Case Report - (2022) Volume 16, Issue 2
Behavior of Necrotizing Enterocolitis in new borns in a Neonatal Intensive Care Unit Monteria, Colombia, between 2015 and 2018
Lucia Margarita Guzman Soto1*,
Angelica Maria de los Reyes Aldana2,
Ximena Lucia Herazo Ortega3,
Asterio Andres Herazo Ortega4,
Oriana Liz Pineda Espitia5,
Mary Carmen Diaz Bermudez6,
Rafael Chica Polo7,
Hector Rafael Pineda Roman8 and
Carlos Mauricio Vergara Lobo9
1Paediatrician, Universidad del Sinu, Colombia
2Neonatologist, Universidad de Buenos Aires, Argentina
3General Physician, Universidad Libre de Barranquilla, Colombia
4General Physician, Universidad del Sinu, Colombia
5Medical Student, Universidad del Sinu, Colombia
6General Physician, Universidad del Norte, Colombia
7Neonatologist, Universidad de Buenos Aires, Argentina
8Neonatologist, Universidad de Buenos Aires, Argentina
9Pediatric Infectologist, Universidad de Buenos Aires, Argentina
*Correspondence:
Lucia Margarita Guzman Soto,
Health Psychology, Royal Victoria Infirmary, Newcastle upon Tyne, NE1,
Colombia,
Received: 29-Dec-2021, Manuscript No. iphsj-21-12200;
Editor assigned: 31-Dec-2021, Pre QC No. Preqc No.12200;
Reviewed: 07-Feb-2022, QC No. QC No.12200;
Revised: 12-Feb-2022, Manuscript No. iphsj-21-12200 (R);
Published:
21-Feb-2022, DOI: 10.36648/1791-809X.16.2.913
Abstract
Introduction: Necrotizing enterocolitis (NEC) is a frequent pathology in newborns (NBs) that generally require attention in the neonatal intensive care unit (NICU). There are few data about the incidence in Latin America and Colombia since it is difficult to establish a timely diagnosis and hospital records do not contain accurate information. The following descriptive, retrospective and quantitative study analyzes the incidence, clinical characteristics, diagnostic methods and treatment of necrotizing enterocolitis in newborns from a neonatal intensive care unit of a clinic in the city of Montería.
Objective: To determine the incidence, clinical characteristics, diagnostic methods and treatment of newborns with NEC hospitalized in the NICU in order to provide therapeutic recommendations.
Material and methods: A descriptive, retrospective study, with a quantitative approach, including 54 medical records of neonates with NEC born in a private clinic in the city of Montería, Colombia and admitted to the NICU between June 2015 and December 2018. The statistical analysis was performed with SPSS and R Studio software.
Results: The global incidence was 4.4%. 77.8% were premature and 22.2% were fullterm newborns. 66.7% developed NEC between the 1st to the 5th day of life. 92.5% of the cases required medical treatment and 4.5% had surgical intervention, the overall mortality was 22.2%.
Conclusions: A history of hypertensive disorder of pregnancy was prevalent in NBs with NEC. There was a higher incidence than that reported in the literature of affected term newborns. The use of empirical antibiotics for a long time was identified as a risk factor. A specific feeding protocol should be established according to the individual risk factors and the perinatal characteristics of the newborn that includes the use of breast milk as the first option.
Keywords
Newborn; necrotizing enterocolitis; neonatal intensive care unit.
Introduction
Necrotizing enterocolitis is a common pathology in newborns that generally requires care in the neonatal intensive care unit [1]. It is the most frequent cause of gastrointestinal disturbance, becoming a medical-surgical emergency, in which adequate and timely treatment can reduce the need for surgery, complications, and fatality [2]. In the 90s until 2000, an estimated mortality for NEC was reported internationally between 5 and 30% depending on the country and level of complexity of the NICU, and can reach up to 100% in newborns under 700 gr and approximately 45% in RN between 750 and 1000 gr [3,4]. There are few data on the incidence of NEC in Latin America and Colombia, given that it is difficult to establish the diagnosis in a timely manner and precise information records are lacking in most hospital centers. For the year 2010 in Colombia, a study was carried out in the city of Cali where 32 newborns who were diagnosed with NEC were included, finding an incidence of 2% for this disease [5]. It is possible that in our environment these figures are higher due to the high rates of maternal and perinatal mortality that are registered in the department of Córdoba and that are linked to poor prenatal control, a risk factor for premature birth and therefore for NEC [6].
