Research - (2022) Volume 16, Issue 11
Ayushman Bharat Mission: Protect the Health of
Families in Uttar Pradesh, India
Kapil Kaushik*
Department of Health and Science, India
*Correspondence:
Kapil Kaushik, Department of Health and Science,
India,
Tel: 09457043048,
Email:
Received: 27-Sep-2022, Manuscript No. Iphsj-22-13095;
Editor assigned: 30-Sep-2022, Pre QC No. Iphsj-22-13095 (PQ);
Reviewed: 28-Oct-2022, QC No. Iphsj-22-13095;
Revised: 02-Nov-2022, Manuscript No. Iphsj-22-13095(R);
Published:
09-Nov-2022, DOI: 10.36648/1791- 809X.16.11.984
Abstract
Along with food, shelter, education and health is a basic need and a requirement for growth and productivity. Health services have a significant role in a country's politics and economy and have a significant impact on the health of individuals and societies. Economic growth and the reduction of inequality are two benefits of health interventions in developing nations. Objectives of the study to identify the disparity in allocation of hospitals as well as medical care units under Ayushman Bharat Mission- Pradhan Mantri Jan Arogya Yojan (PMJAY) in the districts of Uttar Pradesh. Analytical approach is used to present the secondary data obtain from various government agencies. Data presented with suitable statistical techniques and figures. Study reveals that hospitals are not allocated with same ratio to all districts. Total medical and surgical facilities are not available in all districts. There is polarization of medical facilities only in lager districts. In small districts proper medical and surgical facilities are not available. Results indicated that there is need of increase in the numbers of empanelled hospitals under PMJAY in all districts. Numbers of empanelled government hospitals are high in small districts and treatment facilities to patients are low. On the other hand empanelled hospitals private for profit and not for profit are high in large districts. In this scheme focus should be given to increase the medical facilities for improving the health and minimizing the out of pockets expenditures of rural as well as urban population.
Keywords
Universal Health Coverage; Medical cares; Surgical Facilities; Empanelled Hospitals; Beneficiary Families
INTRODUCTION
Population health is widely regarded as a key indicator of development, and health is increasingly viewed as a development issue rather than merely a medical one (Sachs & Weltgesundheitsorganisation, 2001; Sharma, 2018). Many people in India do not have access to healthcare facilities at all, and most of those who do have access to healthcare facilities are under enormous financial pressure to pay for medical care. In this context, supportive role of government in providing universal health coverage (UHC), so that people do not fall into medical poverty is very important [1-5].
Universal Health Coverage (UHC) is defined by the World Health Organization as all individuals and communities having access to adequate and effective quality health promotion, prevention, treatment, rehabilitation, and palliative care services, while ensuring that services are used despite financial constraints. It embodies three goals: fair access, quality and financial risk prevention. The UHC movement gained momentum after it was listed as one of the goals of the United Nations Sustainable Development Goal 3 (SDG-3) in 2015. Many low- and middleincome countries have specific plans, mainly different types of health financing and insurance systems, to achieve universal health coverage (Sustainable Development Goals, n.d.).
In September 2018 India launched an ambitious health plan known as the National Health Protection Plan better known as Ayushman Bharat mission popularly knows Pradhan Mantri Jan Arogya Yojan (PMJAY), is expected to be widespread in India and moving towards UHC would be a step forward [6]. According to the 2011 Socioeconomic and Caste Census Database (Ayushman Bharat for a New India -2022, Announced, nd.), it aims to cover about 40% of India's population divided into rural and urban areas. Ayushman Bharat's stated goal is to provide quality healthcare without putting anyone in financial distress. The plan envisages reducing out-of-pocket expenses (OOPE) and catastrophic health care expenditures through private sector engagement, while building on the existing network of public hospitals [7]. It enables beneficiaries to obtain unrestricted services from public or privately associated hospitals [8].
As part of the Pradhan Mantri Jan Arogya Yojan initiative, the following steps are taken by government:-
(i) Health and Wellness Centers: - National Health Policy, 2017 has focused on the Health and Wellness Centers as the base of the health system in India. Under this about 1.5 lakh centers will be open to provide health care facilities to families closer to their homes. These centers provide comprehensive health services, including maternal and child health services and non-communicable diseases. These centers will also offer free prescription medications and diagnostic services. (How Equitable Will Ayushman Bharat Be? | Economic and Political Weekly, n.d.). Contribution of the private sector through corporate social responsibility (CSR) and nongovernment entities (charitable organisations) are also planned to adopting these centers (Ayushman Bharat - National Health Protection Mission | National Portal of India, n.d.).
(ii) National Health Protection Scheme (NHPS):- The second flagship programme under Ayushman Bharat is NHPS, which will cover over 100 million socio-economically backward families (approximately 500 million persons) providing coverage of rupees 5 lakhs to each family per year for secondary and tertiary care hospitalization (Angell et al., 2019). This is considered as the world’s largest government funded health insurance scheme. Appropriate funds will be available to ensure the smooth operation of this program (Choudhury & Datta 2019; Kaur et al., n.d.).
Implementation Strategy
At the national level, Ayushman Bharat Mission-Pradhan Mantri Jan Arogya Yojan (PMJAY) would be established to monitor and manage this health system. (Reddy et al., 2011). A dedicated institution named the State Health Agency (SHA) would advise states/UTs on how to implement the system. States/ UTs can either use an existing Trust/ Society/ Not for Profit Company/ State Nodal Agency (SNA) or set up a new entity to implement the scheme [9].
Various states use various systems to implement their own health insurance programmes. Some states use private insurance companies to implement their health insurance programmes, while others administer them directly. For implementation of Ayushman Bharat scheme states are free to choose either their own health insurance model or PMJAY. Because it is noted that states are at different levels of development and have varying capacity to manage such schemes. There are three ways through which states can implement the scheme; (i) through assurance/ trust model, (ii) insurance model or (iii) mixed mode. (Annual Report 2018-19 | Official Website Ayushman Bharat Pradhan Mantri Jan Arogya Yojana | National Health Authority, n.d. [10].
The medical insurance under Pradhan Mantri Jan Arogya Yojan incorporates hospitalization expenses of beneficiaries and also incorporates elements likes health checkups, advice and treatment; services before hospitalization; non-intensive care and critical care services; medicine and medical consumables; diagnosis and inspection services; accommodation; medical implant service as much as possible; diet expenses; complications that occur during treatment; up to 15 days follow-up treatment costs and treatment of Coronavirus.
Eligibility Criteria for Rural and Urban Household under Pradhan Mantri Jan Arogya Yojan
Ayushman Bharat Mission-Pradhan Mantri Jan Arogya Yojan was launched to help the country's bottom 40 percent of poor and economically vulnerable households. This scheme is based on the deprivation and occupational criteria of the Socio-Economic Caste Census 2011 for rural and urban areas. The Ayushman Bharat Mission eligibility is designed with pre-conditions, so that only socio-economically backward people of the country benefit from the initiative [10].
Socio-Economic Caste Census 2011 (SECC 2011) presented the ranking of rural households based on their socio-economic condition. All the rural households are ranked on bases of six deprivation criteria [11]. The scheme covers all beneficiaries who were noted at least one of the six deprivation categories. The categories are: Households having single/one room with Kucha walls and roof, No adult family member in the age group 16-59 years, No adult family male member in the age group 16- 59 years, Disabled member and no-abled bodied member in the household, Scheduled Caste and Scheduled Tribes and Landless households and major sources of income are through manual casual labour.
