahumada Ronald9 and
Londono Andres Steven10
1Critical Care Specialist, Universidad Simon Bolívar, Barranquilla, Colombia
2Specialist in critical medicine and intensive care, Pulmonologist. University of Cartagena, Colombia
3Critical Care Specialist, Universidad Simón Bolívar, Barranquilla, Colombia
4Third year resident of Pediatrics. Universidad del Sinu, Colombia
5Critical Care Specialist, Universidad Simón Bolívar, Barranquilla, Colombia
6General Practitioner of the University of Antioquia, Medellin, Colombia
7General practitioner of the rafael nunez university corporation, Colombia
8General practitioner of the Universidad San Martin, Colombia
9Critical Care Specialist, Universidad Simon Bolivar, Barranquilla, Colombia
10General Practitioner of the San Martin University Foundation, Colombia
*Correspondence:
Garcerant Campos Isaias, Critical Care Specialist, Universidad Simon Bolívar, Barranquilla,
Colombia,
Email:
Received: 17-May-2022, Manuscript No. Iphsj-22-12783;
Editor assigned: 19-May-2022, Pre QC No. Iphsj-22-12783(PQ);
Reviewed: 15-Jun-2022, QC No. QC No. Iphsj-22-12783;
Revised: 20-Jun-2022, Manuscript No. Iphsj-22-12783(R);
Published:
27-Jun-2022, DOI: 10.36648/1791-809X.16.S7.957
Abstract
Behaviors in the critical care unit are the fundamental pillar to reduce the morbidity and mortality of patients; diagnostic accuracy and the development of attitudes and skills of health personnel should be the reason for success, however there is little literature that guides the work to meet the desired objective, This publication makes an approach by proposing an easy-to-remember and use strategy when a patient is in critical condition, the most common pathologies are included, their exact diagnosis and how the interdisciplinary group participates in the comprehensive management in the Intensive Care Unit (ICU).
Keywords
Critical pathologies; ICU Intensive Care Unit; Clinic; Driving
Introduction
The intensive care unit or more commonly known by its acronym
ICU, is part of the last link in a comprehensive system of care
for patients with life-threatening injuries or traumatic damage.
It is the place where patients are in critical condition presenting
pathologies of high complexity and sometimes with the possibility
of having a fatal outcome, in other words, in the intensive care
unit, there are people or patients in a very delicate state of
health; Their vital functions are severely altered, determining an
imminent danger of death, so that the possibility of losing their
lives is an important factor to take into account, even when there
is a possibility of survival, of those who survive a year, between
26 and 63% die; and 33% of them never return to work [1,4]. For
this reason, it is essential to emphasize that critical patients need
adequate management with especially warm and comfortable
care, since they are very vulnerable, especially because they are
facing a terrible disease with many discomforts derived from it,
adding, in most cases, the worry of their stay in the ICU [2, 3].
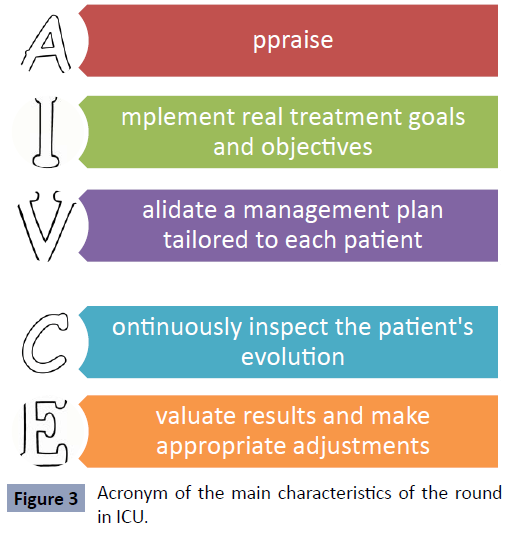
For this reason, and based on the acronym created by Jean Louis
Vincent "fast Hug Bid", we intend to demonstrate in this article
some key tasks in the attention, treatment and final measures of
medical practice and critical care. For this purpose, we propose
the acrostic "IN CRITICAL STATE" as shown in Table 1, which
allows to remember in a simpler way the elements to be taken
into account and that should be performed in the population in
question (Table 1).
| I |
infirmary |
| N |
nutrition |
| E |
scales de ingress UCI y prognostics |
| S |
Sedoanalgesia |
| T |
Roxboro filaxis |
| A |
ntimicrobianos |
| D |
diuresis y Depositions |
| O |
B tener balance |
| C |
abecera |
| R |
evisar catéteres |
| I |
nstaurar Metas |
| T |
earlier antiulcer as |
| I |
inotropicos/Vasoactivos |
| C |
control metabolic |
| O |
xigenación |
Table 1. Acronym of the elements to be present in the patient in ICU
Nursing
One of the important elements is the role of the nursing corps, since, the nursing professional has the ability to project and
sensitize to the point of knowing when and how much a certain
factor is stressful or not stressful in a patient, in addition, part of
the functions of nurses is the clinical care, within it, monitoring
the patient, compliance with medical treatment, performing
procedures, care planning, monitoring vital signs, scheduling
prevention of skin lesions, patient comfort, among others
that promote the maintenance of a stable condition or early
identification of possible complications [4]. In fact, they are very
close to the patient and interact with the patient's family, either by
providing information, explanation of procedures and education,
being in the duty to focus their attention on the bio-psychosocio-
spiritual needs, with individualized care, which manage
an ethic based on respecting the suffering of the other, being
sensitive to his pain, protecting him and his family and making
him feel as little as possible his disability or dependence [5-7].
However, individualized care guides the quality of care, with the
aim of reducing or eliminating negative factors, thus facilitating
the recovery process, reducing the length of hospitalization and,
consequently, the rates of nosocomial infections [8]. Likewise,
in this section, it is relevant to highlight the importance of
preventing falls in ICU patients, this nursing function in hospital
and geriatric units is very abundant, but research for specific ICU
patients is very limited that is why it is usually little mentioned
[9].
In the United States in 2017, more than 3,000,000 falls were
recorded, with age 65 years and older being a risk factor that
accounts for 85% of deaths after falling or, failing that, can
lead to post-fall complications such as fractures, which are
reported between 1-3% after the in-hospital fall, figures that
have undoubtedly increased over the years [10-12]. Additionally,
it should be known that the incidence of falls varies according
to the type of ICU from which they originate according to the
study carried out by Flanders et al. where patients derived from
a medical ICU fell with a fall rate of 52.9 falls per 1000 patients,
followed by neurological ICUs, where the rate was 40.1 per 1000
patients and the incidence of falls in those who came from a
surgical and coronary ICU was considerably lower, with 15.6 falls
per 1000 patients. However, we searched in databases such as PUBMED and several journals such as the NEJM, for predictive
scales that classified and detected patients at risk of falls in
the ICU, on which there seems to be no literature to date, and
although there are several scales such as Morse, STRATIFY,
Downton, Tullamore, and Tinetti that have been evaluated in
acute patients and rehabilitation wards, these are not superior
to clinical judgment to recommend it [13]. For all of the above,
it is more effective to include the risk of falling in the care of
ICU patients to avoid complications leading to death, which is
why meta-analyses to date with the available information seem
to recommend multifactorial interventions as a good strategy
to reduce falls, Among these strategies it is recommended to
identify risk factors inherent to the patient such as previous falls,
use of sedatives, hypotension, fragility, agitation, and impaired
control of urination, in addition, environmental factors such as
poor lighting, carpets on the floor among others that favor falls
should be considered [14,15].
Nutrition
Currently it is considered that nutritional support (NS) is part of
the protocol of care for critical patients, in fact in ICUs parenteral
nutrition (PN) is used in 6%, enteral nutrition (EN) in 72% and
mixed nutrition in 12.4%. Nutritional replacement should be
initiated 24-48 hours and generally 2 or 3 days are required to
progressively increase feeding until the necessary requirements
are reached [16]. During the stay in the ICU it is necessary to
understand that patients, due to the severity of their illness,
usually do not consume food like any other healthy person. For
this reason, there are different feeding routes that become more
important when the patient who is admitted to the critical care
unit has an inadequate nutritional status, which can worsen the
outcome and lead to major complications [17]. Although it is true
that the oral route should be preferred, it is not possible to use
it in all cases, and on the contrary, the enteral route will be used
if there is no contraindication; in fact, enteral nutrition (EN) is
the preferred nutrient supply route in critical patients. According
to standard practice and the recommendations of different
scientific entities, enteral nutrient delivery is preferable because
it has advantages such as the maintenance of the structure
and function of the intestinal barrier, as well as a lower rate of
metabolic complications related to nutrient delivery such as
hyperglycemia. Critically ill patients receiving EN have important
benefits compared to those treated with parenteral nutrition,
such as a lower frequency of infectious complications, shorter
hospital stay and even lower mortality. However, it is not true
to say that it is the only route that should be used, it all depends
on the reason for the patient's admission to the ICU, since there
are exceptions where NE cannot be used, such as >300 ml of
gastric residue, intestinal obstruction, malabsorption, fistula,
paralytic ileus, gastrointestinal ischemia, digestive hemorrhage,
digestive tract surgery, etc. In this case, nutrition is suspended for
6 hours and restarted at half the dose, in addition prokinetics will
be added for intestinal transit, a gastric residue value of 500 ml
can be recommended as a limit in ICU patients under treatment
with EN by nasogastric tube, this is used as an indicator of
tolerance of the diet, if finally it is not tolerated, nutrition will
be parenteral, preferably in the shortest possible time and only
for life in patients with short bowel, since this route brings with it important adverse effects; Gastroparesis should be avoided
because although it is not serious, these patients require much
more medical and nursing time and may change their prognosis
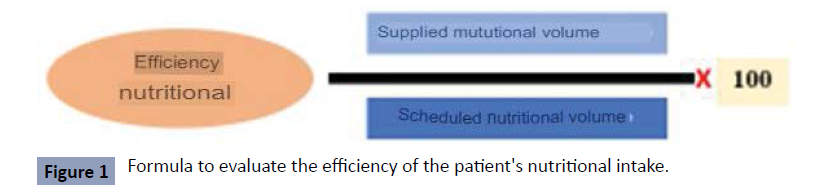
in the unit [18]. The efficacy of nutrient delivery is calculated
using the formula shown in Figure 1 based on the relationship
between the volume of nutrients received by the patients and
the volume prescribed according to the calculations made [19]
(Figure 1).
Figure 1: Formula to evaluate the efficiency of the patient's nutritional intake.
Source: Gonzalez, Juan Carlos Montejo, and Mercedes Catalán González. "New
systems for the implementation of nutritional support in ICU patients." Hospital
Nutrition 6.1 (2013): 60-67.
Initially, the goal of nutritional support in critically ill patients is
to maintain lean body mass, decrease catabolism and increase
nutrient intake within the limitations imposed by the different
degrees of organ failure [20]. The measurement of caloric
requirements and determination of the need for nutrition is
done through scales such as "NUTRIC SCORE", currently a total
of 25 kcal/kg is recommended in patients with BMI<30, for a
more accurate value some formulas can be used (MIFFLIN, PENN
STATE), this result will be distributed in the different nutrients
(CHOS 50-60% (7 GR/KG/DAY or 5MG/KG/MIN, LIPIDS 24-30% (1-
1. 5 GR/KG/DAY), PROTEINS 15-25% (0.8-2 GR/KG/DAY). Now, to
introduce these requirements in the enteral part, feeding tubes
are used, the most common ones include nasogastric tubes
(NG tubes) and gastrostomy tubes (G tubes) where the former
correspond to a non-surgical measure and the latter is purely
surgical. However, there are several types of feeding tubes
depending on how and where they are placed in the digestive
system as shown in Table 2, and in the enteral part, formulas are
used to replace food and supply proteins, carbohydrates, lipids
and other vital components for the body [21] (Table 2).
| Enteral route |
Parenteral route |
| feeding which carries nutrients to the stomach or intestine as liquid instead of solid food |
Feeding by supplying a special formula through a vein, which provides most of the nutrients the body needs. |
| Types of probes and their Access routes |
Access roads |
| 1. Nasogastric tube (NG tube). It is inserted into the stomach through the nose. The tube goes down the throat, through the esophagus and into the stomach |
|
| 2. Nasojejunal tube (NJ probe). It is similar to an NG tube, but continues through the stomach into the small intestine. |
1. Intravenous route: the preferred are the cephalic and the basilica in antecubital situation, not being recommended the veins of the lower limbs due to greater risk of thrombophlebitis. 2. Central route: The route of choice is the subclavian and in patients at risk in the placement of the catheter in the subclavian can be placed in the internal jugular. If the duration is not expected to exceed 12-15 days or direct puncture in large vessels is contraindicated, a catheter may be placed peripherally (brachial vein in the middle of the arm) and advanced to the superior vena cava (drum), but there is a risk of phlebitis and catheter bending |
| 3. Gastrostomy tube (G-tube). It is inserted through a small cut in the skin. The tube passes through the abdominal wall directly into the stomach. |
| 4.Gastrostomy-jejunostomy tube (GJ tube) it is inserted into the stomach as a G-tube, but continues through the stomach into the small intestine. |
| 5. Jejunostomy tube (J probe). Uses a small incision to place the feeding tube through the intestinal wall directly into the small intestine. |
Table 2. Frequent nutrition pathways in the ICU patient.
ICU admission scales and prognoses
Traditionally patients with severe processes, who have
developed pathophysiological alterations that have become
life threatening, are referred to the ICU for active assistance to
stabilize and achieve recovery. The admissions scales are based
on the American College of Critical Care and follow a variety of
categories as presented in Table 3, but are not limited to the
criteria described. Therefore, it is important to highlight some
recommendations including developing a cardiac and vascular
ICU design for the adult patient, diagnosis, parameters and
prioritization should be used for admission and admission to
the ICU. The request process should be addressed to the ICU
office with its respective date and time. It is also based on a
relationship with a high level of attention to the patient who
requires interventions or is in a serious clinical condition [22- 24]. Accordingly, all critically ill patients who require continuous
monitoring (every hour) or invasive monitoring or who require
interventions that cannot be provided in other services of the
institution should be attended at the Intensive Care Unit level
[25] (Table 3).
