Research Article - (2024) Volume 18, Issue 1
ASSESSMENT OF EXCLUSIVE BREASTFEEDING PRACTICE AND ASSOCIATED FACTORS AMONG MOTHERS IN HARGEISA CITY, SOMALILAND.2023.
Mohamed Ibrahim Muhumud*
School of Graduate Studies, College of Health and Medical Sciences, Jigjiga University, Ethiopia
*Correspondence:
Mohamed Ibrahim Muhumud, School of Graduate Studies, College of Health and Medical Sciences, Jigjiga University,
Ethiopia,
Email:
Received: 02-Jan-2024, Manuscript No. iphsj-24-14545;
Editor assigned: 05-Jan-2024, Pre QC No. iphsj-24-14545;
Reviewed: 19-Jan-2024, QC No. iphsj-24-14545;
Revised: 26-Jan-2024, Manuscript No. iphsj-24-14545;
Published:
31-Jan-2024
Abstract
Background: Information breast milk is the one and only natural, complete and complex nutrition for human infants. Also, exclusive breastfeeding is the best and cost effective intervention to prevent childhood morbidities and mortalities, exclusively breastfed children are at a much lower risk of infection from diarrhea, acute respiratory infections, pneumonia, meningitis, ear infections, lower rates of childhood cancers including leukemia and lymphoma than infants who receive other foods. However, over two-thirds deaths occurring worldwide during the first year of life children are often associated with inappropriate feeding practices, especially due to poor exclusive breastfeeding practices.
Objective: To assess exclusive breastfeeding practices and associated factors among mothers who have infants less than six months old at public health facility in Hargeisa, Somaliland. 2023
Methodology: The study was used institution based cross-sectional design and the sample size was 264. Structured questionnaire was also used. The data than was entered, coded and cleaned into Epi data version 3.1 and was exported to Statistical Package for Social Science (SPSS) version 20 for further analysis. Descriptive statistics was used to summarize the socio-demographic characteristics’ of the study participants and bivariate logistic regression was performed to each independent variable with the outcome variable and those variables with a p value < 0.05 was included in the final model (multivariate analysis). Strength of association was measured using odds ratio, and 95% confidence intervals. Statistical significance was declared at P value <0.05.
Results: The prevalence of exclusive breastfeeding in the study area was 50.1%. Among different socio-demographic, health service, maternal, and infant related factors studied; Age of the child, maternal occupation, household income, breastfeeding counseling during ANC, husband support of breastfeeding, colostrum feeding and not feeding prelactal were the determinant factors for higher chance of EBF practice.
Recommendation: The government should work on promoting behavior change communication on exclusive breastfeeding practice and take appropriate actions to avoid other related traditional activities which discourage EBF
Introduccion
Information Breast milk is the one and only natural, complete and complex nutrition for human infants. It is superior to any product given to a baby and it is immediately available, fresh, temperature always correct and constant, economical [1]. It gives all infants nutritional fluid needs in the first six months and is a perfect mixture of proteins, fats, carbohydrate and fluids [2]. Nutrients such as vitamins A and C, iron, zinc and vitamin D are more easily absorbed from breast milk than from other milk. And it contains essential fatty acids needed for the infant’s growing brain, eyes, and blood vessels and these are not available in other milks [1,3]. Breast milk contains antibodies that can protect infants from bacterial and viral infections and it helps the child to fight germs and reduces the risk of developing infections [1]. Breastfed babies have fewer infections in their early life, less diarrhea and vomiting, chest and ear infections because breast milk help a baby’s own immune system work best [2]. Exclusive breastfeeding means babies are given only breast milk and nothing else-no other milk, food, drink, even no water for the first six months of life since it provides best and complete nourishment for the baby during the first six months of life [3-5]. Exclusive breastfeeding is recommended because breast milk is uncontaminated and contains all the nutrients necessary in the first six months of life.
In addition, the mother’s antibodies in breast milk provide the infant with immunity to disease [6]. Exclusively breastfed children are at a much lower risk of infection from diarrhea, acute respiratory infections, pneumonia, meningitis, ear infections, lower rates of childhood cancers including leukemia and lymphoma than infants who receive other foods [3-5]. Early supplementation is discouraged for several reasons. First, it exposes infants to pathogens and thus increases their risk of infection, especially diarrheal disease. Second, it decreases infant's intake of breast milk and therefore suckling, which in turn reduces breast milk production. Third, in low resource settings, supplementary food is often nutritionally inferior [6].