In this Scheme, urban families are divided in various groups on the bases of occupation. The 11 major groups of workers who are eligible for the Pradhan Mantri Jan Arogya Yojan are: Beggar, Domestic helpers, Worker related to collection and sells of rags, Cobbler/Street Vendor/Hawker/Other street service providers, Plumber/Constructor/ Brickman/Painter/Worker/ Welder/Security Guard/Coolie, Sweeper/Gardener/Sanitation Worker, Artisan/Handicrafts Worker/Tailor/Home-based Worker, Driver/Transport Worker/Conductor/Cart or Rickshaw Pullers/ Driver or Conductor's assistant, Workers in shops/ Peon in Small enterprises/Assistant/workers/Attendant/Delivery Agents/ Waiter, Assembler/Mechanic/Electrician/Repair Worker and Watchman/Washer-man [12].
Methodology
This study is entirely based on secondary data sources. The data is drawn from the Ayushman Bharat Pradhan Mantri Jan Arogya Yojan, Uttar Pradesh on September 2020. Beside this data is also used from socio-economic survey-2011. Raw data are converted into percentage as well as in ratio. For better outcome of results correlation technique is also used. The result of correlation is tested at coefficient level at 1 and 5. To represent the data graphs and maps are used. The purpose of this study is to identify the distribution and disparity in allocation of hospitals in districts of Uttar Pradesh. This study also examines the availability of secondary and tertiary care medical as well as surgical facilities in the empanelled hospitals in the districts of state. At the last correlation analysis were carried out between dependent (various types of hospitals) and independent (socio-economic indicators) variables [13].
Situation of Ayushman Bharat Mission in Uttar Pradesh
Uttar Pradesh is the largest state in terms of population (199.8 million, census 2011) in India. Uttar Pradesh (UP) has high rural population (77.73 percent, census 2011). Due to which large percentage of workforce is engaged in agricultural activities. Literacy rate is also low in Uttar Pradesh (67.68 percent, census 2011) as compare to India (72.98 percent) in 2011 (Jahan, n.d.). There is also the unfortunate distinction that the poverty rate is above average and 39.8 percent of the population lives below the poverty line (General Reports: Planning Commission, Government of India, n.d.). In addition, it has the highest illness burden in the country, significantly increasing the demand for affordable health care in the state (Statistics Ministry of Health and Family Welfare | GOI, n.d.). The low availability of public health services, especially in the most needed pockets, explains the high reliance on private providers to meet the health needs of the sick in the state [14].
Discussion
The analysis of data shows that there are 2546 hospitals enrolled under PMJAY in three categories in Uttar Pradesh. The types of hospitals are public hospital (1032 hospitals), private for profit hospitals (1220 hospital) and Private not for profit (294 hospitals).
The highest share fall under private for profit hospital with 47.92 percent, it is followed by public hospitals i.e. 40.53 percent and private not for profit has only 11.55 percent (Table 1).
| S.No. |
District |
Total Hospitals |
Public Hospitals |
Private Hospitals (Not For Profit) |
Private Hospitals (For Profit) |
hospital/Beneficiaries Families |
% of Golden card families v/s total beneficiaries (families) |
| 1 |
Agra |
71 |
30.98 (22) |
4.23 (3) |
64.79 (46) |
1305 |
20.60 |
| 2 |
Aligarh |
53 |
32.08 (17) |
9.43 (5) |
58.49 (31) |
2276 |
19.30 |
| 3 |
Allahabad |
179 |
15.64 (28) |
19.55 (35) |
64.81 (116) |
1243 |
32.40 |
| 4 |
Ambedkar Nagar |
13 |
84.62 (11) |
0.00 (0) |
15.38 (2) |
12373 |
38.10 |
| 5 |
Amethi |
15 |
86.67 (13) |
13.33 (2) |
0.00 (0) |
7328 |
37.30 |
| 6 |
Amroha |
19 |
36.84 (7) |
15.79 (3) |
47.37 (9) |
2340 |
31.10 |
| 7 |
Auraiya |
11 |
81.82 (9) |
0.00 (0) |
18.18 (2) |
7099 |
32.60 |
| 8 |
Azamgarh |
42 |
59.52 (25) |
4.76 (2) |
35.72 (15) |
2652 |
32.00 |
| 9 |
Baghpat |
15 |
46.67 (7) |
13.33 (2) |
40.00 (6) |
3873 |
42.50 |
| 10 |
Bahraich |
21 |
76.19 (16) |
4.76 (1) |
19.05 (4) |
7956 |
28.40 |
| 11 |
Ballia |
24 |
50.00 (12) |
16.67 (4) |
33.33 (8) |
5436 |
25.70 |
| 12 |
Balrampur |
22 |
54.55 (12) |
45.45 (10) |
0.00 (0) |
3633 |
26.80 |
| 13 |
Banda |
12 |
83.33 (10) |
0.00 (0) |
16.67 (2) |
5979 |
21.60 |
| 14 |
Barabanki |
34 |
61.76 (21) |
11.76 (4) |
26.48 (9) |
6752 |
37.30 |
| 15 |
Bareilly |
109 |
18.35 (20) |
15.60 (17) |
66.05 (72) |
1524 |
27.90 |
| 16 |
Basti |
33 |
48.49 (16) |
9.09 (3) |
42.42 (14) |
2825 |
27.00 |
| 17 |
Bhadohi |
28 |
25.00 (7) |
7.14 (2) |
67.86 (19) |
4231 |
37.80 |
| 18 |
Bijnor |
37 |
29.73 (11) |
2.70 (1) |
67.57 (25) |
6589 |
31.30 |
| 19 |
Budaun |
26 |
61.54 (16) |
3.85 (1) |
34.61 (9) |
4104 |
25.80 |
| 20 |
Bulandshahr |
25 |
76.00 (19) |
0.00 (0) |
24.00 (6) |
5242 |
24.40 |
| 21 |
Chandauli |
27 |
18.52 (5) |
11.11 (3) |
70.37 (19) |
3894 |
27.40 |
| 22 |
Chitrakoot |
7 |
100.00 (7) |
0.00 (0) |
0.00 (0) |
8145 |
31.80 |
| 23 |
Deoria |
27 |
66.67 (18) |
7.40 (2) |
25.93 (7) |