| (A) The Priority Model |
| Priority 1: Those unstable and critically ill patients, who require immediate monitoring and intensive therapy. As in the case of patients with ventilator support in the face of acute respiratory dysfunction. Patients who need treatment with vasoactive drugs due to shock or hemodynamic ally unstable |
| Priority 2: Patients limited to intensive monitoring and likely to require rapid investments. There is usually no therapeutic limit. In the case of patients with chronic diseases who develop serious surgical complications. |
| Priority 3: In this group are immersed patients who have few options to recover because of their initial disease, who are unstable and critical, therefore they can receive treatment to manage the acute disease without requiring essential cardiopulmonary resuscitation or intubation. As in the case of a patient with cardiac tamponed. |
| Priority 4: Those patients who did not receive any benefit from their stay in the ICU because their state of health does not merit it, or failing that, those who are in a clinical picture of terminal illness where death is irreversible. |
| B) DIAGNOSTIC MODEL |
| Circulatory system |
| • Cardiac arrest. |
| • Cardiogenic shock. |
| • Acute congestive heart failure with respiratory dysfunction and/or need for hemodynamic support. |
| • Hypertensive emergencies. |
| • Acute myocardial infarction (AMI) with complications. |
| • Unstable angina, with arrhythmias, hemodynamic instability, or persistent chest pain. |
| • Pericardial tamponade with hemodynamic instability. |
| • Aortic aneurysm dissection. |
| • Complex arrhythmias with hemodynamic instability or congestive heart failure. |
| • Complete heart block. |
| Respiratory system |
| • Acute respiratory dysfunction requiring ventilatory support or imminent intubation. |
| • Pulmonary embolism with hemodynamic instability. |
| • Massive hemoptysis. |
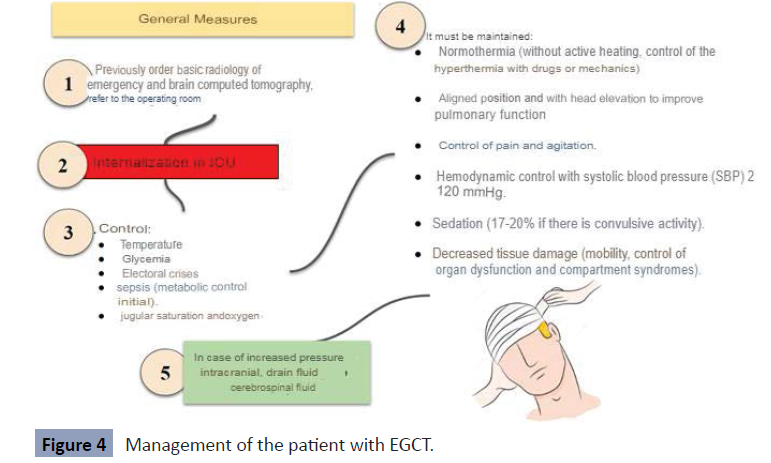
| Neurological disorders |
| • Coma: metabolic, toxic or anoxic. |
| • Acute stroke*. |
| • Meningitis with altered level of consciousness or dysfunction of another organ or system. |
| • Neuromuscular or CNS disorders and dysfunction of another organ or system. |
| • Status epilepticus. |
| • Brain death or its possibility in patients who could donate their organs. |
| • Severe head injuries |
| Poisoning |
| • Hemodynamic instability. |
| • Alteration of the level of consciousness with inadequate protection of the airway. |
| • Seizures. |
| Gastrointestinal disorders |
| • Vitally threatened gastrointestinal bleeding, including hypotension, angina, continuous bleeding, or coexisting pluripathology. |
| • Fulminant liver dysfunction. |
| • Severe pancreatitis. |
| • Esophageal perforation. |
| Endocrine |
| • Diabetic ketoacidosis complicated with hemodynamic instability, altered level of consciousness, respiratory dysfunction or severe acidosis. |
| • Thyroid storm or hypothyroid coma with hemodynamic instability. |
| • Hyperosmolarity with coma or hemodynamic instability. |
| • Adrenal crisis with hemodynamic instability. |
| • Severe hypercalcemia with altered level of consciousness, requiring hemodynamic monitoring. |
| • Hypo or hypernatremia with seizures or altered level of consciousness. |
| • Hypo or hypermagnesemia with hemodynamic involvement or arrhythmias. |
| • Hypo or hypercalcemia with arrhythmias or muscle weakness. |
| • Hypophosphatemia with muscle weakness. |
| Surgical |
| • Postoperative patients who require ventilatory support, hemodynamic monitoring or extensive nursing care. |
| Miscellany |
| • Septic shock or severe sepsis. |
| • Hemodynamic monitoring. |
| • Patients who need a lot of nursing care. |
| • Environmental accidents. |
| • Experimental treatments with potential complications. |
| C) MODEL OF OBJECTIVE PARAMETERS |
| vitals |
| • FC 150 beats pm. |
| • SAD < 80 mmHg or 20 mmHg below your usual TAM < 60 mmHg TAD >120 mmHg |
| • FR > 35 breaths pm. |
| • Severe hypo or hyperthermia |
| Laboratory values |
| • Na + 170. |
| • K+ 7 |
| • PaO2 < 50 mmHg pH 7.7 Glycemia > 800 mg/dL |
| • Calcemia > 15 mg/dL |
| • Toxic levels of drugs or other chemicals in hemodynamic or neurologically compromised patients. |
| Radiological signs |
| • Cerebral hemorrhage, contusion or H. subarachnoid with altered level of consciousness or neurological focus. |
| • Rupture of viscera, bladder, liver, esophagus or uterus with hemodynamic instability. |
| • Aortic aneurysm dissection. |
| • Electrocardiographic signs |
| • Sustained ventricular tachycardia or ventricular fibrillation. |
| • Complex arrhythmias that require close monitoring and treatment. |
| • Complete AV blockade with hemodynamic instability |
| signs (acute onset) |
| • Coma. |
| • Pupillary asymmetry in unconscious patient. |
| • Burned on more than 10% of the body surface (*). |
| • Anuria. |
| • Airway obstruction. |
| • Cyanosis. |
| • Cardiac tamponade. |
| Immediate postoperative period of the following Surgical Procedures |
| General surgery |
| • Esophaguectomy |
| • Duodenopancreatectomy |
| • Partial hepatectomy |
| • Pheochromocytoma resection |
| Thoracic surgery |
| • Chest Wall resections |
| • Major lung resecciones (pneumonectomy, lobectomia) |
| • Mediastinal resection or sternotomy. |
| Vascular surgery |
| • Abdominal aortic surgery |
| • Endovascular thoracic surgery: stents in aneurysms or in some chronic dissection. |
| • Intra-arterial fibrinolysis through catheter. |
| ORL |
| • Command (Tongue-based cancer) |
| • Skull base surgery |
| • Oropharyngeal tamponade due to bleeding (24-48 h) |
| • Prolongad post-surgical intubation (24-48 h) to avoid tracheostomy |
| • Interventions with potential airway involvement (e.g. stenosis |
| Urology |
| • Radical cystectomy |
Table 3. ICU patient admission models under American college of critical care criteria
Fuente: Ehikhametalor K, et al. "Guidelines for Intensive Care
Unit Admission, Discharge and Triage." West Indian Medical
Journal 68 (2019).
Once the critically ill patient has been admitted to the ICU, every
day different studies are carried out to evaluate his care and
progress in his state of health. Therefore, there are tools such
as scales that allow improving patient care, comparing variables and thus building a diagnostic and management criteria and, as
the name itself indicates, their prognosis, so that medical and
nursing staff can compare certain groups of patients and their
state of severity and consequently predict their clinical condition.
They are mainly translated into numerical values and assigned
to severity scales from variables. A mathematical equation is
then produced whose solution is the possibility of an outcome,
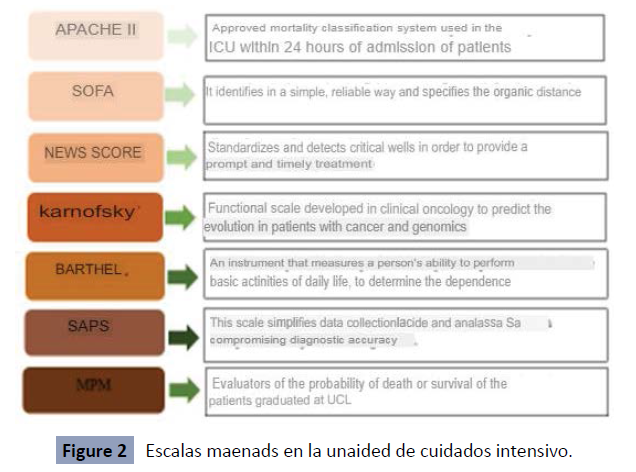
usually mortality [26]. In Intensive Care Units, 4 scales are mainly
used, although there is a great variety as shown in Figure 4: Acute
Physiology and Chronic Health Evaluation or APACHE, Simplified
Acute Physiology Score or commonly known as SAPS, Mortality
Probability Models or MPM and finally, among the most widely
used, the SOFÁ or Sequential Organ Failure Assessment. Acute
Physiology and Chronic Health Evaluation or APACHE arose in
1981 by William Knaus in response to the need to systematically
collect information on patients hospitalized in the ICU and to
improve their results. It allows the severity of patients to be
established through the study of 33 physiological variables
that express the magnitude of the disease and therefore the
prognosis. In 1985, APACHE II emerged, an updated version
based on 12 physiological variables to predict mortality, which
are assigned 0 to 4 points according to their standard deviation
from normality, which is scored as 0. This assessment is based
on the quantification of the acute state of severity of clinical and
biochemical parameters, which reflect the degree of alteration of
the cardiovascular, respiratory, gastrointestinal, renal, metabolic,
hematological and neurological systems. Thus, patients are
classified into 4 groups:
•Group A: Absence of previous functional limitation in patients.
• Group B: Mild presence of previous functional limitation in
patients.
•Group C: Moderate presence of previous functional limitation
in patients.
•Group D: Patients with severe previous functional limitation,
including patients confined to hospital institutions.
In 1991 APACHE III was introduced, it also has a scoring system
and a computerized predictive model, so software is required
to implement the predictive design. It includes variables similar
to the previous version and are the sum of an acute illness
component, which studies neurological, acid-base, vital signs and
laboratory test alterations, while a new variable was introduced
for surgical status. Finally, an update of APACHE IV was published
in 2006. The essential change consists of the introduction of new
categories. Most relevant to the accuracy of the APACHE IV model
was the successful use of risk-adjusted physiological variables,
since it demonstrated that mortality increased as physiological
variables were altered [27-29]. Since then, it has been very useful
in patients with acute cholecystitis, sepsis, cardiogenic shock,
among other clinical conditions [30-32].
The SAPS (Simplified Acute Physiological Simplified Score)
transforms its numerical value, by means of a logit function,
into the possibility of hospital mortality. This predictive scale
arises from the analysis of large series of cohorts of patients
with different medical-surgical diseases. Its main limitations are
its lack of individual prediction or its use on patient populations not included in the studies developed for its design or groups
of patients with specific diseases [33]. Conceptually, the SAPS 3
admission core comprises the following parts: First, the SAPS 3
admission score, represented by the sum of three subscores:
Box I: What we know about patient characteristics prior to
admission and ICU admission: age, previous health status,
comorbidities, location prior to ICU admission, length of hospital
stay prior to ICU admission, and use of major therapeutic options
prior to ICU admission.
Box II: What we know about the circumstances of ICU admission:
reason(s) for ICU admission, anatomic site of surgery, planned or
unplanned ICU admission, surgical status, and infection on ICU
admission.
Box III: What we know about the presence and degree of
physiologic disturbance on ICU admission (within 1 hour before
or after admission).
Secondly, the SAPS 3 Possibility OF DEATH over a defined time
span (in the situation of the primordial model, the possibility of
death at hospital discharge) [34]. Moreover, results from other
studies suggest that the SAPS III score has better predictive ability
than the APACHE II, according to the area under the curve and the
receiver operating characteristic curve: 0.81 and 0.80, respectively
[35]. For its part, the Mortality Prediction Model (MPM0) was
created to estimate the likelihood of in-hospital mortality
among ICU patients. Although this score is widely accepted, its
applicability in patients with primary cardiac conditions has not
been thoroughly evaluated [36]. In this situation, it is the model
used for the initial evaluation on admission to the ICU. It is based
on 15 easily available, changeable variables, since, with the
exception of heart rate and AT, the rest can be obtained from
the patient's clinical history. In relation to other models (SAPS,
APACHE, etc.), it has the virtue of being the only one that has a
tool to evaluate the feasible survival of the patient on admission,
since all the others are evaluated 24 hours after admission. In
addition, it is advantageous that it requires uncomplicated
changes or those that can only be obtained by means of previous
explorations or laboratory tests [37]. Therefore, the use of
MPM0-III will leave more accurate comparisons of actual versus
expected outcomes in functionality of the patient's condition at
the instant of ICU admission [38]. Because MPM prognoses are
based on the results of multicenter studies; 12,500 patients from
all over the world. Finally, SOFA: the Sequential Organ Failure
Assessment; uses basic measurements to calculate the failure of
major organs and assigns a severity score, so it is used to track
the patient's condition during ICU stay [26]. 6 scores are used
to measure the various critical systems of a patient: respiratory,
cardiovascular, hepatic, coagulation, renal and nervous systems.
It includes criteria that are simple and quick to calculate. With
2 criteria of the q-SOFA, the danger of sepsis is identified, and
actions such as rigorous monitoring of vital signs and laboratory
borders are taken [39,40] (Figure 2).
Figure 2: Escalas maenads en la unaided de cuidados intensivo.
Sedoanalgesia
Sedoanalgesia is an essential component of treatment for many
critically ill patients, especially those requiring mechanical
ventilation (MV), which helps to improve their health, decrease anxiety and facilitate certain procedures [41]. It is important to
keep in mind that sedation should be neither too little nor too
much, as both can cause potentially serious adverse effects.
On the other hand, insufficient neural regulation can lead to
severe arousal leading to myocardial ischemia, poor ventilator
adaptation, extubation or extubation or catheter removal,
associated with increased length of stay in the intensive care unit
(ICU), increased costs, increased morbidity and even mortality.
On the other hand, excessive sedation increases the duration
of mechanical ventilation and intensive care unit stay, which
increases the risk of complications, including MV-associated
pneumonia or neuromuscular alterations, promotes the increased
performance of neurological diagnostic tests that bring risk and
high costs, and a higher incidence of cognitive alterations. In
addition, the provision of higher doses of sedatives also involves
an inherent risk of producing adverse and toxic effects such as
hemodynamic, gastrointestinal, infectious, metabolic disorders,
withdrawal symptoms, etc. [42] For this reason, achieving an
adequate degree of sedoanalgesia to the pathophysiological
state of the patient and to the needs of ventilatory support is a
fundamental aspect of the correct therapeutic management and
evolution of the critically ill patient.
The measurement and adjustment of the level of sedoanalgesia
are key to ensure patient comfort and safety, avoiding pain,
agitation, withdrawal, delirium and delayed extubation.
Generally, conscious sedation with drugs such as fentanyl, remifentanil, propofol or dexmedetomidine is recommended
instead of sedative hypnotics in patients on noninvasive
mechanical ventilation or invasive ventilation in spontaneous
mode when extubation is planned, thus reducing days of ICU
stay, early extubation, reducing the frequency of delirium and
the need for some tracheostomies. Measuring the degree of
sedation is possible with different scales observed in Table 4,
such as the Richmond sedation-agitation scale "RASS" (Table 5),
the sedation-agitation scale "SAS" (Table 6), the motor activity
assessment scale "MAAS" (Table 7), and the Ramsay scale (Table
8); however, the RASS scale is recommended and Intensive Care
[43, 44] (Tables 4-8).
| Richmond Sedation-Agitation Scale (RASS) |
Sedation-agitation scale (SAS) |
Motor Activity Assessment Scale (MAAS) |
Ramsay scale |
| It mesures the sedation status of patients and is highly used in Intensive Care Units with patients under medical sedation. This scale was designad in 1999 at Richmond Hospital in the States of Virginia, United States. |
It was described by Riker in 1994 to describe agitation and sedation of both mechanically ventilated and unventilated critical patients. The description was for the use of haloperidol and was the first scale validated in critically ill patients |
Developed by Clement's group in Salt Lake City (Utah) in 1999 and derived from the SAS, it employs a clear and concise description of each category and classifies critical patients through their motor activity, as the main marker of sedation. |
First described by Dr. Michael Ramsey as part of a study on the effect of a steroid anesthetic and published in 1974, it is a subjective scale used to measure the level of sedation in patients, with the aim of avoiding insufficient or excessive sedation. |
Table 4. Scales to measure the degree of sedation
| Points |
Category |
Description |
| 4 |
Combative |
Openly combative or violent. Immediate danger to staff |
| 3 |
Very hectic |
Removes tube(s) or catheter(s) or has aggressive behavior toward staff |
| 2 |
Rough |
Unintentional frequent movement or patient-ventilator asynchrony |
| 1 |
Restless |
Anxious or fearful, but without aggressive or vigorous movements |
| 0 |
Alert and calm |
|
| -1 |
Drowsy feeling |
Not fully alert, but has stayed awake (more than 10 seconds) with eye contact, to voice (call) |
| -2 |
Light sedation |
Briefly, wake up with eye contact (less than 10 seconds) to the call |
| -3 |
Moderate sedation |
Some movement (but no eye contact) to the call |
| -4 |
Deep sedation |
There is no response to the voice, but to physical stimulation there is some movement |
| -5 |
Does not wake up |
No response to voice or physical stimulation |
Table 5. Richmond Sedation-Agitation Scale (RASS)
Source: Bartolomé, Santiago Mencía, and Rocío Tapia Moreno. "Scales of sedoanalgesia in the Pediatric Intensive Care Unit
| Points |
Category |
Description |
| 7 |
Dangerous agitation |
The endotracheal tube is torn off. Pull the catheters. Lash out at the staff. Throws himself out of bed |
| 6 |
Very hectic |
He is not calm, despite explaining it verbally, he requires physical restraint. Bite the endotracheal tube |
| 5 |
Rough |
Anxious or moderately agitated, trying to sit down. Calms down with verbal instructions |
| 4 |
Quiet and cooperative |
Calm, wakes up easily and obeys simple commands. |
| 3 |
Sedated |
Tendency to sleep, wakes up with verbal stimuli but goes back to sleep. Respond to simple commands |
| 2 |
Very sedated |
Responds to physical stimuli. Unable to communicate or obey orders. Has spontaneous movements |
| 1 |
Arreactive |
Minimal or no response to pain, does not communicate or obey orders. |
Table 6. Sedation-agitation scale (SAS)
Source: Tobar Almonacid, Eduardo, et al. "Protocol-guided sedation versus conventional management in critically ventilated patients." (2008).
| Points |
Category |
Description |
| 0 |
Non-reactive |
not respond to pain |
| 1 |
Pain response |
Opens eyes or locates pain or moves limbs to painful stimuli |
| 2 |
Responds when touching or talking to you |
Opens eyes or locates stimuli or moves limbs by touching or calling you |
| 3 |
Quiet and cooperative |
spontaneously, puts on sheets, obeys orders |
| 4 |
At rest and collaborator |
Does not require stimuli to move, obeys orders |
| 5 |
Rough |
Does not require stimuli to move, tries to sit or get up, does not obey orders |
| 6 |
Dangerously agitated |
Does not require stimuli to move, lashes out, tries to tear off probes, does not calm down when talking to him, does not obey orders |
Table 7. Motor Activity Assessment Scale (MAAS)
Source: Oliva Ramos, Alicia. "Sedation in flexible bronchoscopy. Study of the safety and efficacy profile in two work cohorts: Pneumology and Anaesthesiology." (2021).
| Points |
Category |
Description |
| 1 |
Awake |
Agitated, anxious, restless |
| 2 |
Awake |
Collaborator, quiet |
| 3 |
Sleepy |
Responds to verbal commands |
| 4 |
Asleep |
Responds to strong commands |
| 5 |
Asleep |
Responds to pain |
| 6 |
Asleep |
No response |
Table 8. Ramsay scale
Source: Duran-Nah, Jaime Jesus, et al. Knowledge and level of application of the Ramsay scale by Mexican nurses specializing in intensive care. Intensive nursing 17.1 (2006):19-27.