Statement of the problem
Over two-thirds deaths occurring worldwide during the first year of life children are often associated with inappropriate feeding practices, especially due to poor exclusive breastfeeding practices [7]. Suboptimal breastfeeding contributes for 45% of neonatal infectious deaths, 30% of diarrheal deaths and 18% of acute respiratory deaths among under five children in developing countries [8-10]. It also accounts for 10% of the disease burden in children less than 5years old [11].
A total of 96% of all infant deaths (i.e. 1.24 million deaths) occur during the first six months of life are attributable to nonexclusive breast feeding which is much higher in Asia and Africa. It accounts 55% of diarrheal deaths and 53% of acute respiratory deaths in the first six months of life [9].
Compared with exclusive breastfeeding in the first few months of life, partial or no breastfeeding is associated with a 2.23-fold higher risk of infant deaths resulting from all causes and 2.40- and 3.94-fold higher risk of deaths attributable to pneumonia and diarrhea, respectively [10]. Non-exclusive breastfeeding is known to compromise the nutritional status of children.
It results an estimated 40% of underâ?five stunting in Western and central Africa (WCA) and more than 60% in some other countries [11-15].
Significantly, prevented by nutrition interventions such as exclusive breastfeeding [16]. In Ethiopia 52 % of children less than six months old are exclusively breastfed [6]. And Ethiopian HSDP IV planned to increase in the proportion of exclusively breastfed infants under age 6 months to 70 % by the end of 2015 [12].
Breastfeeding and good nutrition for children are recognized as essential for achieving the Millennium Development Goals (MDG), particularly the goals relating to child survival, such as reducing child mortality by 2/3 between 1990 and 2015 [13,14]. Therefore the purpose of this study was to assess exclusive breast feeding practices and associated factors among mothers of children less than 6 months old in Hargeisa city, Somaliland.
Objectives
General objective
To assess exclusive breastfeeding practices and associated factors among mothers who have infants less than six months old at public health facility in Hargeisa, Somaliland. 2023.
Specific objectives
To determine the prevalence of exclusive breastfeeding among mothers attending public health facility in Hargeisa, Somaliland, 2023
To assess socio demographic characteristics among mothers attending public health facility in Hargeisa, Somaliland, 2023
To identify factors associated with exclusive breastfeeding among mothers, attending public health facility in Hargeisa, Somaliland, 2023
Methods and Materials
Study area and period
This study was carried out in Hargeisa city. Hargiesa is a city situated in the Marodi-Jeh region of the self-declared but internationally unrecognized Republic of Somaliland in the Horn of Africa .It is the capital and largest city of Somaliland.
Hargeisa is located in an enclosed valley of them north western Galgodon (Ogo) highlands. It sits at an elevation of 1,334 meters (4,377 feet) above sea level. According to CIA fact book, Hargeisa has estimated population of around 760,000 as of 2015. It is the 700th largest city in the world by population size. The urban area occupies 75 square kilometers (29 sq mi), with a population density of 12,600 inhabitants per square kilometer (33,000/ sq mi). The average temperatures range from 18co in the months of December and January to 24co in the month of June. The common foods consumed in Hargeisa are food items like, rice, pasta, meat, suger , dates and wheat flour product foods.
Hargeisa has one main public Hospital called Hargeisa group hospital and 12 health centers which are managed by the government. This study was started from March 2023 to may 2023 in Hargiesa public health facilities.
Study design
Facility based Cross sectional study design was used.
Source and Study Population
Source population
All mothers who had infant less than 6 months old attending public health facility in Hargeisa.
Study population
All randomly selected mothers who had an infant less than six months old i attending public health facility in Hargeisa.
Inclusion and exclusion criteria
Inclusion criteria
Mothers who had an infant less than 6 months old and available at the time of data collection.
Who lived in the area at least for six month.
Exclusion criteria
Mothers who were seriously ill or unable to give the required information during data collection period were excluded from the study.