4437 |
34.80 |
| 24 |
Etah |
13 |
76.92 (10) |
7.69 (1) |
15.39 (2) |
4921 |
25.70 |
| 25 |
Etawah |
19 |
57.89 (11) |
5.27 (1) |
36.84 (7) |
3996 |
22.80 |
| 26 |
Faizabad |
26 |
57.69 (15) |
7.69 (2) |
34.62 (9) |
6748 |
40.60 |
| 27 |
Farrukhabad |
20 |
50.00 (10) |
10.00 (2) |
40.00 (8) |
4144 |
24.00 |
| 28 |
Fatehpur |
18 |
66.67 (12) |
5.56 (1) |
27.77 (5) |
6344 |
22.70 |
| 29 |
Firozabad |
21 |
52.38 (11) |
9.52 (2) |
38.10 (8) |
4446 |
28.10 |
| 30 |
Gautam Buddha Nagar |
37 |
21.62 (8) |
13.51 (5) |
64.86 (24) |
868 |
29.70 |
| 31 |
Ghaziabad |
33 |
21.21 (7) |
9.09 (3) |
69.70 (23) |
2820 |
21.40 |
| 32 |
Ghazipur |
33 |
48.48 (16) |
15.15 (5) |
36.37 (12) |
3018 |
33.70 |
| 33 |
Gonda |
24 |
75.00 (18) |
4.17 (1) |
20.83 (5) |
5703 |
30.50 |
| 34 |
Gorakhpur |
84 |
27.38 (23) |
13.10 (11) |
59.52 (50) |
2891 |
33.70 |
| 35 |
Hamirpur |
13 |
76.92 (10) |
0.00 (0) |
23.08 (3) |
4836 |
30.00 |
| 36 |
Hapur |
8 |
37.50 (3) |
50.00 (4) |
12.50 (1) |
6330 |
37.00 |
| 37 |
Hardoi |
34 |
58.82 (20) |
0.00 (0) |
41.18 (14) |
5077 |
26.80 |
| 38 |
Hathras |
12 |
75.00 (9) |
16.67 (2) |
8.33 (1) |
4888 |
36.20 |
| 39 |
Jalaun |
15 |
66.67 (10) |
6.67 (1) |
26.66 (4) |
5313 |
30.50 |
| 40 |
Jaunpur |
33 |
75.76 (25) |
0.00 (0) |
24.24 (8) |
4586 |
32.20 |
| 41 |
Jhansi |
26 |
50.00 (13) |
3.85 (1) |
46.15 (12) |
3618 |
30.40 |
| 42 |
Kannauj |
26 |
57.69 (15) |
30.77 (8) |
11.54 (3) |
2919 |
32.60 |
| 43 |
Kanpur Dehat |
23 |
56.52 (13) |
4.35 (1) |
39.13 (9) |
4241 |
31.30 |
| 44 |
Kanpur Nagar |
120 |
14.17 (17) |
19.16 (23) |
66.67 (80) |
990 |
23.30 |
| 45 |
Kasganj |
8 |
75.00 (6) |
12.50 (1) |
12.50 (1) |
11818 |
37.40 |
| 46 |
Kaushambi |
15 |
46.67 (7) |
26.67 (4) |
26.66(4) |
4817 |
28.70 |
| 47 |
Kheri |
26 |
65.38 (17) |
11.54 (3) |
23.08 (6) |
8040 |
26.30 |
| 48 |
Kushi Nagar |
43 |
34.88 (15) |
13.95 (6) |
51.17 (22) |
3257 |
28.10 |
| 49 |
Lalitpur |
14 |
50.00 (7) |
14.29 (2) |
35.71 (5) |
5068 |
41.40 |
| 50 |
Lucknow |
166 |
19.88 (33) |
16.87 (28) |
63.25 (105) |
1199 |
27.00 |
| 51 |
Maharajganj |
20 |
70.00 (14) |
5.00 (1) |
25.00 (5) |
5420 |
31.30 |
| 52 |
Mahoba |
6 |
100.00 (6) |
0.00 (0) |
0.00 (0) |
11105 |
38.30 |
| 53 |
Mainpuri |
22 |
54.55 (12) |
0.00 (0) |
45.45 (10) |
3600 |
29.50 |
| 54 |
Mathura |
38 |
39.47 (15) |
23.69 (9) |
36.84 (14) |
2024 |
25.60 |
| 55 |
Mau |
14 |
57.14 (8) |
0.00 (0) |
42.86 (6) |
6298 |
29.60 |
| 56 |
Meerut |
69 |
21.74 (15) |
18.84 (13) |
59.42 (41) |
2507 |
25.20 |
| 57 |
Mirzapur |
36 |
41.67 (15) |
19.44 (7) |
38.89 (14) |
4425 |
29.40 |
| 58 |
Moradabad |
37 |
24.32 (9) |
18.92 (7) |
56.76 (21) |
5258 |
29.40 |
| 59 |
Muzaffarnagar |
24 |
45.83 (11) |
4.17 (1) |
50.00 (12) |
3159 |
30.20 |
| 60 |
Pilibhit |
14 |
57.14 (8) |
0.00 (0) |
42.86 (6) |
9001 |
30.20 |
| 61 |
Pratapgarh |
42 |
80.95 (34) |
2.38 (1) |
16.67 (7) |
3100 |
25.30 |
| 62 |
Rae Bareli |
28 |
71.43 (20) |
3.57 (1) |
25.00 (7) |
6871 |
33.10 |
| 63 |
Rampur |
15 |
46.67 (7) |
20.00 (3) |
33.33 (5) |
5558 |
28.60 |
| 64 |
Saharanpur |
42 |
54.76 (23) |
4.76 (2) |
40.48 (17) |
2929 |
34.60 |
| 65 |
Sambhal |
13 |
84.62 (11) |
0.00 (0) |
15.38 (2) |
6669 |
26.60 |
| 66 |
Sant Kabeer Nagar |
12 |
58.33 (7) |
0.00 (0) |
41.67 (5) |
5510 |
36.30 |
| 67 |
Shahjahanpur |
29 |
62.07 (18) |
6.90 (2) |
31.03 (9) |
4901 |
25.10 |
| 68 |
Shamli |
14 |
50.00 (7) |
0.00 (0) |
50.00 (7) |
3860 |
38.80 |
| 69 |
Shravasti |
7 |
100.00 (7) |
0.00 (0) |
0.00 (0) |
8016 |
31.60 |
| 70 |
Siddharth Nagar |
16 |
81.25 (13) |
6.25 (1) |
12.50 (2) |
5355 |
34.20 |
| 71 |
Sitapur |
27 |
77.78 (21) |
7.41 (2) |
14.81 (4) |
10106 |
28.80 |
| 72 |
Sonbhadra |
24 |
33.33 (8) |
8.33 (2) |
58.34 (14) |
6540 |
34.20 |
| 73 |
Sultanpur |
38 |
42.11 (16) |
7.89 (3) |
50.00 (19) |
3137 |
34.00 |
| 74 |
Unnao |
46 |
36.96 (17) |
6.52 (3) |
56.52 (26) |
3263 |
26.20 |
| 75 |
Varanasi |
153 |
13.07 (20) |
11.76 (18) |
75.17 (115) |
1332 |
34.40 |
| |
Uttar Pradesh |
2546 |
40.53 (1032) |
11.55 (294) |
47.92 (1220) |
1163 |
30.35 |
| Source: AB-PMJAY Uttar Pradesh, 20/04/2020 |
| Note : in bracket numbers values is given |
Table 1. Hospitals Empanelled In Pmjay in Districts of Uttar Pradesh.
District level study reveals that only five districts in the Uttar Pradesh are noted where numbers of hospitals empanelled under PMJAY in three digits. Allahabad district with 179 hospitals shows first rank in terms of numbers of hospital which provides services under PMJAY. Other districts, where number of empanelled hospitals are more than 100 are Lucknow (166 hospitals), Varanasi (153 hospitals), Kanpur Nagar (166 hospitals) and Bareilly (109 hospitals). On the other hand there is also five districts in the state where numbers of hospitals less than 10 hospitals (Table 2).
| S.No. |
No of hospitals |
No of district |
Total hospitals |
Percentage of hospitals |
| 1 |
Less than 20 |
28 |
378 |
14.85 |
| 2 |
21- 50 |
38 |
1164 |
45.72 |
| 3 |
51-100 |
04 |
277 |
10.88 |
| 4 |
100 & above |
05 |
727 |
28.55 |
| Total |
|
75 |
2546 |
100.00 |
| Source: AB-PMJAY Uttar Pradesh, 20/04/2020 |
Table: 2. Availability of Hospitals by District.
