Keywords
Unmet Obstetric Needs; MOI: Major Obstetric Intervention; AMI: Absolute Maternal Indication; non AMI: non-Absolute Maternal Indication
Background
The health of mothers and children is central to global and national concerns, and improvements in maternal and child survival are two important Millennium Development Goals. The fifth Millennium Development Goal (MDG) set for 2015 aims to improve maternal health through a reduction of the maternal mortality ratio (MMR) by three quarters [1].
In Ethiopia, the maternal mortality ratio is high with estimates 676 maternal deaths per 100,000 live births, the TFR is estimated to be 4.8 and CPR is 32%. The proportion of women attending ANC is 34% with wide variation in Rural (26%) and Urban (74%) respectively. Trained worker assists only 25% of the deliveries home births are almost twice as common in rural areas (95%) as in urban areas (50 %) [2].
Women die from a wide range of complications in pregnancy, childbirth or the postpartum period. Most of these complications develop because of their pregnant status and some because pregnancy aggravated an existing disease. The five major global causes of maternal death are: severe bleeding (mostly bleeding postpartum), infections (also mostly soon after delivery), unsafe induced abortion, hypertensive disorders in pregnancy (eclampsia) and obstructed labour. Globally, about 80% of maternal deaths are due to these causes. Hemorrhage alone accounts for one third of all maternal deaths in Africa, yet many of these deaths are preventable. Among the indirect causes 20% of maternal death are diseases that complicate pregnancy or are aggravated by pregnancy, such as malaria, anaemia and heart disease [3,4].
Most maternal deaths are avoidable if women have access to emergency obstetric care (EmOC). About 15 percent of all pregnant women have childbirth complications that require emergency obstetric care (EmOC), yet few are able to access such services [5]. Developing countries should therefore not expect maternal mortality to decline significantly without functioning and accessible EmOC. This calls for the need to provide information to decision makers on why women are dying, where and what can be done to improve equitable access to services that are critical to the survival of women [6]. The Unmet Obstetric Need (UON) concept takes this idea further by including all major obstetric interventions and then stratifying them according to indications.
One main focus for making pregnancy safer in Ethiopia is proper provision of EmOC through both development of infrastructure and ensuring optimum functionality. This study therefore attempts to identify deficits in MOI for AMI in comparison to the existing need. The information will also highlight where exactly to focus in planning interventions. Strategies to reduce Maternal Mortality in the country require such kind information for decision-making.
Methods and Material
Cross-sectional study design was conducted at Tarcha General Hospital is located south west of Addis Ababa 489km along the Jimma road, Ethiopia. Study population was all mother charts that have AMI and all mother charts who have received MOI in Tercha general Hospital from Apr 2012 to Apr 2014.
The information was gathered from hospital records. These were theatre registries, delivery books/ obstetric records and other relevant documents, by check list questionnaires using trained data collectors.
Data was collected on the socio-demographic variables, parity, maternal complications, perinatal outcome & the type cesarean section using pre-tested structured questionnaire.
The questionnaire was prepared in English. The instrument was adopted from different literatures developed for similar purpose by different authors and tools designed by various organizations.
Data were collected by eight trained data collectors for 15 days and supervised on the daily basis. After data collection was completed, the data were checked for errors, coded and entered to SPSS version 16.0 for windows for further analysis. Descriptive statistics were done using tables, and graphs. Thematic analysis was done for qualitative data and triangulated with quantitative findings. Bivariate analysis was computed for association between dependent and independent variables.
Ethical clearance was obtained from Research Ethics Committee of Jimma University. Letter of permission was obtained from Tarcha General Hospital Administrative office and respective departments of the Hospital. The information found in the patient chart was kept secured or confidential and the information was used only for this study purpose.
Results
During the two years study period, a total 302 major obstetric interventions (MOIs) conducted out of 1284 deliveries.
Socio-demographic characteristics of mother with MOI in TGH
The average age of the respondents was 25.7+6.1 while considering the address from patients charts, the distance from living area to the Hospital in KM was analyzed and 214 (70.9%) cases more than 10KM far from the Hospital and 88 (29.1%) cases within 10KM of radius from Hospital .The ethnicity of majority of mothers were Dawro 222 (73.5%) followed by wolyta 31 (10.3%), Amhara 18 (6.0%), Oromo 14 (4.6%), konta 11 (3.6%) and other 6 (2.0%). While, majority 293 (97%) are married and 9 (3%) unmarried (Table 1).
