Vicente Medrano Martínez*
Department of Neurology, Hospital General Universitario Virgen de La Salud de Elda, Spain
*Corresponding Author:
Dr. Vicente Medrano Martínez
Department of Neurology, Hospital General
Universitario Virgen de La Salud de Elda
Carretera Elda-Sax S/N; CP: 03600 Elda, Alicante, Spain
Tel: 657579812
E-mail: vmedrano714k@icloud.com
Received Date: February 25, 2018 Accepted Date: March 23, 2018 Published Date: March 26, 2018
Citation: Martínez VM (2018). Cerebelous Pseudotumor due to a Localized Vasculitis as First Presentation of Sjögren Syndrome. J Neurol Neurosci Vol.9 No.2:253. doi: 10.21767/2171-6625.1000253
Keywords
Central nervous isolated angiitis; Pseudotumoral brain lesion; Auto-immune disease; Sjögren's syndrome; Vasculitis; Inflammatory pseudotumour
Introduction
Sjögren syndrome is a systemic chronic inflammatory disorder characterized by lymphocytic infiltrates in exocrine organs. It is a systemic autoimmune disease characterized by lymphocytic infiltration in the exocrine glands mainly salivary and lacrimal glands. This disease can occur with extraglandular manifestations that include the CNS and the peripheral nervous system (PNS). We present the first case published in the literature confirmed with brain biopsy, secondary to a cerebellar pseudotumoral lesion due to localized lymphocytic vasculitis as the first manifestation of a Sjögren's Syndrome.
Case Report
A 54-year-old woman with no clinical history of interest who consulted for instability of gait, nausea and oppressive holocranial headache, which had appeared just a few weeks before. In the initial anamnesis, she did not describe any other symptom of neurological dysfunction. The neurological exam showed a patient conscious and oriented, and no papilledema was present in funduscopia. The gait was markedly ataxic, with clearly unstable tandem, without other neurological alterations.
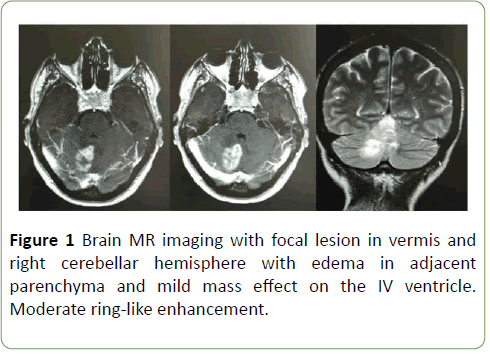
No other anomalies were detected in general physical examination. Complementary tests: A cranial computerized tomography (CT) scan showed a single, hypodense, heterogeneous space-occupying lesion located at the level of the right cerebellar region, which caused a mild mass effect on the fourth ventricle. Magnetic resonance imaging (MRI) confirms the presence of a space-occupying lesion at the right cerebellar region with ring-like contrast enhancement, reported as a possible metastatic lesion versus primary neoplasm of the central nervous system (Figure 1).
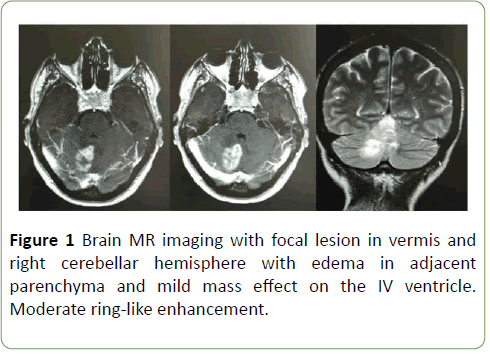
Figure 1: Brain MR imaging with focal lesion in vermis and right cerebellar hemisphere with edema in adjacent parenchyma and mild mass effect on the IV ventricle. Moderate ring-like enhancement.
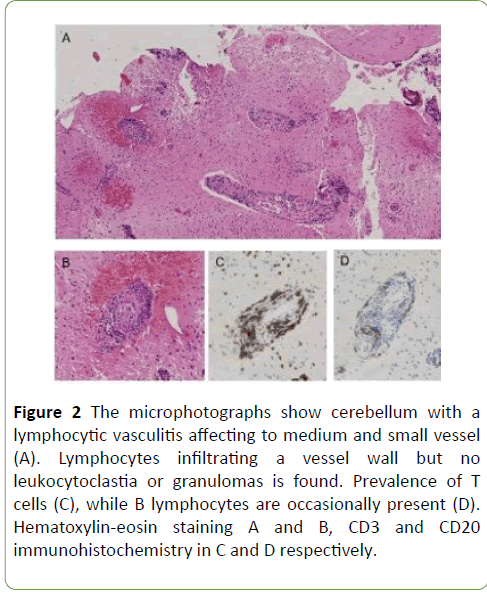
Blood tests did not detect significant alterations. In the cervico-thoraco-abdomino-pelvic CT scan in search of a primary lesion no abnormalities were detected. Brain spectroscopy discards neoplastic origin of the lesion and suggests the presence of an inflammatory or infectious process. At the beginning, an inconclusive stereotactic biopsy of cerebellar lesion was performed. A second biopsy of the pseudotumoral was performed and the sample was sent to a Reference Neuropathology Unit. The report describes histopathological changes compatible with a localized lymphocytic vasculitis of medium and small vessel of the central nervous system (CNS) (Figure 2). A complete study was carried out to discard systemic vasculitis.