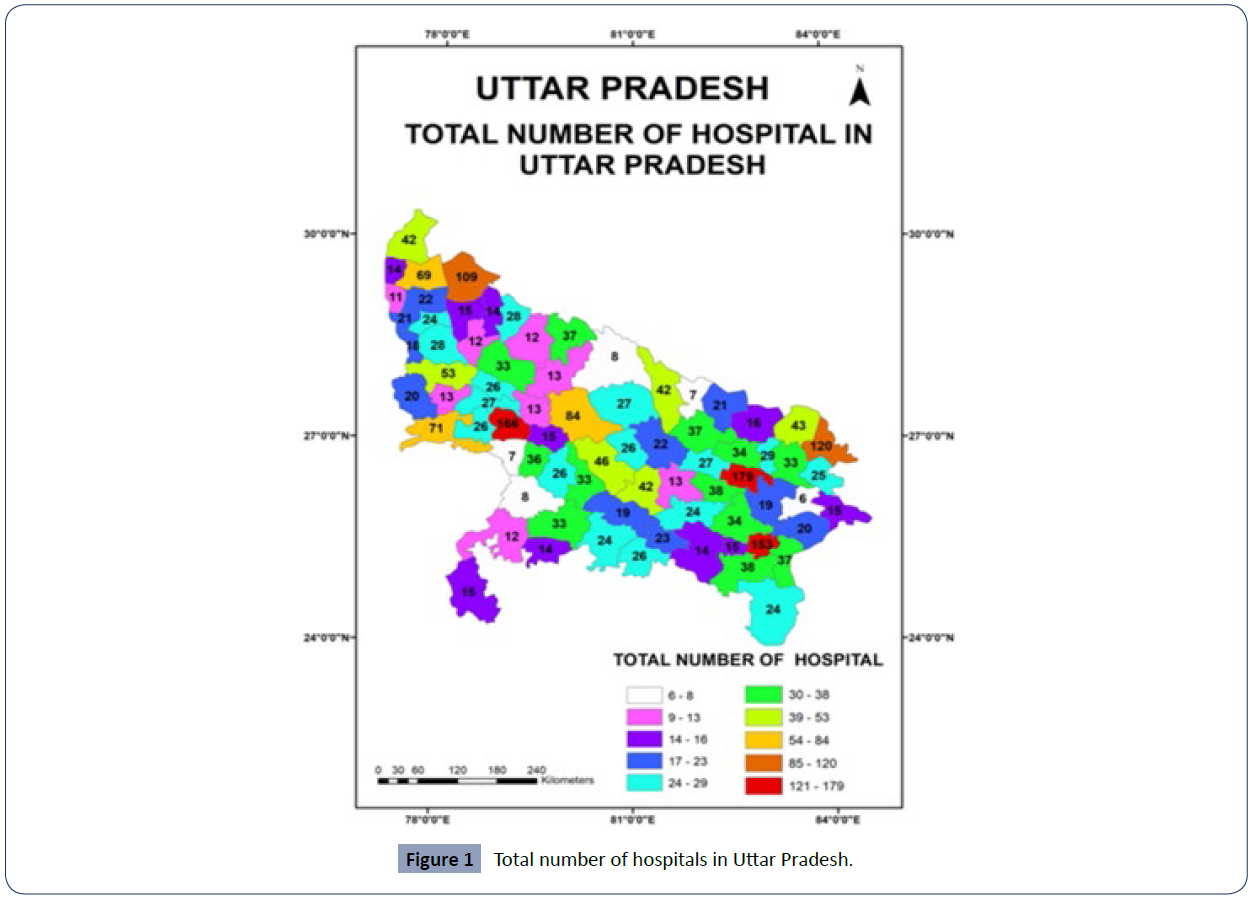
These districts are Mahoba (6 hospitals), Chitrakoot (7 hospitals), Shavasti (7 hospitals), Hapur (8 hospitals) and Kasganj (8 hospitals). From the analysis of data it is revealed that if numbers of total hospitals registered under PMJAY increased in any district at the same time the share of public hospitals decreased. It means if numbers of hospitals is less the number of public hospital is high (Figure 1).
Figure 1 Total number of hospitals in Uttar Pradesh.
The shape of public hospital in Allahabad district is only 15.64 percent. In all the top five districts in terms of numbers of hospital less than 20 percent of public hospitals. At the same time share of private for profit hospitals is nearly two third of total hospitals. Varanasi district shows highest percentage (75.16 percent) private for profit hospitals. In Ghaziabad district, out of total empanelled hospitals under PMJAY 69.70 percent hospitals are note in private (for profit hospitals). Data revealed that highly populated districts are shows more percentage of private for profit hospitals. The share of private for profit hospitals is 64.79 percent in Agra district, 64.80 percent in Allahabad district, 66.79 percent in Bareilly district, 64.86 percent in Gautam Budha Nagar district, 59.52 percent in Gorakhpur district, 66.67 percent in Kanpur Nagar district, 63.25 percent in Lucknow district and 59.42 percent in Meerut district. At the state level the share of private for profit hospitals is less than half (47.92 percent). The main reason is that in small districts of Uttar Pradesh (where numbers of hospital is less) the percentage of public hospitals is very higher. In the state, three districts namely Chitrakoot, Mahoba and Shravasti show all hospitals under PMJAY are public hospitals [15].
Number of hospitals registered in PMJAY is not satisfactory in the stare. More than one third of districts (28 districts) have upto 20 hospitals. The total numbers of hospitals in these 28 districts are 378 which are about 14.88 percent of total hospitals Table 2. Out of 75 districts in Uttar Pradesh 38 districts are marked in range of 21 to 50 hospitals. In the range of 51 to 100 hospitals only four districts are marked, they are Agra (71 hospitals), Alighar (53 hospitals), Gorakhpur (84 hospitals) and Meerut (69 hospitals). In these four districts percentage of public hospitals is very less as compare to private for profit hospitals. Top five districts in terms of total hospitals under PMJAY occupy 28.55 percent of total state hospitals. In these five districts 727 hospitals are note out of total 2546 hospitals noted under PMJAY in the state. It is also quite interesting that 65 districts in the Uttar Pradesh have less than or equal to 20 government hospitals for treatment of person under PMJAY. Only 20 districts shows value of public hospitals more than 20 hospitals (Table 3).
| Category |
Values |
Numbers of districts |
Name of District |
| Very High |
above 37.86 |
7 |
Baghpat, Lalitpur, Faizabad, Shamli, Mahoba, Ambedkar Nagar, Bhadohi |
| High |
37.86-33.22 |
18 |
Kasganj, Barabanki, Amethi, Hapur, Sant Kabeer, Nagar, Hathras, Deoria, Saharanpur, Varanasi, Sonbhadra, Siddharth Nagar, Sultanpur, Gorakhpur, Ghazipur, Rae Bareli, Kannauj, Auraiya, Allahabad |
| medium |
33.22-28.58 |
22 |
Jaunpur, Azamgarh, Chitrakoot, Shravasti, Kanpur Dehat, Bijnor, Maharajganj, Amroha, Jalaun, Gonda, Jhansi, Muzaffarnagar, Pilibhit, Hamirpur, Gautam Buddha Nagar, Mau, Mainpuri, Moradabad, Mirzapur, Sitapur, Kaushambi, Rampur |
| Low |
28.58-23.94 |
21 |
Bahraich, Kushi Nagar, Firozabad, Bareilly, Chandauli, Lucknow, Basti, Balrampur, Hardoi, Sambhal, Kheri, Unnao, Budaun, Etah, Ballia, Mathura, Pratapgarh, Meerut, Shahjahanpur, Bulandshahr, Farrukhabad |
| Very Low |
Below 23.94 |
7 |
Kanpur Nagar, Etawah, Fatehpur, Banda, Ghaziabad, Agra, Aligarh |
| Source: AB-PMJAY Uttar Pradesh, 20/04/2020 |
Table 3. District Wise Golden Family Out of Total Beneficiary Family in Uttar Pradesh.
Beneficiary Families per Hospital
The situation of availability of hospitals in Uttar Pradesh under PMJAY is not satisfactory (Singh & Kumar, 2017). There is one hospital on 1163 beneficiary families in the state. In Ambedkar Nagar district, there are only 13 hospitals for 160853 beneficiary families Table 1. This figures indicate that one hospital server nearly 12373 families. In the study are, four districts namely, Sitapur, Mahoba, Kasganj and Ambedkar Nagar where one hospital is available for more than 10000 families enlisted in PMJAY. Study ravels that 28 districts are marked where one hospital is serving 5000 to 10000 enrolled families for this scheme. Gautam Budha Nagar (868 families) and Kanpur Nagar (990 families) districts are have one hospital less than 1000 families [16, 17].
