Keywords
co-morbidity, substance use, post-traumatic stress disorder
Introduction
The phenomenon of the co existence of two disorders, known as co morbidity or dual diagnosis, of individuals suffering from Post Traumatic Stress Disorder (PTSD) and Substance Use Disorder (SUD) is an issue that worries professionals as it concerns care, therapy, rehabilitation and the relationship between the two disorders. [1] The coexistence of substance dependence and post traumatic stress disorder is common between substance users (35-50%) [2-4] . In most cases, one disorder makes the other worse, increasing in this way the possibility of relapse and decreasing the chances for the social rehabilitation of these people.
Despite improvements in substance use therapy, individuals with current PTSD continue to exhibit increased disability and poorer functioning over the 2-year follow-up. These findings highlight the importance of assessing multiple outcomes. [5]
PTSD is an anxiety disorder that can develop after exposure to one or more traumatic events that threatened or caused great physical harm. It is a severe and ongoing emotional reaction to an extreme psychological trauma.This stressor may involve someone's actual death, a threat to the patient's or someone else's life, serious physical injury, an unwanted sexual act, or a threat to physical or psychological integrity.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) definition, the person has each of the following key symptoms for over a month, which result in decreased ability to function at different levels, for example, at work or in their social life (e.g. work, social life): (a) Intrusion, for example, flashbacks and nightmares, (b) Avoidance, expressed in denial to talk about it or remember it, (c) Arousal, for example, insomnia and anger [6]
Based on National Co morbidity Surveys (NCS), the life time prevalence of PTSD in the general population is 8% [7] . A percentage of 20% to 50% of people will eventually develop symptoms consistent with PTSD diagnosis following exposure to a traumatic event [8,9].
SUD is a term that encompasses both dependence on and abuse of drugs usually taken voluntarily for the purpose of their effect on the central nervous system (usually referred to as intoxication or "high") or to prevent or reduce withdrawal symptoms. These mental disorders form a subcategory of the substance-related disorders [6].
Substance abuse is the compulsion to use drugs despite the negative consequences e.g. legal, physical, social, and psychological caused by the substance. The DSM-IV term is “substance use disorder” with substance abuse presented as a milder form and substance dependence as a more severe one.
In a national United States of America (U.S.A.) sample, [7] It was found that the rates of substance use were 35% for men and 18% for women respectively in lifetime. The rate was higher in whites than blacks or Hispanics.
According to the European Monitoring Centre for Drug and Drug Addiction (EMCDDA) [10] in a general Cypriot population survey carried out in 2006 among Greek speaking adults (15-64 years old), the life prevalence for cannabis was 6.6%. The lifetime prevalence for ecstasy was 1.6%, following cannabis use. In 2007, the problematic opioid users aged 15-64 were estimated to be between 1.6 and 3.9. per 1000 inhabitants. The total number of problematic drug users in Cyprus was estimated to be between 1591-2541.
In Europe, estimations to the adult population (15-64 years old) show for cannabis a lifetime prevalence of at least 71 million (22% of European adults) and for cocaine a lifetime prevalence of at least 12 million (3.6% of European adults). The problematic opioid use is between one and six cases per 1000 adult population [10] .Studies in the USA report a very high percentage of co morbidity of psychiatric and substance use disorders (79%) [11] and even higher in Greece, up to 90, 3% [12] . Post traumatic stress disorder is related to the disorder of substance use, abuse and dependence and the correlation between the two disorders is high. Among people with substance use disorder, PTSD is common. Specifically, the relevant percentage for individuals with opioid use disorder is 33.2% [5].
Clinical observation about the possible co existence and interaction of the two disorders has led to the development of research in the 80’s. Keane et al. [13] were one of the first research teams that identified high rates of problems with alcohol and other drug abuse in treatment-seeking combat returns with PTSD.