Thromboprophylaxis
Thromboprophylaxis is an important clinical care process in
healthcare institutions to prevent a venous thromboembolic
event (VTE), by means of tactics that allow its adherence in
hospital units. The main drugs available are shown in Table 9.
Hospitalized patients show at least one hazard element for a
venous thromboembolic event (VTE), of which about 40% show
3 or more hazard components. It is important to evaluate the
thromboembolic risk in each patient before deciding whether or
not to use preventive measures and, in parallel, which are the
most appropriate for implementation. The non-pharmacological
(mechanical) thrombo-prophylactic treatments currently used
are graduated compression stockings (GCS) and mechanical compression devices (MCD). The mechanism of action is to
minimize venous stasis of the lower limbs, simulating the
impact of muscle spasm and increasing the volume and speed
of venous flow. They are recommended in patients at high risk
of bleeding or as an adjunct to pharmacological measures.
On the other hand, pharmacological thrombo-prophylactic measures according to studies of unfractionated heparin
(5,000 IU subcutaneous), subcutaneous nadroparin reduces the
incidence of Severe Venous Thrombosis, enoxaparin showed
that the application of 40 milligrams every 24 hours significantly
reduces (63%) in VTE [45,46]. In specific situations such as major
orthopedic surgeries like Total Knee Arthroplasty (TKA), Total
Hip Arthroplasty (THA) and Hip Fracture Surgery (HFS), where
there is a high thromboembolic risk, it is also important to
evaluate the risk of bleeding. In addition to the pharmacological
options mentioned above, in these specific cases bemiparin,
fondaparinux, dabigatran, rivaroxaban, apixaban are used as
alternatives. In cases of hip fracture surgery, the same prophylaxis
mentioned above is recommended EXCEPT for the use of the
new oral anticoagulants (OAC) and dicoumarinics, which have
not been evaluated for this indication, so mechanical prophylaxis
is recommended. In cases of patients with knee arthroscopy
without a history of VTE or active neoplastic, it is suggested not
to use pharmacological thromboprophylaxis. The 2012 consensus of the American College of Chest Physicians on VTE prophylaxis
does not recommend the use of systematic prophylaxis in this
group of patients, because the risk of PTE is 0.3% and that of
symptomatic DVT is 2.4%. It is estimated that the incidence of
DVT in ICU patients varies between 25 and 32%, most of them
have a variety of risk factors for VTE and up to 5% already have
DVT at the time of admission to the ICU, as well as an increase in
hemorrhagic complications, Therefore, in this group of patients,
regardless of the reason for hospitalization, we suggest the use of
pharmacological thromboprophylaxis with LMWH or UFH, and in
the case of active bleeding or increased risk of bleeding, studies
suggest that mechanical prophylaxis with CNI (IC) or MCG (IIaC) is
effective [47]. Moreover, a systematic review published in 2015
states that of the LMWH used for thromboprophylaxis, both
tinzaparin and dalteparin are safe in patients with renal failure,
do not require dose adjustment, and do not bioaccumulate;
however, pharmacological thromboprophylaxis with enoxaparin,
bemiparin and certoparin shows accumulation in patients with Cl
Cr less than 30ml/min [48] (Table 9).
| Group |
Drug |
Dose |
Interval |
Route Of Administration |
|
Enoxaparin |
40 Mg |
24 H |
SC |
| Surgical And |
Nadroparin |
0.3 Ml |
24h |
SC |
| Orthopedics |
|
0.4 Ml |
24h |
SC |
| Column And |
Nadroparin |
0.4 Ml |
24h |
SC |
| Clinical |
|
0.6 Ml |
24h |
SC |
|
Bemiparin |
3500 UI |
24h |
SC |
| Moderate |
Heparin No |
5000 UI |
12h |
SC |
|
Fractional |
- |
- |
-- |
| High |
Heparin No |
5000 UI |
8h |
SC |
| - |
Fractional |
- |
- |
- |
| Fondaparinux |
2.5 Mg |
24h |
SC |
|
220 Mg |
24h |
ORAL |
| Dabigatran |
150 Mg |
24h |
ORAL |
| Rivaroxaban |
10 Mg |
24h |
ORAL |
| Apixaban |
2.5 Mg |
12h |
ORAL |
| Acenocumarol |
Individual Adjustment (International Ratio Normalized Between 2-3) |
24h |
ORAL |
| Aspirin |
160 Mg |
24h |
ORAL |
Table 9. Available drugs, dosages, application intervals and route of administration
Source: Javier Vázquez, f. e. r. n. a. n. d. o., et al. "Guía de recomendaciones para la prophylaxis de la enfermedad tromboembolica venosa en adultos en la Argentina." medicina (buenos aires) 73 (2013).
Antimicrobials
Hospital infection (IHD) is one of the most common complications
in health care and has been recognized to influence both
increased morbidity and mortality and hospitalization costs [49].
In icUs there are patients with disruptions in their mechanical
defensive barriers due to the use of catheters, tracheal tubes,
etc. In addition, they are more vulnerable to infections, especially
resistant bacteria that are usually transmitted between patients,
by hand-carrying or vectors. For this reason, the proper use of
antimicrobials is important to avoid possible complications such
as sepsis in the critical patient. Mortality from sepsis increases
from 56 to 78% when the antimicrobial initially administered
is not adequate [50]. For the correct and optimal use of these
drugs, a set of standards and strategies developed to improve the use of antimicrobials was created, this entity is known
as antibiotic policy. Patients in critical condition admitted to
intensive care services have special characteristics that justify
the use of antibiotics in a differential way to that of other
hospitalized patients, characteristics such as severity, pathogens,
and alteration of organs or systems. That is why in some ICUs
they propose standards as observed in Table 10, which promote
the appropriate use of antibiotics in critical patients [51] (Table 10).
| 1 |
Use antibiotics only when there is clinical or microbiological suspicion of an infection |
| 2 |
Obtain samples of infected tissues before starting antibiotic treatment |
| 3 |
empirical antibiotics using consensual therapeutic protocols |
| 4 |
Achieve a rapid response from the microbiology laboratory |
| 5 |
Select a targeted treatment when the etiology of the infection is known |
| 6 |
treatment effectiveness |
| 7 |
Monitor for the occurrence of adverse effects or multidrug-resistant emerging flora |
| 8 |
Limit the duration of treatment based on clinical or microbiological response |
| 9 |
Holding an intensivist physician accountable for the control, surveillance, and treatment of infections |
| 10 |
Co-responsible to all health personnel for adequate compliance with the rules |
Table 10. Basic rules for the use of antimicrobials in critically ill patients. Decalogue of standards.
Source: Lerma, F. Álvarez, et al. "Antibiotic Policy in Critical Patients." Intensive care 34.9 (2010): 600-608.
Table 10. Basic rules for the use of antimicrobials in critically ill patients. Decalogue of standards
Antibiotics should only be used for therapeutic purposes when
there is clinical or microbiological suspicion of infection, although,
in critical patients, it may be difficult to differentiate sepsis and
systemic inflammatory response syndrome, compared to other
inflammatory stimuli of a non-infectious nature such as trauma,
polyarthritis, pancreatitis, hemorrhage, among others that,
initially, occur with the same clinical expressiveness [52]. As for its
applications, there are three general applications that correspond
to experimental therapy, definitive therapy and prophylactic or
prophylactic therapy. Empirical treatment covers all probable
pathogenic microorganisms, since the causative agent is not yet
defined, therefore, a combination of several drugs proposed by
the doctor can be used or if a single broad-spectrum antimicrobial
is considered more appropriate; on the other hand, in the case of
definitive treatment, it is carried out when the causative agent is
identified, with a low-toxic and reduced spectrum antimicrobial
until the therapeutic scheme is finished and finally, in the absence
of a clear indication, prophylactic treatment is used, which uses
antimicrobials when the disease requires it and when there is
a probability that the treatment will be harmful to a serious or
potentially serious infection. Additionally, Table 11 contains the
most commonly used antimicrobials, however, to administer
some type as the scenario corresponds, the pharmacokinetics
and pharmacodynamics of the drug must be taken into account,
in order not to make errors in terms of adverse reactions,
duration of treatment, etc. [53] (Table 11).
| |
- Amoxicillin+clavulanic acid
- Ampicillin
- Ampicillin sulbactam
- Benzyl penicillin sodium
- Benzylpenicillin procainica
- Benzyl penicillin Benzathine
- Dicloxacillin
- Phenoxymethyl
- penicillin
- Oxacillin
|
| |
| B-lactamicos |
| |
| |
| Cefalosporin |
• Cephalexin
• Cefazolin |
• Cefuroxime
• Ceftazidime
• Ceftriaxone |
| Carbapenems |
• Imipenem + cilastatin
• Meropenem |
| Macrolides |
• Azithromycin
• Clarithromycin
• Erythromycin |
| Lincosamides |
• Clindamycin |
| Aminoglycosides |
• Amikacin
• Gentamicin |
| Sulfonamides with diaminopyrimidines |
• sulfamethoxazole + Trimethoprim |
| Quinolones |
• Ciprofloxacin |
| Tetracyclines |
• Doxycycline |
| Amphinenic |
• Cloranfenicol |
| Miscellany |
• Furazolidone
• Metronidazole |
• Nitrofurantoin
• Vancomycin |
| |
Table 11. Main antimicrobials
Source: Cordova Tacza, Isabel Rosario, and Maria Orejon Cuadros. "Incidence of reserve antimicrobials used in patients with Bacterial Resistance Hospitalized in ICU of the Ramiro Priale Essalud Huancayo National Hospital-2019." (2020).
Diuresis and bowel movements
Critically ill patients undergo important physiological changes
during their stay in the intensive care unit as a consequence of the
course of the disease. Monitoring hourly fluid intake and output,
urine flow control and urine characteristics during hospital stay is of vital importance in order to assess renal and circulatory
function, as well as transcutaneous loss by electrophoresis.
Diuresis depends on fluid intake and patient weight and in this
case hourly diuresis should not be less than 80 cc, in fact, diuresis
is a useful biomarker and continues to be so today, it is measured
in mL/kg/hour, considering oliguria or low production when it is
<0.5 mL/kg/hour for 6 or more consecutive hours [54] although
according to Mobeen Z. Haider and Ahsan Aslam in 2020, they
consider changing the definition to <0.3 mL/kg/hour for at least
24 hours [55,56]. A low urine output is recognized as an early
predictor of mortality in the intensive care unit when it is altered
in isolation, i.e. without increasing serum creatinine, compared
to those without acute renal injury 8.8% vs. 1. 3%, in addition
to increasing hospitalization times and costs [57] Within the
management approach for oliguria, volume replacement should
be initiated when the etiology is suspected and the maintenance
of adequate hemodynamic stability should be sought, and if there
is no response, a diuretic (furosemide 1-1. 5 mg/kg) and if urinary
production is less than 100 mL/hour in the following 2 hours, it
suggests with high sensitivity and specificity diuretic failure due
to lack of functional integrity of the tubule and risk of progression
of acute renal injury to advanced stages, reaching up to 75% of
those who required renal replacement therapy [58]. In the first
case, it refers to diarrheal processes, which represent a frequent
finding in critically ill patients, whatever the cause of their
admission to an ICU, generally through this parameter can be
reflected those gastrointestinal complications, not hemorrhagic,
more frequent that usually occur in such subjects causing hydro
electrolytic imbalances, interruption of enteral nutrition schemes,
malnutrition, worsening of the morbid condition, prolongation
of hospital stay, and even death, therefore, it is considered by
some authors as a factor of poor prognosis, which can prevent
the delivery of an adequate amount of nutrients by enteral route,
thus prolonging the days of hospitalization, and generating
greater morbimortality, in addition to an increase in the costs
related to medical care [59,60]. On the other hand, when bowel
movements are reduced, we speak of constipation, some authors
define it as the absence of bowel movements for 3 or more days,
for others 6 or more days, however, speaking of the ICU patient,
the best definition is "absence of bowel movements after 3
days from the beginning of enteral nutrition" [61]. Among the
conclusions of several studies it is suggested that constipation is associated with risk factors such as: sedation, analgesia, poor
motility or lack thereof, surgery, sepsis, delay in starting enteral
feeding, changes in motility induced by commonly administered
drugs, and considering that in the ICU it is difficult to eliminate
any of these factors from the beginning, it is important to suggest
to the reader to monitor this parameter during the follow-up
and monitoring of patients in the unit [62]. In short, diuresis
and bowel movements provide valuable information that can
evaluate the ICU patient's condition and prevent or treat possible
diseases or infectious processes.
Get balance
The objective of intensive care units is to take care of the patient's
life regardless of its severity, so it is important to train specialized
health personnel who can help to make an appropriate record
of the monitoring sheet of the water balance and adequate
care of patients; above all, it is necessary to be alert and make
a decision about the balance of fluids and electrolytes in order
to avoid at all costs complications derived from the alteration
of homeostasis that can cause renal injury, changes in the heart
rhythm and above all can compromise the life of this type of
patients [63]. It is for them that, keeping a record of daily and
accumulated balances, helps in making daily decisions, seeking
to impact for the benefit of the patient and more considering
that this is a modifiable variable as Anupama Upadya et al in
2005 suggested when seeing a possible relationship between a
previous positive daily and / or accumulated balance with failure
in some procedures that are vital for the critical patient [64]. And,
other antecedents such as the study of Boyd, John et al, in 2011
which found that when the positive water balance was increased
more than 3L in 12 hours, survival decreases, and having an
accumulated balance greater than 4 days presents a greater risk
of mortality in patients with septic shock [65]. Likewise, Claure-
Del Granado et al in 2016 report that a positive cumulative
balance or water overload is associated with higher mortality,
congestive heart failure, deterioration of intestinal function,
delayed scarring, and pulmonary edema [66].
For the monitoring of the balance, it is previously important to
take into account the weight of the patient in each shift, since this
allows assessing the income and discharges of the hospitalized
patient in the intensive care service [67]. Such information
must be contrasted with other data that also contribute to the
knowledge of the patient's hydro electrolytic balance, such as the
individual's clinic, the electrolytes present in plasma and urine,
blood gases, blood count and blood biochemistry [68]. For this, it
is important to recognize normal values according to age, sex and
BMI. Therefore, it is proposed by authors to use Table 12, to have
a daily, accurate record and make the necessary modifications to
avoid a positive accumulated water balance (over hydration) or
failing that, a negative accumulated water balance (dehydration)
(Table 12).
Weight |
| Income in 24 hours |
| Expenses in 24 hours |
| balance (Income-Expenses) |
| Accumulated balance (Total Income-Total Expenditures) |
Table 12. Balance sheet records.
