Ogolodom Michael Promise1*, Obetta Thaddaeus Chinedu2, Bakre Abdulfati Kolawole3 and Egbeyemi Oluwafemi Olumide4
1Department of Radiology, Braithwaite Memorial Specialist Hospital Port Harcourt, Rivers State, Nigeria
2Technomedics Diagnostics, Port Harcourt Rivers State, Nigeria
3Esteem Diagnostic Medical Services Limited, Lagos Nigeria
4Department of Radiography and Radiological Sciences, Faculty of Health Sciences and Technology, Nnamdi Azikiwe University, Anambra State, Nigeria
*Corresponding Author:
Ogolodom Michael Promise
Department of Radiology
Braithwaite Memorial Specialist Hospital Port Harcourt
Rivers State, Nigeria
Tel: +234803997393
E-mail: mpos2007@yahoo.com
Received Date: 08 October 2018; Accepted Date: 20 October 2018; Published Date: 29 October 2018
Citation: Promise OM, Chinedu OT, Kolawole BA, Olumide EO (2018) Assessment of Awareness and Usage of Insecticide Treated Bednets among Pregnant Women Referred for Obstetric Scans in Port Harcourt Metropolis Rivers State Nigeria. Health Sci J Vol.12.No.5:597.
Copyright: © 2018 Promise OM, et al. This is an open-access article distributed under the terms of the creative commons attribution license, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
DOI: 10.21767/1791-809X.1000597
Keywords
Malaria; Pregnancy; Obstetric scan
Introduction
Malaria in pregnancy is a major public health challenge with significant risks for pregnant mother, her fetus and the newborn [1]. Malaria related maternal illness and low birth weight is often due to Plasmodium falciparium infection and occurs mostly in Africa [1]. The WHO defines malaria as a disease poverty caused by poverty. Twenty five million of pregnant women are recently at risk for malaria, and according to World Health Organization, malaria accounts for more than 10,000 maternal and 200,000 neonatal deaths per year [1]. Malaria in pregnancy causes higher rates of miscarriage, intrauterine discharge, low-birth weight neonates, neonatal death and premature delivery [2]. Malaria is treated when infected mosquito plasmodium sporozoites are transferred from the mosquito saliva into the capillary bed of the host. After sometimes, the parasite moves to the liver, where it further undergoes cycling and replication before been released back into the host’s blood stream [2,3]. In previous studies [2-4], they reported that pregnant mothers are 3 times more likely to be attacked by diseases related to malaria infection compared to their non-pregnant counterparts, and have a mortality rate from severe disease that approaches 50%. According to Julianna and Nawal [2], the main sequelae in pregnancy is due to two main factors; the placental sequestration of the infected erythrocytes which contributes to increasing risk and severity of obstetric conditions such as post-partum hemorrhage by as much as 50%, pre-eclampsia/ eclampsia and the immune compromised state of the pregnancy [5,6]. A study conducted in Ghana among 300 women delivering in rural areas, shows that babies born by mothers with placental malaria infections were more than twice as likely to be underweight at birth which can be detected with Ultrasound scan [7].
Increasing funding the in combating malaria and maternal mortality has spinned into action the creation of awareness of the preventive measures for malaria which is a collective responsibilities of both health practitioners and nonpractitioners alike. According to WHO, the preventive measures for malaria in pregnancy is centered on the use of insecticide treated bed nets (ITNS) and intermittent presumptive treatment (IPT) with anti-malaria medications? The WHO recommended that all pregnant women living in malaria endemic regions should use insecticide treated bed nets. The meeting of the African Heads of state held in Abuja in 2000, the major outcome, was the introduction of insecticide treated bed nets with pregnant women and children between the ages of 0-5 years were the target population, since they are more prone to malaria attack [8,9]. Similar studies [10,11] reported that insecticide treated bed nets used in pregnancy drastically reduced the incidence of malaria and its complications in pregnancy. Several studies have reported poor practice of using insecticide treated bed nets among pregnant women in Nigeria, which according to them, could be to inadequate awareness of the preventive ability of ITNs against malaria infection during pregnancy, and they also asserted that the level of awareness varies from one place to another [12-18]. Although similar studies [19,20] show a slight improvement in the use and awareness of insecticide treated bed nets. There is need to help the government and other health care providers across the globe to create awareness of the preventive measures for malaria in pregnancy to reduce malaria related diseases and its complications among pregnant women especially in Nigeria. This study is aimed at evaluating the level of awareness and usage of insecticide treated bed nets among pregnant women referred for obstetric scan in Port Harcourt Rivers State, Nigeria.