Methodology
The following retrospective descriptive study, with a quantitative approach, was carried out during the period from June 2015 to December 2018, in which 11,571 births were attended; of which 1,234 required care in the neonatal intensive care unit and these 54 patients were diagnosed with NEC, whose medical records were entered into the study.
NEC was defined as 1) two or more of the following signs: abdominal distension, abdominal pain on palpation, occult or macroscopic blood in the stool, pathological gastric residue: boring or bilious, abdominal mass, erythema of the abdominal wall.
2) One or more of the following signs on the abdominal radiograph: asymmetric distention of the intestinal loops, edema of the intestinal wall, pneumatises gas in the portal system or pneumoperitoneum.
The information collected was entered into a Microsoft Excel database with the variables of interest in accordance with the study objectives. A descriptive and inferential statistical analysis was carried out with the SPSS and R Studio software.
Results
Between June 2015 and December 2018, 11,571 births were attended; of these, 1,234 were admitted to the neonatal intensive care unit, of which 4.4% had a diagnosis of NEC, the incidence rate was 4.6 per 1000 live new-borns at the institution. Regarding sex, there was a 1:1 relationship. The presentation of the disease occurred between 1 to 5 days of birth in 66.7% of the cases.
The Apgar score> 7 at minute was recorded in 48% of the NBs. 11.1% had some degree of asphyxia evidenced by Apgar less than or equal to 6. The reason for admission to the NICU was respiratory distress in 72.2% of the cases, followed by suspected NEC in 18.5% of the cases, as shown in Table 1.
| Characteristic |
% |
| Male gender |
50,0 |
| Emergency cesarean delivery |
81,5 |
| Average age of the mother |
25 years |
| Mother with hypertensive disorder of pregnancy |
46,3 |
| Average gestational age |
33,4 |
| Birth weight 1500 -2499 gr |
46,3 |
| Apgar < 6 |
11,1 |
| Apgar > 7 |
89 |
| Reason for admission: respiratory distress |
72,2 |
| Average age days of life at the on set of symptoms |
4,6 |
Table 1: Characteristics of the study population.
Source: Database.
Maternal age ranged from 13 to 40 years, with an average of 25 years. 81.5% of the children were born by emergency caesarean section and the most frequently encountered maternal disease was hypertensive disorder of pregnancy with 46.3%, followed by premature membrane rupture greater than 18 hours with 16.7%. When crossing the variable hypertensive disorder of pregnancy with gestational age and birth weight, it was found that there was a statistically significant association between these variables, with a value of p-0.05, evidencing the association between the mother's hypertensive disorders with the prematurity of the baby. New-born with NEC.
According to the gestational age at birth, a higher proportion of 29.7% cases of NEC is observed in new-borns with a gestational age between 34 and 36 weeks. 22.2% of the cases corresponded to term neonates. The average gestational age was 33.4 weeks.
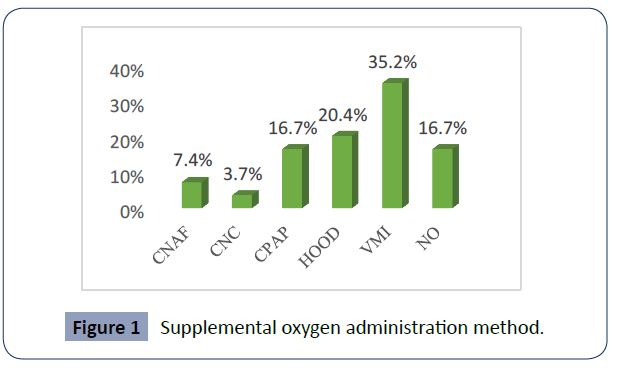
Upon admission to the NICU, 35.2% of the neonate’s required supplemental oxygen for invasive mechanical ventilation, 16.7% were admitted to non-invasive ventilation by CPAP mode. Figure 1 shows the percentages corresponding to the supplementary oxygen administration method that these patients received (Figure 1).
Figure 1 Supplemental oxygen administration method.
CNAF: high-flow nasal cannula, CNC: conventional nasal cannula, CPAP: continuous positive airway pressure, HOOD: cephalic chamber, IMV: invasive mechanical ventilation)
Source: Database.
The empirical antibiotics most widely used at admission were Ampicillin plus Gentamicin in 74.1%. In these children, antibiotic use was indicated at the beginning of care in the NICU due to the identification of risk factors for sepsis. 24.1% of the newborns did not require antibiotic therapy upon admission. It was identified that at the time of the diagnosis of NEC, 52.1% of the NBs had 4 to 7 days of antibiotic management for sepsis with an average of 5 days.