Studies [14,15] demonstrated that co morbidity of substance and alcohol use among the veterans with PTSD diagnosis fluctuated from 64-84%. Later studies supported this result and found that patients with PTSD and SUD perceived their two disorders as functionally correlated, [7,16,17] . A Back et al. [18] study found that there is a high correlation between PTSD and people addicted to cocaine. The 42% in this study [18] and 21% in similar studies [19] satisfied the criteria for a PTSD diagnosis and in the general population this percentage is only 7,8%, a difference that causes many concerns. Clinical studies also showed high rates of PTSD among people in treatment for heroin dependence (life-time 14-29%, current: 20-31%). These rates are higher than those observed among the general population - life time: 1-8%, current: 1-4% [5]
There is also a debate in the literature on whether PTSD precedes SUD or if it increases the risk for significant drug abuse or dependency [7,20] . Alternative explanations suggest that a substance using lifestyle may predispose such individuals to trauma exposure and subsequent PTSD or that drug use increases susceptibility to PTSD following a traumatic exposure [20].
In the question as to whether PTSD and SUD share common causes [20] , 24, 3% of those who were addicted had a history of PTSD compared to the 9, 6% of those who did not make use of psychoactive substances. [20] The possibility of starting on drugs was 29, 1% for patients with a history of PTSD compared to 11, 9% of those who did not have a PTSD diagnosis [20] . Identical twins were studied in order to explore the genetic effect on PTSD and SUD and it was found that genetic influence is responsible for 15, 3% for the PTSD, SUD and alcohol consumption and 20% for PTSD specifically. It was also found that for all the 3 disorders there are common environmental factors and specific for each phenotype, suggesting that alcohol and drug dependence have different etiological elements as well as important common genetic and environmental contributions.
Other researchers [17,21] explored the severity of drug use and PTSD and found that PTSD symptomatology has a strong correlation with the severity of drug use, showing that psychological discomfort because of the trauma may be an important factor for serious drug abuse. Although drug use may reduce the negative effects of trauma, severe abuse may trigger the appearance of PTSD symptoms and increase discomfort. Therefore, if PTSD if left untreated, SUD may develop severely in time and lead to worse treatment results for drug abuse [22].
Methodology
Aim of the study
The aim of this study was to answer the questions which are based on the available literature and clinical observation:
1. Is there a relation between SUD and PTSD?
2. Does addiction severity differ between individuals with co morbidity and those with substance use disorder only?
3. Is the level of severity of PTSD related to the level of severity of addiction?
Design
This is a cross-sectional co relational design with the use of two samples: one with PTSD – SUD co morbidity and one with SUD without PTSD.
Sample
The sample was drawn from a substance use therapeutic program based on the model of therapeutic communities in Cyprus. The inclusion criteria were to have treatment and be free of substances and the exclusion criteria were the age below 18 years and over 70 years old and a diagnosis of psychotic disorder, brain trauma or organic psychosyndrome. Forty people participated in the therapeutic program; all of them fulfilled the criteria of participating in the research. After a personalized informative meeting, 35 people agreed their participation in the research. Eventually, two of those people did not complete the questioners. The 33 people consisted the researcher’s sample (N=33).
Permission to conduct the study was obtained from the Ministry of Health. As this study was a part of a BSc final project a supervisory committee reviewed and approved the protocol. The participants signed an informed consent. The anonymity, confidentiality and protection of personal data were assured.
Research instruments
• Treatment Demand Indicator T.D.I.
The Treatment Demand Indicator (TDI) is one of the five key epidemiological indicators which contribute to the overall aim of providing objective, reliable and comparable information at a European level concerning drug and drug addiction. It was designed on November 1996 and it consists of categorical and numerical questions related to socio-demographic information, drug use and high risk behaviors [23].
• Addiction severity index (ASI)
The ASI was originally developed in the USA [24] in 1980 and it was modified for use in Europe and renamed to European Addiction Severity Index (EuropASI) [25].