Material and Methods
A prospective cross sectional study design was adopted in this study. All the ultrasound obstetric scans were performed with different ultrasound machines by Sonographers. This study was restricted to Rivers State South-South geopolitical zone of Nigeria and the population recruited for this study was pregnant women who were referred by their physicians for obstetric ultrasound scan with malaria related clinical indications such as fetal growth restriction, placental problems, suspection of miscarriages, low maternal weight and low maternal body mass index. An ethical approval was obtained from the institutions research and ethic committees. Informed consent was also obtained from the participants, and all the information obtained were treated with high level of confidentiality, and used only for the purpose of this research. The data used for this study were collected using structured questionnaires. The questionnaires were administered to the subjects at the various waiting areas immediately after the scan while waiting for their scan reports. The support of the Sonographers performing the scan was properly sought. A total of 456 pregnant women were recruited in this study using convenience sampling technique. The obtained data were processed and analyzed using Scientific Package for Social Sciences (SPSS) version 21 and descriptive statistic. This study was conducted between August, 2017 and October, 2017.
Results
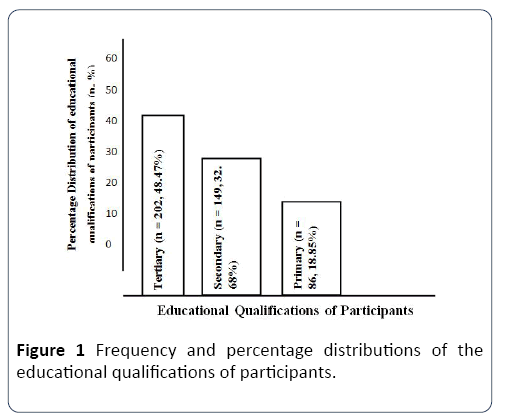
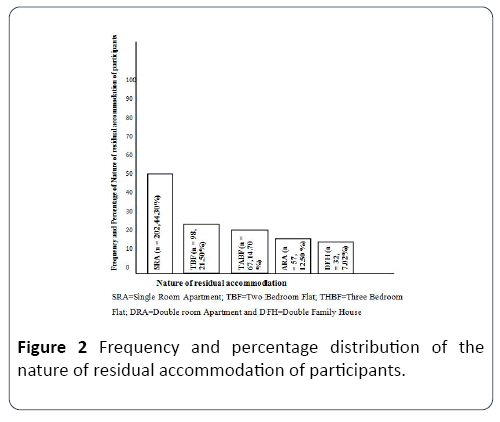
Table 1 shows the age group distributions of the pregnant women. Age group 20-30 years has the highest percentage 54.61% (n=249) and the least was within age group 41-50 years which is 8.77% (n=40). From Figure 1, those with higher educational qualifications were highest 48.47% (n=202) and the least were primary school certificate holders which is 18.85% (n=86). From Table 2, the greater numbers of the participants were within pregnancy age of first trimester 47.81% (n=218) while the least were within the second trimester 20.83% (n=95). The same Table 2 also shows that 75.22% (n=343) participants had their antenatal clinic registration while the remaining 24.78% (n=113) participants did not had any antenatal registration. From Table 2 also, majority of the participants were those that has only one pregnancy 41.01% (n=187) followed by those without previous pregnancy 20.83% (n=95). Out of 456 participants, 45.40% (n=207) of those that used the ITNs sometimes were highest followed by those that used it always 27.41% (n=125) and the least were those that never used it 27.19% (n=124). Among those that used ITNs always, 19.74% (n=90) had normal pregnancy in their obstetric scan findings, while 3.51% (n=16) had placenta problems (Table 3). Out of 27.19% (n=124) participants that never used ITNs during their pregnancies, 10.09% (n=46) had normal pregnancy findings in their obstetric scan while the remaining 17.10% (n=78) had abnormal obstetric scan findings (Table 3). Large numbers of the participants had no specific reasons for not using ITNs 40.32% (n=50) and the least were those that said it was expensive 9.68% (n=12) (Figure 2). In Table 4, out of 125 participants that uses ITNs always, those that have four and above number of previous pregnancies were highest 35.2% (n=44) and the least were those without previous pregnancy 8% (n=10). Among the participants, those that lived in single room apartment were highest 44.30% (n=202) and the least were those that lived in Duplex family house 7.02% (n=32) (Figure 3).
