Review Article - (2022) Volume 0, Issue 0
Bakri Balloon as Last Non-Surgical Therapeutic Action to Control Postpartum Hemorrhage
Christian Camilo Galindez Guerrero1*,
Juan Carlos Aristizabal Mendoza2,
Lilian Paola Navarro Mercado3,
Andrea Carolina Montana Alarcon4,
Joselyn Ayme Hernandez Golon5,
Marilyn Alejandra Gomez Rosero6,
Lina Paola Velez Marin7,
Maite Isabel Rodríguez Acosta8 and
Rodrigo Alejandro Gomez Rodriguez9
1Gynecologist and Obstetrician, Universidad de Antioquia, Colombia
2General Physician, Universidad Cooperativa de Colombia Sede Santa Marta, Colombia
3General Physician, Fundación Universitaria San Martin, Sede Caribe, Colombia
4General Physician, Universidad de la Sabana, Colombia
5General Physician, Universidad San Carlos de Guatemala, Colombia
6General Physician, Universidad El Bosque, Bogota, Colombia
7General Physician, Universidad de Manizales, Colombia
8General Physician, Universidad del Magdalena, Colombia
9General Physician, Universidad Cooperativa de Colombia, Colombia
*Correspondence:
Christian Camilo Galindez Guerrero, Gynecologist and Obstetrician, Universidad de Antioquia,
Colombia,
Email:
Received: 22-Apr-2022, Manuscript No. Iphsj-22-12745;
Editor assigned: 24-Apr-2022, Pre QC No. QC No. Iphsj-22-12745;;
Reviewed: 10-May-2022, QC No. QC No. Iphsj-22-12745;
Revised: 15-May-2022, Manuscript No. Iphsj-22-12745(R);
Published:
23-May-2022, DOI: 10.36648/1791-809X.16.S7.947
Abstract
Postpartum hemorrhage is defined as blood loss greater than 500 ml after vaginal delivery or 1000 ml after caesarean section. This alteration is among the most frequent obstetric complications and with the highest mortality rate, in fact, postpartum haemorrhage is currently one of the leading causes of maternal death worldwide, considering that 25% of maternal death is caused by this complication, that is why its early diagnosis and management should be known by any doctor, regardless of the level at which they are. It is also important to highlight the role of this complication, both due to its magnitude and the need to develop methods that manage to mitigate the problem, thus causing the existence of various tools available to avoid or minimize its occurrence, currently counting on multiple medical interventions, surgical and non-surgical potentially effective for its treatment, such as the Bakri Balloon. Which is considered a non-invasive, fast and safe method to treat postpartum hemorrhage mainly secondary to uterine atony?
Keywords
Hemorrhage; Postpartum; Bakri balloon; Control; Blood loss; Therapeutic measure
Introduction
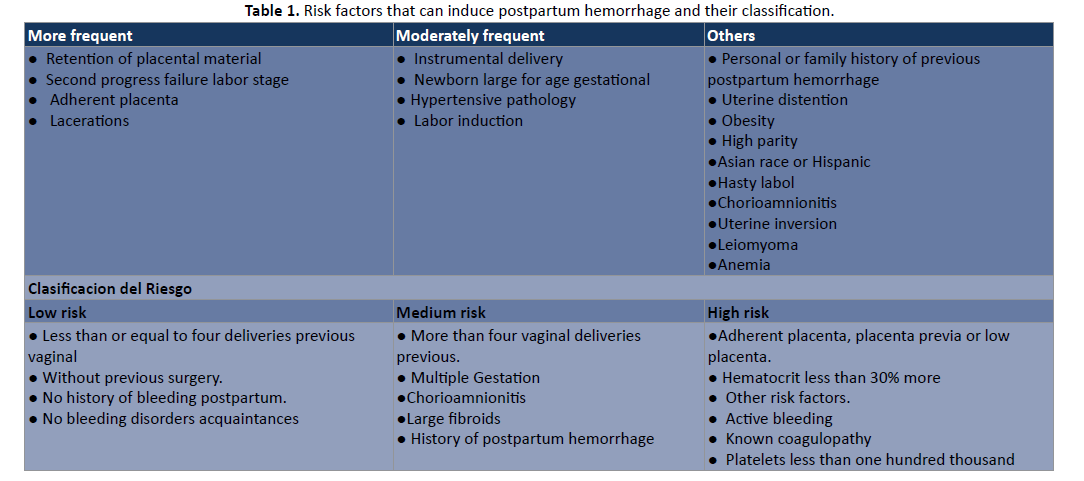
Postpartum hemorrhage or also known by its acronym as PPH, is considered blood loss greater than 1000 millilitres or bleeding associated with signs/symptoms of hypovolemic within the first 24 hours after birth, regardless of the route of delivery, other authors define it as any blood loss greater than 500 milliliters after a vaginal delivery or greater than 1000 milliliters after a caesarean section, or any blood loss after delivery that causes hemodynamic instability, always taking into account the type of delivery performed [1]. However, despite advances in the field of obstetrics, obstetric hemorrhage remains one of the main causes of maternal death in several countries, in fact, it was estimated that at least 25% of deaths are due to these haemorrhages and, additionally, 14 million women suffer from postpartum hemorrhage and of these it is estimated that more than 125,000 women die of PPH in the world annually, likewise, it is well known that 99% of these deaths occur in developing countries with an onset of characteristic signs and symptoms in women such as: dizziness, loss of consciousness, presence of hypotension, acceleration of heart rate, and an abnormal reduction in urine during a period of twenty-four hours [2]. Therefore, without a doubt, the authors affirm that it is a significant obstetric emergency, for this reason it is very important that the doctor detects the risk factors Table 1 of the patient and possible causes, for a correct prevention during consultations for prenatal controls, for a subsequent early diagnosis and thus provide the most appropriate treatment, according to the needs of the case [3, 4] (Table 1).