Headboard
The posture of the head of the bed proved to be an efficient
measure to prevent pneumonia linked to mechanical ventilation
and for the functioning of the Neurocritical patient. The semiintegrated
posture of the patient on mechanical ventilation
(VM), with height of between 30 and 45° of the head, decreases
the incidence of aspiration and secondary pneumonia [69]. A
study that quantified the hours of the bedside ≥ 30° of patients
with mechanical ventilation, its results showed that the mean
of theoretical hours that patients should remain at ≥ 30° was
21h15'(3 h), and the real ones, of 14 h (5 h) (p < 0.001) [70].
Underlying the fact that the group of critically ill patients staying
in the ICU often needs a machine to help maintain breathing.
However, this could leave sequelae such as ventilator-associated
pneumonia so the bedside position can prevent infection, so
moderate-quality evidence from eight studies involving 759
participants showed that the semi-lying position (30° to 60º)
reduced clinically suspected ventilator-associated pneumonia by
25.7% compared to the supine position from 0° to 10°. However,
sufficient evidence to draw definitive conclusions on other
outcomes and the comparison of alternating semi-recumbent
positions does not remain accessible. Adverse events, especially
venous thromboembolism, were underreported [71].
Catheter review
Bloodstream infection associated with the central catheter is
defined as a primary bloodstream infection. Recommendations
for the prevention of sepsis generally refer to two well-defined
procedures to consider: 1) the introduction of central vascular
equipment and 2) their care or maintenance. Therefore, postimplantation
surveillance lies in the control of blood pressure
every 2 hours for the first 8 hours and check for bruises in the area
of pressure. If they occur, compress and apply the cooler locally.
Monitor bleeding regularly, keep the head of the bed elevated
if you tolerate it for the first 6 hours, administer analgesics as
prescribed if the patient needs them, change the sterile dressing
after 24 hours, and check the status and level of fluid retention.
In addition, each lumen should be sterilized and the catheter
with smaller diameter lumen should be used as far as possible
[72, 73]. This is important since, the 2018 nosocomial infection
incidence study in Spain (EPINE) considered vascular catheterassociated
sepsis as the fourth (15.17%) cause of nosocomial
infection (NI), after respiratory, surgical and urinary infections.
Although it ranks fourth, vascular catheter-related NI can be
considered among the most serious, with deaths ranging from 25
to 60% of cases. So studies suggest that proper hand hygiene is
required before and after any operation using a vascular catheter
access point, such as sterilization or removal. Please note that
the use of gloves does not affect the operation. The use of
chlorhexidine for disinfection prior to catheterization and each
dressing change with the corresponding therapy is reasonable
and should be done systematically. The reduction of the sepsis
rate will be achieved through the use of septal measures in the
management of catheters and the implementation of aseptic
technique with sterile barriers such as hats, gloves, gowns,
masks and clothing. This will help us achieve our goal, which is to
reduce the number of catheter manipulations and make only the most necessary connections. In addition, eliminate unnecessary
central vascular catheters and reduce the number of days our
patients use the above devices [74, 75]. Following this model and
with the aim of reducing the incidence of catheter-associated
sepsis in Spanish intensive care units, the Spanish Society of
Intensive Care Medicine and Coronary Artery Units (SEMICYUC)
collaborated with the WHO Global Alliance for Patient Safety to
develop the Bacteremia Zero project [76].
Set goals
This point refers to the establishment of final parameters that
promote the improvement of the patient, that is, propose
treatments, processes, strategies and others to return to the
normal values of the patient and seek homeostasis. Considering
the heterogeneity of the disease of patients in ICU, it is evident
that each patient must be prepared exclusive goals that improve
their specific condition; however, there are goals that can be
addressed in a general way by the existence of specifically
established parameters. That is why, setting the scene in front of
an adult patient, the following goals are proposed.
• Glycemic target: between 140-180 mg/dL (see metabolic
control below).
• Mean arterial pressure (MAP) goal: An adequate
MAP should be monitored in patients in the ICU and then it is
not proposed to classify a MAP for each diagnosis, but to set a
minimum MAP that serves as an alert to take early behaviors in
favor of the patient. In healthy people, a MAP <50 mm Hg begins
to compromise the self-regulation of cerebral blood flow with the
consequent decrease in cerebral perfusion [77]. It is therefore
proposed that in patients following successful cardiopulmonary
resuscitation and septic shock, a MAP≥65 mm Hg through the
use of fluids and/or vasopressor such as norepinephrine [78].
The SEPSISPAM study found no difference in mortality between
low target 65-70 mmHg and high target 80-85 mmHg, however,
in hypertensive patients with high target, they had less renal
impairment and need for renal replacement therapy and having
low goals had less frequency of atrial fibrillation [79]. Therefore,
the initial goals are to maintain a mean arterial pressure of 65 to
84 mmHg with systolic blood pressure not less than 90 mmHg,
a cardiac index of 3 l.min.m2, with central venous pressure of
8-12 mmHg and pulmonary capillary pressure of 12-15 mmHg.
By laboratory tests, hematocrit greater than 30%, serum lactate
levels less than 2 mg and venous oxygen saturation greater than
70% [80].
• Oxygen saturation target: Values between 88-95% [81]
are recommended, higher goals were associated with worse
clinical outcomes, including death and longer ICU time in patients
with ARDS [82].
• Goal of minimizing risk of ulcers: To do this, you should
opt for changes of position from time to time (See pressure ulcers
in anti-ulcer therapy)
• Infection Avoidance Goal: Proper compliance with
biosecurity regulations must be carried out, in order to limit
possible transmissions between health personnel and patients,
and even between patients, in addition, the use of antimicrobials is recommended (Check section on antimicrobials)
• Nutrition Goal: The primary goals of nutritional support
for critically ill patients are to maintain lean body mass, reduce
catabolism, and increase nutrient intake within the limits of
use with varying degrees of organ failure. ( Check the nutrition
section)
• Water Balance Goal: Procure homeostasis, Avoid
positive accumulated balances or negative accumulated balances
(Check the section obtaining balances)
Anti-ulcer therapy
Pressure ulcers (UPPs) are a common, arduous-looking problem in
hospitalized patients. This requires constant vigilance by experts
who cannot afford the challenge of preventing and treating it.
Once the ulcer is established, it increases the morbidity and
mortality of patients and slows down the healing process. In
addition, among those admitted to intensive care that required
mechanical ventilation (MRA), the presence of PPL was identified
as an independent predictor of mortality [83]. These ulcers are
localized damage to the skin and/or underlying tissue, which
often protrudes above the bone, due to the pressure or pressure
associated with the breastbone. Sometimes it can also appear
in soft tissues under external pressure by various materials or
examination equipment. Therefore, 20 mmHg can be considered
the maximum capillary occlusion pressure. Once a pressure
greater than 20 mmHg is generated in a confined area and over
a long period of time, the ischemia process begins to block the
supply of oxygen and nutrients, causing the blood vessels to
deteriorate. Tissue damage due to anaerobic respiration, which
induces changes in the cell membrane and the release of active
amines which, if not reversed over time, leads to necrosis and
death of cells in this region [84, 85]. The GNEAUPP proposes
to classify UPPs as shown in Table 13. Among the tools for the
early detection of UPP risks, we have the Braden Scale (Table
14), which is based on 5 risk factors: sensation, humidity, activity,
movement, nutrition, friction and shear. With scores ranging
from 6 to 23, remember that the lower the score, the higher the
risk [86, 87]. However, some studies conclude that the Braden
scale shows predictive insufficiency and poor accuracy for both
a cut-off point of 18 and 16, which are accepted in the different
clinical scenarios [88] (Tables 13 and 14).
Category I: Non-bleachable erythema |
The skin is intact with non-bleaching redness of an area usually located on a bony prominence. The affected area can be painful, firm, soft, and hotter or colder compared to adjacent tissues and may be more than 15mm in diameter. |
| Category II: Partial thickness ulcer |
Partial loss of the thickness of the dermis, presenting as an open superficial ulcer with a pink-reddish base and without erosion. This category does not include injuries caused by adhesives, abrasions, or tears on the skin. |
| Category III: Total loss of skin thickness |
Complete loss of skin tissue. Subcutaneous fat is visible, but no bones, tendons, or muscles are seen. There may be scabs and/or necrotic tissue that does not mask the depth of tissue loss. These can be compartments and/or tunnels. |
| Category IV: Total loss of tissue thickness |
There is a total loss of tissue thickness with exposed bone, tendon, or muscle. They may have sfacements and/or necrotic tissue. It is often associated with cavitations and/or tunneling. |
Table 13. Classification of Pressure Ulcers
| |
1 POINT |
2 POINTS |
3 POINTS |
4 POINTS |
| Sensory Perception |
Completely Limited |
Very Limited |
Slightly Limited |
No Limitation |
| Exposure To Moisture |
Always Wet |
Often Wet |
Occasionally Wet |
Rarely Wet |
| Physical Activity Wandering |
Scaling |
In Chair |
Wander Occasionally |
Wander Frequently |
| Mobility Postural Changes |
Motionless |
Very Limited |
Slightly Limited |
No Limitation |
| Nutrition |
Very Poor |
Probably Inadequate |
Adequate |
Excellent |
| Shear And Rubbing |
Maximum |
Potential Risk |
No Apparent |
- |
| Rubbing |
- |
Risk |
Risk |
- |
Table 14. Braden scale
Source: villamea, Silvia martínez, and Beatriz brana marcos. "Prevention of pressure ulcers in the care of patients placed in prone position. Lessons derived from the covid-19 crisis.'' Jan Journal of Nursing 15.1 (2021).
The main goal of treating UPPs is to find a way to cure or close
them as quickly as possible. The first thing to get is a clean
granulation fabric. To achieve this, you must follow these steps
[89].
• Establish prevention measures to prevent the emergence of
new UPPs.
• Debridement of devitalized tissue and, if necessary,
extensive debridement under surgical intervention.
• Management of infection where necessary.
• Control pain, secretions, and odors.
The treatment has several dimensions. In patients in good general
condition, ulcers can heal well with topical treatments. Use of
platelet growth factors to stimulate the formation of granulation tissue. The fastest methods yielded very varied results. In
circumstances where there is the impossibility of closing, a surgical
treatment is chosen, focused on a reconstructive technique
with cutaneous, fasciocutaneous or randomized muscle flaps
according to the patient's conditions. In addition, the application
of stem cell cultures induced by platelet mediators to accelerate
the healing of pressure ulcers of torpid evolution open a totally
new field and a future to be able to definitively cure these ulcers
without going through surgery [90]. Therefore, a summary of
evidence gives indications on critically ill patients; reported that
exercise every 2 hours may not reduce the risk of developing
pressure ulcers compared to exercise every 4 hours, but may
increase the risk of adverse events in adults requiring mechanical
ventilation (at level 2 [moderate]); this recommendation is based
on a randomized clinical trial, conducted in a Spanish hospital with
330 adults, all of whom had special surfaces for active pressure
management and required invasive mechanical ventilation for 24
hours. Eligible participants are randomly assigned to fill every 2
hours (n = 165) or every 4 hours (n = 164). The primary endpoint
was the occurrence of at least one grade 2 pressure ulcer during
intensive care unit stay [91]. New evidence proposes that olive
oil is shown as an alternative to hyper oxygenated fatty acids
for prevention since they are equally effective in prevention and
with respect to the use of dressings prophylactically, hydrocolloid
dressings and transparent polyurethane dressings show greater
effectiveness [92].
Additionally, gastric ulceration in critically ill patients should
also be taken into account as these can cause exponential
and permanent damage to the gastric mucosa, increase the
incidence of clinically significant gastrointestinal bleeding,
prolong hospital stay in the intensive care unit and increase the
risk of death. To prevent these types of complications, there
are several pharmacological options. Some studies have shown that 75% of patients in the intensive care unit develop gastric
mucosal abnormalities within a few hours of admission [93]. It
is known that patients with shock, sepsis, severe burns, severe
trauma, or traumatic brain injury may have ulcers or stress
gastritis [94]. Its main component is splanchnic hypo perfusion;
however, progressing to a more significant lesion requires an
associated acidic medium. Other agents involved are the release
of catecholamine’s and subsequent reperfusion with free radical
release and increased nitric oxide levels [95]. We group patients
into four categories: low risk, moderate risk, high risk, and highest
risk. In patients at higher risk (>8%), PPIs and H2RAS reduce
clinically important bleeding by 3-5%. In critically ill patients at low
risk (<2%), PPIs and H2RA reduce clinically important bleeding by
less than 1% [96]. The modification of gastric pH as a prophylaxis
against gastric bleeding in critical patients, which decreased the
incidence of this entity and became a routine practice in intensive
care units; multiple studies were subsequently conducted to
try to establish which patients benefit most from this measure.
Gastric acid suppression with proton pump inhibitors (PPIs)
or histamine-2 receptor antagonists (H2RAS) is commonly
performed to prevent gastrointestinal bleeding in critically ill
patients. Existing guidelines vary in their recommendations on
which population. Histamine H2 receptor inhibitors (Ranitidine)
their mechanism of action is based on binding to the histamine
receptor in the parietal cell to inhibit gastric acid secretion;
reduces hydrogenion concentration and gastric volume. Proton
pump inhibitors (omeprazole) are drugs that block acid secretion
by irreversibly binding to the cysteine residue from the H+/K+
ATPase pump found on the luminal face of the parietal cell [97].
Onotropics/vasoactives
Many patients admitted to the ICU will need to use vasopressors
during their stay in the unit. These agents can be broadly classified as vasopressors, which increase blood pressure, and
inotropics, which improve myocardial function, while improving
oxygen availability and reducing tissue ischemia and organ
failure, due to their effect on the caliber of blood vessels (dilation
or contraction). Some patients will need both medications at the
same time or at different times during their hospital stay. They
are used daily in the treatment of hemodynamic instability in
critical patients in the intensive care unit. The different drugs
have an inhibition or stimulation effect on different receptors,
therefore the response will be specific according to the required
objective as in the case of sympathomimetic, in addition to these,
and there are phosphodiesterase III inhibitors, prostaglandins,
vasopressin antagonists, and calcium sensitizers [98]. In the case
of sympathomimetic have effects on α-1 receptors that cause
smooth muscle contraction, glycogenolysis and gluconeogenesis,
α-2 receptors decrease the production of aqueous humor and
insulin secretion. The β-1 increase frequency, contractility and
cardiac conduction while there is an increase in renin secretion.
The effects on β-2 are relaxation of bronchial, gastrointestinal,
uterine, bladder and vascular smooth muscle in skeletal muscle,
hepatic glycogenolysis and skeletal muscle. Finally, there is δ,
which causes smooth muscle relaxation in renal, splanchnic,
coronary and cerebral arterioles [99]. The drugs supplied are
shown in Table 15, with the aim that critical patients restore
and maintain adequate tissue oxygenation, since tissue hypoxia
plays an important role in the development of multiple organ
dysfunctions, a frequent cause of death in the critical patient
population [100] (Table 15).
| Drug |
Dosis Típica |
β-1 |
β-2 |
α |
| Isoproterenol |
0,01-0,1 µg/kg/min |
+++ |
+++ |
0 |
| Norepinephrine |
0,05-1 µg/kg/min |
++ |
0 |
+++ |
| Epinephrine |
0,05-2 µg/kg/min |
+++ |
++ |
+++ |
| Phenylephrine |
0,5-5 µg/kg/min |
0 |
0 |
+++ |
| Dopamine |
1-5 µg/kg/min |
+ |
+ |
+ |
| Dopamine |
5-20 µg/kg/min |
++ |
+ |
++ |
| Dobutamine |
2,5-20 µg/kg/min |
+++ |
+ |
´+ |
Table 15. Inotropic/Vasoactive Drugs Used in the Critically Ill Patient
0: no effect; +: minimal effect; ++, moderate effect; +++, substantial effect
Source: Lovesio, Carlos. "Intensive medicine. Chapters 1 through 90." (2008).
Metabolic control
Dysglycaemia in acute patients (hyperglycemia, hypoglycemia,
variability and duration of glycemia) is an indicator of the severity
of severe disease in relation to mortality. However, this effect
appears to be weak in diabetic patients. Diabetes, especially in
people who had poor glycemic control before the disease, is
known as the "diabetes paradox." Changes in glucose metabolism
during severe illness are caused by a variety of factors, including
increased insulin resistance, impaired insulin production, and
cytokine activation. In critically ill patients, the hyper metabolic
state shows a strong activation of anti-regulatory hormones
and cytokines, such as tumor necrosis factor alpha (TNF-α),
interleukin-1 (IL-1) and interleukin-6 (IL-6), is an important
mediator of insulin resistance and, therefore, hyperglycemia.
