Abstract
A prospective cross-sectional study was carried out at the Specialized Surgical Hospital in Medical City to assess the characteristics of major complications related to continuous epidural anesthesia. Demographic data, epidural procedure specifics, and problems (from the pre-anesthetic phase until resolution) were documented. Categorical variables were expressed as a number (%) whereas continuous variables were expressed as a mean (SD). Of the 120 patients enrolled, the mean age (SD) was 42.1 ±17.0 years old; 52.5% were in the age ˃ 40 years old; 72.5% were male. The mean of BMI (SD) was 29.9 ± 5.2 kg/m2. 18.3% of them underwent gynaecological surgery, while 27.5% underwent general surgery, 64.2% of surgeries took less than 60 minutes. The result of the present study reported more than a quarter of them were overweight, and the majority of patients exhibited levels indicative of a lumber puncture. Epidural anesthesia was the cause of post-operative neurologic deficits in half of them, either new or worsening. Further researches are needed on large scale.
Keywords
Epidural anesthesia; Complication; Dural puncture; Hematoma
Introduction
An approach for perioperative pain management with many uses
in anaesthesiology is epidural anesthesia [1]. Although it can be
used as a primary anesthetic, it is most frequently a pain control
adjuvant [2]. For long-term pain treatment, either a single shot
or a continuous infusion can be used [3]. Additionally, it has
been demonstrated to shorten hospital stays, lower cortisol
levels, speed up the recovery of bowel function, and reduce the
risk of PE and DVT following surgery [4]. Improved knowledge
of the pathophysiology and risk factors for problems would aid
anaesthesiologists in using the procedure safely and reduce the
likelihood of unfavourable outcomes [5]. Although a number
of sizable studies have examined the dangers associated with
epidural blocks, the majority of these studies did not examine a
continuous cohort of patients and often only included patients
with persistent pain, expectant mothers, or patients undergoing
spinal-epidural anesthesia [6-9]. Because of this, it may be
challenging to adapt the reported incidence of complications to
a general surgical population or to compare it to those of other
organizations or healthcare systems. Additionally, numerous
severe occurrences brought on by epidural anesthesia have been
documented in retrospective case series or individual case reports
[10-12]. Only a small number of prospective surveys with sizable
patient populations, the majority from several centers, have been
reported [13-15]. From this point, this study aimed to assess
the characteristics of major complications related to continuous
epidural anesthesia.
Methods
Between March 2023 and May 2023, a prospective crosssectional
study was carried out at the Specialized Surgical
Hospital in Medical City to assess the characteristics of major
complications related to continuous epidural anesthesia among
120 patients who had continuous epidural anesthesia in the
medical city, demographic data, epidural procedure specifics,
and problems (from the pre-anesthetic phase until resolution)
were documented. Three anaesthesiologists who were blinded to
all information but the patient's name, medical record number,
surgical technique, and operation date performed the postoperative
follow-up. The same anaesthesiologist saw each patient
twice on the ward on the first and second postoperative days
(24-48 hours following surgery). The level of pain related to the
epidural itself was assessed on each occasion using an 11-point
visual analog scale, with 0 denoting "no pain," 1-3 denoting mild
pain, 4-6 denoting moderate pain, and 7-10 denoting severe
pain. A neurological examination was also conducted on each
occasion to identify any significant problems. Between the
seventh and fourteenth post-operative days, all patients who
had reported complications were re-interviewed over the phone.
They were continued until the patient was unable or unwilling to be reached again, the difficulties had fully resolved, or both. The
length of the follow-up and the duration of the problems were
noted. If neurological consequences persisted for more than
six months, they were regarded as permanent. The two skilled
anesthesiologists who had evaluated the initial assessment
made the final determination that follow-up was finished in each
case. Before we started gathering our data, we received ethical
permission from the Iraqi Ministry of Health. The data were
recorded into an excel spread sheet with each variable, and SPSS
version 20 was used to analyze the results. Categorical variables
were expressed as a number (%) whereas continuous variables
were expressed as a mean (SD).
Results
Of the 120 patients enrolled, the mean age (SD) was 42.1 ±17.0
years old; 47.5% were in the age ˂40 years old and 52.5% were in
the age ˃ 40 years old; 72.5% were male and 45% had overweight
of BMI. The mean of BMI was 29.9 and the SD was 5.2 kg/m2.