Golden Card Family Out of Total Beneficiary Family
Golden card is a card with the help of which any person of the country can get free treatment up to Rs 5 lakh in government and private hospitals empanelled under Ayushman Bharat Mission- Pradhan Mantri Jan Arogya Yojan. This golden card will be given to those poor people who will be the beneficiaries of Ayushman Bharat Yojana [18]. This card is very essential for medical care in enrolled hospitals under PMJAY Table 1.
The range of percentage of golden card families to total beneficiary families varies from as low as 19.3 percent in Alighar district to as high as 42.5 percent in Baghpat district. Not even a single district shows value of issued card more than 50 percent. The very high percentage of golden card having families (above 37.86 percent) marked in 07 districts. These districts are Baghpat (42.50 percent), Lalitpur (41.1 percent), Faizabad (40.6 percent), Shamli (38.8 percent), Mahoba (38.3 percent), Amedkar Nagar (38.8 percent) and Bhadohi (37.8 percent). High grade (33.22- 37.86 percent) is observed in 18 districts. Out of these 18 districts 02 districts, Varanasi (34.4 percent) and Allahabad each have more than 100 hospitals enrolled in PMJAY. At the same time these two districts also have satisfactory value of beneficiary families per hospital. Total 22 districts are observed in medium range (28.55-33.132 percent) of family having golden card. In this groups most of districts having less than 30 hospitals under PMJAY. It is also noted that all these districts having high ratio of beneficiary families to hospitals. Some districts of this category are, Sitapur (28.8 percent) having beneficiary families to per hospitals are 10106 families, Pillibhit (30.2 percent) shows 9001 families per hospital, Chitrkoot (31.8 percent) and Shravasti (31.6 percent) have this ratio 8154 families and 8016 families respectively. Low level (23.94-28.58 percent) observed in 21 districts Table 3. Some of the important districts of this group are Firozabad (28.1 percent), Bareilly (27.9 percent), Lucknow (27.0 percent), Mathura (25.6 percent) and Meerut (25.2 percent).Very low percentage of golden card families (below 23.94 percent) is marked in seven districts [19].
Many districts of this category having satisfactory ratio of beneficiary families to hospitals. Kanpur Nagar having 23.3 percent of golden card families but the ratio between beneficiary families to hospitals is 990 families per hospital. Similarly Alighar (19.3 percent) and Agra (20.6 percent) districts having beneficiary families to hospitals ratio below 2000 families per hospital. This analysis shows that if number of families having golden card is low than the beneficiary families to hospitals ratio is better [20].
Facilities Available in Hospitals
Hospitals enhance the functioning of many other areas of the health-care system by providing continuous access to services for both acute and chronic illnesses. Hospitals are also an essential part of health system development. Hospitals matter to people and often mark central points in their lives. Hospitals should represent the needs and values of the communities they serve, while also being robust and capable of maintaining and scaling up services in the event of an emergency (Hospital, n.d.). The empanelled hospitals under PMJAY scheme including both government and private hospitals. Hospitals will only be allowed to view and apply treatment package for the especially for which they are empanelled. The major focus of PMJAY scheme is to cover tertiary care for beneficiaries near their locality. All the empanelled hospitals provide beneficiaries to medical packages which including surgery and day care treatment, cost of medicines and diagnoses (Bharat, n.d.). It is noted that private hospitals more likely to offer surgical packages on the other hand public hospitals are more likely to offer medical packages only (Chatterjee et al., 2013). Uttar Pradesh government has been provided facility to benificries under PMJAY to purchase medical services through the trust model. In this insurance scheme hospitals provides both medical (M) as well as surgical (S) specialties to golden card holding families [21].
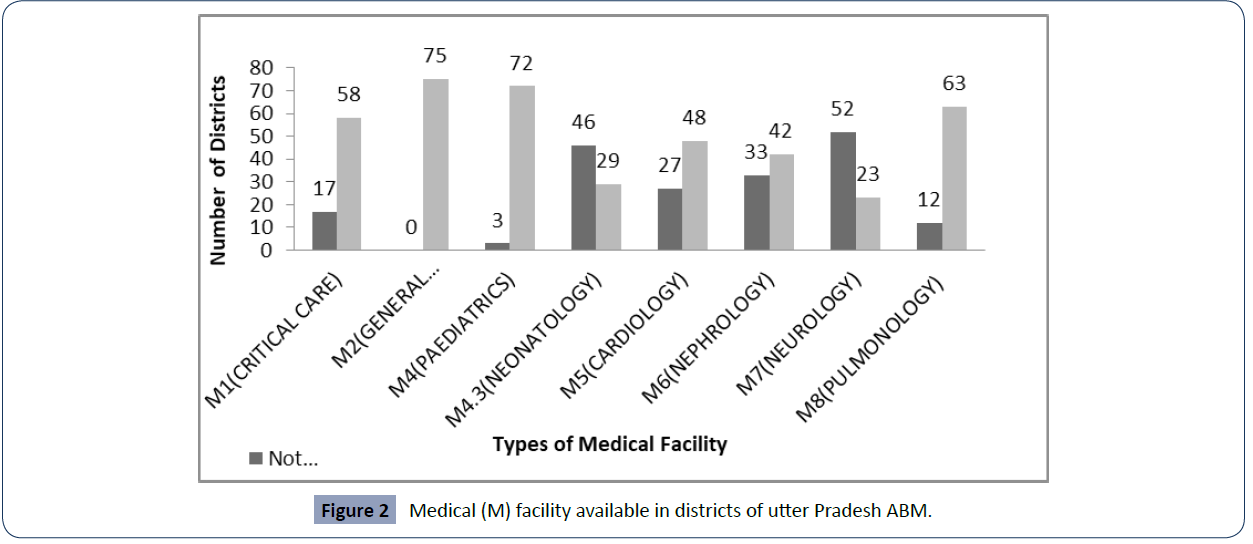
Medical Facilities (M) Packages: In the Uttar Pradesh there is total 75 districts and eight different types of medical packages are available in public, private (for profit) and private (not for profit) hospitals. M1 (critical Care) is founded in 58 districts and there is not a single hospitals is available in 17 districts in state Many districts where this facility is not available are related to Bundelkhand region like Banda, Chitrakoot, Jalaun, Lalitpur and Mohaba. It is also not available in districts of eastern Uttar Pradesh like Ghazipur, Kaushambi, Kushi Naga, Mirzapur, Rampur, Sant Kabeer Nagra etc. (Table 4).
| S.No. |
Facilities available in Hospitals |
No. of Hospital |
| 1 |
Data not Available |
24 |
| 2 |
only one |
1006 |
| 3 |
Two |
314 |
| 4 |
Three |
268 |
| 5 |
Four |
188 |
| 6 |
Five |
129 |
| 7 |
Six |
93 |
| 8 |
7 & ABOVE |
524 |
| |
TOTAL |
2546 |
| Source: AB-PMJAY Uttar Pradesh, 20/04/2020 |
Table 4. Numbers of Medical and Surgical Facilities Available in Hospitals.
Total 421 hospitals provide this facilities and only 15.68 percent (66 hospitals) are public hospitals. M2 i.e. general medicine is available in all districts (Table 8). Total 1744 hospitals are providing M2 facility in the state. Out of total hospitals 831(47.65 percent) are public hospitals, 187 (10.72 percent) are private (for profit) hospitals and 726 (10.72 percent) are public (not for profit) hospitals. M4- Paediatrics (the area of medicine connected with diseases of Children) specialty is noted 72 districts. Mahoba, Sambhal and Shravasti are only districts where M4 is not available. Total 728 hospitals provide this facility to member families of PMJAY, in which more than half 54.53 percent (397 hospitals) are private hospitals (not for profit hospitals). Neonatalogy-M4.3 is the branch of medicine concerned with the treatment and care of new born babies, is not available in 46 districts (61.33 percent) [22].