Sample size determination
Sample Size Determination for the First Objective
Sample size calculated by using single proportion population formula. It was calculated by considering 39% (prevalence of breast feeding in Somalia according to UNICEF report 2016. 5% margin of error and 95% confidence interval (CI), Sample size is calculated as follows:
n = [(Zα/2)2p (1-p)]/d2
n= desired sample size, Z = the normal standard deviate (level of statistically significant) which is set at 1.96 the corresponds to 95% confidence level, P = estimated prevalence breast feeding practices is 39 % in Somalia, q= 1-p =1-0.558=0.442, d = degree of accuracy essential, usually set at 0.05 %.
Sampling procedure and technique
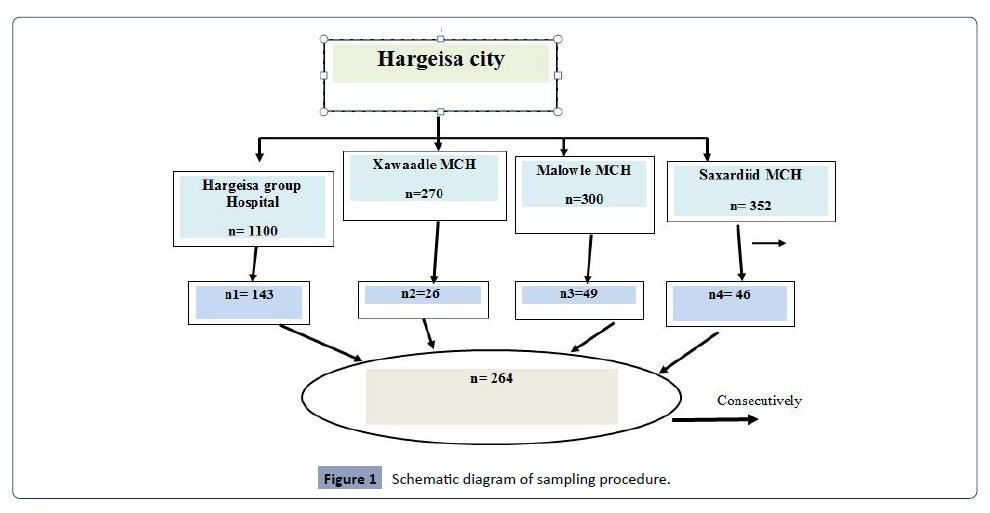
This study was carried out in one Public Hospital and three Health center in Hargeisa city. Hargeisa has one public hospital and three health centers, one public hospital and three health centers are selected randomly by lottery method. Then 264 of sample size was distributed among health facilities according to proportional allocation to their size (PAS). Breast feed mothers who will come in selected public health facilities was selected consecutively and their mothers was interviewed. The data was collected and recorded until the sample size is achieved (Figure 1).
Figure 1: Schematic diagram of sampling procedure.
Data collection techniques and procedures
Structured questionnaire was prepared after reviewing different published literatures and then adapted to the local situation. The questionnaire was first prepared in English and then translated to Somali language. Retranslation was also be made to see the consistency of both questionnaires. After this, the questionnaire was used in interviewing the study participants through face to face interview method. Data collection was facilitated by health professionals using structured and pretested questionnaire. Further, supervision was also made by the principal investigator.
Study variables
Dependent variable
Exclusive breastfeeding practice
Independent Variable
Maternal related (Age, Ethnicity, Religion, Marital status, Educational status, Occupation, Mothers knowlege on breastfeeding, Exposure to information about breastfeeding, Maternal illness).
Obstetric & Health service related (Parity, Antenatal care, Breast feeding counseling during pregnancy, Place of delivery 24, Mode of delivery).
Postnatal care Infant related (Age, Sex, Birth order, Birth interval, Timely initiation of breastfeeding, Colostrum feeding status, Prelacteal feeding status.
Sociocultural related factors (Husband occupation, Husband educational status, Husband support, Income, Type of family, Cultural support, Organizational support).
Data quality control
To assure the quality of data, training was given for data collectors about the objective of the study, confidentiality issues, study participant’s right, consenting, and techniques of interview.
Daily supervision was made during the data collection period. The Questionnaires was pre-tested prior to the actual data collection. The collected data was checked for their consistency and completeness daily.
Data processing and analysis
All data should be checked for completeness than was entered, edited, coded and cleaned into Epi data version 3.1 and was exported to Statistical Package for Social Science (SPSS) version 20 for further analysis. Descriptive statistics was used to summarize the socio-demographic characteristics’ of the study participants and the prevalence of exclusive breast feeding. To identify factors associated with exclusive breastfeeding practice, binary logistic regression analysis carried out at two levels, first bivariate logistic regression was performed to each independent variable with the outcome variable and those variables with a p value <0.05 was included in the final model (multivariate analysis). Strength of association was measured using odds ratio, and 95% confidence intervals. Statistical significance was declared at P value <0.05.