Table 1: Risk factors that can induce postpartum hemorrhage and their classification.
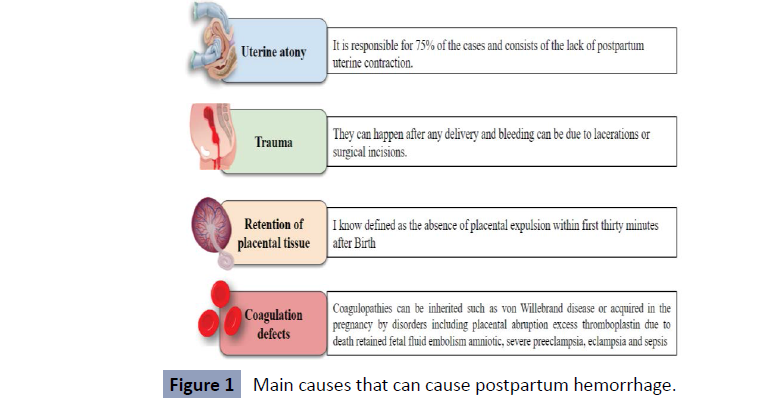
Among the causes, the most common capable of triggering postpartum hemorrhage is uterine atony, which complicates 1 in 40 births in the United States and is responsible for at least 75% of cases of postpartum hemorrhage, followed by trauma that Generally, damage resulting from precipitous or uncontrolled delivery or instrumental delivery of a large infant is considered; however, they can occur after any delivery due to lacerations and surgical incisions. Other widely described causes are retention of placental tissue and coagulation defects, as shown in Figure 1. In the first case, it refers to the absence of expulsion of the placenta. placenta after 30 min after delivery, this period can be extended to 90-120 minutes in deliveries in the second trimester and the main risk factor for retained placenta is gestational age less than 26 weeks and in the latter case, disease Von Will brand’s is the most common hereditary coagulopathy with a prevalence of 1.3%, however, coagulopathies acquired in pregnancy are more frequent, which can be due to various obstetric disorders, including placental abruption, excess thromboplastic due to a retained fetal death, fluid embolism among others [5,6] (Figure 1).
Figure 1: Main causes that can cause postpartum hemorrhage.
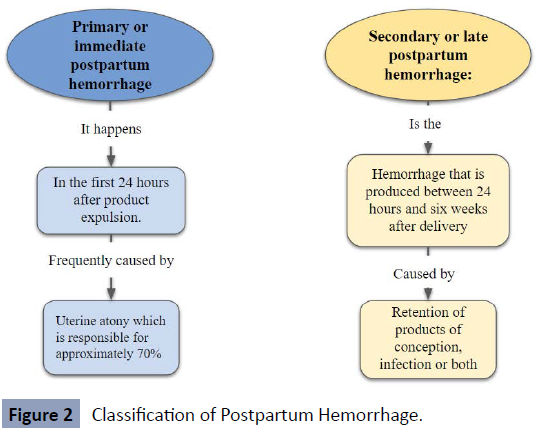
In addition to knowing the causes and risk factors of postpartum hemorrhage, it is also essential for the doctor to know the time elapsed since the start of the hemorrhage to prevent mortality; for this, there is a classification of hemorrhages after childbirth. Such classification is divided into two aspects as shown in Figure 2, in the first instance there is primary or early postpartum hemorrhage that occurs within the first 24 hours of the puerperium and according to the medical literature, uterine atony is the most frequent cause that It triggers it where it causes a failure in the myometrium contraction mechanism, promoting the inability of the uterus to contract and restore itself, after the delivery of the fetus, while, in the second instance, there is late or secondary postpartum hemorrhage that occurs after the 24 hours up to 6 weeks, although some authors mention 12 weeks after vaginal delivery or caesarean section, whose Etiology may be due to retention of products of conception, infection or both [7] (Figure 2).
Figure 2: Classification of Postpartum Hemorrhage.