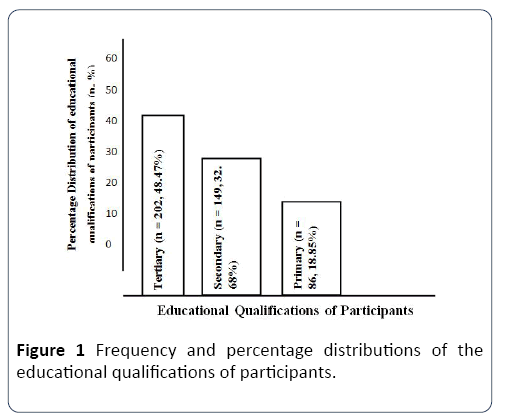
Figure 1: Frequency and percentage distributions of the educational qualifications of participants.
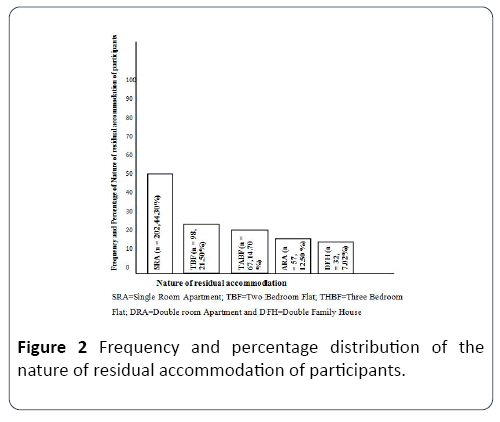
Figure 2: Frequency and percentage distribution of the nature of residual accommodation of participants.

Figure 3: Frequency of not using insecticide treated bed nets (ITNS).
Table 1 Age distributions of pregnant women.
| Age group (Years) |
Frequency (N) |
Percentage (%) |
| 20-30 |
249 |
54.61 |
| 31-40 |
167 |
36.62 |
| 41-50 |
40 |
8.77 |
| Total |
456 |
100 |
Table 2 Frequency and percentage distributions of participants obstetric history.
| Obstetric History |
Frequency (N) |
Percentage (%) |
| Number of pregnancies |
| None |
95 |
20.83 |
| One |
185 |
41.01 |
| Two |
81 |
17.70% |
| Three |
43 |
9.43 |
| Four and above |
50 |
10.97 |
| Age of their present pregnancies |
| First trimester |
218 |
47.81 |
| Second trimester |
95 |
20.83 |
| Third trimester |
143 |
31.83 |
| Antenatal clinic registration |
| Yes |
343 |
75.22 |
| No |
113 |
24.78 |
| Time of registration at the antenatal clinics |
| 0–3 months |
235 |
51.54 |
| 4–6 months |
164 |
35.97 |
| 7–9 months |
57 |
12.49 |
| |
Table 3 Frequency distribution of the obstetric scan findings and the usage of Insecticide Treated Bednets (ITNs).
| Obstetric scan findings |
Rate of Usage of ITNs |
| Sometimes |
Always |
Never |
Total |
| Normal pregnancy |
28.07 (n=128) |
19.74 (n=90) |
10.09 (n=46) |
57.90 (n=264) |
| Intrauterine fetal death |
1.32 (n=6) |
0.88 (n=4) |
2.41 (n=11) |
4.61 (n=21) |
| Placenta problems |
4.82 (n=22) |
3.51 (n=16) |
8.34 (n=38) |
16.67 (n=76) |
| Intrauterine growth retardation |
5.26 (n=24) |
1.97 (n=9) |
2.2 (n=10) |
9.43 (n=43) |
| Other findings not specified |
5.92 (n=27) |
1.32 (n=6) |
4.15 (n=19) |
11.39 (n=52) |
| Total |
45.40 (n=207) |
27.41 (n=125) |
27.19 (n=124) |
100 (n=456) |
Table 4 Frequency of previous pregnancy and the regular usage of ITNs.