Ethical consideration
Ethical approval was obtained from new generation University department health services management Ethical Review Committee. Official letter will send to Somaliland ministry of health than data collection will star after permission will get. To ensure confidentiality, it was study that names of the study subjects will not write on the questionnaire. Written consent from the study participants will obtain after they was briefed about the research intent and was asked for their willingness to participate in the study and will not be forced. Their right of denial to participate in the study will also assure Information.
Results
Socio-demographic characteristics
Total of 264 were agreed to participate in this study, which made a response rate of 100%. . Around one third (36 %) of mothers were between 25-30 years. With regard to educational status, 121(45.9%) mothers were Illiterate at all. Majority 154 (58.3%) of study participants were house wife mothers. From all, 221 (83.7%) mothers were married. The average household income of the respondents was $100 and less per month, and 101(38.2%) respondents earn between $ 100- $200 per month (Table 1).
| Variable |
Category(n=246) |
Frequency |
Percent |
| Age of mother( in years) |
15-19 |
9 |
3.4% |
| |
20-24 |
81 |
30.7% |
| |
25-30 |
95 |
36% |
| |
31-40 |
70 |
26.5 % |
| |
41 and above |
9 |
3.4.% |
Level of education of
Mother |
Illiterate |
121 |
45.9 % |
| Primary level (1-8 grade) |
41 |
15.5 % |
| |
Secondary school and above |
102 |
38.6% |
Occupational status of
Mother |
Housewife |
154 |
58.3% |
| Government employed |
63 |
23.9% |
| |
Private organization employed |
19 |
7.2% |
| |
Merchant |
28 |
10.6% |
| Current marital status |
Married |
221 |
83.7% |
| |
Widowed |
23 |
8.7% |
| |
Divorced |
20 |
7.6% |
| Household income |
<$100 |
129 |
48.9% |
| |
$100-$2000 |
101 |
38.2% |
| |
>$200 |
34 |
12.9% |
Table 1: Socio-demographic characteristics mothers who have infants less than six months old, at health facility, in Hargeisa, Somaliland, 2023.
Maternal and infant health characteristics
Nearly half (46.6 %) of mothers have 2-3 children. Majority of the infants 164 (62.2%) were females, and 103 (39.0%) infants were between 2-3 months old. Almost half 134 (50.8%) infants were first in birth order. Majority230 (87.1%) of mothers received antenatal care (ANC) during period of pregnancy out of them only 173 (65.5%) were counseled concerning to breast feeding .With regarding to place of delivery, most 234 (88.6%) mothers delivered in health institution. From total respondents, majority 180 (68.2%) of mothers received postnatal care (Table 2).
| Variable |
Response (n=264) |
Frequency |
Percent (%) |
| Number of children |
One |
93 |
35.2% |
| |
Two to three |
123 |
46.6% |
| |
Four and above |
48 |
18.2% |
| Sex of child |
Male |
100 |
37.7% |
| |
Female |
164 |
62.1% |
| Age of child |
0-1month |
93 |
35.2% |
| |
2-3month |
103 |
39.0% |
| |
4-5 month |
68 |
25.8% |
| Birth order |
First |
134 |
50.8% |
| |
Second |
95 |
36.0% |
| |
Third and above |
35 |
13.2% |
| ANC follow up |
Yes |
230 |
87.1% |
| |
No |
34 |
12.9% |
| Number of ANC follow up |
Less than or equal to three |
63 |
23.9% |
| |
Four times |
201 |
76.1% |
Counseling related breast feeding during
ANC |
Yes |
173 |
65.5% |
| No |
91 |
34.5% |
| Place of birth |
Health facility |
234 |
88.6% |
| |
Home |
30 |
11.4% |
| PNC |
Yes |
180 |
68.2% |
| |
No |
84 |
31.8% |
Counseling related breastfeeding
during PNC |
Yes |
241 |
91.3% |
| No |
23 |
8.7% |
Table 2: Infant and maternal health characteristics of study participants at health facility, in Hargeisa, Somaliland, 2023.