Table 1: Socio-demographic characteristic of mother with MOI in TGH from April 1, 2012-April 30, 2014.
| Maternal age in years |
Frequencies |
% |
| =<20 |
79 |
26,2 |
| 21-35 |
203 |
67.2 |
| >35 |
20 |
6.6 |
| Distance from hospital in KM |
|
|
| >10 KM |
234 |
82.1 |
| <10 KM |
68 |
17.9 |
| Marital Status |
|
|
| Married |
293 |
97 |
| Single |
9 |
3 |
| Place of Delivery |
|
|
| Tarcha hospital |
295 |
97.7 |
| home |
4 |
1.3 |
| Other institution |
3 |
1 |
Obstetrics profile
Among 302 patient with MOI, majority of mother were between Para I-IV 118 (39.1%) followed by primipara 97 (32.1%) and 87 (28.8%) above Para IV. Most 200(62.2%) of the mothers have history of ANC follow up at least once, 94 (31.1%) of patient hadn’t ANC follow up and 8 (2.6%) unknown. Many of the women 295 (97.7%) delivered in the institution, while 7 (2.7%) delivered at home. Among the mothers who had specific illness and risk at the present pregnancy 156 (55.3%), majority had anemia 95 (60.8%) followed by malaria 24 (15.4%), HIV7 (4.5%) Preeclampsia 9 (5.7%) and multiple pregnancy 7(4.5%) (Table 2).
Table 2: Obstetrics profile of MOIs in TGH from April 2012-April 2014.
| Parity |
Frequency |
Percent |
| primi |
115 |
39.1 |
| para2-4 |
125 |
41.4 |
| para>=4 |
59 |
19.5 |
| ANC follow up |
|
|
| YES |
200 |
66.2 |
| NO |
94 |
31.1 |
| Missing |
8 |
2.6 |
| Present OB.Hx |
|
|
| Anemia |
95 |
60.8 |
| PROM |
24 |
15.4 |
| malaria |
13 |
8.3 |
| preeclampsia |
9 |
5.7 |
| HIV |
7 |
4.5 |
| Multiple gestation |
7 |
4.5 |
| Total |
156 |
51.7 |
Distribution of major obstetric Intervention’s in tarcha general hospital
The presented analysis for comparability reasons partly follows the scheme given by the UON-network. The UON-network aims at putting light at the rural/urban difference of the interventions and their respective indication.
The predominant MOI was a CS 245 (81%) followed by laparotomy for repair of uterus 25(8.3%). Hysterectomy counted for 20 (6.6%) of all MOIs and a destructive delivery was performed in 12(4%) of the cases. Caesarean sections were performed more often in urban areas 81 (92%) and in rural areas 164 (76.6%). These differences were statistically significant (p <0.002). The crude CSrate, regardless of indication was 0.6% per expected birth in the study area.
There were also differences in the percentage of laparotomies for repair of ruptured uterus and hysterectomies done in urban and rural areas. In urban areas the proportion of laparotomy for repair of uterus was 3.4% and for hysterectomy 2.3% whereas in rural areas laparotomy for repair of uterus accounted for 10.3% of all interventions and hysterectomy for 8.4%. The urban/rural differences were statistically significant for laparotomy for repair of uterus (p=0.049) and for hysterectomy (p=0.051) (Table 3).