Stress-induced hyperglycemia is a common disorder in hospitalized patients without pre-existing diabetes Diabetes
mellitus (DM), defined by fasting blood sugar above 126 mg/dL
or results greater than 200 mg/dL. High blood glucose levels are
associated with increased morbidity and mortality in patients with
burns, surgery, stroke, acute coronary syndromes, and traumatic
brain injury. Intravenous insulin therapy is suggested in this group
of patients, once a multidisciplinary team has made the decision.
In turn, the authors differ in the definition of hypoglycemia in the
intensive care unit, but patients with levels below 70 mg/dl were
taken into account. Associated symptoms include headache,
weakness, altered state of consciousness, sweating, seizures,
and others. Risk factors for its development are sepsis, diabetes
mellitus, and severe severity of the disease, kidney damage or
liver dysfunction, the need for a vascular plug, discontinuation
of therapeutic feeding during insulin infusion. The third domain
of glycemic control in ICU is given by the variability of glycemia.
Blood glucose levels in critically ill patients fluctuate widely, even
when continuous feeding and insulin infusions are used, this
is an independent risk factor for Intensive Care Unit Mortality,
usually expressed as the standard deviation (SD) of the mean
glycemic value or the mean amplitude of glycemic fluctuations.
Time in target range has been introduced more recently as the
4th domain or "unifier" domain (TERO) of disglycemia in ICU,
this is defined as the time accumulated in the target range and
represents the percentage of time your blood sugar level is in the
target range. The presence of a TERO above 70% is statistically
significantly related to an increase in survival in critical disease
[101-103].
Oxygenation
Oxygen transport in critically ill patients is often affected because
the coping mechanisms to maintain an adequate tissue supply
can become inadequate, so assessment and correction are
essential. Therefore oxygen has become the cornerstone in
critically ill patients, in the literature it is estimated that up to
15% of hospitalized patients received supplemental oxygen, to
avoid complications such as hypoxemia and cellular hypoxia. In
clinical practice, the main objective of oxygen therapy is to avoid
hypoxemia in critically ill patients, the recommendation of the
British Thoracic Society (BTS) for titration is based on ventilator
insufficiency and hypercapnia, especially in clinical pictures
of cardiac arrest or resuscitation, shock, sepsis, major trauma,
anaphylaxis, major pulmonary hemorrhage, severe head injury
and carbon monoxide poisoning. However, care must be taken
not to exceed the adjustment for the appearance of hyperoxia
PaO2 >16 kPa (equivalent to >120 mmHg) and FiO2 >0.21, can
lead to serious adverse effects on inflammation, oxidative stress,
lung function, micro vascular perfusion and coronary and cerebral
blood flow [104, 105]. In addition, conservative use of oxygen was
associated with a decrease in infection (bacteremia) (RAR 5%,
95% CI 0-9%, p = 0.049) and a decrease in the incidence of shock
episodes (RAR 6.8). 95% CI 2-12%, p = 0.006). In a patient with
acute respiratory failure, in addition to treating the underlying
disease, there are two treatments that cause an immediate
increase in PaO2 (and SatO2): oxygen administration and excess
pressure. The latter mainly depends on the level of the profile,
which largely reflects the severity of the ventilation support.
Thus, to reverse hypoxia in patients on mechanical ventilation, we can increase FiO2 and/or PEEP, while conducting diagnostic
studies to reverse the cause In one study they concluded that
the main prognostic factors of oxygen therapy in critical patients
were: oxygen blood pressure, total oxygen concentration, P50, Px
index (reflects the suitability of the contribution of arterial blood
to the oxygen supply to the cells), tracheostomy and orotracheal
intubation.
Characteristics Of The Round In ICU
In the ICU round, initially a series of rehabilitation processes
of the patient must be carried out, this process is divided into
5 phases, which, in this review, we propose the acronym "LIVE"
as seen in Figure 3. In the first case, having a patient in the
ICU, the health situation of the internalized individual, his level
of functionality and the deficits he presents, as well as some
limitations to carry out certain activities of daily living, must be
assessed. In addition, treatment objectives and goals should be
implemented in favor of patient improvement, the validation of a
management plan adjusted to the specific needs of each patient,
monitor the patient's evolution and, above all, evaluate results,
reevaluate and make adjustments that are considered pertinent
(Figure 3).
Figure 3: Acronym of the main characteristics of the round
in ICU.
Source: authors of this study
Speaking of the duration of the round, each shift has a duration
of 12 hours; are divided into Day Shift (7AM – 7 PM) and Night
Shift (7PM –7AM 9), Once each shift is reached, the initial activity
carried out by the incoming doctor, is the reception of the shift
to the outgoing partner, thus, with the delivery and receipt of
each shift, the continuity of patient care by the medical staff is
guaranteed as well as the existence of the necessary elements
for their care
Diagnostic Accuracy Of The Patient In Icu
The great challenge in the ICU is to face the heterogeneity of
patients, taking into account the complexity and ambiguity that can occur in different syndromes and critical diseases,
which are why the diagnostic accuracy in this group of patients
becomes somewhat complex and even the health professional
body can act in an imprecise way. For the attending physician
there are multiple challenges that must be taken into account
when making decisions about the approach and therapy of each
patient, among the most common challenges are infrastructure,
availability of diagnostic resources, the identification and
execution of urgent interventions, ethical dilemmas and
assertive communication with the patient's relatives to explain
the clinical status. Diagnostic precision goes hand in hand with
interdisciplinary and team work; where nursing staff, respiratory
therapy, physiotherapists, general practitioners and specialists
must act synchronously and safely around the same goal, a
systemic and holistic approach of each patient. Likewise, in this
article, we highlight the management and treatment of the main
pathologies that are usually grounds for hospitalization in the
intensive care unit.
Frequent neurological pathologies in the patient
in icu, treatment and proper management
Neurological diseases represent an important part in intensive
care units, especially when talking about the pediatric population
(PICU) where they are considered a cause of morbidity and
mortality. Neurological patients in the ICU may be internalized as
a result of a wide variety of pathological conditions that require,
due to their lethality and severity, medical care with permanent
monitoring. In the case of adult patients, diseases such as
cranioencephalic trauma and cerebral vascular disease usually
occur, which include ischemic, hemorrhagic, anoxia and brain
death conditions. In addition, other conditions such as infections
of the central nervous system can also occur, where meningitis
is very common.
Cranioencephalic trauma: This pathology is defined as physical
injury or functional deterioration of the cranial contents due to
a sudden exchange of mechanical energy. There are different
types of TBI ranging from mild to severe, however, the patient
with severe traumatic brain injury (GTCT) constitutes a global
pandemic and one of the leading causes of death and disability,
especially in young adults. It is characterized by a high complexity,
so it is important that an adequate specialization in care is
maintained. Pathophysiology, monitoring and familiarization
are paramount to provide quality care and promote patient
safety, thus reducing adverse effects and fatal consequences in
such a population. Therefore, it is essential to carry out general
measures such as those mentioned above throughout this
research, as well as the performance of the basic care used in
patients with cranioencephalic trauma.
For management is included what is proposed in the acronym "IN
CRITICAL CONDITION" in addition, a very detailed neurological
control is recommended that includes an initial assessment of the
levels of consciousness, in fact, severe cranioencephalic trauma
(EGCT) is considered to those patients who present a score on
the Glasgow Scale less than or equal to 8 points within the first
48 hours after the accident, additionally, an examination of the
pupils is recommended; as well as monitoring of intracranial pressure, tissue oxygen pressure, jugular saturation, and
Spectral monitoring (Table 16). This aspect is essential to avoid
complications and mitigate secondary damage at the brain level.
(Figure 4).
Figure 4:Management of the patient with EGCT.
Taken and modified from: López, Emilio Alted, Susana Bermejo Aznárez, and
Mario Chico Fernández. "Updates on the Management of Severe Traumatic Brain
Injury." Intensive care 33.1 (2009): 16-30.
Initially, performing a correct assessment of the EGCT allows
quickly implementing an appropriate treatment. Additionally,
the proper treatment of severe traumatic brain injury necessarily
requires an adequate understanding of the pathophysiology of
the different types of injuries and to monitor the hemodynamic
parameters on which attention should be focused, above all, on
achieving an adequate cerebral supply of oxygen and avoiding all
those factors that increase intracranial pressure (ICP). For them,
it is that there is no treatment as such described, if not, resort to
surgical processes and carry out a correct management, keeping
rest and medicating sedatives and analgesics of which the most
used are: sedatives such as Midazolam (0.04-0.2 mg / kg / h) or
Propofol (0.8-4 mg / kg / h) and analgesics such as Morphine EV
(0.07-0.5 mg / kg / h) and Fentanyl (0.7-10mcg / kg / h) being the
latter the least used (Table 16).
| Intracranial pressure (ICP) monitoring |
oxygenation monitoring |
of brain metabolism |
| Normal values are considered those that are less than or equal to 15mmHg. Its measurement is performed to diagnose intracranial hypertension and as a therapeutic guide in the treatment of the patient |
Normal oxygen tissue pressure values are between 15-40mmHg. Less than 15mmHg are indicators of tissue hypoxia. |
Various metabolites derived from physiological metabolic processes or as a result of tissue injury such as glucose, lactate, pyruvate, glycerol and glutamate can be quantified. Glucose, lactate and pyruvate are markers of cerebral ischemia. |
| |
Oxygen saturation in the jugular bulb consists of the measurement of blood oxygen saturation obtained through a catheter placed in the jugular bulb. |
|
Table 16. Monitoring to be taken into account in the management of the patient with EGCT
Source: Rada Martín, Sarai. "Nursing care recommendations for patients with severe traumatic brain injury admitted to the ICU-A of the Hospital Complex of Navarra." (2014).
Cerebrovascular disease
Cerebrovascular disease (CVD) or stroke is defined by the World
Health Organization as the rapid development of focal or global
signs of functional compromise at the brain level, with the
presence of symptoms lasting 24 hours or more that can lead
to death. This pathology, represents the third cause of mortality
of the adult population and the first of resulting disability,
for this reason, it constitutes an important health problem
worldwide, in addition, it should be noted that it is currently
considered by many authors as a syndrome that includes a group
of heterogeneous diseases with a common point based on the
alteration in the vasculature of the central nervous system,
which leads to an imbalance between oxygen supply and oxygen
requirements, the immediate consequence of which falls on the
brain tissue, where it causes focal dysfunction. CVD can occur in
two forms: a hemorrhagic form, which represents 15% of cases
and is defined as the rupture of a blood vessel that leads to a
blood accumulation, either within the cerebral parenchyma or
in the subarachnoid space, and the other form is ischemic, which
takes place by the occlusion of an arterial vessel and involves permanent damage by ischemia; but, if the occlusion is transient
and self-resolved, momentary manifestations will occur, which is
called transient ischemic attack, which is defined as that episode
of focal neurological deficit due to cerebral ischemia, of less
than 60 minutes of duration, complete subsequent resolution,
and without changes in neuroimaging, additionally, in general,
ischemic pathology represents 85% of cases. In addition to the
proposed management "IN CRITICAL CONDITION" table 17 shows in summary form the therapeutic scheme that should be
provided to patients with cerebrovascular/ischemic disease and
cerebrovascular/hemorrhagic disease (Table 17).
Stroke |
Hemorrhagic Stroke |
| An intravenous injection of recombinant tissue activator of plasminogen or antiplatelet agents: Aspirin 325 mg daily (if intolerance or history of allergy to aspirin Ticlopidine or Clopidogrel is used,preferentemente éste último) |
Diuretics: 20 percent mannitol (0.5 to 1 g per kilogram of body weight) and follow-up with furosemide at the rate of 20 mg every 6 hours |
| 400 mg every 8 hours |
Nimodipine in constant infusion by central venous catheter (first choice in Subarachnoid Hemorrhage) |
| General supportive measures depending on the patient's requirements (ventilation, blood pressure and cardiovascular status, fluids, control of homeostasis, nutrition, analgesics, etc.) |
General supportive measures depending on the patient's requirements (ventilation, blood pressure and cardiovascular status, fluids, control of homeostasis, nutrition, analgesics, coagulation status, etc.) |
| nursing surveillance of neurological status with special attention to the level of consciousness and progression of motor deficit |
Investigations for diagnosis and location of the damaged cerebral vessel and surgical procedures for possible surgical evacuation or prevention of cerebral hemorrhage in cases that required it |
| complementary tests (electrocardiogram, Doppler echocardiogram, brain mapping electroencephalogram, bilateral carotid Doppler) |
Strict nursing surveillance of neurological status with special attention to the level of consciousness and progression of motor deficit |
| Physiotherapy and Rehabilitation (if stable evolution and non-progression of CVD was started within 72 hours of the onset of symptoms) |
Physiotherapy and Rehabilitation (if stable evolution and non-progression of CVD was started between the third and fifth day of the onset of symptoms) |
Table 17. Management and treatment used in the patient ischemic stroke and haemorrhagic stroke
Source: Turrent, Jose, et al. "Behavior and management of cerebrovascular disease in an intensive care unit." Cuban Journal of Intensive Medicine and Emergencies.
Cardiovascular pathologies in the patient in the
ICU, treatment and proper management
Cardiovascular diseases are those that constitute a group
of entities that involve the heart and blood vessels. When it
affects blood vessels, it can affect organs such as the brain
(cerebrovascular disease described above), lower limbs, kidneys,
and heart. These diseases have been reflecting figures very
similar to those of global epidemics, and have been identified
as the leading cause of disability and millions of early deaths
worldwide; account for 60% of all deaths, of which 80% are
common in low- or middle-income countries. In Colombia,
in 2010 according to data from WHO and PAHO there were
28,996 deaths from chronic no communicable disease (CNCD)
in men between the ages of 30 and 69 years, of which 48%
corresponded to cardiovascular diseases, on the other hand,
in women between 30 and 69 years there were 26,203 deaths
from CNCD, and 37.8% of these correspond to these disorders,
which indicates that diseases associated with alterations at the
cardiac and vascular level are one of the main causes of deaths
nationwide. Among the cardiovascular diseases the ones with
the highest occurrence according to studies are: coronary heart
disease and cerebrovascular disease, however, in view of the fact
that this last pathology has a great impact on the CNS, it was
decided to describe it in the section on neurological pathologies.
Therefore, in this section of cardiovascular pathologies, the 3
most frequent heart diseases in the ICU will be described.
Coronary syndrome: Acute coronary syndrome (ACS) refers to
the abrupt interruption of the arrival of blood to a specific area of
the heart and as a consequence of the obstruction of a coronary
artery by the rupture of an athermanous plaque, for this reason,
many authors mention myocardial infarction when talking
about ACS since, commonly the frequently affected part is the
myocardium. Likewise, as mentioned before, it is part of one of
the sets of diseases of greatest interest in emergencies, both in its
pre-hospital and hospital phases; due to the need for immediate
therapeutic action and the need to make the differential diagnosis
of other processes. For the correct management and treatment
of this, it must be identified whether or not there is an increase
in the ST segment, for this an Electrocardiogram, cardiac markers
(troponins), chest x-ray and a coronary angiography must be
previously performed, in addition to taking into account what is
reflected in the acronym "In Critical Condition".
Currently, management guidelines for acute myocardial infarction
with and without ST elevation report that effective treatment in
the younger population may usually also be recommended in
critically ill elderly patients (Table 18).
Medicament |
Evidence |
| Anticoagulants |
-Fondaparinux is of choice, as it is associated with lower risk of bleeding and lowers mortality in the long term. Not recommended in STEMI taken to primary percutaneous coronary intervention (PCI)
-Enoxaparin: do not use bolus in people over 75 years of age, Use according to glomerular filtration rate. In clinical trials it has been administered at doses of 0.75 mg/kg every 12 hours in people over 75 years of age, instead of 1 mg/kg every 12 hours used in the younger population.
-Unfractionated heparin is the leading medicine in the treatment of patients with advanced chronic kidney disease (GFR< 30 ml/min/1.73 m2)17. Patients over the age of 60 may require lower doses |
Inhibidores G IIb/IIIa
|
• Eptifibatide is the preferred agent for the observed benefit. Reduce infusion doses of eptifibatide and tirofiban according to renal function. Increasing age can increase the risk of bleeding.
• In general, there are no age-related treatment interactions, although greater adverse events occurred in women12. |
| Antagonistas de receptors P2Y12
Fibrinolytic |
• It is suggested to use ticagrelor as the medicine of choice, followed by clopidogrel as the second option. As for this, although the evidence is inconclusive, it is suggested not to administer loading doses in people over 75 years of age because it may increase the risk of major bleeding.