Regarding the feeding patterns, 61.1% were fasting and 38.8% of them received some type of milk at the time of the onset of clinical manifestations. 72.2% received formula milk while only 27.8% received breast milk. The infants had a mean fasting time of 6.7 days, with a range of 29 days and a standard deviation of 6 days. A statistically significant association was found between the fasting days of the children with respect to their gestational age at birth with a value of p-0.05. Of all those who were fed, 50% received a low volume of milk between 10 - 19 cc / kg / day at the time of suspicion of NEC.
The most frequent clinical manifestations were abdominal distention in 88.9%, and pathological gastric residue in 70.4%, while vomiting and bloody stools were manifested in 33.3% and 3.7%, respectively. For its part, the most frequent radiological manifestations were interase edema in 94.2% and dilation of intestinal loops in 81.1%, and Pneumatises and Pneumoperitoneum were presented in 5.8%.
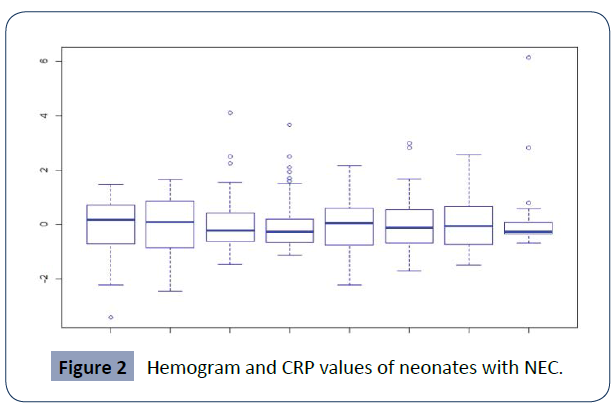
In the hemogram, it was found that the average value of hemoglobin was 13.5 g / dl, and the average hematocrit was 40.5%. Regarding leukocytes, 82.7% of the patients had leukocytes in the normal range, 7.7% had leukopenia, and 9.6% had leucocytosis above 30,000. Regarding platelets, 88.5% of the patients had platelets above 100,000, only 11.5% of the neonates had platelets, the mean platelet value was 209,076. The average of Monocytes was 9.9. 50% of the patients had CRP> 6, the average CRP was 9.8. As can be seen in graph 2. In turn, arterial blood gases showed that 38.9% of new-borns had acid-base balance and the most frequent disorder found was metabolic acidosis with 11.1%. Furthermore, 92.5% of the cases received medical management while 4.5% of the patients required surgical management (Figure 2).
Figure 2 Hemogram and CRP values of neonates with NEC.
Source: Database.
Hb: hemoglobin, Hcto: hematocrit, Plt: platelets, Leu: leukocytes, Neu: neutrophils, Lympho: lymphocytes, Mono: monocytes and CRP: quantitative C-reactive protein.
92.6% of the cases had antibiotic treatment, in 31.5% of the cases the initial antibiotic Ampicillin plus Gentamicin was continued, 22.2% were treated with Cefepime plus Amikacin and in 14.8% of the cases were started Ampicillin plus Gentamicin; the rest of the neonates received various antibiotics directed to the nature of the disease and the usual microbiota of the NICU (Table 2).
| Antibiotic |
N° |
% |
| Ampicillin Gentamicin (Initial Scheme) |
17 |
31,5 |
| Cefepime Amikacin |
12 |
22,2 |
| Ampicillin Gentamicin |
8 |
14,8 |
| Vancomycin Meropenem |
6 |
11,1 |
| Other antibiotics |
7 |
13,0 |
| NO |
4 |
7,4 |
| Total |
54 |
100,0 |
Table 2: Antibiotic therapy used in the treatment of neonates with NEC.
Source: Database.
An overall mortality of 22.2% was identified. In 2016, 3 out of 10 new-borns with NEC had died. An increase in cases of enter colitis was observed in 2018 compared to previous years, however, in 2018 out of 10 children with NEC 2 died.