Table 3: Distribution of Major Obstetric Intervention according to place, TGH from April 2012-April 2014.
| MOI |
|
Urban Area |
Rural Area |
|
|
Total |
p-value |
| |
N |
% |
N |
% |
N |
% |
|
| CS |
81 |
92 |
164 |
76.6 |
245 |
81.1 |
0.002 |
| Lap. For repair of Uterus |
3 |
3.4 |
22 |
10.3 |
25 |
8.3 |
0.049 |
| Hysterectomy |
2 |
2.3 |
18 |
8.4 |
20 |
6.6 |
0.051 |
| Destructive Operation |
2 |
2.3 |
10 |
4.7 |
12 |
4 |
0.332 |
| Total |
82 |
100 |
220 |
100 |
302 |
100 |
|
Distribution of indications for major obstetric interventions
The number of women with AMI was 238 where majority of them were cephalo-pelvic disproportion (CPD) 91(38.2%) followed by malpresentation 69 (29%), uterine rupture 40 (16.8%) and major placenta previa 22(9.2%) and failed induction 12 (5%). The number of MOI done without AMI was 64 (21.2%) where majority were done for foetal distress 42 (65.6% and previous c/s scar 11 (17.2%). The predominant Absolute Maternal Indication was CPD 91 (38.2%). The indication rupture of uterus was 3.73 times more common for mothers from rural areas. The difference was statistically significant (p=0.005). For two or more previous CS the opposite was found which implies indication was 2.6 times more often listed when the mother came from urban areas. Also, malpresentation was mentioned slightly more often for urban mothers, but the difference was not significant.
Uterus rupture was the main indication in 40 (13.2%) of all MOIs mothers. There was a major difference between the urban and rural group of women. This indication was reported in only 4.5% of the total MOIs for urban mothers compared to 16.8% for rural mothers. The difference was statistically significant (p=0.005). Very few MOIs only 5 (1.7%) were done because of postpartum hemorrhage (PPH).
Ante partum hemorrhage (APH) was the indication for 22 (7.3%) of all MOIs. The distribution of MOIs for APH among the urban 5 (5.7%) and rural 17 (7.9%) but the difference was not statistically significant.
The number of MOI done without AMI was 64 (21.2%) where majority were done for Fetal distress which accounts 42 (13.9%) of all indications and 65.6% non-AMIs. This indication was significantly higher among urban mothers 26.1% and rural mothers 8.9% and difference was statistically significant (p<0.001). Also, failed induction was mentioned slightly more often for urban mothers, but the difference was not significant.
Others were mentioned as Non-AMI (3.3% of all interventions) there was no significant difference with address. The most often given reason were the Hypertensive disorders 2 cases, breech presentation 4 cases, cord prolapse 2 cases and bad obstetric history 2 cases (Table 4).
Table 4: Distribution of indications in urban and rural area, TGH from April 2012-April 2014 .
| Absolute Maternal Indications (AMIs) |
Urban Area |
Rural Area |
Total |
p-value |
| |
N |
% |
N |
% |
N |
% |
|
| CPD |
16 |
18.2 |
75 |
35 |
91 |
30.1 |
0.004 |
| Malpresentation |
21 |
23.9 |
48 |
22.4 |
69 |
22.8 |
0.877 |
| Uterine rupture |
4 |
4.5 |
36 |
16.8 |
40 |
13.2 |
0.005 |
| APH |
5 |
5.7 |
17 |
7.9 |
22 |
7.3 |
0.629 |
| 2 or more CS |
8 |
9.1 |
3 |
1.4 |
11 |
3.6 |
0.004 |
| PPH |
1 |
1.1 |
4 |
1.9 |
5 |
1.7 |
1 |
| Total |
55 |
62.5 |
183 |
85.4 |
238 |
78.7 |
|
| Non-Absolute Maternal Indications (Non-AMIs) |
|
|
|
|
| Fetal distress |
23 |
26.1 |
19 |
8.9 |
42 |
13.9 |
0 |
| Failed induction |
6 |
6.8 |
6 |
2.8 |
12 |
4 |
0.111 |
| Other |
4 |
4.5 |
6 |
2.8 |
10 |
3.3 |
0.478 |
| Total |
33 |
37.4 |
31 |
14.5 |
64 |
22.2 |
|
Perinatal outcome
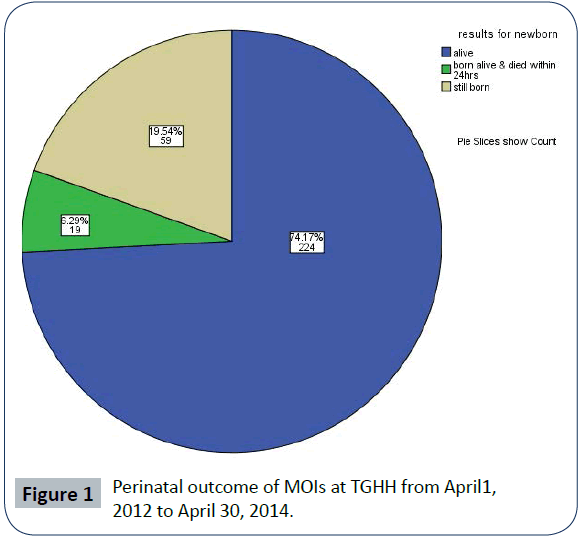
Out of the 302 reported deliveries resulting in a MOI regardless of the indication, 224 (74.2%) babies were born and discharged alive, 59 (19.5%) of the babies were still born. While 19 (6.3%) were born alive but died within 24 hours of delivery. The overall perinatal mortality in the group of mothers having undergone a MOI during the study period was 258 per 1000 live births (Figure 1).