18.3% of them underwent gynaecological surgery, while 27.5%
underwent general surgery. According to Table 1, 64.2% of
surgeries took less than 60 minutes, and 77.5% of patients had
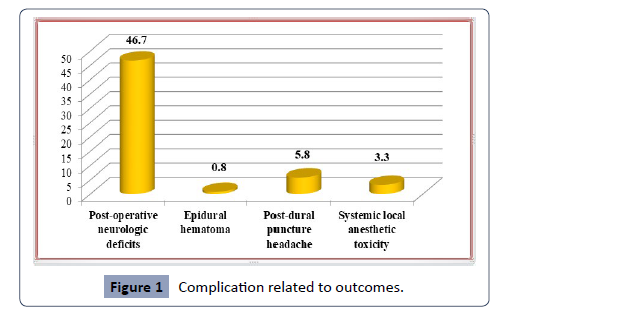
lumber puncture levels. As indicated in Figure 1, of those 68
(56.7%), 56 (46.7%) had new or deteriorating post-operative
neurologic impairments attributable to epidural anesthesia, 7
(5.8%) had headaches following dural puncture, and only 1 (0.8%)
had an epidural hematoma.
| Characteristic |
Frequency (n=120) |
Percent |
| Age(years) |
˂ 40 |
57 |
47.5 |
| |
> 40 |
63 |
52.5 |
| |
Mean age ± SD |
42.1 ± 17.0 |
|
| Gender |
Male |
87 |
72.5 |
| |
Female |
33 |
27.5 |
| BMI(kg/m2) |
Normal |
21 |
17.5 |
| |
Overweight |
54 |
45.0 |
| |
Obese |
45 |
37.5 |
| |
Mean age ± SD |
29.9 ± 5.2 |
|
| Type of surgery |
Orthopedic |
27 |
22.5 |
| |
Urologic |
12 |
10.0 |
| |
General |
33 |
27.5 |
| |
Gynecological |
22 |
18.3 |
| |
Thoracic |
11 |
9.2 |
| |
Vascular |
15 |
12.5 |
| Duration of surgery |
˂ 60 min |
77 |
64.2 |
| |
≥60 min |
43 |
35.8 |
| Puncture level |
Lumber level |
93 |
77.5 |
| |
Thoracic level |
27 |
22.5 |
Table 1. Characteristics of the patient.
Figure 1: Complication related to outcomes.
Discussion
This study aimed to assess the characteristics of major
complications related to continuous epidural anesthesia. One of
the findings of the existing study is that 52.5% of people were
over the age of 40 and 47.5% were under the age of 40. Elfeky et
al. conducted a prospective, randomized, controlled clinical trial in Egypt in 2019 with 100 patients 65 years of age or older of both
sexes; their BMI was 28.9, and the surgery lasted 183.1(18.9)
minutes [16]. A hospital-based cross-sectional study including
328 females was carried out in Saudi Arabia. The majority of the
women (172, or 52.4%) were in their 30s and 40s. 106 women
(32.3%) reported having an EA-positive previous pregnancy. A
small minority of them (13 [12.3%]) had a history of issues, while
the majority (93 [87.7%]) had no issues with EA. The side effects
were absent in 77 (72.6%) of the participating ladies [17]. In the
current study, there were 27.5% women and 72.5% men. In China,
a survey of 5083 surgical patients receiving epidural anesthesia
was done. Their mean age was 52.7± 17.0 years, with 3560 (70%)
men and 1523 (30%) women present [18]. A high body mass index
(BMI) has been associated with both epidural analgesia failure and
more challenging neuraxial method performance [19]. Studies
on the connection between obesity and regional anesthesia in
the context of obstetric anesthesia frequently concentrate on
the subarachnoid block and the lumbar epidural block [20]. 45%
of participants in the current study had an overweight BMI, and
37.5% had an obese BMI. We were unable to demonstrate a
clinically meaningful impact of thoracic epidural anesthetic on
the frequency of major complications following elective heart
surgery in compared to fast-track cardiac anesthesia without
epidural anesthesia. Given the potentially deadly complications
of an epidural hematoma following the installation of an epidural
catheter, it is questionable whether this procedure should
be utilized regularly in cardiac surgery patients who require
complete heparinization [21]. In the current study, 18.3% of them
had gynaecological surgery, followed by general surgery (27.5%)
and thoracic surgery (9.2%). In a prospective study conducted in
2018 with 150 patients, 58.3% of whom underwent open surgery
with epidural analgesia; Narayanappaa et al found that patients
who receive epidural analgesia have better surgical results [22].
Spinal anesthesia combined with fast-acting local anaesthetics
was preferred to general anesthesia in ambulatory procedures
and was associated with high levels of patient satisfaction [23].