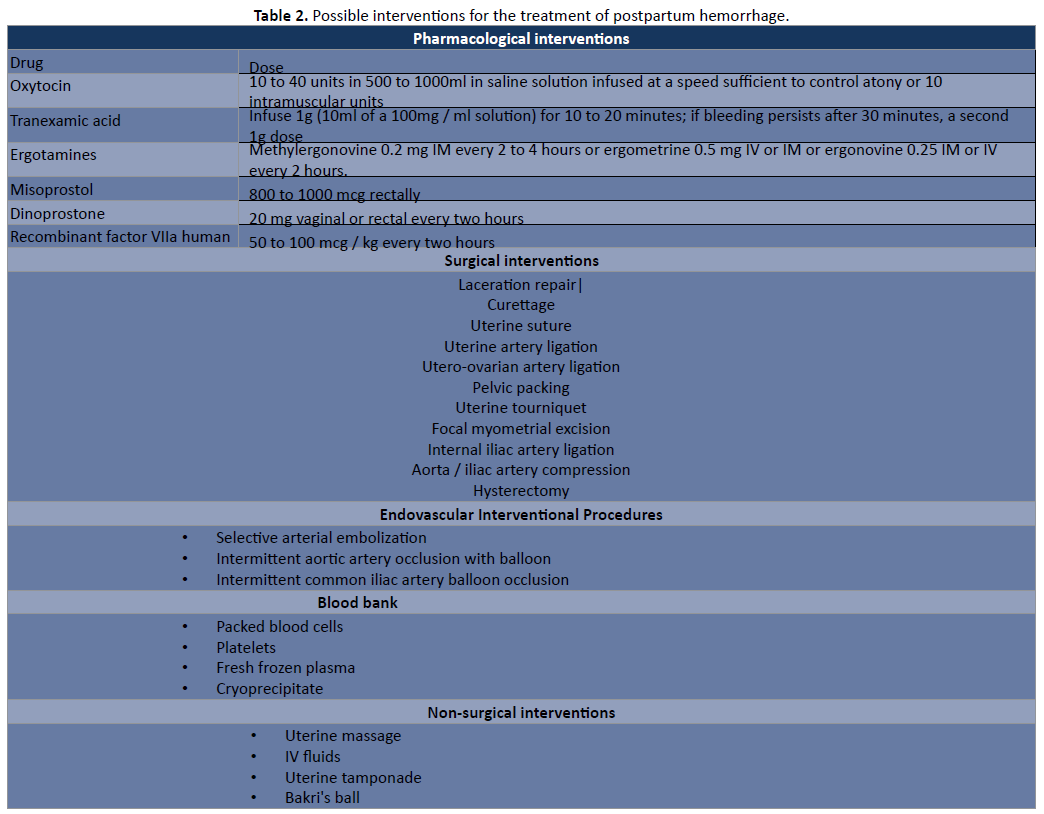
According to the WHO, global maternal mortality has been reduced by approximately 44% between 1990-2015, despite the decrease in the percentage of deaths; the figures remain high in developing countries, mostly due to deaths after hemorrhages. Postpartum. Due to these figures, the current goal to reduce the rate of maternal death due to hemorrhage in the world is less than 70/100,000 live births in a period between 2016-2030 [8]. For this and what has been mentioned throughout In this bibliographic review, it is considered important to highlight the role of this complication, both due to its magnitude and the need to develop methods that manage to mitigate the problem, thus causing the existence of various tools available to avoid or minimize its occurrence, currently counting on multiple potentially effective medical and surgical interventions for its treatment as shown in (Table 2) [9, 10, 11].
Table 2: Possible interventions for the treatment of postpartum hemorrhage.
Source: Dahlke DJ, Mendoz-Figueroa H, Maggio L, Hauspurg AK, Sperling JD, Chauhan SP, Rouse DJ. Prevention and management of postpartum hemorrhage: a comparison of 4 national guidelines. Am J Obstet Gynecol.