Breastfeeding and related practices
All mothers have breastfed their current infant for a certain period of time. From total, 243 (92.0%) mothers initiated breast milk to infant immediately within one hour of birth. Most mothers (79.8%) fed colostrum/first milk to the newborn. Majority 250 (94.6%) of mothers didn't give pre-lactal food other than breast milk within three days of an infant life. Among mothers who didn’t exclusively breastfeed their infant, the main reasons mentioned were; perception of breast milk only not sufficient for infant 41(37.3 %%), maternal illness 25 (22.7%%), and infant become thirsty 15(13.6%) .42 (38.2%) of mothers were taking own decision to give other feeding (Table 3).
| Variables |
Responses (n=264) |
Frequency |
Percent |
Breastfeeding experience of
current infant |
Yes |
264 |
100% |
| No |
0 |
0.0% |
| Timely initiation of breastfed |
Yes |
243 |
92.0% |
| |
No |
21 |
8.0% |
| Colostrum feeding |
Yes |
234 |
88.6% |
| |
No |
30 |
11.4% |
| Prelacteal feeding |
No |
250 |
94.7% |
| |
Yes |
14 |
5.3% |
| Reasons for not exclusively breastfed n=110) |
Decreased breast milk secretion |
23 |
20.9% |
| |
Breast milk only not sufficient for infant |
41 |
37.3% |
| |
Infant becomes thirsty |
15 |
13.6% |
| |
Lack of time |
6 |
5.5% |
| |
Maternal illness |
25 |
22.7% |
| Who influence you to give other feeding (n=110) |
Husband/spouse |
28 |
26% |
| |
My mother |
27 |
24.5% |
| |
Mother in law |
4 |
1.5% |
| |
Health worker |
9 |
8.2% |
| |
My own decision |
42 |
38.2% |
Table 3 : Exclusive breastfeeding related practices of mothers who have infants less than six months old at health facility, in Hargeisa, Somaliland, 2023.
Factors associated with exclusive breastfeeding
According to study findings of the study participants almost 58.5% 95%CL: 49.22%-58.98%], of mothers practiced exclusive breastfeeding. In bivariate analyses (age of infant, occupation of mother, marital status, income of the household, antenatal care, breast feeding counseling during ANC, place of birth, mode of delivery, postnatal care, timely initiation of breast feeding, Colostrum feeding, prelactal feeding and husband support. Variables which were associated in exclusive breast feeding) (Table 4).
| Variables |
|
Yes |
No |
COR (95% CL) |
AOR(95% CL) |
| (N & %) |
(N & %) |
| Age of child |
0-1 |
37(67.3) |
18(32.7) |
2.840(1.526,5.283) |
3.858(1.642, 9.067)* |
| in months |
3-Feb |
69(58.0) |
50(42.0) |
1.906(1.218, 2.984) |
2.235(1.160, 4.308)* |
| |
5-Apr |
97(42.0) |
134(58.0) |
1 |
1 |
| Occupational |
Unemployed |
173(53.6) |
150(46.4) |
1.999(1.213, 3.295) |
3.008(1.459, 6.202)* |
| status |
Employed |
30(36.6) |
52(63.4) |
1 |
1 |
| Marital |
Married |
182(52.4) |
165(47.6) |
1.943(1.093, 3.455) |
|
| status |
Unmarried |
21(36.2) |
37(63.6) |
1 |
|
| Income |
<$100 |
114(57.6) |
84(42.4) |
2.634(1.597, 4.346) |
3.605(1.745, 7.451)* |
| |
$100-200 |
55(51.4) |
52(48.6) |
2.053(1.171, 3.599) |
2.342(1.116, 4.914)* |
| |
>$200 |
34(34.0) |
66(66.0) |
1 |
1 |
| ANC |
yes |
185(53) |
164(47) |
2.381(1.308, 4.335) |
|
| |
no |
18(32.1) |
38(67.9) |
1 |
|
| Breastfeedin g counseling |
yes |
131(63.6) |
75(36.4) |
2.879(1.851, 4.476) |
2.764(1.522,4.998)* |
| during ANC |
no |
54(37.8) |
89(62.2) |
1 |
1 |
| Place of birth |
Health |
185(54.7) |
153(45.3) |
3.292(1.841, 5.885) |
|
| facility |
| |
Home |
18(26.9) |
49(73.1) |
1 |
|
| Mode of |
Normal/ |
190(51.8) |
177(48.2) |
2.064(1.024, 4.160) |
|
| delivery |
vaginal |
| |
C/S |
13(34.2) |
25(65.8) |
1 |
|
| PNC |
yes |
116(58.9) |
81(41.1) |
1.992(1.341,2.958) |
|
| |
no |
87(41.8) |
121(58.2) |
1 |
|
| Timely |
yes |
184(57.7) |
135(42.3) |
4.806(2.757, 8.378) |
|
| initiation |
No |
19(22.1) |
67(77.9) |
1 |
|
| Colostrum |
yes |
185(57.3) |
138(42.7) |
4.767(2.702, 8.407) |
3.503(1.451, 8.452)* |
| feeding |
No |
18(22) |
64(78) |
1 |
1 |
| Pre-lacteal |
No |
189(58.7) |
133(41.3) |
6.902(3.726,12.786) |
4.483(1.823, 11.028)* |