| Number of Previous pregnancy |
Always users of ITNs (N) |
Percentage (%) |
| None |
10 |
8 |
| One |
17 |
13.6 |
| Two |
24 |
19.2 |
| Three |
30 |
24 |
| Four and above |
44 |
35.5 |
| Total |
125 |
100 |
Discussion
The finding in this study shows that there is increased awareness and usage of Insecticide Treated Bed nets (ITNs) among pregnant women referred for obstetric scans included in our study with 90% awareness level. This is in keeping with other similar studies conducted in Nigeria and other part of African [18,21,22]. Similar studies conducted in South West geopolitical zone of Nigeria precisely Osun and Lagos states [12,19] reported 41.1% and 91% as ITNs awareness level respectively. Other previous studies [19,23-25] documented awareness levels of ITNs as 91%, 88.6%, 36% and 91% in South-East, South-South and Northern Zones of Nigeria respectively. The discrepancies in our findings could be ascribed to the sample size studied, geographical variation and inclusion criteria used for sample selection. In this study, only pregnant women with clinical history of malaria and were referred for obstetric scans were included, whereas in other studies, their sample size was drawn from women that attended antenatal clinics. With the increasing efforts of both government and private organizations on the disseminations of information about the uses and importance of Insecticide Treated Bed nets during pregnancy, one would have expected that the awareness level should have reached 98%.
Greater proportions of the participants were within the 2nd and 3rd decades. This could be attributed to the fact that pregnant women of this age group are usually very anxious to know the physical wellbeing of their fetus with an Ultrasound scan. Majority of the participants were people with first time pregnancy.
With regard to the reasons for not using the ITNs by participants, over 40% had no specific reasons for not using the Insecticide Treated Bed nets. This is in agreement with the findings of similar studies [18,26,27]. According to Edelu et al. [25], they attributed this finding to nonchalant behavior of pregnant women towards the use of ITNs. We equally agreed with Edelu et al. [25] reasons, following the fact that huge population in this study were those with tertiary educational levels, which one would have expected that those without specific reasons for not using Insecticide Treated Bed nets should have been the lowest percentages of the total participants when compared with those with reasons for not using the ITNs. From the above, one can deduced that educational status has no influence on the ITNs usage during pregnancy.
The patterns of obstetric scan findings were also evaluated and greater number of the participants had normal obstetric scan reports. This is not in keeping with observations documented by Julianna and Monif [2,3]. According to them, pregnant women are 3 times likely to be attacked by diseases related to malaria infections such as placenta problems, fetal growth restriction and intrauterine fetal death. These differences may be attributed to the sample size studied, the increased level of awareness and usage of ITNs during pregnancy and the geographical variation. The abnormal ultrasound scan findings noted in study were malaria -related. Further research study should be carry out on this subject area and the statistical correlation between the obstetric scan report’s findings and the level of awareness and usage of Insecticide Treated Bed nets should be evaluated.
Conclusion
Although there is increased awareness level and usage of Insecticide Treated Bed nets among participants recruited in this study, the awareness level is still below expectation of about 98%. Large numbers of the participants were younger pregnant women with high percentage of tertiary educational status. This higher educational status does not really influenced their attitude of not using the Insecticide Treated Bed nets, as majority of them said they have no specific reasons for not using the net. Although there are abnormal obstetric scan findings among the participants, normal obstetric scan finding was the most common findings and this shows that the net is useful in preventing malaria-related infections and complications in pregnancy. To actually win a war against malaria related complications in pregnancy, both the government and health workers need to increase the ITNs awareness and usage campaign via health education at all the levels of educational system.
23555
References
- World Health Organisation. Global Malaria Programme: Pregnant women and infants. 2007.
- Julianna SD, Nawal MN (2009) Malaria and pregnancy: a global health perspective. Rev Obstet Gynecol 2: 186-192.
- Monif GRG, Baker DA (2004) Infectious disease in obstetrics and gynecology. (6th edn.). New York, Parthenon, pp: 280-286.
- World Health Organization. Guidelines for treatment of malaria. Geneva. WHO, 2006.
- Brabin BJ, Johnson PM (2005) Placental malaria and pre-eclampsia through the looking glass backwards? J Reprod Immunol 65: 1-15.
- Brain BJ, Verhoeff F (2002) The contribution of malaria. In: Maclean AB, Neilson JP (Eds.). Maternal, morbidity and mortality. London, RCOG Press. pp: 65-78.
- Ofor MF, Ansah E, Agyepong Ofori-Adjei D, Hviid L, et al. (2009) Pregnancy-associated malaria in rural community in Ghana. Ghana Med J 43: 13-18.