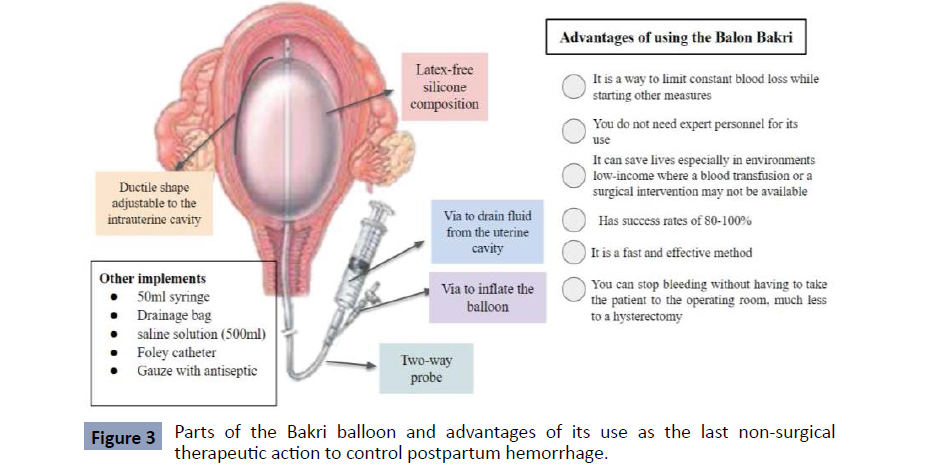
Among the interventions described to treat postpartum hemorrhage, there are the non-surgical ones that arise with the purpose that doctors, in any kind of hospital, regardless of their level, can provide the best management of the complication in question, in a simple way. fast and safe. This prevents a permanent invasive surgical procedure and death. Among the non-surgical techniques highlighted as the latest therapeutic action is the Figure 2 Classification of Postpartum Hemorrhage. Bakri balloon, discovered in 1992 by Bakri, which is made up of 100% silicone (without latex) as shown in Figure 3, with a ductile shape that allows it to conform to the uterine anatomy. It has a probe with two pathways: One for balloon inflation and the other to drain the uterine cavity (occult bleeding), where it allows the application of up to 500 g of traction tension. Once deflated it is very easy to remove, which is why it is considered a non-surgical procedure. In addition to the catheter, a 50 mL syringe, drainage bag, saline solution (500 mL), Foley catheter, and antiseptic gauze for vaginal plug are required. It can be inserted transvaginally or abdominally, depending on the type of delivery, provided that uterine rupture, tears and retention of placental fragments is ruled out [12]. Generally, this measure is used to control hemorrhage. In fact, massive blood loss must be avoided through three basic manoeuvres and a fourth action, which is the application of the Bakri balloon. The three established containment manoeuvres are: abdominal aortic compression, bimanual compression and vaginal clamping of the uterine arteries, and lastly the use of a Bakri balloon, the latter being the first paradigm shift, which aims to prevent bleeding by immediately closing the site of bleeding originating after delivery [13]. Similarly, it is well known that among the advantages of this technique, the Bakri ball is a very useful and easy method to perform, which requires a minimum level of training, in addition, it has a high level of safety, with a rate of success reported in the different series that ranges between 75 and 97%, where postpartum hemorrhage was stopped and surgical resolution was avoided, this device manages to stop bleeding, without requiring invasive or permanent techniques, nor does it associate longterm complications, which it becomes a last form of therapeutic action although some authors mention it as a first-line use [14].
Figure 3: Parts of the Bakri balloon and advantages of its use as the last non-surgical therapeutic action to control postpartum hemorrhage.
Materials and Methods
A detailed bibliographic search of the most relevant published information is carried out in the databases PubMed, scielo, medline, national and international libraries specialized in the topics covered in this review article. The following descriptors were used: Hemorrhage, Postpartum, Bakri balloon, Control, Blood loss, Therapeutic measure. The data obtained range between 5 and 40 records after the use of the different keywords. The search for articles was conducted in Spanish and English, limited by year of publication, and studies published from 2013 to the present were used.
Results
After applying the search strategies in the different databases,
between 5 and 30 records were obtained that met the
inclusion criteria. The study by Aibar et al. aimed to evaluate
the effectiveness of the Bakri balloon (BBT) in the treatment
of postpartum hemorrhage. After the analysis of 24 women
with postpartum hemorrhage treated with a Bakri balloon as a
conservative therapeutic option. The Bakri balloon managed to
control bleeding in 87.5% of women. It was effective in all women
with vaginal delivery (five out of five) and in all women with
uterine atony who did not respond to medical uterotonic therapy
(eight out of eight) [15]. Likewise, Gronval et al. present a series
of cases where they conclude that the bakri balloon is a simple,
easily available, effective and safe procedure for the treatment of
PPH in selective cases. Even if BBT fails, it can provide temporary
packing and time to prepare for other interventions or transport
from the local hospital to the tertiary center. From their results
with an overall success rate of 86% [16]. However, in a study
where the effectiveness of the Bakri balloon was estimated for the
treatment of postpartum hemorrhage in 35 women, the success
rate was 67.57%. Bakri failure was associated with caesarean
section (67% versus 16%, p = 0.031) and Pitocin before delivery
(67% versus 28%, p = 0.003) and with more ICU admissions (58%
versus 4%, p = 0.0003), transfusions (5.4 units of red blood cells
vs. 1.6, p = 0.007) and days of hospitalization (5.65 vs. 3.75,
p = 0.011). The reasons for failure were continuous bleeding or
extrusion of the balloon [17]. Other reports report that the Bakri
balloon is the quick and least invasive method for the treatment
of bleeding due to placenta previa with minimal complications,
since the Bakri tamponade was effective in 22 cases (88%) and in
the cases in which that failed required additional procedures such
as hypo gastric artery ligation, B-Lynch suture, and hysterectomy
[18]. BBT is an effective, easy-to-use, and safe procedure for massive PPH that can minimize recourse to hysterectomy after
failed medical treatment, reflected in 43 women where its use
was successful with an overall success rate 91.4%, since the
remaining 4 cases required an additional surgical procedure [19].