| feeding |
Yes |
14(17.1) |
68(82.9) |
1 |
1 |
| Husband |
Yes |
174(56.1) |
136(43.9) |
4.222(2.010, 8.869) |
2.686(1.037, 6.953)* |
| support |
No |
10(23.3) |
33(76.7) |
1 |
1 |
Table 4 : Factors that affect EBF practice among mothers of infants age less than 6 months using bivariate and multivariate logistic regression analysis model, Hargeisa, Somaliland, 2023.
In the final multivariate analysis to see their significant association with exclusive breast feeding practice. After adjusting for potential confounders in multivariate logistic regression analysis; age of infant, maternal occupation, household income, breastfeeding counseling during ANC, and husband support of breastfeeding, colostrum feeding and prelactal feeding were remained significant in the final model.
Discussion
This study has attempted to assess the of exclusive breastfeeding practice and associated factors during the first six months of infant life among mother-infant at health facility in Hargeisa city, Somaliland. the prevalence of EBF was 58.5% , This finding was greater than that of a study conducted in Dabat district, northwest Ethiopia, whose prevalence of EBF was 30.7% [15]. It was also higher than the national level prevalence of 52% reported by Ethiopian Demographic and Health Survey (EDHS) in 2011 [16]. This difference could be the result of efforts and multisectoral collaborations that have been made by the Government of Ethiopia on child nutrition since 2013 [14], while the studies mentioned above used data collected before the implementation of these revised national nutrition programs. In addition, the national study included samples from the less developed and pastoral regions with less health service coverage, which might have resulted in less awareness about exclusive breastfeeding.
The main reasons mentioned by mothers for early discontinuation of exclusive breastfeeding were; mothers perception of breast milk only not sufficient for infant 41(37.3%), maternal illness 25 (22.7%), and infant become thirsty 15(13.6%) ,lack of time 6 (5.5%). These results are consistent with other studies done in Brazil [17], Dare salaam, South Africa [18], Tanzania [19].
The present study, women without employment reported feeding their infants other types of milk before six months of age more often compared to formally employed women. This finding disagrees from the results of other studies [20], which found that staying at home was a positive factor, i.e., favorable to successful breastfeeding. Thus, one might hypothesize that the women without employment are less informed and more susceptible to environmental influences. Those mothers, along with the primiparous mothers (possibly less experienced) are more prone to believe that feeding other (non-human) types of milk is necessary or that it does not interfere with EB. One study conducted with 48 puerperal women from Uberaba, Minas Gerais, found that 14.6%).
In this study household income was significantly associated with exclusive breastfeeding. Mothers earning less money per month (<$100 month) were 3.6 times more likely to practice exclusive breastfeeding than mothers whose average monthly household income was 200 dollar /month and above. This is in line with research findings in Cape Metropole [21] and Nigeria [22,23]. This might be mothers who earn less money have no any option to buy other food and give to the infant rather than feeding breast milk exclusively. In this study most mothers who earn less money per month were unemployed mothers those who have sufficient time to feed breast milk exclusively. But this result is not in conformity with findings in Bangladish [24].
REFERENCES
- Kliegman RM, Behrman RE, Jenson HB, Stanton BF (2007) Nelson Textbook of Pediatrics e-book. Elsevier Health Sciences.
Google Scholar
- UNICEF (2009) Tracking Progress on Child and Maternal Nutrition:A Survival and Development Priority. New York: UNICEF.