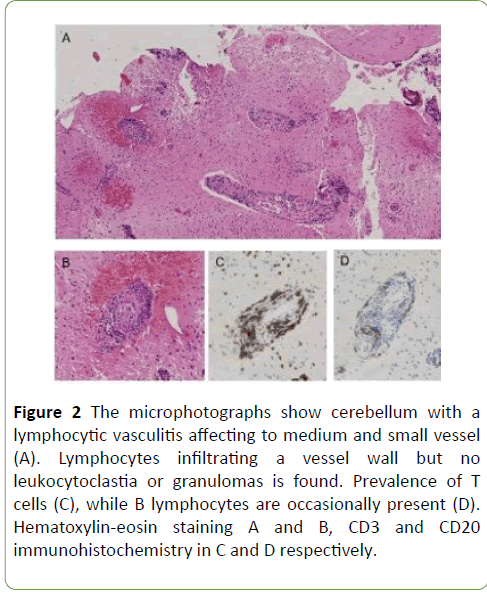
Figure 2: The microphotographs show cerebellum with a lymphocytic vasculitis affecting to medium and small vessel (A). Lymphocytes infiltrating a vessel wall but no leukocytoclastia or granulomas is found. Prevalence of T cells (C), while B lymphocytes are occasionally present (D). Hematoxylin-eosin staining A and B, CD3 and CD20 immunohistochemistry in C and D respectively.
The results showed positive ANA test (1/320) with a mitochondrial pattern and a positive ENA Ro at a titre of 127 AU/ml. These analytical outcomes guided the diagnosis toward a SS, so that a Schrimer test is performed, although the result was negative. Finally, the study of a biopsy of a minor salivary gland detected an inflammatory process with lymphocyte aggregates compatible with Sjögren's disease. With the pathological diagnosis of isolated vasculitis at the cerebellar level a treatment course with 1 g of intravenous methylprednisolone for 5 days. After confirming systemic involvement by Sjögren Syndrome (SS), according to the criteria of the American College of Rheumatology, treatment with the administration of intravenous cyclophosphamide in monthly boluses of 1 gram for a year was started. The patient remains asymptomatic at the present time, with complete resolution of her cerebellar lesion in the last follow-up control by brain MRI.
Discussion
The neuroimaging performed in our patient detects a unique space-occupying lesion in the cerebellum, suggesting a primary tumor or a metastatic lesion. Indeed, the differential diagnosis in the context of a single space-occupying lesion includes the presence of metastases, glioma, lymphoma, but also, abscesses, progressive multifocal leukoencephalopathy, histiocytosis, adrenoleukodystrophy, vasculitis and other autoimmune and demyelinating diseases such as Baló- Marburg disease [1,2].
The cerebellar biopsy of the current case resulted in the diagnosis of isolated vasculitis of the CNS, which is a rare entity that affects the brain and spinal cord with just over 500 cases described in the literature [3]. Finally, after performing a thorough blood test, the presence of ENA Ro positive antibodies was detected, in the absence of another relevant systemic symptoms. With the suspect of a systemic SS, a minor salivary gland biopsy was performed, and the pathological report confirmed Sjögren's disease. Because the patient did not present typical SS symptoms, the definitive diagnosis was an important challenge, since the presence of isolated nodular lesions in the form of pseudotumor as the first manifestation of Sjögren's disease is very uncommon.
Sjögren's disease is a systemic autoimmune disease characterized by lymphocytic infiltration in the exocrine glands mainly salivary and lacrimal glands. This disease can occur with extraglandular manifestations that include the CNS and the peripheral nervous system (PNS). Peripheral neuropathy is more frequent, consisting of axonal injury of sensory and autonomic nerves, small fiber and multiple mononeuritis neuropathy due to small vessel vasculitis. The involvement of CNS may be as diffuse or localized lesions, being associated with increased extraglandular involvement and presence of autoantibodies. Two pathogenetic factors are considered to be the cause of CNS disease in primary SS. The first is the direct mononuclear cell infiltration. The second is vasculitis, which is based on peripheral vasculitis, proven at biopsy, and CNS findings [4].