In addition, rapid diagnosis or prognosis of PPH, in combination
with early use of the Bakri postpartum balloon, is important.
The success rate is quite similar between studies, it was 91.65%
(373/407 women) in another report. Furthermore, blood loss
before and after balloon insertion was significantly higher in
the Bakri balloon failure group (1700 ± 1429.88 mL before and
1209.58 ± 1139.72 mL after balloon use) than in the success group
[918 ± 493.92 ml before (P = 0.002) and 266.57 ± 361.60 ml after
using the balloon (P = 0.001)] [20]. Brown et al. They carried out
a retrospective study including 58 patients, in whom postpartum
bleeding was controlled without further surgical intervention
in 55 (95%) with the use of the Bakri balloon, successfully
controlling PPH in 52 women [21]. A single-blind randomized
controlled trial conducted at Assiut Women's Health Hospital
compared condom-loaded Foley catheter versus Bakri balloon
in the treatment of primary atonic postpartum hemorrhage
(PPH) secondary to vaginal delivery in 66 women, the results
indicate that Both treatment modalities successfully controlled
primary atonic PPH without a statistically significant difference
[30/33 (91.0%) and 28/33 (84.84%), p = .199; respectively]. But
the Bakri balloon had the advantage of requiring a shorter time
to stop uterine bleeding (9.09 min vs. 11.76 min, p = 0.042,
respectively) [22]. Other studies have tested the Bakri balloon
with other therapeutic techniques in combination to be more
effective than the use of BBT alone, as indicated by the results
of Guo et al. where a group of study patients underwent double
compression, and these patients had a better clinical efficacy
rate of 96.3% (157 of 163), while the efficacy in cases using the
Bakri balloon alone (group control) was 87.3% (124 of 142).
Postoperative complication rates for these two groups were
9.4% and 8.7%, respectively [23]. It is also important to note
that the introduction of the Bakri balloon is consistent with a
decrease in the postpartum hysterectomy rate from 7.8/10,000
deliveries to 2.3/10,000 deliveries (p = 0.01) [24]. The same thing
happened in the report by Maher et al. where they identified
one hundred fifty-one cases such as low-lying placenta and PP,
of which 114 developed PPH. Two patients were unstable and
required immediate hysterectomy. The remaining 112 cases
were managed using balloon (72 cases) or non-balloon (40 cases)
protocols. The balloon only achieved haemostasis in 87.5% of
cases. When specifically analyzed, balloon success was associated
with no accreta (odds ratio 0.001, confidence interval 0.000–
0.974) and short operative time (odds ratio 1.143, confidence
interval 1.018–1.282), so they concluded that the application of
the Bakri balloon for the management of PPH after caesarean
section in cases of PP is an effective strategy [25]. In the report by
Soyama et al. Of the 266 women with placenta previa, 50 were in
the balloon group and 216 in the non-balloon group. The amounts
of bleeding were significantly less in the balloon group than in
the non-balloon group: intraoperative bleeding (991 vs. 1250
g, p < 0.01), postoperative bleeding (62 vs. 150 g, p < 0.01) and
total bleeding (1066 vs. 1451 g, p < 0.01). In addition, the mean
duration of surgery was shorter in the balloon group than in the
non-balloon group (30 vs. 50 min, p < 0.01). In the balloon group, five patients experienced increased bleeding due to balloon
prolapse from the uterus postoperatively, but the bleeding was
controlled by balloon reinsertion without additional haemostatic
procedures. Therefore, using a Bakri balloon during caesarean
section significantly decreased intraoperative and postoperative
bleeding [26]. In the presentation of a clinical case of a 29-yearold
woman who had PPH at the time of caesarean delivery,
which was effectively controlled by placing an intraoperative
Bakri balloon. On examination, approximately 1000 ml of blood
loss was estimated and the uterus was still stunned, so at this
time, a Bakri balloon was aseptically removed and placed in the
uterine cavity, and 150 ml of normal saline to distend the balloon
(refer to the discussion portion of the case report for full details
of the placement technique). Slowly, the tamponade effect of the
Bakri balloon improved the bleeding. Therefore, Bakri balloon
tamponade is usually indicated as second-line therapy for severe
PPH only when initial trials of bimanual compression of the
uterus and uterotonic drugs fail to control bleeding. This appears
to have minimal adverse effects on subsequent reproductive
and menstrual function when intrauterine balloon tamponade is
used for the treatment of severe PPH. Early use of intrauterine
balloon tamponade is a way to effectively limit on-going uterine
blood loss while other measures are initiated, and can be easily
implemented by providers with minimal training [27].
