Zahouani T*, Recinos A and Mota J
Department of Pediatrics, Lincoln Medical and Mental Health Center, USA
- *Corresponding Author:
- Tarik Zahouani
Department of Pediatrics, Lincoln Medical and Mental Health Center
237 East 149th St Bronx, NY 10451, USA
Tel: 718-579-5030
E-mail: Tarikzahouani@gmail.com
Received Date:November 29 2016; Accepted Date:December 03 2016; Published Date:December 07 2016
Citation: Zahouani T, Recinos A, Mota J. Clinical Image: Omphalitis. Ann Clin Lab Res. 2016, 4: 4 doi: 10.21767/2386-5180.1000135
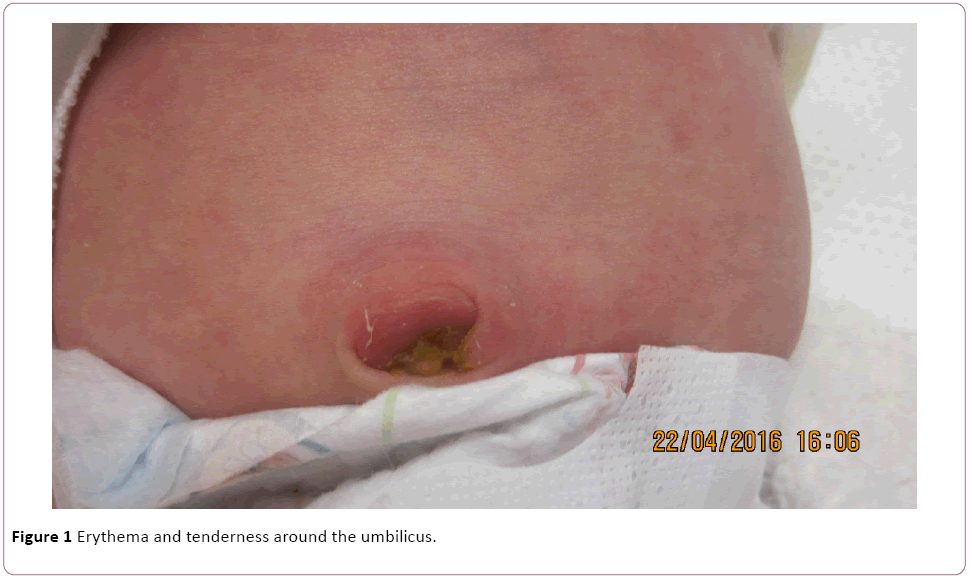
A 13-day old baby girl was brought to the emergency department due to redness, induration and swelling of the umbilical cord. On physical exam, we found an afebrile, irritable infant with erythema and tenderness around the umbilicus
Clinical Blog
A 13-day old baby girl was brought to the emergency department due to redness, induration and swelling of the umbilical cord. On physical exam, we found an afebrile, irritable infant with erythema and tenderness around the umbilicus (Figure 1). The white blood cell count was normal (15.2 x 109 per liter), C-Reactive protein mildly elevated at 0.44 mg/dL. An abdominal Ultrasound was performed revealing a hypoechoic structure in the umbilical area that may represent an abscess. Patient was subsequently admitted to the hospital with the diagnosis of omphalitis for 6 days where she received intravenous antibiotics and was discharged home to complete 14 days of antibiotics. In the follow up appointment, the patient had complete resolution of the omphalitis with no erythema or induration.
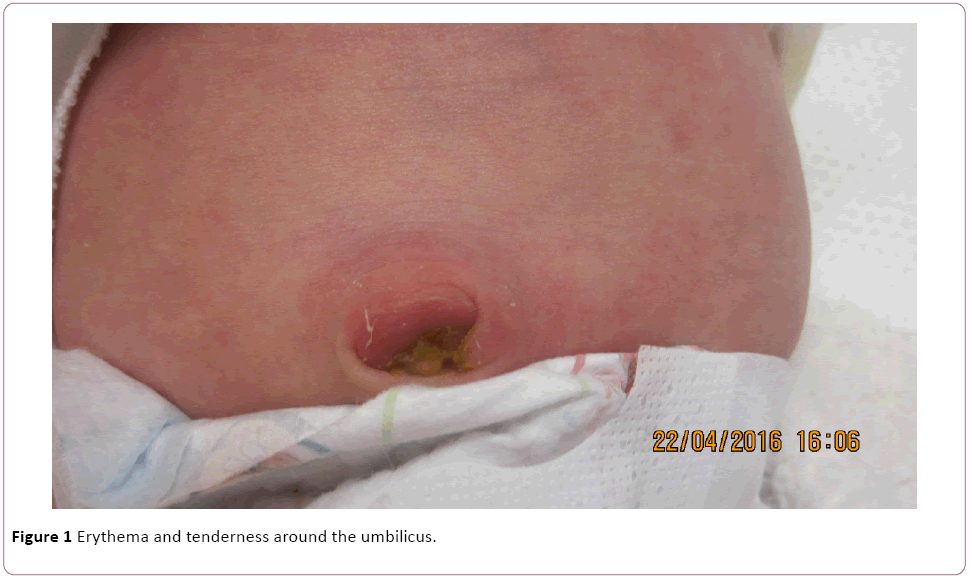
Figure 1: Erythema and tenderness around the umbilicus.
Omphalitis is an infection of the umbilicus primarily affecting neonates. It is uncommon in developed countries but remains a common problem in underdeveloped countries where health care is not readily available [1]. The devitalized tissue of the umbilical cord is prone to bacterial infection as it is rich in substrate with a lack of normal skin barrier and the undergoing ischemia after the umbilical stump dries and falls off [2]. The most common organisms involved are Staphylococcus aureus, Group A streptococcus and Escherichia coli. Symptoms include periumbilical erythema, purulent discharge, tenderness, fever or hypothermia and in advanced cases septic shock or necrotizing fasciitis [2]. The diagnosis is clinical and the workup including CBC, wound and blood cultures, abdominal radiography and ultrasound is performed to rule out other diagnoses or to diagnose complications such as evisceration, necrotizing fasciitis, peritonitis and abscesses [1,2]. Antibiotic therapy for 10-14 days targeting Staphylococcus aureus is the mainstay of treatment along with supportive care if required [2].
17710
References
- Ameh EA, Nmadu PT (2002) Major complications of omphalitis in neonates and infants. Pediatr Surg Int 18:413-416.
- Bugaje MA (2013) Omphalitis. Paediatric surgery: A Comprehensive Text for Africa.