The prevalence of CNS participation in primary Sjögren's disease is unknown, some studies showed a prevalence of CNS involvement in the range of 3,6-10% [5]. The diagnosis of the extension of this disease to the CNS is performed by Magnetic Resonance, in a compatible clinical context. The most common neuroimaging findings are those related to signal changes such as hyperintensity in T2 sequence of subcortical and periventricular white matter [6]. Other less frequent findings are lesions in the gray matter of the basal ganglia and in the corpus callosum. Although these lesions may be similar to those of patients with multiple sclerosis, they are usually smaller [7]. Hasiloglu ZI et al. in their report present a 35-yearold woman with primary Sjögren's syndrome with central nervous system vasculitic involvement diagnosed by digital subtraction angiography [8].
Conclusion
There are very few cases published in the literature about pseudotumor secondary to Sjögren's Syndrome. A similar case, published in 2008 by Sanahuja et al. [9], describes a spaceoccupying lesion in the right temporo-occipital region with demyelinating characteristics in a 50-year-old woman with arthralgia and oral dryness of one year of evolution. Three months later, a new tumor-like lesion with ring enhancement located in the right frontoparietal brain region appeared in this patient. Michel et al. [10] report the case of a woman with primary SS presenting with hemiparesis and Broca's aphasia secondary to a pseudotumoral lesion in the white matter of the corona radiata. These two articles together with the one published in 2014 by Sassi et al. [11], and the case of our patient show that a pseudotumoral injury at the brain level may be the first manifestation of SS. On the other hand, the clinical case that we present is the first description confirmed with a brain biopsy in a patient with a cerebellar pseudotumoral lesion secondary to a small and medial vessel vasculitis as the first manifestation of a Sjögren's Syndrome.
Disclosure of Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be considered as a potential conflict of interest.
22444
References
- Shiboski SC, Shiboski CH, Criswell LA, Baer A, Challacombe S, et al. (2012) American College of Rheumatology Classification Criteria for Sjögren’s Syndrome: A data-driven, expertconsensus approach in the Sjögren ÃŒÂÂÂÃÂs International Collaborative clinical alliance cohort. Arthritis Care Res 64: 475-487.
- George T (2016) Multifocal tumefactive demyelination mimicking intracranial neoplasm. J Clin Diagnostic Res 10: 10-11.
- Elliot IS (1993) Primary angiitis of the central nervous system: Unusual MR apperance. Autoimmunity Rev 12: 463-466.
- Méndez PC, Sangüesa GC, Fernández-Castro M, Andreu SJL (2013) Manifestaciones neurológicas del síndrome de Sjögren primario. Semin la Fund Española Reumatol. Elsevier 14: 80-85.
- Carvajal AG, Guellec D, Mariette X, Gottenberg JE, Dernis E, et al. (2016) Epidemiology of neurological manifestations in Sjögren’s syndrome: data from the French ASSESS Cohort. RMD Open 2: e000179.
- Morgen K, McFarland HF, Pillemer SR (2004) Central nervous system disease in primary Sjögren’s syndrome: The role of magnetic resonance imaging. Semin Arthritis Rheum 34: 623-630.
- García-Carrasco M, Ramos-Casals M, Rosas J, Pallarés L, Calvo-Alen J, et al. (2002) Primary Sjögren syndrome: clinical and immunologic disease patterns in a cohort of 400 patients. Medicine (Baltimore) 81: 270-280.
- Hasiloglu ZI, Albayram S, Tasmali K, Erer B, Selcuk H, et al. (2012) A case of primary Sjögren's syndrome presenting primarily with central nervous system vasculitic involvement. Rheumatol Int 32: 805-807.
- Sanahuja J, Ordoñez-Palau S, Begué R, Brieva L, Boquet D (2008) Primary Sjögren syndrome with tumefactive central nervous system involvement. Am J Neuroradiol 29: 1878-1879.
- Michel L, Toulgoat F, Desal H, Laplaud DA, Magot A, et al. (2011) Atypical neurologic complications in patients with primary Sjögren’s syndrome: Report of 4 cases. Semin Arthritis Rheum Elsevier 40: 338-342.
- Sassi SB, Nabli F, Boubaker A, Ben I, Neji S, et al. (2014) Pseudotumoral brain lesion as the presenting feature of primary Sjögren’s syndrome. J Neurol Sci 339: 214-216.