Discussion
The incidence for NEC in this study was 4.4%, which is in accordance with that reported in the literature, where figures are estimated between 1 and 15% 4 currently, an increase in NEC cases in full-term new-borns has been reported in the last decade. In this study, full-term new-borns with necrotizing enter colitis are 22.2% of the cases, surpassing the reports in the literature where there is an incidence in this group of 10 to 15%. [7, 8]
Advances in knowledge about the genetic predisposition of newborns [9]. The alteration in the intestinal microbiota [10] and pro-inflammatory mediators [11] has contributed to a better understanding of the pathophysiology in NEC. It is also known that the low Apgar score at birth [12]. The hypertensive disorder of pregnancy [13]. The administration of high concentrations of oxygen, the use of formula milk and the empirical postnatal use of antibiotics [14, 15]. Are factors contributors to the development of necrotizing enter colitis. The literature describes the appearance of NEC with transfusions of blood products [16]. However, in this study no relationship was found between blood transfusions and the appearance of necrotizing enters colitis.
Formula milk was widely used in the new-borns in the present study, which has been identified as a risk factor for NEC, [17]. In contrast, breast milk reduces the incidence of necrotizing enter colitis even in neonates with extreme prematurity [18]. In the absence of milk from the same mother, the advantage of administering donor breast milk without great risks and with multiple benefits has been described [19].
It is currently known that starting enteral feeding in new-borns early does not increase the risk of NEC or mortality and represents great advantages for these patients [20]. However, in this study the average start of feeding was at 6.7 days old with low volumes of 10 to 19 cc / kg / day. The standardization of a feeding protocol that takes into account gestational age, birth weight and the risk factors of the new-born has shown great utility in the hospital centers where it is implemented [21, 22].
The disease was early onset with an average of 4.6 days of life at the time of diagnosis. There are world epidemiology reports where the age of onset is later in most cases between 8 and 10 days of life.
In this study, the most frequent symptoms were pathological gastric residual, abdominal distension, vomiting and, ultimately, stool, which can be initially specific and confused with sepsis in some cases. The least frequent clinical sign found was blood in the stools, despite the fact that it is a predominant sign in the literature.
Patients who require surgical management have higher mortality and even have higher morbidity during the first year, which was related to surgery for NEC [23]. The need for surgical management in new-borns with necrotizing enter colitis is variable; it is reported between 20% and 40% [24]. The report of surgical intervention in the present work was 4.6%, which shows to be below that reported in the publications; there are probably failures in the identification of surgical management.
The mortality of this entity is variable; there are centers of high international complexity where mortality of 11.4% is reported. In Colombia, a mortality rate for 2011 was reported in a study carried out in Cali of 37.5%. In this study, an overall mortality of 22.2% is reported.
Conclusions
Necrotizing enter colitis is of great impact and deserves importance in neonatal intensive care units due to its high mortality and comorbidity. The diagnosis of the disease must be predominantly clinical since the laboratory tests in most cases are normal or nonspecific. Strict radiological follow-up should be carried out to identify possible cases that require early surgical management and thus avoid postponing the intervention once the hemodynamic compromise is reached, given the progression of the disease. Despite not being widely used, abdominal ultrasound can be useful in the follow-up of new-borns.
It is necessary to implement a specific feeding protocol for each new-born taking into account risk factors, gestational age and birth weight to help reduce the incidence of NEC. Breast milk is an important, inexpensive and irreplaceable tool and should be included in NEC prevention strategies in the NICU whenever it is available. More local and national studies should be carried out to establish precise and effective strategies to reduce its incidence, which has been increasing over the years.
REFERENCES
- Neu J, Walker AW (2011) Necrotizing enterocolitis. N England J Med 364:255-264.
Indexed at, Google Scholar, Crossref
- Guzman J, Ruiz D (2012) Prevención de la enterocolitis necrotizante en el recién nacido. An Pediatr Contin 10:295-297.
Google Scholar
- Méndez FA, Bancalari M, Ernst EI (2000) Enterocolitis necrotizante: Experiencia de 15 años. Rev Chil Pediatr 71: 390-97.
Indexed at, Google Scholar, Crossref
- Tamayo P Maria, Arango R Maria, Tamayo M Carolina (2006) Fisiopatología y factores de riesgo para el desarrollo de enterocolitis necrosante en neonatos menores de 1.500 gr. Iatreia, diciembre 19:356-367.
Indexed at, Google Scholar, Crossref
- Torres, Javier (2011) Características de recién nacidos con enterocolitis necrotizante en un hospital universitario de tercer nivel en Colombia. Colomb Med Mayo 42:1-8.
Indexed at, Google Scholar, Crossref
- Sharma R, Hudak ML (2013) A clinical perspective of necrotizing enterocolitis: Past, present, and future. Clin Perinatal 40:27-51.