Discussion
The results of the studies analyzed in this systematic review
reveal the existence of a technique that replaces surgical therapy
in cases of postpartum hemorrhage. It was Bakri who initially
described (1992) the use of the balloon for the control of obstetric
hemorrhage due to placenta previa accreta [28]. Recently, a
summary of studies showed that intrauterine balloon tamponade
(IUBT), such as the Bakri balloon (Cook Medical, Bloomington, IN,
USA), is an effective tool to avoid invasive procedures treating
persistent PPH, and 75% of women do not need further treatment
after IUBT [29]. It is made of silicone, has a drainage lumen,
and is shaped like a sausage-like spindle. The study by Sayori
et al. agree with our results, as their findings suggest that Bakri
balloon tamponade can be applied for the treatment of massive
PPH in uterine atony and placenta previa. The Bakri balloon
appears to have the following merits: (1) easy insertion into the
uterine cavity and low slip rate, (2) adequate adaptability to the
haemorrhagic area due to its spindle shape, (3) ability to control
blood loss through the drainage lumen even after insertion. The
median (third and first quartile ranges) duration of stay in the
Bakri balloon was 24 hours (24-11 hours). The overall success rate
of Bakri balloon tamponade was 90% (9/10) [30]. Additionally,
the study by Cetin et al. He compared the therapeutic action of
the Bakri balloon with the Hayman compression suture and his
results indicate that the success rates of both methods were
similar (76.7% in the Hayman group and 74.4% in the BBT group).
In both groups, the success rate increased with the addition of
arterial ligations (93% in the Hayman group and 87.2% in the
BBT) [31]. Therefore, the literature reports that Bakri balloon
tamponade is an effective, safe and practical method in the
treatment of postpartum hemorrhage, based on the findings of a
report, where the frequency of massive postpartum hemorrhage was 0.61%. (n = 168). Among the 168 patients with massive
postpartum hemorrhage, there were 50 patients in whom the
Bakri balloon catheter was used and recovery was satisfactory
[32]. It is also important to mention that in cases with placenta
accreta/increta, with expected placental abruption and who are
willing to preserve fertility, the application of uterine balloon
tamponade devices before hysterectomy is encouraging with
its advantages compared to hysterectomy. , as indicated by
the results of Pala et al. since among the 36 patients diagnosed
with placenta accreta or increta, 19 patients were treated with
Bakri balloon tamponade while 17 cases were treated with
hysterectomy. Intraoperative blood loss was 1,794 ± 725 ml
in G1, less than in G2 (2,694 ± 893 ml). The amount of blood
transfusion was 2.7 ± 2.6 units in G1, lower than that in G2 (5.7
± 2.4 units) as well. The operation time was 64.5 ± 29 min and
140 ± 51 min in G1 and G2, respectively, showing significant
differences between the two groups, obtaining a Bakri balloon
success rate of 84.21% [33]. However, a meta-analysis by Suarez
et al. They conclude that the evidence on the efficacy of uterine
balloon tamponade and the effectiveness of randomized and
non-randomized studies is conflicting, with experimental studies
not suggesting any beneficial effect, in contrast to observational
studies [34]. Which is consistent with the conclusion of Said et
al. that the Bakri balloon appears to be a more effective tool for
the treatment of PPH, either after vaginal or caesarean delivery,
in addition to finding that displacement of the Bakri balloon
from the uterine cavity was reported in five publications, with an
overall rate of 9% (95% CI: 5-15%) [35]. Even so, measurements
of balloon displacement during inflation showed that the
shaft cover significantly prevented the Bakri balloon from
displacement. The volume of residual fluid in the upper uterine
cavity was significantly less with the Kyoto balloon system than
with the Bakri balloon system, indicating the efficacy of the Kyoto
balloon for tamponade of the upper uterine cavity [36]. Thus, the main cause of BBT failure was balloon prolapse [37]. Strange
situations can also occur as in the case that describes a very rare
complication of Bakri Balloon during the treatment of postpartum
hemorrhage; massive hem peritoneum with hemodynamic
shock, due to migration through the right broad ligament, with
anterior rupture of the uterus and irreversible injury to the right
uterine artery [38]. Despite its advantages, if we compare it
with other techniques it could be limited. The advantages of the
B-Lynch suture include rapid application without the need for a
lithotomy position or additional material; while the Bakri balloon
is less invasive and easier to learn, but more time consuming
and expensive compared to the B-Lynch suture. Therefore, they
suggest that the B-Lynch suture may be preferred in uterine atony
during caesarean section in low-resource settings; however, the
less invasive Bakri balloon should be the first line in full resource
settings [39]. The clinical implications they recommend are:
women should not be required to fast to remove the balloon;
balloon removal should occur at 12 hours if considered stable
and adequately resuscitated; deflation and balloon removal can
occur at the same time; and antibiotics should be discontinued
after balloon removal. This will allow women to mobilize and
recover sooner, and will improve flow and performance in our
high-acuity care areas [40].