Google Scholar
- Federal Ministry of Health, Family Health Department of Ethiopia (2004) National Strategy on Infant and Young Child Feeding. Addis Ababa, Ethiopia.
Google Scholar
- Indian academy of pediatrics (2010) Infant and young child feeding guidelines. India:Indian acadamy of pediatrics.
Indexed at
- Ministry of human resource development department of women and child development government of India (2004) National guide line of infant and young child feeding. India.
Google Scholar
- Central Statistical Agency (2012) Ethiopia Demographic and Health Survey 2011 A.A, Ethiopia: ICF International, Calverton, Maryland, USA.
Google Scholar
- Iowa women, infant and child Program (2001) Breastfeeding Promotion and Support Guidelines for Healthy Full Term Infants. Iowa Department of Public Health.
Google Scholar
- Horwood LJ, Fergusson DM (1998) Breastfeeding and later cognitive and academic outcomes. Pediatrics 101.
Indexed at, Google Scholar, Crossref
- WHO (2003) Global strategy for infant and young child feeding. Geneva:WHO.
Indexed at, Google Scholar
- Ca X, Wardlaw T, Brown DW (2012) Global trends in exclusive breast feeding. International Breastfeeding Journal 7: 12.
Indexed at, Google Scholar, Crossref
- WHO (2009) Mortality and burden of disease attributable to selected major risks. Geneva: WHO.
Google Scholar
- WHO (2009) Infant and young child feeding Model Chapter for textbooks for medical students and allied health professionals. Geneva: WHO.
Indexed at, Google Scholar
- Lauer JA, Betrán AP, Barros AJ, de Onís M (2006) Deaths and years of life lost due to suboptimal breast-feeding among children in the developing world: a global ecological risk assessment. Public health nutrition 9: 673-85.
Indexed at, Google Scholar, Crossref
- Arifeen S, Black RE, Antelman G, Baqui A, Caulfield L, et al. (2001) Exclusive breastfeeding reduces acute respiratory infection and diarrhea deaths among infants in Dhaka slums. Pediatrics. 108: e67-e70.
Indexed at, Google Scholar, Crossref
- UNICEF (2010) A successful start in life: Improving breastfeeding in West and Central Africa. New York: UNICEF.
Google Scholar
- Ethiopian Federal Ministry of Health (2015) National Strategy for child survival. Addis Ababa, Ethiopia.
Indexed at, Google Scholar, Crossref
- Federal Ministry of Health (2010) Ethiopian Health Sector Development Programme IV:2010/2011- 2014/2015. Adddis Ababa,Ethiopia.
Google Scholar
- USAID (2008) MCH program description, overall MCH and health sector situation of Ethiopia. USAID,Ethiopia.
- Hafizan N, Telba Z, Sutan R (2014) Socio-demographic Factors associated with duration of exclusive breast feeding practice among mothers in East Malaysia. IOSR Journal of Nursing and Health Science (IOSR-JNHS) 31: 52-56.
Google Scholar
- Tan KL (2011) Factors associated with exclusive breastfeeding among infants under six months of age in peninsular Malaysia. Int Breastfeeding J 6: 2.
Indexed at, Google Scholar, Crossref
- Amin T, Hablas H, Al Qader AA (2010) Determinants of Initiation and Exclusivity of Breastfeeding in Al Hassa, Saudi Arabia. Breastfeed Med 6: 59-68
Indexed at, Google Scholar, Crossref
- Joshi PC, Angdembe MR, Das SK, Ahmed S, Faruque ASG, et al. (2014) Prevalence of exclusive breastfeeding and associated factors among mothers in rural Bangladesh: a cross- sectional study. Int Breastfeeding J 9: 7
Indexed at, Google Scholar, Crossref
- Khanal V, Cruz JLN, Karkee R, Lee AH (2014) Factors Associated with Exclusive Breastfeeding in Timor-Leste: Findings from Demographic and Health Survey 2009–2010. Nutrients 6.
Indexed at, Google Scholar, Crossref
- Saka FJ (2012) Factors influencing exclusive breastfeeding among HIV positive mothers at ilala municipality -Dar es Salaam.
Google Scholar
Citation: Muhumud MI (2024) Assessment of Exclusive Breastfeeding Practice and Associated Factors among Mothers in Hargeisa City, Somaliland 2023. Health Sci J. Vol. 18 No. 1: 1100.