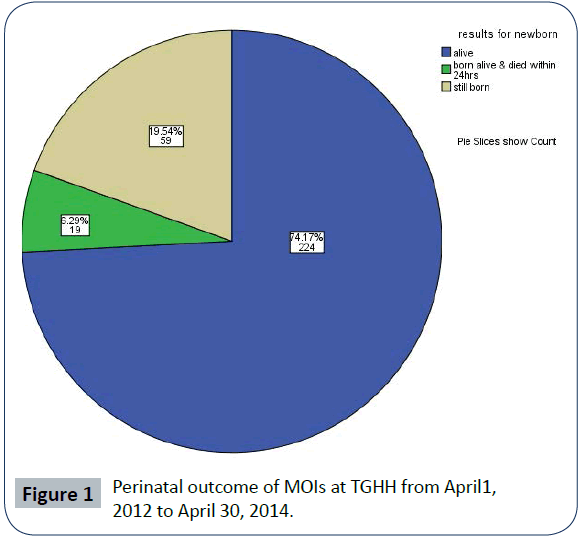
Figure 1: Perinatal outcome of MOIs at TGHH from April1, 2012 to April 30, 2014.
Maternal Outcome
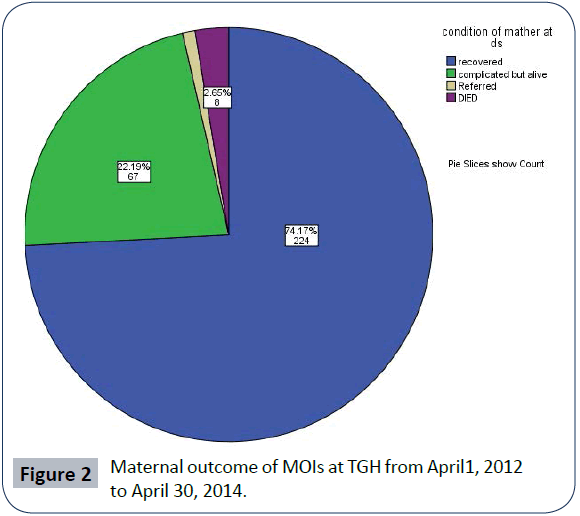
Regarding the maternal outcome of the 302 reported MOI 238 (74.2%) survived the intervention with no adverse effects, 67 (22.2%) women developed a complication such as hemorrhage 29, sepsis 20, wound site infection 12, anesthetic complication 6. And severe postoperative malaria 7, obstetric fistula 3 whereas 8 (2.6%) women died but three woman was referred, but it was not possible to follow up the outcome.
The case fatality rate in relation to a MOI was 2.65%.The causes incriminated were sepsis 5 (62.5%) and haemorrhage 3 (37.5%). There was differences distribution of maternal deaths after a MOI in relation to the indication and rural/urban. 2.3% (7 out of 302) of mother from rural areas died after a MOI but only 0.3% (1 out of 302) of mothers from urban areas.
A hysterectomy for a ruptured uterus had the highest case fatality rate for the mother4cases out 8 followed by laparotomy for a ruptured uterus 3cases out of 8.only 1 cases died after CS for APH (Figure 2).