This indicate very critical situation for treatment of new born in Uttar Pradesh. According to Sample Registration System Bulletin, 2018 state shows very high infant mortality rate 43 per thousand lives birth as compare to 32 per thousand lives birth in India (Census of India Website : Office of the Registrar General & Census Commissioner, India, n.d.). Only 10.39 percent hospitals (29 hospitals) are provides this facility to the golden card families are of public hospitals. Specialty of Cardiology (M5) is available in 187 hospitals in state. District wise it is observed that only 48 districts are able to provides this facility to patient (Table 5). It also to interest to note that more than 80 percent hospitals are follow in categories of private hospitals (61.50 private not for profit and 20.32 private for profit). M6 i.e. Nephrology (the branch of medical science that deals with the Kidney) is not available in 33 districts of states. There are 197 hospitals in the Uttar Pradesh which provides this facility and out of which only 13 hospitals (6.60 percent) are public. These 13 hospitals are found in only nine districts. Aligarh, Farrukhabad, Gorakhpur, Hamirpur, Kanpur Nagar, Kaushinagar, Mathura and Varanasi districts have one hospitals each and Lucknow district having five hospitals. Neurology (M7) is a discipline of medicine that focuses on the structure, function, and illnesses of the human nervous system. This specialty is absent in 53 districts of stare. It is not available in some of the big populated districts like Azamgarh,Bulandshahr, Etawah, Hathras, Lalitpur, Muzaffarnagar, Pratapgarh, Saharanpur, Siddhartha Nagar, Unnao etc. Out of total 217 hospitals only 13 are public hospitals have this facility for families listed in PMJAY in state Table 5.
| Type of Hospital |
M1 (critical Care) |
M2 (General Medicine) |
M4 (Paediatrics) |
M4.3 (Neonatology) |
M5 (Cardiology) |
M6 (Nephrology) |
M7 (Neurology) |
M8 (Pulmonology) |
| Public |
15.68 (66) |
47.65 (831) |
29.26 (213) |
10.39 (29) |
18.18 (34) |
6.60 (13) |
6.45 (14) |
23.22 (98 ) |
| Private (For Profit) |
19.00 (80) |
10.72 (187) |
16.21 (118) |
19.35 (54) |
20.32 (38) |
17.26 (34) |
17.97 (39) |
18.25 (77) |
| Private (Not For Profit) |
65.32 (275) |
41.63 (726) |
54.53 (397) |
70.25 (196) |
61.50 (115) |
76.14 (150) |
75.58 (164) |
58.53 (247) |
| Total |
100 (421) |
100 (1744) |
100 (728) |
100 (279) |
100 (187) |
100 (197) |
100 (217) |
100 (422) |
| Source: AB-PMJAY Uttar Pradesh, 20/04/2020 |
Table 5. Medical Facilities available in different types of Hospitals.
The distribution of these 13 hospitals shows that Aligarh, Farrukhabad, Gorakhpur, Hamirpur, Kanpur Dehat, Kanpur Nagar and Kaushinagar one hospital in each district where as two hospitals in Varanasi district and four hospitals in Lucknow district. M8 i.e. Pulmonology is the study and treatment of conditions of lungs and respiratory system. It is not available in 12 districts of the state. Out of total 422 hospitals only 98 hospitals are public hospitals where as 247 (58.53 percent) hospitals are private (not for profit) (Figure 2) [23].
Figure 2 Medical (M) facility available in districts of utter Pradesh ABM.
Surgical Facilities (S) Packages: - Empanelled hospitals under Ayushman Bharat Mission-Pradhan Mantri Jan Arogya Yojan in Uttar Pradesh provide 18 different types of surgical packages to beneficiary families. General surgery-S1 is available in all districts in 1353 hospitals in the state. S2- ENT is available for beneficiary of PMJAY in 67 districts (Table 6).
| Type of Hospital |
S1 (General surgery) |
S2 (ENT) |
S3 (Ophthalmology) |
S4 (OBS. & Gynecology) |
S5 (Orthopedics) |
S7 (Cardio Thoracic Surgery) |
S8 (Pediatric Surgery) |
S9 (Genitourinary Surgery) |
| Public |
17.52 (237) |
21.54 (95) |
24.01 (134) |
22.68 (279) |
15.28 (141) |
32.61 (15) |
11.04 (18) |
7.31 (19) |
| Private(For Profit) |
15.23 (206) |
17.91 (79) |
22.04 (123) |
15.12 (186) |
17.01 (157) |
19.57 (9) |
17.79 (29) |
15.00 (39) |
| Private(Not For Profit) |
67.26 (910) |
60.54 (267) |
53.94 (301) |
62.20 (765) |
67.71 (625) |
47.83 (22) |
71.17 (116) |
77.69 (202) |
| Total |
-1353 |
-441 |
-558 |
-1230 |
-923 |
-46 |
-163 |
-260 |
| |
|
|
|
|
|
|
|
|
| Type of Hospital |
S10 (Neuro Surgery) |
S11 (Surgical Oncology) |
S12 (Medical Oncology) |
S13 (Radiation Oncology) |
S14 (Burns, Plastic & Reconstructive Surgery) |
S15 (Polytrauma) |
S16 (Paediatric Cancer) |
S18 (Dental Surgery) |
| Public |
5.02 (13) |
17.20 (16) |
17.65 (15) |
42.11 (16) |
11.16 (24) |
6.77 (17) |
25.53 (12) |
27.85 (115) |
| Private(For Profit) |
19.31 (50) |
15.05 (14) |
12.94 (11) |
13.16 (5) |
18.60 (40) |
16.73 (42) |
23.40 (11) |
19.13 (79) |
| Private(Not For Profit) |
75.68 (196) |
67.74 (63) |
69.41 (59) |
44.74 (17) |
70.23 (151) |
76.49 (192) |
51.06 (24) |
53.03 (219) |
| Total |
-259 |
-93 |
-85 |
-38 |
-215 |
-251 |
-47 |
-413 |
| Source: AB-PMJAY Uttar Pradesh, 20/04/2020 |
Table 6. Surgical Facilities available in different types of Hospitals.
The districts where this facility is absent are Chitrakkot, Etah, Kasganj, Mohba, Mainpuri, Rae Bareli and Sambhal. Total 441 hospitals provide facility of ENT surgery in state. S3- Ophthalmology (it is a branch of medicine and surgery that deals with the diagnosis and treatment of disorders of the eye) is available in 71 districts. It is noted 134 (24.01 percent) are public hospitals, 123 (17.91 percent) are private (for private) hospitals and 301 (53.94 percent) are private (not for profit) hospitals. S4- OBS. and Gynaecology is available in all districts. More than two third hospitals which provide this facility are private (for profit and not for profit) hospitals. S5 i.e. Orthopedics specialty is found in all the districts except Mahoba in Uttar Pradesh. There are total 923 hospitals out of which only 141 (15.28 percent) are public hospitals and remaining are private hospitals. Package of Cardio Thoracic Surgery (S7) is available only in 46 hospitals in state. These 46 hospitals are spreads over 20 districts [24-28].
There are 09 hospitals in Agra district and 07 hospitals in Lucknow district which provides S7 specialty to the patient. S8- Paediatric Surgery (It is a subspecialty of surgery involving the surgery of fetuses, infants, children, adolescents and young adults) is observed in 163 hospitals. This facility is available only in 27 districts. District wise distribution of hospitals in the Uttar Pradesh showing that Kanpur Nagar has highest number of hospitals (37 hospitals), it is followed by Lucknow (21 hospitals), Agra (15 hospitals), Bareilly (14 hospitals), Varanasi (12 hospitals), and Allahabad (11 hospitals) districts. In the state only 18 hospitals (11.02 percent) are public which provides this facility. Genitourinary (S9) refers to the Urinary and genital organs. This specialty available in 260 hospitals in state and it is mainly observed in private (not for profit) hospitals. S10- Nero surgery is noted in 259 hospitals of state. Only 13 hospitals (5.02 percent) are public hospitals which provide this facility to register families in PMJAY. More than one third of total hospitals marked in three districts Lucknow (36 hospitals), Kanpur Nagar (34 hospital) and Allahabad (32 hospitals). S11 (Surgical Oncology) and S12 (Medical Oncology) are available in 93 and 85 hospitals respectively. S13 i.e. Radiation Oncology found only in 38 hospitals in state. It is available only in 18 districts out of which more than half hospitals noted in two districts namely Lucknow (15 hospitals) and Meerut (6 hospitals) [29, 30].
