Perspective - (2024) Volume 14, Issue 4
Beta Blockers: A Pharmacological Perspective
Katarzyna Bilska*
Department of Pharmacology, University of Rhenden, Shendi, Sudan
*Correspondence:
Katarzyna Bilska, Department of Pharmacology, University of Rhenden, Shendi,
Sudan,
Email:
Received: 02-Jul-2024, Manuscript No. IPFT-24-14977;
Editor assigned: 05-Jul-2024, Pre QC No. IPFT-24-14977 (PQ);
Reviewed: 19-Jul-2024, QC No. IPFT-24-14977;
Revised: 01-Aug-2024, Manuscript No. IPFT-24-14977 (R);
Published:
29-Aug-2024
Introduction
Beta blockers, also known as beta-adrenergic blocking agents
are a class of medications widely used in clinical practice to
manage various cardiovascular and non-cardiovascular
conditions. These drugs exert their effects by blocking the action
of beta-adrenergic receptors, which are primarily found in the
heart, kidneys, blood vessels and other tissues. This
pharmacological intervention results in diverse therapeutic
benefits and considerations across different patient populations.
Description
Mechanism of action
Beta blockers function by competitively antagonizing betaadrenergic
receptors, specifically the beta-1 (β1) and beta-2 (β2)
receptors. Beta-1 receptors are predominantly located in the
heart and kidneys, whereas beta-2 receptors are found in
vascular smooth muscle, bronchial smooth muscle and liver cells.
By blocking these receptors, beta blockers inhibit the binding of
endogenous catecholamines (e.g., adrenaline and
noradrenaline), which are responsible for stimulating these
receptors under normal physiological conditions.
Beta-1 receptor blockade in the heart leads to decreased
heart rate (negative chronotropy), reduced myocardial
contractility (negative inotropy) and decreased cardiac output.
These effects are beneficial in conditions such as hypertension,
angina pectoris and congestive heart failure, where reducing the
workload and oxygen demand of the heart can improve
symptoms and outcomes.
Beta-2 receptor blockade in the lungs and peripheral
vasculature can lead to adverse effects such as
bronchoconstriction and peripheral vasoconstriction. Therefore,
beta blockers are generally avoided or used cautiously in
patients with asthma or Chronic Obstructive Pulmonary Disease
(COPD) due to the risk of exacerbating bronchospasm.
Cardiovascular conditions
Hypertension: Beta blockers are effective in reducing blood
pressure by decreasing cardiac output and inhibiting renin
release from the kidneys.
Angina pectoris: By reducing myocardial oxygen demand,
beta blockers can alleviate angina symptoms and improve
exercise tolerance.
Arrhythmias: They are used to manage certain types of
arrhythmias by stabilizing the electrical activity of the heart.
Heart failure: Selective beta blockers improve symptoms and
reduce mortality in patients with chronic heart failure.
Hypertension: Beta blockers reduce blood pressure by
decreasing cardiac output and suppressing renin release.
Angina: By reducing myocardial oxygen demand, beta
blockers alleviate angina symptoms.
Non-cardiovascular conditions
Migraine prophylaxis: Propranolol, a non-selective beta
blocker, is used to reduce the frequency and severity of
migraines.
Essential tremor: Beta blockers like propranolol are effective
in controlling tremors in patients with essential tremor.
Glaucoma: Topical beta blockers can reduce intraocular
pressure in patients with glaucoma by decreasing aqueous
humor production.
Pharmacokinetics
Beta blockers exhibit varying pharmacokinetic profiles,
including absorption, distribution, metabolism and excretion.
These properties influence their onset of action, duration of
effect and dosing regimens. For instance, lipophilic beta blockers
tend to have better tissue penetration and longer durations of
action compared to hydrophilic ones.
Commonly used beta blockers
Metoprolol: A selective beta-1 blocker commonly prescribed
for hypertension and angina.
Propranolol: A non-selective beta blocker used in treating
hypertension, arrhythmias and migraine prophylaxis.
Atenolol: Another selective beta-1 blocker often used in
hypertension management.
Carvedilol: A non-selective beta blocker with alpha-blocking
activity used in heart failure and hypertension.
Adverse effects and considerations
While beta blockers are generally well-tolerated, they can
cause several adverse effects due to their mechanism of action.