• Prasugrel: the Food and Drug Administration (FDA) issued
Alert message for excess bleeding without benefit clinical. It is not recommended in ≥ 75 years or < 60 kg or patients with a history of stroke or transient cerebral ischemia, except in those at high risk such as diabetics or with previous infarction • They are effective in older patients; in patients ≥ 75 years undergoing this therapy, there is a reduction in relative mortality of 15%1. • As a serious adverse effect, intracranial hemorrhage occurs in 2.9% in > 85 years 1. Tenecteplase was associated with a lower frequency of intracranial hemorrhage than with tissue plasminogen activator, although none showed superiority in cardiac outcomes.
• They should be used, preferably, with anticoagulants such as enoxaparin as it has been shown that in > 75 years the risk of bleeding decreases with a dose of 0.75 mg / kg every 12 hours omitting the loading dose |
Table18. Pharmacological management of ACS
Source: Pemberthy-López C, et al. Treatment of the elderly with acute coronary syndrome. Rev Colomb Cardiol. 2016.
Pulmonary pathologies frequent in the patient in ICU, treatment
and proper management
Any alteration that prevents proper functioning in the lungs is
considered a lung disease. There are mainly three types: Airway
diseases, lung tissue diseases, and lung circulation diseases
(Table 19). Common lung diseases include: asthma, atelectasis,
bronchitis, COPD, lung cancer, pneumonia, pulmonary edema,
and pulmonary embolism (Table 19).
Airway diseases |
Lung tissue diseases |
Diseases of the pulmonary |
| These diseases affect the ducts (airways or airways) that carry oxygen and other gases to and from the lungs. They often constrict or block the airways. These include asthma, chronic obstructive pulmonary disease (COPD), and bronchiectasis. People with respiratory illnesses often say they feel like they're "trying to exhale through a straw." |
They affect the structure of lung tissue. Scarring or inflammation of the tissues that prevents the lungs from expanding completely (restrictive lung disease). This makes it difficult for the lungs to absorb oxygen and expel carbon dioxide. People with this type of lung disorder often say they feel "like they're wearing a jacket or jacket that's too tight." As a result, he couldn't breathe deeply. Pulmonary fibrosis and sarcoidosis are examples of lung tissue diseases. |
They affect the blood vessels in the lungs. They are caused by blood clotting, scarring, or inflammation of these vessels. It affects the ability of the lungs to absorb oxygen and expel carbon dioxide. It can also affect the functioning of the heart. An example of this type of disease is pulmonary hypertension. People with these conditions often find it difficult to breathe during exercise. |
Table 19. Classification of lung diseases
First, acute atelectasis (ALA) is the collapse of the main pulmonary
compartments that presents as a frequent complication of
intubated patients when mechanical ventilation is used in the
intensive care unit (ICU), especially when there are predisposing diseases such as old age and obesity. In addition to excess
bronchial secretion, weakness of the respiratory muscles or
pulmonary edema. Traditionally, treatment of atelectasis in
intensive care patients has focused on aspiration of airway
secretions, supplemented with chest physiotherapy and
bronchoscopy. For ALA, bronchoscopy should be considered,
especially in relation to changes in oxygen in the context of failed
conventional catheter aspiration. The main goal is to reconstruct
the affected lung. There are specific treatments such as
humidification hydration, respiratory physiotherapy techniques
directed by a rehabilitation specialist, breathing with ventilation
with intermittent positive pressure, ventilation with continuous
expiratory positive pressure and positive pressure at the end of expiration and bronchoscopy, previously mentioned. However,
there is a specific treatment directed according to the etiology
(Table 20).
Treatment |
Etiology Of Atelectasias |
| Non-Surgical |
| • Bronchodilators. |
• Asthma, Cystic Fibrosis. |
| • Antibiotics. |
• Bacterial infections (pneumonia, TB, sinusitis, bronchiectasis) |
| • Chemotherapy and radiation therapy. |
• Intrathoracic tumors (lymphoma, osteogenic sarcoma, Wilms tumor) |
| • gamma globulins |
• Hypogammaglobulinemia, |
| |
• Immunodeficiency’s. |
| • Steroids. |
• Inflammatory processes. |
| • Postural treatment and thickening of the diet. |
• Gastro esophageal reflux and aspiration. |
| Surgical |
| • Resection |
• Bronchiectasis, vascular ring, bronchial adenoma and others. |
| • Extraction |
• Foreign body aspiration. |
| • Correction |
• Congenital heart disease, tracheotic fistula. |
| • Dilatation |
• Tracheal stenosis |
| • Gastrostomy |
• Swallowing and esophageal motility disorders with aspiration. |
Table 20. Specific treatment for atelectasis
Severe chronic obstructive pulmonary disease (COPD) is one
of the reasons why large numbers of patients are admitted to
intensive care units. This is a group of lung diseases that make
it difficult to breathe and get worse over time. Normally, the
airways and alveoli are flexible or distended. As for treatment
strategies, for bronchodilators, the authors found that β2-
adrenergic drugs and anticholinergic drugs are equally effective,
because anticholinergic bronchodilators have fewer side effects
and are milder and should be considered as first-line drugs. They also found that inhalation was more effective than injection, and
the benefits of adding a second inhaled bronchodilator were only
noticed after the maximum dose of the first drug was reached.
Overall, a large proportion of COPD exacerbations were attributed
to infection (51% infection, 26% heart failure, 43% pneumonia,
and 24% heart failure in SUPPORT2). Therefore, decompensating
can be seen as antibiotic therapy may be beneficial for the initial
treatment of COPD exacerbations. Another very important
aspect is the recommendation to use non-invasive mechanical
ventilation, since several studies support this strategy. According
to the results of several studies, this mode of ventilation reduces
the need for intubation and mortality in patients with copd
respiratory failure. It is also important to perform laboratory
tests to search for criteria for systemic inflammatory response
syndrome, sepsis or severe sepsis. Some of the drugs indicated
such as corticosteroids could cause metabolic alterations such
as metabolic alkalosis, hyperglycemia. In addition, it is important
to consider leukocytosis as a risk factor for exacerbations. For
specific treatment it is recommended to perform PCR, pharyngeal
swab, Gram, cultures and procalcitonin. Likewise, evaluating the
existence of cardiovascular alterations allows a more specific
treatment.
On the other hand, pneumonia is the second most frequent
infectious complication in hospitals and the first in intensive care
units. Eighty percent of nosocomial pneumonia episodes that
occur in patients with artificial airways are known as ventilatorassociated
pneumonia (NAV). VAP is the most common
cause of death among hospital infections in the ICU, primarily
due to Pseudomonas aeruginosa and methicillin-resistant
Staphylococcus aureus (MRSA). In addition, the number of days
on mechanical ventilation and the average stay in ICU and hospital
increased. Although classically the four disease pathways for
developing VAP (aspirations local secretions of the oropharynx
contiguous, bloody and through vessels or ducts) have been
distinguished, aspiration of secretions from the oropharynx is
the predominant and almost the only route. The management
involves 2 simultaneous treatments. On the one hand the
supportive treatment and on the other, the antibiotic treatment.
The purpose of mechanical ventilation is to find the best possible
oxygen for the tissue while reducing secondary damage. To do this, it is important to remember that the best oxygen fraction
(FiO2) is the lowest FiO2, as high concentrations of oxygen can
be toxic. In fact, in patients with lung infections, only 50% of FiO2
can be toxic, although studies that clearly identify the threshold
of FiO2 that can be considered toxic to humans are lacking. The
use of positive expiratory pressure (PEP) improves oxygenation,
but requires a balance between oxygenation, pulmonary over
distension, and patient needs. With antibiotic therapy, it is very
important not to delay effective treatment, as inadequate initial
empirical treatment is associated with increased mortality
(Table 21).
| Microorganisms |
Therapy |
| Central microorganisms |
Aminoglycosides (Gentamicin, tobramycin, amikacin) or quinolones (Ciprofloxacin, Levofloxacin) |
| P. aeruginosa |
Beta-lactams anti pseudomonas: ceftazidime, cefepine, piperacillin, ticarcillin, mezlocillin. |
| Acinetobacter sp. |
Beta-lactam inhibitors of beta-lactamases: ticarcillin, clavulanate, piperacillin-tazobactam. |
| |
Aztreonam (efficacy limited to gram-negative bacilli with or without Vancomycin/teicoplanin. |
Consider Staphylococcus aureus methicillin resistant
High rate of polymicrobial infections |
|
Table 21. Terraria con antibiotics para pneumonia associate al ventilator
Finally, we consider Covid 19 among the most frequent diseases in
ICU patients, where all countries have created their own treatment
and action protocols against this disease. The replication cycle of
the SARS-COV-2 virus provides a potential target for developing
effective treatments for the disease. It is a single-stranded RNA
virus whose cycle begins with the binding of the viral structural
mutant protein (S) to the angiotensin-converting enzyme 2 (ACE2)
receptor, followed by the passage of serine protease 2 (TMPRSS2)
through the host membrane. Cells facilitate cellular entry after
binding to receptors through intracellular mechanisms. Studies
have shown that the ACE2 receptor can be inhibited with the use
of chloroquine/hydroxychloroquine because it interferes with its
terminal glycosylation and therefore the drug can act at various
stages of the SARS-COV-2 virus replication period. Likewise,
other drugs have been used according to the replication cycle as
shown in Table 22 (Table 22).
envelope membrane fusion inhibitor |
Umifenovir (also known as Arbidol) is a promising antiviral agent with a potent mechanism of action during most phases of the viral replication cycle of various viruses. First study showing efficacy against SARS-CoV-2 with a clear benefit for the patient. |
| TMPRSS2 inhibitors |
Kamostat and Nafamostat (Mesylate) are protease inhibitors. They inhibit trypsin (Ki = 1 nM) and several inflammatory proteases, including plasmin, kallikrein, and thrombin. Camostat inhibits the binding of severe acute respiratory syndrome coronavirus (SARS-CoV) and SARS-CoV-2 surface glycoproteins in vesicular stomatitis virus (VSV) into vero cells, Calu-3 cells, and primary pulmonary epithelial cells in the form of pseudo granules. To date, there have been no clinical trials demonstrating its efficacy against COVID-19, but based on the mechanism of action described above and experience with SARS-COV, it may have broad potential.. |
| Entry inhibitors and endocytosis |
Chloroquine and its derivative, hydroxychloroquine, have traditionally been used in the treatment of malaria and some autoimmune diseases, however, these drugs may be active against SARS-CoV 1 and SARS-CoV 2 similarly in vitro and in clinical practice. A 2005 study showed that chloroquine's ability to raise intraatomic pH, thereby inhibiting the pH-dependent viral replication phase, was effective in limiting the spread of infection to other host cells |
| 3-chymotrypsin inhibitors such as protease |
At this stage, antiviral drugs that inhibit this enzyme act, such as lopinavir/ritonavir and darunavir. The justification for use is based on in vitro studies in animal models showing potential activity for SARS-CoV and MERS-CoV; because lopinavir and ritonavir can bind to M pro, a key enzyme for coronavirus replication, suggesting that it may suppress coronavirus activity. |
| Viral RNA-dependent RNA polymerase inhibitors. |
The antiviral drugs that inhibit this enzyme, currently under study in their effectiveness against COVID-19, are Ribavirin, Favipiravir and Redemsevir. |
| Interferon’s |
Interferon means that it interferes with viral multiplication. It is a natural compound whose function is aimed at creating an inhibition mechanism at the first level of response of the organism; it is divided into three types: beta, alpha (which groups a large number of these) and gamma. In ICU (3 million units, intramuscularly, on alternate days, for one month) |
Table 22. Drugs for the management of covid 19
In the exacerbation stages, aerosols or micro droplets are
avoided through the use of low-risk procedures such as; the
placement of the Guide tube and oxygenation facial mask with
expiratory filter, chest compression, defibrillation, cardio version,
and transcutaneous pacemaker placement, insertion of venous
or arterial route, administration of drugs or intravenous fluids.
In addition, according to the Association of Respiratory Care
Physiotherapists in the UK, the need to apply bronchial drainage
techniques in SARS-COV2 infected patients can be decided if the
following criteria are met:
- Evidence of retention of secretions with difficulty expectorating
- Ineffectiveness of cough or drainage capacity
Another important aspect is the prone position of the patient, as
it improves oxygenation and increases survival in patients with
a clinical picture similar to ARDS. Recommendations are made
when PaO2/FiO2 <150 even with protective ventilation (tidal
volume <6 ml/kg ideal body weight and high PEEP). Exercises
should be performed by a well-coordinated group with as few
people as possible, and an experienced physical therapist may
participate. It is important to prevent and maintain complications
of treatment (extubation), accidents, onset of medium and/or
peripheral intubation, shoulder dislocation, pressure ulcers and
hemodynamic changes in the most sensitive areas).
Risk and prognostic factors in COVID-19 patients requiring
mechanical ventilation with or without ARDS are not fully
understood, and more clinical research is needed in this area
to improve outcomes. Nor have the data analyzed by artificial
intelligence been published in the group of patients in intensive
care. On the contrary, the respiratory, cardiovascular and longterm
quality of life consequences of admission to the ICU are
unknown, so CIBERESUCICOVID aims to identify the risk and
prognostic factors of COVID-19 patients admitted to Spanish ICUs
since the beginning of the Spanish pandemic in October 2020
using artificial intelligence analysis. Patients discharged were followed up and one year after discharge, mortality at 6 months
and one year, effects on respiratory and cardiovascular function,
and effects on quality of life were determined. The accelerated
discovery of this new infection has allowed studies to highlight
that in patients admitted to the ICU, high-flow nasal cannulas,
invasive mechanical ventilation (IMV), the use of prone position
and corticosteroids have been used more frequently, reducing
the number of patients in VMI and the time spent in ICU and
hospital stay.
Frequent gastrointestinal pathologies in the patient in the ICU,
treatment and proper management
The most frequent pathologies that enter the ICU are digestive
problems, compartmental abdominal syndrome, intestinal
ischemia, and digestive hemorrhage, postoperative complications
of digestive surgery, peritonitis and acute pancreatitis. First,
gastrointestinal problems in the ICU can be classified into nonsurgical
and surgical, which include problems in intestinal motility
to ischemia and inflammation as presented in (Table 23).
| Non-Surgical |
Surgical |
| Motility problems |
Intestinal obstruction |
| Diarrhea |
Ischemia |
| • Infectious |
Perforation |
| • No- Infectious |
Stress-related bleeding or mucosa |
| constipation |
Haemorrhage |
| Malabsorption |
Intra-abdominal compartment syndrome |
| Hepatitis |
Pancreatitis |
| Hepatic impairment |
Cholecystitis (calculus and calculus |
Table 23. Classification of gastrointestinal problems in ICU
Diarrhea is a cause of hydroelectrolytic imbalances, interruption
of enteral nutrition schemes, malnutrition, aggravation of the
morbid picture, prolongation of hospital stay, and even death.
The occurrence of diarrhea is multifactorial (related to enteral
nutrition, medications, altered gastrointestinal motility, or
secondary to antibiotics and/or the disease itself) and can have
serious and important consequences for the patient. In its most
common form, diarrhea is any change in bowel habits that a
patient identifies as their own. Therefore, any definition of
diarrhea should include an increase in stool volume, a change in
appearance, and an increase in frequency. Diarrhea, as defined
by the World Health Organization, is the evacuation of three
(or more) bowel movements in 24 hours in a container, or even
liquid; it may be accompanied by blood. Severe diarrhea responds
to different pathophysiological mechanisms. Some of the most
frequent would be as follows: osmotic diarrhea, secretory
diarrhea and exudative diarrhea. Physical examination should
indicate the determination of abdominal pain and pain, fever and
anemia are a sign of diarrhea. The impact of diarrhea on patients'
hydro electrolytic status should also be evaluated, looking for
internal mass spasms, hypertension, and arterial hypotension,
among others. Additional tests include: 1) Number of white blood
cells, 2) copolytics to determine microorganisms, 3) determine
the A and B variety of toxins calculated by translation of exempt
enzyme analysis (ELISA). 4) other laboratory methods may be
necessary to assess the level of hydro electrolytic involvement
and modification and modify the plasma ion concentration as well
as the acid balance. 4) The calculation of the remaining osmosis
of the fertilizer material is an important step before starting any
specific treatment and can be made of the concentrations of NA
and KIS in the fecal matter (Equation 1).
Equation 1.