Burns, Plastic and Reconstruction Surgery (S14) are marked in 36 districts with total 215 hospitals in state (Table 7).
| Type of Hospital |
M1 (critical Care) |
M2 (General Medicine) |
M4 (Pediatrics) |
M4.3 (Neonatology) |
M5 (Cardiology) |
M6 (Nephrology) |
M7 (Neurology) |
M8 (Pulmonology) |
| Available (%) |
77.33 (58) |
100 (75) |
96.0 (72) |
38.67 (29) |
64.0 (48) |
56.0 (42) |
30.67 (23) |
84.0 (63) |
| Not Available (%) |
22.67 (17) |
--- |
4.0 (3) |
61.33 (46) |
36.0 (27) |
44.0 (33) |
69.33 (52) |
16.0 (12) |
| Source: AB-PMJAY Uttar Pradesh, 20/04/2020 Note: in brackets Numbers of Districts |
Table 7. Medical Facilities Available in the District of Uttar Pradesh.
Distribution of hospitals according to types shows that 24 (11.16 percent), are public hospitals, 40 (18.60 percent) are private (for profit) hospitals and 151 (70.23 percent) are private (not for profit) hospitals. S15- Poly Trauma (two or more severe injuries in at least two areas of the body) facility is available in 45 districts with 251 hospitals. It is observed that a more than 75 percent hospital which provides this facility belongs to private (not for profit) category. Allahabad and Kanpur Nagar each have 31 hospitals. Pediatric Cancer i.e. S16 is noted only in 18 districts and available in 47 hospitals in the state. More than half of the hospitals marked in four district as Kanpur Nagar (8 hospitals), Agra (6 hospitals), Lucknow (6 hospitals) and Bareily (4 hospitals). S18 (Dental Surgery) is available in almost all the districts except Sambhal and Chitrakoot districts. Total 413 hospitals provide this facility and out of which more than half are marked as private (not for profit) hospitals Lucknow district with 44 hospitals shows highest numbers of hospital in a district (Figure 3).
Significance Test of Relationship
Finally an effort has been done to work out relationship between the dependent variables {Hospitals: Total (Y1), Public (Y2), Private-for profit (Y3) and Private- not for profit (Y4)} and the independent variables {indicators of socio-economic survey (X1- X12)} have been analyzed and tested (Table 9). The correlation analysis shows that nearly all the indicators of socio- economic survey are positively related to the number of hospitals. It means as that if the numbers of families increase under PMJAY there is need to increase hospital to serve the register families (Tables 8 and 9).
| Type of Hospital |
S1 (General surgery) |
S2 (ENT) |
S3 (Ophthalmology) |
S4 (OBS. & Gynecology) |
S5 (Orthopedics) |
S7 (Cardio Thoracic Surgery) |
S8 (Pediatric Surgery) |
S9 (Genitourinary Surgery) |
| Available (%) |
100 (75) |
84.33 (67) |
94.67 (71) |
100 (75) |
98.67 (74) |
26.67 (20) |
36.0 (27) |
69.33 (52) |
| Not Available (%) |
-- |
10.67 (8) |
5.33 (4) |
-- |
1.33 (1) |
73.33 (55) |
64.0 (48) |
30.67 (23) |
| Type of Hospital |
S10 (Neuro Surgery) |
S11 (Surgical Oncology) |
S12 (Medical Oncology) |
S13 (Radiation Oncology) |
S14 (Burns, Plastic & Reconstructive Surgery) |
S15 (Polytrauma) |
S16 (Pediatric Cancer) |
S18 (Dental Surgery) |
| Available (%) |
44.0 (33) |
26.67 (20) |
29.33 (22) |
24.0 (18) |
48.0 (36) |
60.0 (45) |
24.0 (18) |
97.33 (73) |
| Not Available (%) |
56.0 (42) |
73.33 (55) |
70.67 (53) |
76.0 (57) |
52.0 (39) |
40.0 (30) |
76.0 (57) |
2.67 (2) |
| Source: AB-PMJAY Uttar Pradesh, 20/04/2020 Note: in brackets Numbers of Districts |
Table 8. Surgical Facilities Available in the District of Uttar Pradesh.
| Independent Variables |
Dependent Variables |
| Total Hospital |
Public |
Private(For Profit) |
Private(Not For Profit) |
| (Y1) |
(Y2) |
(Y3) |
(Y4) |
| Total Number of Households Rural (X1) |
.309** |
.668** |
0.212 |
0.17 |
| Total Number of Households Urban (X2) |
.660** |
.305** |
.676** |
.614** |
| Beneficiaries Verified (X3) |
.500** |
.584** |
.443** |
.380** |
| Population(2011) (X4) |
.647** |
.718** |
.579** |
.506** |
| Total Households considered for deprivation (X5) |
0.194 |
.547** |
0.101 |
0.103 |
| No. of Deprived Households with deprivation criteria Only one room with kucha walls and kucha roof (X6) |
0.06 |
.419** |
-0.027 |
0.01 |
| No. of Deprived Households with deprivation criteria No adult member between age 16 to 59 (X7) |
0.163 |
.518** |
0.069 |
0.089 |
| No. of Deprived Households with deprivation criteria Female headed households with no adult male member between age 16 to 59 (X8) |
0.155 |
.554** |
0.056 |
0.061 |
| No. of Deprived Households with deprivation criteria Disabled member and no able bodied adult member (X9) |
0.159 |
.461** |
0.077 |
0.094 |
| No. of Deprived Households with deprivation criteria SC/ST households (X10) |
0.218 |
.539** |
0.13 |
0.129 |
| No. of Deprived Households with deprivation criteria No literate adult above 25 years (X11) |
0.144 |
.420** |
0.064 |
0.107 |
| No. of Deprived Households with deprivation criteria Landless households deriving major part of their income from manual casual labor (X12) |
.308** |
.425** |
.250* |
.260* |
| Source: Computed by Authors |
|
|
|
|
Table 9. Results of Correlation Co-Efficient (r) Between Types of hospitals and Variables Socio-economic survey.
Total hospitals (Y1) is positively correlated with total numbers of rural households (r = 0.309), total number of urban households (r = 0.660), beneficiaries verified (r = 0.500) and total population (r = 0.647) at 1 percent of significance. Public hospital (Y2) is positively correlated with all variables at 1 percent of significance. The data reveals that private -for profit hospital (Y3) is positively related with total number of urban household (r = 0.676), beneficiaries verified (r = 0.443) and total population (r = 0.579) at 1 percent of significance, while negatively correlated with numbers of deprived households with deprivation criteria only one room with kucha walls and kucha roof (r = -0.0.27). Private – not for profit hospitals (Y4) is positively correlated with numbers of disadvantaged households with deprivation criterion landless households relying on manual casual labour for the majority of their income (r = 0.260) at 5 percent level of significance [31, 32].