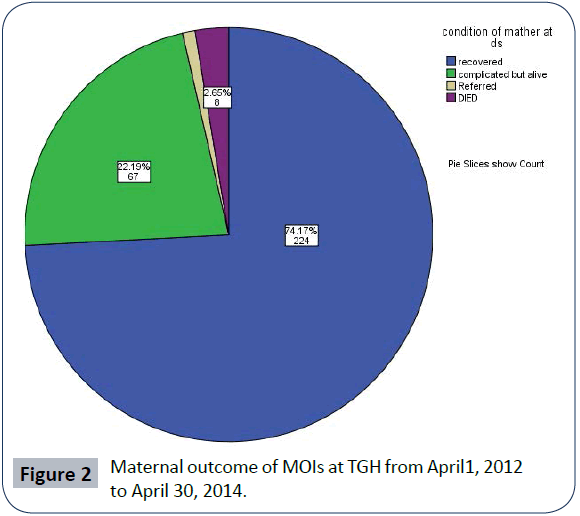
Figure 2: Maternal outcome of MOIs at TGH from April1, 2012 to April 30, 2014.
Binary logistic analysis was done to show the association between perinatal and maternal outcome and other independent variables. Distance from hospital have significant statistical association with perinatal outcome (p>0.046). Also, ANC follow up have significant statistical association with perinatal outcome (p=0.008). Mothers whose have ANC follow up have 22.3% less likely chance to have fetal loss when compared with mothers no history of ANC follow up (Table 4).
Moreover, the association between the maternal outcome and independent variables were assessed, the results revealed that there was significant statistical association between maternal outcome and distance from hospital (p-value=0.002). The mother who come from urban have 27.2% less likely chance to develop complications than those mother who come from rural area (COR0.272, 95%CI 0.121-0.609). There was also highly significant statistical association in maternal outcome and ANC follow up (p-value<0.001) Mothers who have not attended ANC follow up have 3 times chance to develop complications than mothers who attended ANC follow up. (COR 3.064, 95%CI; 1.720-5.458) (Table 5).
Table 5: Binary logistic analyses for selected variables and fetal and maternal outcome, TGH from April 2012-April 2014.
| |
Perinatal outcome |
COR (95%CI) |
p-value |
| Alive (per 100) |
Dead (per 100) |
| Maternal Age |
| <=20 |
71(89.9) |
8(10.1) |
0.44 (0.09,2.27) |
0.329 |
| 21-35 |
143(70.4) |
60(29.6) |
0.89(0.31,2.52) |
0.826 |
| >35 |
10(50) |
10(50) |
1 |
|
| Distance from hospital in km |
| >10km |
148(69.2) |
66(30.8) |
2.07(1.00,4.26) |
0.049, 4.26 |
| <10km |
76(86.4) |
12(13.6) |
1 |
|
| Parity |
|
|
|
|
| Primipara(para 1) |
86(88.7) |
11(11.3) |
0.28( 0.09,0.93) |
0.038 |
| Multi para (para 2-4) |
93(78.8) |
25(21.2) |
0.40(0.21,0.79) |
0.009 |
| Grand multi para(>= para5) |
45(51.7) |
42(48.3) |
|
|
| ANC follow up |
| Attended |
162(81) |
38(19) |
0.44(0.24,0.80) |
0.007 |
| Not attended |
58(61.7) |
36(38.3) |
1 |
|
| |
Recovered |
Complicated |
|
|
| |
(per100) |
(per100) |
|
|
| Maternal Age |
| <=20 |
64(81) |
15(19) |
|
0.07 |
| |
|
|
0.24(0.05,1.12) |
|
| 21-35 |
150(73.9) |
53(26.1) |
0.54(0.18,1.58) |
0.261 |
| >35 |
10(50) |
10(50) |
1 |
|
| Distance from hospital in km |
| >10km |
144(67.3) |
70(32.7) |
|
|
| |
|
|
3.50(1.55,7.91) |
0.003 |
| <10km |
80(90.9) |
8(9.1) |
1 |
|
| Parity |
| Primi(para 1) |
76(78.4) |
21(21.6) |
1.17(0.39,3.43) |
0.779 |
| Multipara(para2-4) |
96(81.4) |
22(18.6) |
0.59(0.28,1.22) |
0.152 |
| Grand multi para(>= para5) |
52(59.8) |
35(40.2) |
1 |
|
| ANC follow up |
| Attended |
166(83) |
34(17) |
0.32(0.18,0.58) |
0.001 |
| Not attended |
54(57.4) |
40(42.6) |
1 |
|
The Unmet Obstetric Need-indicator
To calculate the unmet obstetric need all MOIs done for AMIs were taken in consideration. A total of 238 MOIs for AMI were carried out during the study period.