Osmolar Remaining Anion = 290 mOsm – (Na+ + K+) * 2
It is important to consider that the only cause of DANE that can
be controlled with specific treatment is cl infection. Difficile, in
persistent cases antibiotic therapy (metronidazole, vancomycin
or teicoplanin) and endoscopy are necessary. The use of
antidiarrheal medication should be reserved for cases of DANE
that are not controlled despite other measures.
In another order of ideas, the European Society of Clinical
Nutrition and Metabolism (ESPEN) published in 2015 the
recommendations on "Definition and classification of intestinal
insufficiency in adults". Intestinal insufficiency is defined as
intestinal activity that falls below the minimum required to
absorb such macronutrients and/or water and electrolytes,
intravenous (IV) supplementation to maintain health and/or
growth. Reduced intestinal absorption function that does not require IV supplementation can be considered as intestinal
insufficiency or dysfunction. Expert group to classify intestinal
insufficiency into three categories, by presentation and duration
and intensity.
Type I: It is deep, usually lasts a short time and is self-limiting.
It usually occurs after abdominal surgery, but can also occur in
critically ill patients (pneumonia, traumatic brain injury, acute
pancreatitis).
Type II: Long-term, often in metabolically unstable patients,
requires multimodal care and intravenous supplementation (i.e.)
for weeks or months.
Type III: Chronic disease in metabolically stable patients,
requiring months or even years of treatment. It can be reversible
or irreversible.
Resuscitation to ensure an abdominal perfusion pressure greater
than 50 mmHg and hydro mineral and acid-base balance are
recognized as actions for treatment. Also the strict glycemic
control, since these conditions a better metabolic control, but
also improves intestinal motility. In addition, a treatment that
includes intestinal dysmotility to minimize the use of medications
that produces it (alpha-agonists, proton pump inhibitors, calcium
channel blockers, sedatives, muscle relaxants, analgesics and
vasoactive drugs). The efficacy of metoclopramide has been
shown. Another important point is the control of sepsis, if surgical
treatment is necessary; and indicates antibiotics, especially
according to the result of the crops. Finally, nutritional support is
recommended to start in the first 24-48 hours, once the patient
is hemodynamic ally stable, to reduce the effects of increased
catabolism and avoid malnutrition. Early EN is suggested (48-72
hours), although it is difficult to initiate it because the patient
does not tolerate it initially. The severe patient with IF usually
presents with high-expenditure fistula or enterostomy, sepsis
and problems associated with SIC (dehydration, malnutrition,
and hydro electrolytic alterations) in the context of FIA type II, so Figure 5 shows some of the commonly used solutions and their
composition in relation to plasma (Figure 5).
Figure 5: IF Management.
From:Agüero, Aldo, and Kenia Infante. "Intestinal failure in the critical patient."
Revista Medical del Uruguay 37.2 (2021): e37209-e37209.
Another point is Abdominal Compartment Syndrome, which is the
end result of a continuum that begins with a persistent increase
in intra-abdominal pressure (IAP) that can alter blood flow to the
region and potentially lead to multi-organ failure. (FOM). Due
to abdominal trauma, acute pancreatitis, hypovolemic shock
and secondary peritonitis. Values below 10 mmHg are generally
considered normal. The increase in IAP in critical patients is
usually multifactorial, reaching 15 mmHg in the presence of
visceral edema and pain after surgery and 20-50 mmHg after
intensive resuscitation (shock), severely affecting other systems.
Measurement of IAP in clinical situations indirectly confirmed
by nasogastric tube, bladder catheter, gastrostomy or vascular
probe placed in the inferior vena cava, all well correlated with
direct measurements. The treatment of choice is decompression.
Therefore, decompressive medical measures such as nasogastric
and rectal catheter, nasogastric and colonic catheterization,
rectal enema, aspiration, 20% human albumin combined
with furosemide, positive continuous venous hemodialysis,
ultrafiltration, continuous negative extra peritoneal dialysis
should be considered. Pressure, increased sedatives and eventual neuromuscular blockade before attempting surgical
decompression. Improvement is sometimes seen with
percutaneous drainage of peritoneal fluid before attempting to
decompress the abdomen using laparotomy. In addition, there
is the option of surgical treatment with the following indications:
1. Decompression with PIA values ³ 20 mmHg is recommended.
2. The concept of damage-controlled laparotomy has gained
wide acceptance among trauma surgeons.
3. The abdomen cannot be closed due to the high risk of severe
HIA, and when a second examination is planned immediately,
the patient should be transferred to the intensive care unit
for overheating to correct the entanglement. Coagulation
disorders, optimizing hemodynamics and oxygen transport.
4. If during the operation there is still clear evidence of HIA,
some temporary abdominal closure technique is preferred
to prevent the development of an ACS.
Intra-abdominal infections (IAI) are common surgical emergencies
and, despite advances in surgical techniques, antibiotic therapy
and resuscitation, are characterized by morbidity, mortality
and complications impose high costs on health systems. Acute
peritonitis (AP) includes any acute inflammatory process of
the peritoneal serous, regardless of its etiology. It should be
noted that, if not treated properly, these patients can quickly
develop sepsis, and the involvement of organs and systems will
vary depending on the different factors we will analyze. The
surgical management of intra-abdominal infections is based on:
the elimination of the source of contamination, reduction of
contamination of the peritoneal cavity and treatment of residual
infection. Fluid and electrolyte replacement is a priority, and saline
infusion is started immediately. Vasopressors (norepinephrine,
dopamine, and epinephrine) are necessary in patients with
inadequately compensated hemodynamic ally compensated
volumes (septic shock). Pathogens associated with secondary
BP are often derived from the patient's own flora and typically
include enter bacteria (mainly Escherichia coli and Klebsiella), Streptococcus viridans, and anaerobes (especially Bactericides
fragile), enterococci, and gram-positive bacteria. Established.
Therefore, amino penicillin in combination with a beta-lactamase
inhibitor is usually included in the management plan.
Renal pathologies and frequent in the patient in ICU, treatment
and proper management
Acute renal failure (AKI) is defined as a sudden drop in the
glomerular filtration rate, resulting in the accumulation of urea,
creatinine, and other toxic waste products and changes in water
and electrolyte balance. There are different definitions and
stages of severity of AKI, and the most commonly used measures
in clinical practice are the KDIGO, RIFLE and AKIN criteria. There
are three types of renal failure as shown in (Table 24).
Pre-renal Renal Insufficiency |
| There is a decrease in renal perfusion, which will be compensated by hormonal mechanisms and nerve stimuli that condition the elimination of electrolytes and therefore also the decrease in urine flow. This urine is concentrated in urea, cretonne, phosphates, ammonium. All this is if the urine volume of 500 ml / day is low, although the kidney works properly and focuses on maximum capacity, it is not possible to eliminate all waste and part of the maintenance of nitrogen products producing azotemia. |
| Intrinsic Renal Insufficiency |
| It may be affected by other causes not directly attributable to renal hypo perfusion, such as: systemic or local immune causes, such as Vasculitis or acute interstitial nephritis due to drug-induced immune hypersensitivity; vascular problems, such as atherosclerotic disease, renal artery or thrombosis, or venous thrombosis. |
| Post-renal Or Obstructive Renal Failure |
| The kidneys adequately fulfill their missions of filtering, absorbing and secreting, an obstruction to the urinary flow ends up affecting these functions and can cause anuria. In this case, we speak of acute obstructive or pre-renal renal failure. The degree of reversibility is high and renal function quickly returns to its initial values when the cause is corrected or simply facilitates the exit of urine (by probing, catheterization or nephrostomy). |
Table 24. Classification of renal failure and its pathophysiology
Several studies suggest that early hemodialysis may improve
mortality outcomes. As with any other treatment in the ICU, the
dose of Renal Replacement Therapy should be determined in an
attempt to optimize solute clearance and fluid and electrolyte
balance. There is considerable heterogeneity between variables,
such as inclusion criteria or start time, such as the use of time
criteria (6, 8 or 12 hours) in some studies, or analytical criteria
(serum urea or creatinine) in others). The time periods used are
also significant, with some settings starting in the first 6 hours
and some in the first 12 hours. Clearly, there are large temporal
differences in the severity of rapidly progressing patients, and
temporal factors can be decisive for the prognosis of the disease.
Technically, we emphasize that ultrasound should be the method
used for central or arterial venous catheterization because
it reduces the risk of complications. We believe that in critical
patients with AKI, the dilemma of continuous or intermittent HRT
modalities should not be considered, but a dynamic approach to
adapt the technique to the clinical and hemodynamic status of the
patient over time. In this context, techniques such as intermittent
hemodialysis should be an additional RRT to ICU patients, as
there were no differences in mortality or renal recovery. Because
it can be beneficial for some patients who may benefit compared
to treatment. Mobility and recovery after cessation of TRS.
Frequent metabolic pathologies in the patient in the ICU,
treatment and proper management.
Some authors argue that the caloric needs in critical condition
are very high, assuming that they are accompanied by a
substantial increase in basal metabolic expenditure, that is, in
critical patients, it is important to strongly increase metabolism.
However, some authors have indicated that the degree of hyper
metabolism is actually mild. The early stages of stress, usually no
more than 10% higher than resting metabolic rate, as opposed
to being highly catabolic, this is represented by increased
excretion of nitrogen and urea. Usually, severely ill patients
develop hyperglycemia and, in some cases, hyperinsulinemia.
Once a patient has hyperglycemia of unknown cause, glucose
distribution appears to be a physiological paradox and insulin
resistance is thought to be one of the causes. Evidence that
hyperglycemia in acute medical or surgical diseases increases
morbidity and mortality in the ICU, and increases length of
hospital stay and days on mechanical ventilation. Intravenous
insulin therapy is suggested, the advantages of using an
algorithm or protocol include greater glucose control, less error
in treatment, so it provides guidance on how to achieve specific
blood glucose levels, adjust insulin doses, and stop or slow the
rate of infusion based on the individual patient's blood glucose
level and dietary pattern and avoid hypoglycemia [101]. During
trauma and stress, two major changes have been observed in
relation to insulin, a hormone that also plays an important role
in amino acid and protein homeostasis. These changes include inhibition of catecholamine-mediated secretion and insulin
resistance, followed by the release of amino acids from skeletal
muscle for gluconeogenesis and decreased glucose utilization by
insulin-dependent tissues. To determine and determine protein
requirements, it is necessary to understand protein metabolism
and quantify daily protein turnover by determining the turnover
of various measurable proteins, such as plasma, muscle and
urinary protein excretion. Under normal circumstances, lipid
homeostasis depends on a balance between anabolic (insulin)
and catabolic (catecholamines and glucagon) stimuli. During
sepsis, the predominance of catabolism occurs transiently, which
involves the breakdown of lipids into free fatty acids, which are
therefore precursors of hepatic ketone bodies and primary fuel
for cells to consume glycogen. As sepsis progresses and leads to a
lack of nutrients, glucose and amino acid consumption is reduced,
making lipids the main source of energy. Glucose oxidation can
also be inhibited by altering lipid metabolism.
Conclusion
In conclusion, having knowledge of the steps, management
and approach of the behaviors that health personnel must
have in the intensive care unit, are essential to reduce the
morbidity and mortality of patients, therefore, the acronym "IN
CRITICAL CONDITION" and the recognition of the most frequent
pathologies found in the ICU, are a very useful proposal for the
fulfillment of a comprehensive care of the critical patient with a
previous and adequate precision Diagnostic.
REFERENCES
- Garcia landa, paolo cesar (2018) The effectiveness of the family participation program in the basic care of the patient in the ICU.
Google Scholar
- Stayt lc (2009) Death empathy and self preservation: the emotional labour of caring for families of the critically ill in adult intensive care. j clin nurs 18:1267-1275.
Google Scholar, Crossref
- Ayllon N, Alvarez M, Gonzalez m (2007) Stressful environmental factor perceived by patient in an intensive care unit. intensive care 18:159-167.
Google Scholar
- Reinoso, lissette alejandra aviles, claudia soto nunez (2014) Nursing models in critical patient units: a step towards advanced care. Global Nur 13:323-329.
Indexed at, Google Scholar
- Brasil (2010) programa nacional de humanização da assistência hospitalar [internet]. acesso em 08 set disponível em.
Indexed at
- Marosti ca, dantas ras (2006) patient assessment of stressors in a coronary care unit. minutes paul nursing 19:190-195.
Google Scholar
- Lescaille Taquechel, Marlina (2006) Relationship of the ethics of caring and nursing models with the person and their dignity. Cuban J Nur 22.
Google Scholar
- Haddad MCL, alcantara C, praes CS (2005) feelings and perceptions of the patient in the postoperative period of cardiac surgery, experienced in an intensive care unit. science care and health 4:65-73.
Indexed at, Google Scholar
- Flanders SA, Harrington L, Fowler RJ (2009) Falls an Patient Mobility in Critical Care: keeping patients and staff safe. AACN 20:267-276
Indexed at, Google Scholar, Crossref
- KOCHANEK K D (2017) National Vital Statistics Reports,Deaths: Final Data for 68:9.
Indexed at
- Oliver, David, Frances Healey, Terry P. Haines (2010) "Preventing falls and fall-related injuries in hospitals." Clin geria med 26:645-692.
Indexed at, Google Scholar, Crossref
- Spaniolas, Konstantinos (2010) Ground level falls are associated with significant mortality in elderly patients. J Trauma Acute Care Surg 69:821-825.
Indexed at, Google Scholar, Crossref
- Bueno-García, Maria Jesus ((2017) Characteristics of the Downton fall risk assessment scale in hospitalised patients. Enfermeria Clinica 27: 227-234.
Indexed at, Google Scholar, Crossref
- Rimland, Joseph M (2016)"Effectiveness of non-pharmacological interventions to prevent falls in older people: a systematic overview. The SENATOR Project ONTOP Series." PloS one 11:e0161579.
Indexed at, Google Scholar, Crossref
- Cameron, Ian D (2018) "Interventions for preventing falls in older people in care facilities and hospitals." Cochrane database of systematic reviews 9
Indexed at, Google Scholar, Crossref
- Heyland DK, Dhaliwal R, Day A, Jain M, Drover J (2004) Validation of the Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients: results of a prospective observational study. Crit Care Med 32: 2260-2266.
Indexed at, Google Scholar, Crossref
- Mc ClaveSA, TaylorBE, WarrenMM MartindaleRG, Braunschweig C and JohnsonDR (2016) "Guidelines for the provision and assessment of nutrition support therapy in the adult critically Ill patient: Society of critical care medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN)." JPEN J Parenter Enteral Nutr 40:159-211.
Google Scholar
- Codner PA (2012) enteral nutrition in the critically ill patient. Surg Clin North Am 92:1485-1501.
Indexed at, Crossref
- Gonzalez, Juan Carlos Montejo, Mercedes Catalan Gonzalez (2013) New systems for implementing nutritional support in ICU patien. Nutricion Hospitalaria 6:60-67.
Google Scholar
- Muguercia, Hilev Larrondo (2003) enteral nutrition vs. parenteral nutrition in the critical patient. Acta medica 11:26-37.
Indexed at, Google Scholar, Crossref
- Munoz, Pilar Gomis, MA Valero Zanuy (2010) parenteral nutrition. Ángel Gil Hernández. Nutrition Treaty. Ed. Médica Panamericana. Madrid 143-169.
- Ehikhametalor K (2019) "Guidelines for Intensive Care Unit Admission, Discharge and Triage." West Indian Medl J 68.
Indexed at, Google Scholar
- American College of Critical Care Medicine of the Society of Critical Care Medicine (1998) Guidelines on admission and discharge for adult intermediate care units. Crit Care Med 26:607-610.
Indexed at, Google Scholar, Crossref
- Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med 27:633-638.
Indexed at, Google Scholar
- De Salud, Institutions Prestadoras de Servicios, and Expertos Clinics Participantes en el Consenso. Grupo Desarrollador.
Indexed at
- Vicente, Jose Fidencio Mata (2012) Tercer lugar Premio «Dr. Mario Shapiro Escalas pronósticas en la Unidad de Terapia Intensiva. Medicina Critica 26:234-241.
Indexed at, Google Scholar
- Granados, Aldemar Yanett (2009) “Severity scales in ICU care. Duazary 6:71-75.
Google Scholar
- Rodriguez, Lissette Liliana Muñoz (2019) SCORE predictive use, prognosis of mortality in patients in intensive care. RECIMUNDO: Sci J Res and Know 3:1164-1179.