Conclusion and Findings
There is need of increase in the numbers of empanelled hospitals under PMJAY in all districts. The share of government is hospitals less in all the districts. Private for profit and private for not profit hospitals are empanelled in large numbers in the stare. Less than 10 hospitals empanelled under PMJAY sachem in the districts marked in Mahoba (6 hospitals, all are government hospitals), Chitrakoot (7 hospital, all are government hospitals), Shravasti (7 hospital, all are government hospitals), Hapur (8 hospitals) and Kasganj (8 hosapitals). Only nine districts are note where more than 50 hospitals are registered under PMJAY. Private hospitals are the main center for providing critical care facilities to patients, whereas Governments hospitals provides basic and First aid facilities to beneficiaries families. In small districts proper medical and surgical facilities are not available. Numbers of empanelled government hospitals are high in small districts and treatment facilities to patients are low. On the other hand empanelled hospitals private for profit and not for profit are high in big districts. Nearly in 50 percent of medical facilities are available in the private- not for profit hospitals. M2 i.e.
General Medicine is available in 47.65 percent of Government hospitals. In the case of surgical facilities private- not for profit hospitals are playing important role for beneficiaries’ families under PMJAY. Only M2 (General Medicine), S1 (General surgery) and S4 (OBS. &Gynaecology) facilities are available in all districts. M7 (Neurology) and M4.3 (Neonatology) are available in only in 23 and 29 districts of state respectively. S7 (Cardio Thoracic Surgery), S8 (Paediatric Surgery), S10 (Neuro Surgery), S12 (Medical Oncology), S13 (Radiation Oncology, S14 (Burns, Plastic & Reconstructive Surgery) and S16 (Paediatric Cancer) are surgical facilities which are available in less the half of the districts in Uttar Pradesh. Out of total empanelled hospitals nearly 40 percent of hospitals provide only one type of medical facility to patients.
This is very unique scheme which help to improve the health and decreases the out of pockets expenditures of rural as well as urban poor. Focus should be given to increase the medical facilities to patients in all types of hospitals. However, significant hurdles must be solved in order for these benefits to be recognised by the people and for the scheme to make a long-term contribution to Uttar Pradesh's development toward Universal Health Coverage.
REFERENCES
- Aggarwal A (2014) National standards of care quality would help India enable health coverage for all. BMJ 348: g3056-g3056.
Indexed at, Google Scholar, Crossref
- Angell B J, Prinja S, Gupt A, Jha V, Jan S (2019) The Ayushman Bharat Pradhan Mantri Jan Arogya Yojana and the path to universal health coverage in India: Overcoming the challenges of stewardship and governance. PLOS Medicine 16: e1002759.
Indexed at, Google Scholar, Crossref
- Annual Report 2018-19 Official Website Ayushman Bharat Pradhan Mantri Jan Arogya Yojana National Health Authority (n.d.).
Google Scholar
- Ayushman Bharat for a new India 2022 announced. (n.d.)
Google Scholar
- Ayushman Bharat-National Health Protection Mission (2021) National Portal of India. (n.d.).
Google Scholar
- Bharat A (n.d.). Guideline on Star Rating of Ayushman Bharat Pradhan Mantri -Jan Arogya Yojana (AB PM-JAY) Empanelled Hospitals 7.
Google Scholar
- Bhattacharjya A S, Sapra PK (2008) Health Insurance in China And India: Segmented Roles For Public And Private Financing. Health Affairs 27: 1005-1015.
Indexed at, Google Scholar, Crossref
- Bose M, Dutta A (2018) Health financing strategies to reduce out-of-pocket burden in India: A comparative study of three states. BMC Health Services Research 18: 830.
Google Scholar, Crossref
- Census of India (2021) Website Office of the Registrar General & Census Commissioner, India. (n.d.).
- Chakraborty L, Singh Y, Jacob J (2012) Public Expenditure Benefit Incidence on Health: Selective Evidence from India. In Working Papers.
Indexed at, Google Scholar
- Chatterjee S, Levin C, Laxminarayan R (2013) Unit Cost of Medical Services at Different Hospitals in India. 8: e69728.
Google Scholar, Crossref
- Chaudhuri A (2012) Socio-economic inequity in health care utilization & expenditures in richer States in India. IJMR 136: 368-369.
Indexed at, Google Scholar, Crossref
- Choudhury M, Datta P (2019) Private Hospitals in Health Insurance Network in India: A Reflection for Implementation of Ayushman Bharat.
Google Scholar
- Fan V Y, Karan A, Mahal A (2012) State health insurance and out-of-pocket health expenditures in Andhra Pradesh, India. Int J Health Care Finance Econ 12: 189-215.
Indexed at, Google Scholar, Crossref
- Garg CC, Karan A (2008) Health and Millennium Development Goal 1: Reducing Out-of-pocket Expenditures to Reduce Income Poverty - Evidence from India. In Working Papers.
Google Scholar
- General Reports: Planning Commission, Government of India. (n.d.) 2021.
Google Scholar
- Giannouchos T V, Vozikis A, Koufopoulou P, Fawkes L, Souliotis K (2020) Informal out-of-pocket payments for healthcare services in Greece. Health Policy 124:758-764.
Indexed at, Google Scholar, Crossref
- Gul A (2021) Ayushman Bharat Arogya Card. PM Modi Yojana.
- How Equitable Will Ayushman Bharat Be? Economic and Political Weekly. (n.d.) 2021.
Google Scholar
- Jahan B I (n.d.) Public Private Partnership in Uttar Pradesh Health Care Delivery System- UPHSDP as an Initiative 18.
Indexed at, Google Scholar
- Kaur S, Jain D N, Kumar S (2011) Addressing gender issues under Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY) in India- implications for equity 31.
Google Scholar, Crossref
- Keshri V, Gupta S (2019) Ayushman bharat and road to universal health coverage in India. JMGUMST 24:65.
Indexed at, Google Scholar, Crossref
- Kumar V, Mishra A (2015) Quality of health care in primary health care system: A reflection from Indian state. Int j health Sym disaster Manag 3: 136.
Google Scholar, Crossref
- Lahariya C (2018) Ayushman Bharat’ Program and Universal Health Coverage in India. Indian Pediatrics 55: 495-506.
Indexed at, Google Scholar, Crossref
- Paul V (2019) Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PMJAY): Hope for Millions and Exciting New Prospects for Neuro-Healthcare. Neurology India 67: 1186.
Indexed at, Google Scholar, Crossref
- Reddy K S, Patel V, Jha P, Paul V K, Kumar A K S et al. (2011) Lancet India Group for Universal Healthcare. Towards achievement of universal health care in India by 2020: A call to action. Lancet (London, England) 377: 760-768.
Indexed at, Google Scholar, Crossref
- Reshmi B, Nair NS, Sabu KM, Unnikrishnan B (2020) Awareness Of Health Insurance In A South Indian Population A Community-Based Study 12.
Google Scholar
- Sachs J (2001) Weltgesundheitsorganisation (Eds.) Macroeconomics and health: Investing in health for economic development report of the Commission on Macroeconomics and Health. World Health Organization.
Indexed at, Google Scholar
- Sharma SD (2018) Health Care for India’s 500 Million: The Promise of the National Health Protection Scheme. Harvard Public Health Review 18.
Indexed at, Google Scholar
- Singh P, Kumar V (2017) Insurance coverage under different health schemes in Uttar Pradesh, India. CEGH 5: 33-39.
Google Scholar, Crossref
- Ved RR, Gupta G, Singh S (2019) India’s health and wellness centres: Realizing universal health coverage through comprehensive primary health care. WHO South-East Asia Journal of Public Health, 8: 18-20.
Indexed at, Google Scholar, Crossref
- Woolhandler S, Himmelstein DU (2016) The Cadillac Tax on Health Benefits in the United States Will Hit the Middle Class Hardest: Refuting the Myth That Health Benefit Tax Subsidies Are Regressive. Int J Health Plann Manage. Administration, Evaluation 46: 325-330.
Indexed at, Google Scholar, Crossref
Citation: Kaushik K (2022) Ayushman Bharat
Mission: Protect the Health of Families in
Uttar Pradesh, India. Health Sci J. Vol. 16 No.
11: 984.