Conclusion
In conclusion, the use of the intrauterine Bakri balloon is a safe and effective technique for early management of postpartum hemorrhage, with extremely high success rates greater than 75%, regardless of its Etiology. What makes it even more considerable, in addition to its use as a last therapeutic action or even as a first line, is its ability to stop bleeding, thus completely stopping bleeding, without requiring a high level of experience to carry out the procedure. , without the use of invasive or permanent techniques, or associated with long-term complications.
REFERENCES
- Belfort MA (2019) Overview of postpartum hemorragia.
Google Scholar
- Belfort MA (2019) Postpartum hemorragia: Medical and minimally invasive management.
Indexed at, Google Scholar
- Clinical Practice Guide (2013) Prevention diagnosis and treatment of postpartum hemorragia. Ministry of Public Health of Ecuador.
Indexed at, Google Scholar
- Clinical Practice Guide Immediate labor (2015) delivery and postpartum care. Ministry of Public Health of Ecuador.
- Conrad LB, Groome LJ, Black DR (2015) Management of Persistente Postpartum Hemorragia Caused by Inner Myomertrial Lacerations. Obstet Gynecol 126:266.
Indexed at, Google Scholar, Crossref
- Decherney AH (2014) Obstetrics and Gynecology Diagnosis and Treatment. Mexico McGraw-Hill
Google Scholar
- Guzman, Narvaez, Seguel, Lizana (2017) B-Lynch suture in postpartum hemorragia due to uterine inertia. Hospital Dr. Luis Tisne Brousse experiencia. J Obstet Gynaecol Res 11.
Indexed at, Google Scholar, Crossref
- Maternal Mortality Facts and Figures WHO February 2018.
Google Scholar
- Quijada, Brigida Piedad Ramirez, Katia Castro Paniagua (2017) Silvia Karhuayo Lugan Prevalence and epidemiological profile of puerperal women with postpartum hemorragia. Ayacucho 2000-2015. Colombian Magazine Salud Libr 12:7-14.
Indexed at, Google Scholar
- World Health Organization WHO recommendations for the prevention and treatment of postpartum haemorrhage Geneva: WHO.
Indexed at
- Solari A, Solari C, Wash A, Guerrero M, Enriquez O (2014) Postpartum hemorragia Main etiologies, their prevention, diagnosis and treatment. Rev Med Clin Earls 25:993-1003.
Google Scholar, Crossref
- Hernandez Cabrera, Yoan (2017) Uterus-conserving surgical alternatives for postpartum hemorragia. Medisur 15:684-693.
Indexed at, Google Scholar
- Garcia-Benavides, Juan Luis (2018) Postpartum obstetric hemorragia: proposal for a comprehensive Basic management, algorithm of the. Mexican J Anesth 41:190-194.
Indexed at, Google Scholar
- Kaya B (2014) Balloon tamponade in the management of postpartum uterine hemorragia. J Perinat Magazine Med 42:745-753.
Indexed at, Google Scholar, Crossref
- Aibar, Laura (2013) Bakri balloon for the management of postpartum hemorrhage." Acta Obstet Gynecol Scand 92: 465-467.
Indexed at, Google Scholar, Crossref
- Grönvall, Maiju (2013) "Use of Bakri balloon tamponade in the treatment of postpartum hemorrhage: a series of 50 cases from a tertiary teaching hospital. Acta Obstet Gynecol Scand 92: 433-438.
Google Scholar, Crossref
- Olsen, Richelle (2013) Bakri balloon effectiveness for postpartum haemorrhage: a “real world experiencia. J Matern-Fetal Neonatal Med 26:1720-1723.
Indexed at, Google Scholar, Crossref
- Kumru, Pınar (2013) The Bakri balloon for the management of postpartum hemorragia in cases with placenta previa. Euro J Obstet Gynecol and Reprod Biol 167:167-170.
Indexed at, Google Scholar, Crossref
- Alkış, İsmet (2015) The fertility sparing management of postpartum haemorrhage: A series of 47 cases of Bakri balloon tamponade. Taiwaneses J Obstet Gynecol 54: 232-235.
Indexed at, Google Scholar, Crossref
- Wang, Dongyu (2018) Early usage of Bakri postpartum balloon in the management of postpartum hemorrhage: a large prospective, observational multicenter clinical study in South China. J Perinat Med 46: 649-656.
Indexed at, Google Scholar, Crossref
- Brown, Haywood (2016) The Bakri tamponade balloon as an adjunct treatment for refractory postpartum hemorragia. Int J Gynaecol Obstet 135: 276-280.
Indexed at, Google Scholar, Crossref
- Darwish, Atef M (2018) "Bakri balloon versus condom-loaded Foley’s catheter for treatment of atonic postpartum hemorrhage secondary to vaginal delivery: a randomized controlled trial." J Matern-Fetal Neonatal Med 31: 747-753.
Indexed at, Google Scholar, Crossref
- Guo, Yuna (2018) Intrauterine Bakri balloon and vaginal tamponade combined with abdominal compression for the management of postpartum haemorrhage. J Obstet Gynecol Canada 40: 561-565.