Indexed at, Google Scholar, Crossref
- Aguilera, Julio Cesar Gonzalez, Luis Antonio Algas Hechavarria (2016) General prognostic indices for the assessment of critically ill patients in intensive care units. Multi med 20:665-680.
Google Scholar
- Jiang H, Yao Z, Guo G, Wang Y, Li F (2019) APACHE IV Score is Useful For Assessment and Stratification of Elderly Patients Over 65 Years With Acute Cholecystitis. Surg Laparosc Endosc Percutan Tech 29:524-528.
Indexed at, Google Scholar, Crossref
- Sadaka, Farid (2017) Predicting mortality of patients with sepsis: A comparison of APACHE II and APACHE III scoring systems. J Clin med res 9:907.
Indexed at, Google Scholar, Crossref
- Alvarez-Avello J M (2021) "Usefulness of severity scales in predicting in-hospital mortality in cardiogenic shock. Proposal for a new prognostic model." Spanish J Anesthe Resuscita.
Indexed at, Google Scholar, Crossref
- Sanchez-Casado M (2016) Prognostic scales in multi-organ dysfunction: cohort study. Medicina Intensiva 40:145-153.
Google Scholar
- Moreno, Rui P (2005) “SAPS 3--From evaluation of the patient to evaluation of the intensive care unit. Part 2: Development of a prognostic model for hospital mortality at ICU admission.” Intensive care medicine vol. 31:1345-55. doi:10.1007/s00134-005-2763-5
Indexed at, Google Scholar, Crossref
- Alvear-Vega Sandra, Canteros-Gatica Jorge (2018) Evaluation of the performance of APACHE II and SAPS III, in an intensive care unit. Rev Public health 20:373-377.
Indexed at, Google Scholar, Crossref
- Rodrigo, Maria E (2014) "Performance of the Mortality Probability Model (MPM0) in a Contemporary Cardiac Intensive Care Unit." Circulation 130.suppl_ 2: A17002-A17002.
Google Scholar
- Lemeshow S, Teres D, Klar J (1993) Mortality Probability Models (MPM-II) based on an International cohort of intensive care patients. JAMA 20: 2478-86
Indexed at, Google Scholar
- Higgins, Thomas Teres, Daniel Copes, Wayne Nathanson, Brian Stark et al. (2005) Updated Mortality Probability Model (MPM -III). CHEST Journal. 128.
Indexed at
- Donati, Pablo (2017) Adaptation of the Surviving Sepsis campaign.
Indexed at, Google Scholar
- De Mendonça, Arnaldo (2000) Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score." Intensive care medicine 26: 915-921
Indexed at, Google Scholar, Crossref
- Arroliga A, Frutos-Vivar F, Hall J, Esteban A, Apezteguía C et al. (2005) International Mechanical Ventilation Study Group. Use of sedatives and neuromuscular blockers in a cohort of patients receiving mechanical ventilation. Chest 128:496---506.
Indexed at, Google Scholar, Crossref
- Devlin JW, Mallow-Corbett S, Riker RR (2010) Adverse drug events associated with the use of analgesics, sedatives, and antipsychotics in the intensive care unit. Crit Care Med;38 Suppl 6:S231---43
Indexed at, Google Scholar, Crossref
- (Celis Rodríguez E, Pardo Oviedo JM, De la Cal MA, Arellano GC, Hernandez A et al. (2013) Evidence-based clinical practice guideline for the management of sedation and analgesia in critically ill adult patients. Intensive medicine.37:519 - 574.
Indexed at, Google Scholar, Crossref
- Mera, MJ Frade (2009) Analysis of 4 assessment scales of sedation in critically ill patients. Intensive Nursing 20:88-94.
Indexed at, Google Scholar, Crossref
- Carrillo-Esper, Raúl (2011) Clinical practice guideline for thromboprophylaxis in the Intensive Care Unit." Medicina Crítica 25: 227-254.
Google Scholar
- Luque Fernández, Daniel (2019) " Clinical practice guideline for thromboprophylaxis in the intensive care unit.".
Google Scholar
- Javier Vázquez, F E R N A N D O (2013) “Guideline Of Recommendations For The Prophylaxis Of Venous Thromboembolic Disease In Adults In Argentina." Medicina (Buenos Aires) 73.
Indexed at, Google Scholar
- Hermosilla J, M Aguayo, L Aguayo (2017) Pharmacological thromboprophylaxis in critically ill patients and the accumulation of low molecular weight heparins. Medicina Intensiva 41:130-130.
Indexed at, Google Scholar
- Brenner P, Nercelles P, Pohlenz M (2003) Cost of nosocomial infections in Chilean hospitals of high and medium complexity. Rev Chilena Infectol 20:285-90.
Google Scholar
- Leone M, Bourgoin A, Cambon S (2003) Empirical antimicrobial therapy of septic shock patients: adequacy and impact on the outcome. Crit Care Med 31:648-50
Indexed at, Google Scholar, Crossref
- Alvarez-Lerma F, Olaechea P, Grau S, Marin M, DomInguez A et al. (2008) Group de Estudio de Infeccion en el paciente crItico (GEIPC-SEIMC). Recomendaciones para la monitorización de antibiotics en pacientes de la UCI. Enferm Infec Microbiol Clin 26:230-239.
Indexed at, Google Scholar, Crossref
- Lerma F, Alvarez (2010) Political de antibiotics en pacientes critics." Medicina intensive 34:600-608.
Google Scholar
- Cordova Tacza, Isabel Rosario, Maria Orejon Cuadros (2020) Incidencia de antimicrobianos de reserva usados en pacientes con Resistencia Bacteriana Hospitalizados en UCI del Hospital Nacional Ramiro Priale Priale Essalud Huancayo-2019.
Google Scholar
- Klein, Sebastian J (2018) Oliguria in critically ill patients narratives review. J nephron 31:855-862.
Indexed at, Google Scholar, Crossref
- Berman (2008) Audrey Fundamentos de enfermeria conceptos, proceso y práctica. Madrid: Pearson Educación.
Google Scholar
- Macedo, Etienne (2011) Oliguria is an early predictor of higher mortality in critically ill patients." Kidney international 80:760-767.
Indexed at, Google Scholar, Crossref
- Btaiche IF, Chan LN, Pleva M, Kraft MD (2010) Critical illness, gastrointestinal complications, and medication therapy during enteral feeding in critically ill adult patients. Nutr Clin Pract 25:32-49.
Indexed at, Google Scholar, Crossref
- Martinuzzi, Andres Luciano (2012) Nicolas Diarrhea en el paciente critic. Su actual dad. Revista Cubana de Alimentación y Nutrición 22:120-134.
Google Scholar
- Azevedo RP, Freitas FGR, Ferreira EM, Machado FR (2009) Intestinal constipation in intensive care units. Rev Bras Ter Intensive 21:324-331.
Indexed at, Google Scholar, Crossref
- Perez-Sanchez J (2017) Evaluation y Abordaje del estrenimiento en el paciente critic. Enfermería intensive 28:4.
Indexed at, Google Scholar, Crossref
- Fernandez Gamboa, Gerardo (2021) Manejo del balance hídrico por el profesional de enfermería en los servicios de la unidad de cuidados intensives del Hospital Apoyo Puquio.
Indexed at, Google Scholar
- Upadya, Anupama (2005) Fluid balance and weaning outcomes. Inten care med 31.12.
Indexed at, Google Scholar, Crossref
- Boyd, John H (2011) Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Critic care med 39:259-265.
Indexed at, Google Scholar, Crossref
- Claure-Del Granado, Rolando, Ravindra L, Mehta (2016) Fluid overload in the ICU: evaluation and management. BMC nephrology 17:1-9.
Indexed at, Google Scholar, Crossref
- Asencio (2010) Factores que influyen en las enfermeras para la realización del balance hídrico en los pacientes criticos en el servicio de emergences del INEN, Universidad Nacional Mayor de San Marcos.
Indexed at, Google Scholar
- Herraaiz y (2017) Manual de enfermeria tecnicas y procedimientos, ediciones Barcel Baires.
Google Scholar
- Fernandez Elena (2005) Montial Nuria Ruiz de Escudero García, and Elena Prieto Arriba. Intuition o exactitud? Posicionamiento intuitivo de la cabecera de la cama en pacientes críticos. Necesitamos medirlo Enfermeria intensive 16:54-61.
Indexed at, Google Scholar, Crossref
- Del Cotillo Fuente, Mercedes, Valls Matarin J (2014) Analysis del compliment de 2 medidas para prevenir la pneumonia associate a la ventilación mecánica. Enfermeria intensiva 25:125-130.
Indexed at, Google Scholar, Crossref
- Wang L (2016) Elevation de la cabecera de la cama versus la cama plana para la prevencion de la pneumonia asociada al respirator (nar) en adultos bajo asistencia respiratoria mecánica.
Google Scholar
- Estrada-Orozco, Kelly Insertion y (2020) mantenimiento del catheter venoso central Recomendaciones clínicas basadas en la evidence. Revista Columbiana de Obstetrician y Ginecología 71:115-162.
Google Scholar, Crossref
- Soria-Carrion, Gema-Maria (2014) Cuidados de enfermería para la insertion y mantenimiento Del catéter venoso central.
Google Scholar
- Lazaro, Maria Josefa (2021) Ponce Bacteriemia Zero en el paciente con cateter venoso central en la UCI. Revista Sanitaria de Investigation 2:36.
Indexed at, Google Scholar
- Delgado Bohorquez, Laddy X, Jessica D, Monsalve Lago, Dearly M etal. (2018) Estrategias effectives’ en la prevención de las bacteremias asociadas al cateter venoso central en las unidades de cuidado intensivo: Una revisión sistemática de literature.
Indexed at, Google Scholar
- Badia, Irene Fernandez Prevencion de la bacteremia relacionadas con catéter intravascular en el hospital: programa de formacion para estudiantes de enfermeria.
Google Scholar
- Russell, James A (2014) Is there a good MAP for septic shock. N Engl J Med 370:1649-1651.
Indexed at, Google Scholar, Crossref
- Grand, Johannes (2018) Validation and clinical evaluation of a method for double-blinded blood pressure target investigation in intensive care medicine. Critic care med 46:1626-1633.
Indexed at, Google Scholar, Crossref
- ASFAR (2014) Pierre High versus low blood-pressure target in patients with septic shock. N Engl J Med 370:1583-1593.
Indexed at, Google Scholar, Crossref
- Carrillo-Esper, Raul, Jesus Fidel Rocha-Machado (2005) Reanimacion dirigida por metas. Revista Mexicana de Anestesiologia 28:164-168.
Google Scholar
- Aggarwal, Neil R (2018) Oxygen exposure resulting in arterial oxygen tensions above the protocol goal was associated with worse clinical outcomes in acute respiratory distress syndrome." Critica care med 46:517.
Indexed at, Google Scholar, Crossref
- Villamea, Silvia Martínez, Beatriz Brana (2021) Marcos Prevención de ulcers por presion en el cuidados de pacientes colocados en decúbito prono. Lecciones derivadas de la crisis covid-19." Revista Ene de Enfermería 15.1
Indexed at, Google Scholar
- Ourcilleon A, Astrid (2004) Ulceras por presion en pacientes de Unidades de Cuidados Intensivo Como medir su riesgo?. Rev chil med intensiv 91-98.
Indexed at, Google Scholar
- Bravo (2021) Carlos Calzado Prevencion de las ulceras por presion en pacientes de unidades de cuidados intensivos.
Indexed at
- Villamea, Silvia Martínez (2021) Beatriz Brana Marcos Prevención De Ulceras Por Presion En El Cuidados De Pacientes Colocados En Decúbito Prono. Lecciones Derivadas De La Crisis Covid-19. Revista Ene de Enfermeria 15:1.
Indexed at, Google Scholar
- Menegon, Doris Baratz (2012) Analysis de las subescalas Braden Como indicativo de riesgo para las ulcers por presión. Texto Contexto-Enfermagem 21:854-861.
Indexed at, Google Scholar
- Lima-Serrano, Marta Validez (2018) predictive y fiabilidad de la escala de Braden para valoración Del riesgo de úlceras por presión en una unidad de cuidados intensivos. Med intensive 42:82-91.
Indexed at, Google Scholar, Crossref
- Porto, Saith Hoyos (2015) Ulcers por presion en pacientes hospitalizations. Universities Medical 56:341-355.
Google Scholar
- Samper, Albert (2014) Diego Carrillo Úlceras por person. Sobre Ruedas 86:4-7.
Google Scholar
- Peris Armero, Alejandra, Victor M, Gonzalez-Chorda (2018) Prevención de ulcers por person en el paciente encamado nuevas evidencias.
Google Scholar
- Casallas, Julio Cesar Garcia (2013) Lizeth Katherine Barrera Prophylaxes de sangrado gastrointestinal en paciente crítico. Revista Colom de Enfer 8:123-130.
Indexed at, Google Scholar
- Sanchez, Yurisnel Ortiz El (2019) uso de antiulcerosos como profilaxis en pacientes hospitalizations en el servicio de cardiología. Revista Cubana de Farmacia 51.4.
Google Scholar
- Chaves, Ninfa Marlen, Diego A Nivia (2015) Uso de inhibidores de la bomba de protones y antagonistas de los receptores H2 de histamina como profilaxis en úlceras por estres una practica justificada. Revista Colombiana de Enfermeria 11:82-92.
Google Scholar
- Ye Zhikang (2020) Gastrointestinal bleeding prophylaxis for critically ill patients: a clinical practice guideline. Bmj 368.
Indexed at, Google Scholar, Crossref
- Valle, Betsy (2017) Evaluación de la prescripcion profiláctica de omeprazol y ranitidina mediante la identification de factores de riesgo de sangrado gastrointestinal. Revista Colombiana de Ciencias Quimico-Farmaceuticas 46:49-60.
Indexed at, Google Scholar
- Balcells, Joan (2005) Farmacos inotropicos y vasoactivos. pediatr Contin 3:244-247.
Indexed at, Google Scholar
- Lopez Ferreruela (2021) Irene Delia Maria Gonzalez de la Cuesta. Drogas vasoactivas en UCI, cuidados y responsabilidades de enfermería y su importancia para el paciente.
Google Scholar
- Perez-Calatayud, Angel Augusto (2017) Actualidades en el control metabolic Del paciente critic hyperglycemia, variabilidad de la glucosa, hypoglycemia e hypoglycemia relative. Cirugia y cirujanos 85:93-100.
Indexed at, Google Scholar, Crossref
- Aramendi, Ignacio, Gaston Burghi, William Manzanares (2017) Disglucemia en el paciente crítico: evidencia actual y perspectives futuras. Revista Brasileira de Terapia Intensiva 29:364-372.
Google Scholar
- Arias-Amaya, Adriana Milena (2020) Aspectos clínicos Del tratamiento de la hiperglucemia no complicada en la unidad de cuidados intensivos." Médicas UIS 33:49-54.
Google Scholar, Crossref
- Paredes MC (2009) Luna Fundamentos de la oxigenoterapia en situaciones agudas y crónicas: indicaciones, métodos, controls y seguimiento. Anales de Pediatria 71:2.
Indexed at, Google Scholar, Crossref
- Machado Garcia, Jorge Luis, Zaily Fuentes Diaz, Orlando Rodríguez Salazar (2011) Monitorización de la oxigenación en pacientes críticos. Revista Archivo Medico de Camaguey 15:697-704.
Google Scholar
- Fuentes-Diaz, Zaily (2018) Evaluation the oxygenation prognosis factors in critical patients with airway adjuncts. Revista Archivo Medico de Camaguey 22:715-724.
Indexed at, Google Scholar
- Wilches, Esther Cecilia (2004) Rehabilitation functional del paciente neurologic en la UCI." Guía Neurological 119-142.
Indexed at, Google Scholar
- Maslove D M, Lamontagne F, Marshall J C, Heyland D K (2017) A path to precision in the ICU. Critical Care 21:1-9.
Indexed at, Google Scholar, Crossref
- Murphy (2012) Pediatric Neurocritical care. Neurotherap 9:3-16
Indexed at, Google Scholar, Crossref
- Munoz-Cespedes JM, Paul-Lapedriza N, Pelegrin-Valero C, Tirapu-Ustarroz J (2012) Factores de pronostico en los traumatismo craneoencefálico. Revista cubana de Neurologia y Neuro 2:28-33.
Indexed at, Google Scholar
Citation: Isaias GC, Duenas C, Perales K,
Tafur Delgado Juan E, Andres SG, et al.
(2022) Approach to patient Management In
Critical Condition. Health Sci J. Vol. 16 No. S7:
957.