- Okwa OO (2004) Preliminary investigations on malaria in sickle cell patients among pregnant women and infants in Lagos, Nigeria. Niger J Parasitol 25: 81-85.
- Richard WS, Bernard L, Nah L, Mornica E, Clara PM (2001) The burden of malaria in pregnancy in malaria endemic areas. Am J Trop Med Hyg 64: 28-35.
- Adenyemi AS, Adekande DA, Akinola SE (2007) Use and prevalance of insecticide treated mosquito bed nets among pregnant population in Oshogbo Nigeria. Nigerian Medical Practice 52: 29-32.
- Gamble CL, Ekwaru JP, Terkuile FO (2006) Insecticide treated nets for preventing malaria in pregnancy. Cochrane data base of systematical reviews.
- Aina BA, Ayeni FA (2011) Knowledge and use of insecticide treated nets as malaria preventive tool among pregnant women in a local government area in Lagos State Nigeria. J Appl Pharmaceut Sci 1: 162-166.
- Aluko JO, Oluwatosin AO (2012) Utilization of insecticide treated nets during pregnancy among postpartum women in Ibadan Nigeria: A cross sectional study. BMC Pregnancy Childbirth 29: 12-21.
- Musa OI, Salaudeen GA, Jimo RO (2009) Awareness and use of insecticide treated nets among women attending antenatal clinic in a Northern State Nigeria. J Parkisan Med Assoc 59: 354-358.
- Isah AY, Nwobodo EI (2009) Awareness and Utilization of insecticide treated mosquito nets among pregnant mothers in a tertiary health institution in North-Western Nigeria. Niger J Med 18: 175-178.
- Salaudeen GA, Jimoh RO (2009) Awareness and use of insecticide treated net among women attending antenatal clinics in a Northern State of Nigeria. J Parkisan Med Assoc 59: 354-358
- Runsewe-Abiodum TI, Inyanwura AC, Sotimehin SA (2009) Awareness and Knowledge about insecticide treated nets amongst pregnant mothers in Ogun State, Western Nigeria: A descriptive cross sectional study. Educ Res J 2: 138-145.
- Ukibe SN, Mbanugo JI, Ukibe NR, Ikeakor LC (2013) Level of awareness and use of insecticide treated bed nets among pregnant women attending antenatal clinics in Anambra State, South Eastern Nigeria. J Public Health Epidemiol 5: 391-396.
- Adeneye AK, Jegede AS, Mafe MA, Nwokocha EE (2007) A pilot study to evalutate malaria control strategies in Ogun State, Nigeria. World Health Population 9: 83-94.
- Osero JS, Otien ME, Orago AS (2005) Maternal use of insecticide treated nets in prevention of malaria among children under 5 years in Nyamira district Kenya. East AfrMed J 82: 495-500.
- Baume CA, Marin MC (2008) Gains in awareness, ownership and use of insecticide treated nets in Nigeria, Senegal, Uganda and Zambia. Malar J 7: 153.
- Sangare LR, Weis NS, Brentilinger PE, Richardson BA, Staekete SG, et al. (2012) Determination of use of insecticide treated nets for the prevention of malaria in pregnancy: Jinga Uganda. Plos One 7: e39712.
- Okoye CA, Isara AR (2011) Awareness on the use of insecticide treated nets among women attending antenatal clinic in tertiary health in South-South Nigeria. Nigeria Med Prac J 52: 67-70.
- Oche MO, Ameh IG, Umar AS, Gana G, Njoku CH Awareness and use of insecticide treated nets among pregnant women attending antenatal at Usman Dan Fodio University Teaching Hospital Sokoto. Nigeria J Parasitol 53: 162-165.
- Edelu BO, Ikefuma AN, Emodi JI, Adimora GN (2010) Awareness and use of insecticide treated bed nets among children attending outpatient clinic at UNTH, Enugu-the need for an effective mobilization process. Afr Health Sci 10: 117-119.
- Onwujekwe O, Uzochukwu B, Ezumah N, Shu E (2005) Increasing coverage of insecticide treated nets in rural Nigeria: implications of consumers’ knowledge, preference and expenditure for malaria prevention. Malar J 4: 29.
- Oreanya OB, Hoshen M, Sofola OT (2008) Utilization of insecticide treated nets by under five in Nigeria: Assessing progress towards the Abuja target. Malar J 7: 145.