Indexed at, Google Scholar, Crossref
- Lo, Anderson (2017) The impact of Bakri balloon tamponade on the rate of postpartum hysterectomy for uterine atony. J Matern-Fetal Neonatal Med 30: 1163-1166.
Indexed at, Google Scholar, Crossref
- Maher, Mohammad Ahmed, Ahmed Abdelaziz (2017) Comparison between two management protocols for postpartum hemorragia during cesarean section in placenta previa: Balloon protocol versus non‐balloon protocol. J Obstet Gynecol Res 43:447-455.
Indexed at, Google Scholar, Crossref
- Soyama, Hiroaki (2017) Effect of routine rapid insertion of Bakri balloon tamponade on reducing hemorrhage from placenta previa during and after cesarean section. Arch Gynecol Obstet 296:469-474.
Indexed at, Google Scholar, Crossref
- Pillarisetty, Leela Sharath (2019) Postpartum Hemorragia: Use of Bakri Balloon During Cesarean Delivery, a Case Report and Review. J Clin Obstet Gynecol 8: 57-61.
Google Scholar
- de Jesús Ortega-Castillo, Verónica María, Salvador Espino, and Tomás Herrerías-Canedo (2013)"Control of obstetric haemorrhage with the Bakri balloon." Gynecology and Obstetrics of Mexico 81: 435-439.
Google Scholar
- Grange, Joséphine (2018) Predictors of failed intrauterine balloon tamponade for persistent postpartum haemorrhage after vaginal delivery. PLoS One 13: e0206663.
Indexed at, Google Scholar, Crossref
- Nagai S, Kobayashi H, Nagata T, Hiwatashi S, Kawamura T et al. (2016) Clinical Usefulness of Bakri Balloon Tamponade in the Treatment of Massive Postpartum Uterine Hemorragia. Kurume Med J 62:17-21.
Indexed at, Google Scholar, Crossref
- Çetin, Berna Aslan (2019) Comparing success rates of the Hayman compression suture and the Bakri balloon tamponade. J Matern-Fetal Neonatal Med 32: 3034-3038.
Indexed at, Google Scholar, Crossref
- Kadioglu, Berrin Goktug, Esra Cinar Tanriverdi, Ayse Nur Aksoy (2016) Balloon tamponade in the management of postpartum hemorrhage: three years of experience in a single center. Open J Obstet Gynaecol 6:698-704.
Indexed at, Google Scholar, Crossref
- Pala, Şehmus (2018) Comparison of results of Bakri balloon tamponade and caesarean hysterectomy in management of placenta accreta and increta: a retrospective study. J Obstet Gynaecol 38:194-199.
Indexed at, Google Scholar, Crossref
- Suarez S, Conde-Agudelo A, Borovac-Pinheiro A, Suarez-Rebling D, Eckardt M et al. (2020) Uterine balloon tamponade for the treatment of postpartum hemorrhage: a systematic review and meta-analysis. Am J Obstet Gynecol 222:293.e1-293.e52.
Indexed at, Google Scholar, Crossref
- Said Ali A, Faraag E, Mohammed M, Elmarghany Z, Helaly M et al. (2021) The safety and effectiveness of Bakri balloon in the management of postpartum hemorrhage: a systematic review. J Matern Fetal Neonatal Med 34:300-307.
Indexed at, Google Scholar, Crossref
- Kondoh E, Chigusa Y, Ueda A, Mogami H, Mandai M (2019) Novel intrauterine balloon tamponade systems for postpartum hemorrhage. Acta Obstet Gynecol Scand 98:1612-1617.
Indexed at, Google Scholar, Crossref
- Soyama, Hiroaki (2019) Analysis of prophylactic Bakri balloon tamponade failure in patients with placenta previa. Taiwan J Obstet Gynecol 58:159-163.
Indexed at, Google Scholar, Crossref
- Rocher G (2019) Massive hemoperitoneum due to uterine perforation by the Bakri Balloon, during the treatment of postpartum hemorrhage. J Gynecol Obstet Hum Reprod 48:75-76.
Indexed at, Google Scholar, Crossref
- Kaya, Baris (2016) Which uterine sparing technique should be used for uterine atony during cesarean section? The Bakri balloon or the B-Lynch suture?. Arch Gynecol Obstet 294:511-517.
Indexed at, Google Scholar, Crossref
- Dorkham MC, Epee-Bekima MJ, Sylvester HC, White SW (2021) Experience of Bakri balloon tamponade at a single tertiary centre: a retrospectiva case series. J Obstet Gynaecol 41:854-859.
Indexed at, Google Scholar, Crossref
Citation: Guerrero CCG, Mendoza JCA,
Mercado LPN, Alarcon ACM, Golon JAH, et
al. (2022) Bakri Balloon as Last Non-Surgical
Therapeutic Action to Control Postpartum
Hemorrhage Health Sci J. Vol. 16 No. S7: 944.