In the current study, 64.2% of procedures finished in 60 minutes
or less, whereas 35.8% took longer. Capdevila et al. did a cohort
study in 2020 at 33 commercial or public hospitals practicing
ambulatory surgery in France, and they found that the mean and
SD of the surgical procedure were 27.9 ±17.1 [23]. Karim 2021
noticed that 66 of the 286 patients had a delayed recovery, and
a significant relationship was discovered with a p-value of 0.005 among the 180 (62.94%) male patients. Rural residents are more
likely to be patients 174 (60.84%). From the age of six months
to 91 years old, the mean age was 42.8 21.6 years. The majority
of the patients were over 50 (44.05%), followed by those who
were under 18 years old [24]. Post-dural (post-lumbar) puncture
headache (PDPH) is a frequent and incapacitating consequence
following an intentional puncture of the dura-arachnoid, whether
for diagnostic, therapeutic, or spinal anesthetic purposes, or
unintentionally during an epidural procedure. In the current
investigation, lumber puncture levels were identified in 77.5% of
the patients [25].
Forty-eight (7.5%) of the patients in Brazil developed PDPH. Age
[11.0% 31-50 years of age vs. 4.2% others, OR 2.21 (1.12-4.36);
p = 0.02], gender [11.1% female vs. 3.6% male, OR 2.25 (1.07-
4.73); p = 0.03], previous history of PDPH [26.4% positive vs.
6.2% negative, OR 4.30 (1.99-9.31); p 0.01], and bevel orientation
[16.1% perpendicular vs. 5. Between lumbar puncture and
headache onset, there is a lag of 6 to 72 hours, lasting 3 to 15 days.
Neck stiffness, tinnitus, hypoacusia, photophobia, or nausea were
all present in 34/48 (71%) of the patients with PDPH, according
to Amorim (2012) [25]. Retrospective data analysis of patients
who underwent continuous thoracic epidural injections of local
anesthetics was shown by Zengin et al. in 2021 [26]. Taking into
account the fact that local anesthetics were not administered in
high dosages or volumes, rates of hypotension and other issues
that may have been connected were comparable across all
groups. The incidence of only a few hemodynamic side effects
may be associated with the use of local anesthetics at low dosages
and small volumes. Anatomical, technical, and pharmaceutical
factors such abnormalities of the vertebral spine, traumatic
spinal taps, many attempts at needle placement, and the use
of antiplatelet and anticoagulant medicine may all contribute
to the development of a spinal epidural hematoma [27]. Some
of the factors suspected of predisposing patients to epidural
hematoma include the use of epidural catheters, simultaneous
administration of medications that affect hemostasis, exceeding
the recommended dose of enoxaparin, administering enoxaparin
to surgical patients prior to the establishment of hemostasis, the
presence of vertebral column abnormalities, advanced age, and
female gender. Only 1 (0.8%) of the findings showed an epidural
hematoma. Epidural anesthesia was found to be the cause of
56 (46.7%) new or worsening post-operative neurologic deficits,
and dural puncture was the cause of headaches in 7 (5.8%)
cases. In China, a study was conducted. In a study by Kang et al.
in 2014, they found that out of 5083 patients, 69 (1.36%) had
major complications, including epidural hematoma in 1 patient
(0.02%), post-operative neurologic deficits in 57 patients (1.12%),
post-dural puncture headache in 7 patients (0.14%), and systemic
local anesthetic toxicity in 4 patients (0.08%). Only one patient
experienced unilateral lower limb paraesthesia as a persistent
sequel [3]. In the US, 0.7% of patients who had a neuraxial
anesthesia reported a headache after having their spinal cord
punctured. One EBP was administered to 55.7% of patients who
had a postural puncture headache, and 10.7% of these patients
needed a second EBP. The SCORE Project was not intended to
monitor the frequency of accidental epidural needle dural
punctures [28].
In China, a survey of 5083 surgical inpatients receiving epidural
anesthesia was done. Their mean age was 52.7±17.0 years, and
there were 1523 women and 3560 men (70:30) [29]. According to
Kang et al. in 2021, 460 (9.05%) patients reported localized pain
at the epidural insertion site, while 532 (10.5%) patients reported
problems. Other problems included epidural hematoma in 1
patient (0.02%), negative neurological outcomes in 57 patients
(1.12%), systemic toxicity of local anesthetics in 4 patients (0.08%),
aberrant broad block of the spinal nerve in 3 patients (0.06%),
and PDPH in 7 patients (0.14%) [18]. According to Kadhim, 2020,
post-spinal puncture headache (PSPH) incidence and intensity in
Iraq are substantially correlated with the size of the spinal needle;
with narrower needles being linked to a less common and milder
form of headache compared to wider diameter needles [30].
Conclusion
According to the results of the current study, there were more
male instances than female cases, more than a quarter of them
were overweight, and the majority of patients exhibited levels
indicative of a lumber puncture. Epidural anesthesia was the
cause of post-operative neurologic deficits in half of them, either
new or worsening. Further researches are needed on large scale.
Conflict of interest:
None