Common side effects include fatigue, dizziness, bradycardia
(slow heart rate) and hypotension (low blood pressure). In
patients with diabetes, beta blockers can mask signs of
hypoglycemia (low blood sugar) by attenuating sympathetic
responses.
Bradycardia: Excessive heart rate reduction.
Hypotension: Particularly in patients with pre-existing low
blood pressure.
Bronchoconstriction: Non-selective beta blockers can
exacerbate respiratory conditions like asthma.
Fatigue and depression: Central nervous system effects that
may impact quality of life.
Special precautions are necessary when using beta blockers in
specific patient populations
Pregnancy and lactation: Beta blockers should be used
cautiously during pregnancy and breastfeeding, as they can
cross the placenta and enter breast milk.
Elderly patients: Due to age-related changes in
pharmacokinetics and pharmacodynamics, lower initial doses
and gradual titration are recommended.
Renal and hepatic impairment: Dose adjustments may be
necessary in patients with impaired renal or hepatic function to
avoid drug accumulation and toxicity.
Future directions and conclusion
The field of beta blocker pharmacology continues to evolve
with ongoing research into novel agents and applications. Future
directions include exploring beta blocker therapy in conditions
such as Post-Traumatic Stress Disorder (PTSD), perioperative
management and neuroprotection in neurodegenerative
diseases.
Conclusion
In conclusion, beta blockers represent a cornerstone in the
management of cardiovascular and certain non-cardiovascular
conditions. Their diverse pharmacological effects, clinical
applications and considerations underscore their importance in
modern medicine. By understanding their mechanisms of action
and optimizing their use based on individual patient
characteristics, healthcare providers can maximize therapeutic
efficacy while minimizing potential adverse effects.
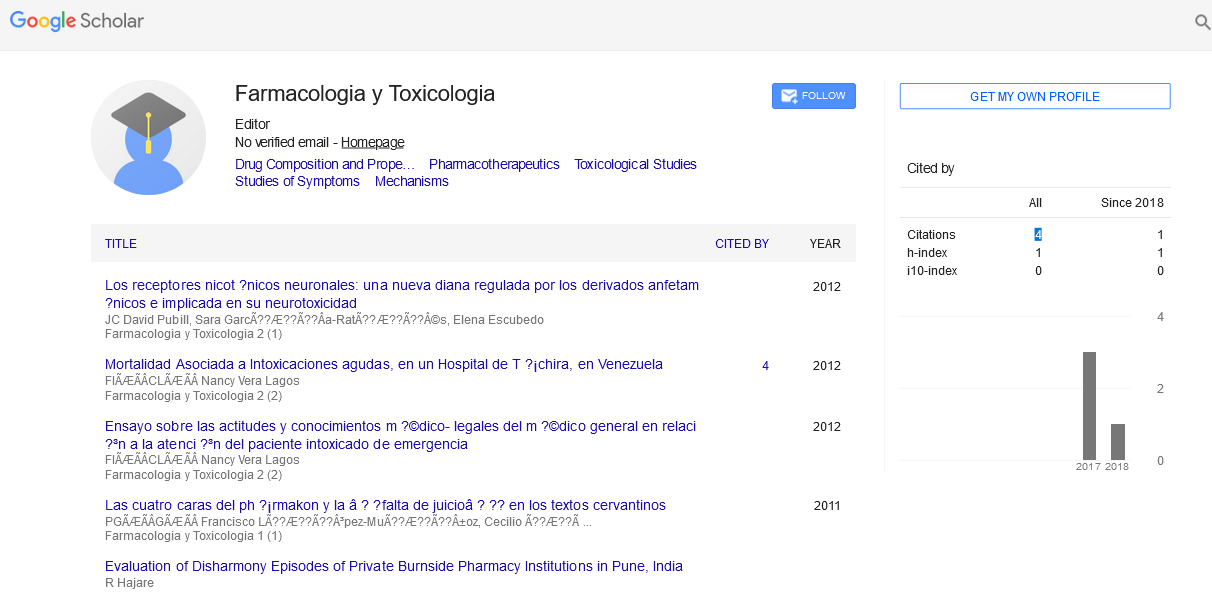
Citation: Bilska K (2024) Beta Blockers: A Pharmacological Perspective. Farmacologia Toxicologia, Vol.14 No.4: 040