Quantification of UON
The indicator of unmet need for major obstetric interventions for a given population in a
Given period is calculated as follows:
Unmet obstetric need = (BE x RR) – (number of MOI/AMI),
BE = number of births expected in the period under study,
RR = reference ratio of MOI for AMI, and number of MOI/AMI = number of major obstetric interventions for absolute maternal indications carried out in the same population during the same period
EB =40114 (Expected birth; this is taken from the estimate for Dawro zone obtained from health indicator of Ethiopia 2011EC to be 20057 for two years assuming no seasonality it will be 40114), rural EB=34098,urban EB=6016.
The RR (reference ratio) is estimated to be 1.4% (95%CI, 1.27– 1.52) (benchmark the median for five sub-Saharan African countries, Haiti, Morocco and Pakistan (https://www.uonn.org/ uonn/pdf/engintc00.pdf).)
MOI/AMI= 238 (Major Obstetric Intervention actually performed for Absolute Maternal Indication in the same population in the same period).
The UON is therefore 40114*1.4% -238 =323cases or 57.6% relative Need %
For urban 6016*1.4%-55=29cases or 34.5% relative Need %
For rural 34098*1.4%-183=294cases or 61.6% relative Need % Nearly 323 births which needed major obstetric intervention in study area during the period of data collection (April2012-April, 2014) did not receive it
This analysis follows the schema proposed by the UON-network that tries to consider rural/urban differences in the study areas. The table 5 shows substantial differences in the reached number of MOIs per AMIs between urban (0.9%) and rural areas (0.5%) but in overall no urban or rural areas achieved a minimum requirement of 2% expected MOIs for AMIs as a cut-off value.
There is a considerable discrepancy when the expected and actual MOI for AMI are compared to whether the woman comes from an area classified as rural or urban. The low level of MOI for AMI (0.5%) amongst the rural population points to major unmet obstetric need there (Table 6).
Table 6: Comparison between Actual MOI for AMI in relation to Residence, TGH from April 2012-April 2014GC.
| |
Exp. Birth (EB) 2 years |
Estimated Needs for MOIs/AMIs (1.4% of EB) |
Met Need (Actual MOIs/ AMIs) |
Unmet Need (Deficit in absolute figure) |
Actual % MOIs/ AMIs for EB |
Unmet Need (Relative Need %) |
| Urban (<10km) |
6016 |
84 |
55 |
29 |
0.9 |
34.5 |
| Rural(>10km) |
34098 |
477 |
183 |
294 |
0.5 |
61.6 |
| Total |
40114 |
561 |
238 |
323 |
0.8 |
57.6 |
Discussion
This study was carried out to estimate the unmet obstetric need and possible maternal and perinatal outcome of major obstetric interventions in Tarcha General Hospital, south-west Ethiopia.
The result shows that there was the major unmet obstetric need in Dawro zone, 297cases (58%) of mother with life threatening obstetric complications(AMIs) was not get intervention and this was interpreted as the number of women who should have benefited from a lifesaving intervention but actually did not, meaning that they probably died or suffered very severe complications. The findings show an overall of major obstetric interventions for AMI rate of 0.8% which is below a minimum requirement UN range of 1% up to 2% expected MOIs for AMIs of UON-indictor. This study is similar with other UON studies in sub-Saharan Africa [3,7].
There is an important gap regarding the availability of services when urban and rural areas are compared. In the group of women living in areas classified as urban, and thus residing within 10 km of the hospital, the 55 MOIs for AMIs represent 0.9% of all deliveries and 183 MOIs for AMIs in rural women represent only 0.5% of all deliveries. While in Benin, Burkina Faso, Mali and Niger ranged from 1.4 to 0.8 in urban areas and 0.9 to 0.15 in rural areas [6,8].