Indexed at, Google Scholar, Crossref
- Gasque-Góngora JJ (2015) Revisión y actualización de enterocolitis necrosante. Rev Mex Pediatr 82:175-185.
Indexed at, Google Scholar, Crossref
- Cuna A, George L, Sampath V (2018) Genetic predisposition to necrotizing enterocolitis in premature infants: current knowledge, challenges, and future directions, Seminars in Fetal and Neonatal Medicine.
Indexed at, Google Scholar, Crossref
- Mark A Underwood (2018) Probiotics and the prevention of necrotizing Enterocolitis. J Pediatr Surg 54:405-412.
Google Scholar, Crossref
- Michel Hosny (2017) Updating on gut microbiota and its relationship with the occurrence of necrotizing enterocolitis. Hum Microbiome J 4:14-19.
Indexed at, Google Scholar, Crossref
- Young CM, Kingma SD, Neu J (2011) Ischemia-reperfusion and neonatal intestinal injury. J Pediatr 158:e25-e28.
Indexed at, Google Scholar, Crossref
- Ju-young Lee, Kyo-Hoon Park, Ahra Kim, Hye-Ran Yang (2012) “Maternal preeclampsia is associated with increased risk of necrotizing enterocolitis in preterm infants. Early Human Dev 88:893-898.
Indexed at, Google Scholar, Crossref
- Ayasree Nair, Longendyke Rachel, Lakshminrusimha Satyan (2018) Necrotizing Enterocolitis in Moderate Preterm Infants. Biomed Res Int 1-6.
Indexed at, Google Scholar, Crossref
- Kim C, Claud E (2018) Necrotizing Enterocolitis Pathophysiology How Microbiome Data Alter Our Understanding. Clin Perinatol
Indexed at, Google Scholar, Crossref
- Jonathan Blau, Johanna M Calo, Donna Dozor, Millicent Sutton, Gad Alpan (2011) Transfusion-related acute gut injury: Necrotizing enterocolitis in very low birth weight neonates after packed red blood cell transfusión J Pediatr 158:403-409.
Indexed at, Google Scholar, Crossref
- Tian Qian (2017) Necrotizing enterocolitis in low birth weight infants in China: Mortality risk factors expressed by birth weight categories. Pediat Neonatol 58:509-515.
Indexed at, Google Scholar, Crossref
- Swati Murthy (2018) Low rate of necrotizing enterocolitis in extremely low birth weight infants using a hospital-based preterm milk bank Am J Perinatol Springer Nature America.
Indexed at, Google Scholar, Crossref
- Quigley M, McGuire W (2014) Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst Rev: CD002971.
Indexed at, Google Scholar, Crossref
- Perez Luis A (2011) Incidencia de enterocolitis necrosante en niños prematuros. Biomédica 31:485-91.
Indexed at, Google Scholar, Crossref
- Barr Priscilla (2018) Standardized Nutrition Protocol for Very Low-Birth-Weight Infants Resulted in Less Use of Parenteral Nutrition and Associated Complications, Better Growth, and Lower Rates of Necrotizing Enterocolitis. J Parenter Enteral Nutr 11:1-10.
Indexed at, Google Scholar, Crossref
- Sánchez Tamayo (2016) Reducción de la enterocolitis necrosante tras la introducción de un protocolo de alimentación enteralbasado en la evidencia en recién nacidos de muy bajo peso. An Pediatr
Indexed at, Google Scholar, Crossref
- Heladia Garcia (2012) Cirugía en enterocolitis necrotizante en niños supervivencia y mortalidad. Rev Med Inst Mex Seguro Soc 50:427-436.
Indexed at, Google Scholar, Crossref
- García Gonzáleza, Miriam Pita Fernández, Salvador Caramés Bouzána, (2017) characterísticas poblacionales de neonatos afectos de enterocolitis necrosante en un centro terciario en los últimos 12 años. Cirugía y Cirujanos Octubre 85:411-418.
Indexed at, Google Scholar, Crossref
- Escalona P (2018) enterocolitis necrotizante. Revista médica Sinergia abril 3.
Google Scholar
Citation: Citation: Guzmán Soto LM, de los Reyes Aldana AM, Herazo Ortega XL, Herazo Ortega AA, Pineda Espitia OL, et al. (2022) Behavior of Necrotizing Enterocolitis in new-borns in a Neonatal Intensive Care Unit Monteria, Colombia, between 2015 and 2018. Health Sci J. Vol. 16 No. 2: 913.