Among the MOI conducted Caesarean section took the largest share (81.5%) of MOIs and 19% of all institution deliveries. Caesarean sections were performed more often in urban areas 81 (92%) and in rural areas 164 (76.6%). These differences were statistically significant (p <0.002). The most common intervention in all the studies published by the UON-network is CS. The crude CS-rate, regardless of indication was 0.6% per expected birth in the whole of DAWRO Zone during the study period is below the UN range of 5% to 15%. Using the UN guidelines as reference caesarean sections were far below what is regarded as adequate in order to reduce maternal deaths. These result is agree with earlier research conducted in rural, Ethiopia, as well as in other developing countries [9,10]. The possible reasons for these findings could be because people live far away from adequately functioning institutions or because of social and cultural restrictions for women to use health institutions during deliveries
The second most often intervention carried out is laparotomy for ruptured uterus 25 cases (8.3%) of all MOIs. This intervention accounted for between 0.8% (Pakistan) and 14.8% (Burkina Faso) of all MOIs (UON-network, 2004a).
The commonest AMI in this study was Obstructed Labor accounting for 39.5% which is one of the five commonest causes of maternal death in the world [7,11]. Nearly half of the MOI were done for non AMI mainly for Previous C/S and foetal distress. The UON study done in Burkina also showed foetal distress to be the commonest non-AMI [7,8,11,12].
The study in TGH showed a perinatal mortality in relation to a MOI of 258 per 1000 births and a stillbirth-rate of 195 per 1000births and early neonatal death 63 per 1000 births. The main obstetrical risk factors were ruptured uterus, APH, CPD and malpresentations. Stillbirth and early neonatal mortality have also been assessed in other UON-studies. The overall stillbirth rate in relation to a MOI was between 30 per 1000 (in Pakistan) and 240 per 1000 births (in Benin). The early perinatal mortality in relation to a MOI ranged from 30 per 1000 births (in Pakistan) to 410 per 1000 (in Benin) [7,8,12]. In this study there was 2 times higher for rural than for urban mothers.
The mothers that suffered from complication after delivery accounted for 25.8%% whereby majority of the causes were sepsis and hemorrhage. The case fatality rate was 2.65% which was higher than the upper limit set by the UN i.e. 1%.This is comparable with ratios found in other hospital studies in Tanzania [13,14].
There was differences distribution of maternal deaths after a MOI in relation to the indication and rural/urban. 2.3% (7 out of 302) of mother from rural areas died after a MOI but only 0.3% (1 out of 302) of mothers from urban areas. In our study higher maternal mortality was found for interventions done for relation to uterine ruptur7out of 8 and only one for APH. This trend has also been described in other UON-studies: uterus rupture is a major reason of hospital deaths in mothers coming from rural areas whereas hemorrhages, APH, PPH are predominant in urban mothers [7,8,14].
Conclusion and Recommendation
Based on the 2% threshold, with an overall level of major obstetric interventions for absolute maternal indications of 0.8% and a caesarean section rate of 0.6% and high proportion of negative maternal and perinatal outcomes has significant unmet obstetric need with a considerable rural-urban disparity. The low level of MOI for AMI (0.5%) amongst the rural population points to major unmet obstetric need. The UON-indicator showed to be useful to monitor access to emergency obstetric care and perinatal and maternal mortality using data available through the routine hospital information system.
Therefore, estimating the amount of 'unmet need for major obstetric interventions' provide the information necessary for planning and prioritizing the development of services; and lead to action for the reduction of maternal mortality at local level by changing certain attitudes, mobilizing resources and more effectively adapting professional practices to the needs of patients.
Improvement in the health care system can lead to decline in the rate of morbidity and mortality. This requires a multidisciplinary approach including refresher training for health professionals, upgrading of peripheral health services with transportation facilities and posting of skilled professionals in rural area.
Competing of Interests
We declare that we have no competing of interests
Authors' contributions
All authors carried out the study and participated in the statistical analysis and design of the study and the drafting of the manuscript. All authors read and approved the final version.
Acknowledgements
We wish to thank Jimma University for funding the study and Tarch General Hospital administrative bodies where the study was conducted for permitting us to use data. Data clerks for accessing the database in those hospitals. Regional laboratory staffs and other health professionals for their cooperation during the interview.
7903
References
- Campbell OM, Graham WJ, Lancet Maternal Survival Series steering group (2006) Strategies for reducing maternal mortality: getting on with what works. Lancet 368: 1284-1299.
- CSA-Ethiopia, ICF-International: Ethiopia Demographic and Health Survey 2011. (2012) Maryland, USA: Central Statistical Agency of Ethiopia and ICF International Addis Ababa, Ethiopia and Calverton.
- Ababa A (2010) Federal democratic republic of Ethiopia, ministry of health. Basic emergency obstetric & newborn care (BEMONC) training manual Ministry of health, (1stedn) Ethiopia.
- Maternal Mortality in 2000: Estimates developed by WHO, UNICEF, UNFPA. Geneva (2004) WHO, UNICEF, UNFPA.
- Field-friendly Guide to Integrate in Humanitarian Programs (2005)Emergency Obstetric Care, New York.
- Belghiti A, De Brouwere V, Kegels G, Van Lerberghe W (1998) Monitoring unmet obstetric need at district level in Morocco. Trop Med Int Health 3: 584-591.
- Tackling unmet need for major obstetric interventions: Part1. Concepts, general principles and international network (2011) Antwerp: UON Network.
- Alihonou E (2004)With support from Swiss Health Programme and in partnership with GTZ, UNICEF, PADS and USAID, Tackling Unmet Obstetric Needs: Benin Tackling Unmet Needs for Major Obstetric Interventions.
- Meseret G, Yaliso Y,Gebrehanna E, Berhane Y, Lindtjørn B (2013) Lifesaving emergency obstetric services: a formidable challenge to reducing maternal mortality in Ethiopia. Ethiop J Health Dev13:459
- FIGO, ESOG. (2003) Reasons for underutilization of emergency obstetric services in three woredas of west Shoa zone, Oromia Region, Ethiopia: A qualitative approach.3: 23.
- WHO, UNICEF, UNFPA, AMDD (2009) Monitoring Emergency Obstetric Care, a handbook. WHO publications, Geneva, Switzerland: World Health Organization.
- UNICEF, World Health Organization, UNFPA(1997) Guidelines for monitoring the availability and use of obstetric services. New York: UNICEF
- AMDD working group on indicators (2003) Averting maternal death and disability. Program note, Using UN process indicators to assess needs in emergency obstetric services: Niger, Rwanda and Tanzania.
- Elizabeth E (2009) Assessing coverage in emergency obstetric care services and unmet needs in Malindi District, Kenya.
- Paxton A, Maine D, Freedman L, Fry D, Lobis S (2005) The evidence for emergency obstetric care. Int J GynaecolObstet 88: 181-193
- Victoria R., Charlotte W., Yared A (2006) Final report on the safe motherhood community based survey. Addis Ababa: FHD, MOH.
- FDRE MOH Family Health Department(2002) Facility based rapid needs assessment for making pregnancy safer initiative. Implementation at four pilot regions in Ethiopia. 1-5
- Prytherch H, Massawe S, Kuelker R, Hunger C, Mtatifikolo F, et al. (2007) The unmet need for emergency obstetric care in Tanga Region, Tanzania. BMC Pregnancy Childbirth 7: 16.
- Nigussie M, Hailemariam D, Mitike G (2004) Assessment of safe delivery service utilization among women of childbearing age in north Gondar Zone, northwest Ethiopia. EthiopJ Health Dev 18: 146-151.
- HIMS department of Tarcha General Hospital 2005 annual report. (Unpublished)
- Berhan Y, Abdela A (2004) Emergency Obstetric care Performance with emphasis on operative delivery outcome. Ethiop J Health Dev 18: 96-106
- AbouZahr C (2001) Cautious champions: international agency efforts to get Safe Motherhood onto the agenda. Studies in HSO&P 17: 387-414.
- Islam M, Yoshida S (2009) Women are still deprived of access to lifesaving essential and emergency obstetric care. Int J GynaecolObstet 106: 120-124.