The EuropASI is a 30 item questionnaire that is used for research and diagnostic purposes and evaluates 7 domains: the medical condition, occupation and financial support network, substance use, legal condition, family and social relations, as well as the psychiatric condition. The participant is given a score on each of these domains so as to develop a “severity profile” which means the severity of substance use. At the same time, the instrument can be used for re-evaluation and the effectiveness of any therapeutic intervention. The test-retest in the first reliability study was found to be 0.89. [24]
• Post Traumatic Stress Diagnostic Scale
This was the main instrument of the study that was used for the differentiation of the participants into two groups. PDS is a 49 item scale designed for the diagnosis and the symptom severity of the PTSD as it is reflected in the DSM-IV. The PDS consists of 6 factors: the exposure to the traumatic event, avoidance, arousal, symptom duration / delayed onset and functioning [26].
The reliability of the scale is reported by the author for the 17 items with a Cronbach alpha on .92, indicating a high internal consistency and the test-retest reliability provided good support for the interval consistency and stability. The convergent validity was examined by correlating the symptom severity score with other scales that measure psychological constructs associated with PTSD. Correlation between the PDS and the scales measuring associated constructs (N=230) are as follows:
Beck Depression Inventory (BDI) =.79
State index of state – trait Anxiety Inventory (STAI) =.73
Trait Index of State – Trait anxiety Inventory =.74
Impact of Event scale intrusion index=.80 and Avoidance index =.66 [27]
For the purpose of this study, the PDS was translated and back translated in the Greek language.
Data collection
The data was collected in 2007 and the first evaluation consisted of the information included in the participant’s medical record. Personal data were collected from the EuropASI and TDI questioners which were used according to the evaluation schedule of the therapeutic program. The TDI provided information about the demographic characteristics of the individuals as well as information for the substance use and the ASI confirmed the diagnosis of SUD. The second step was to administer all the P.D.S for the diagnosis of PTSD. The sample was divided into 2 groups: the group N consisting of individuals suffering from co morbidity of PTSD and SUD and the group O consisting of individuals with SUD and absence of PTSD.l
Results
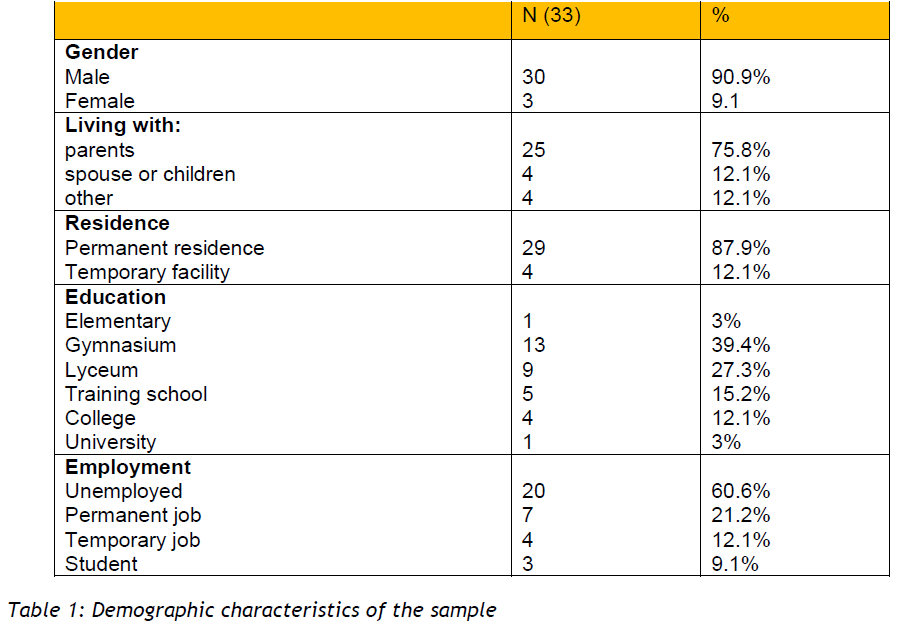
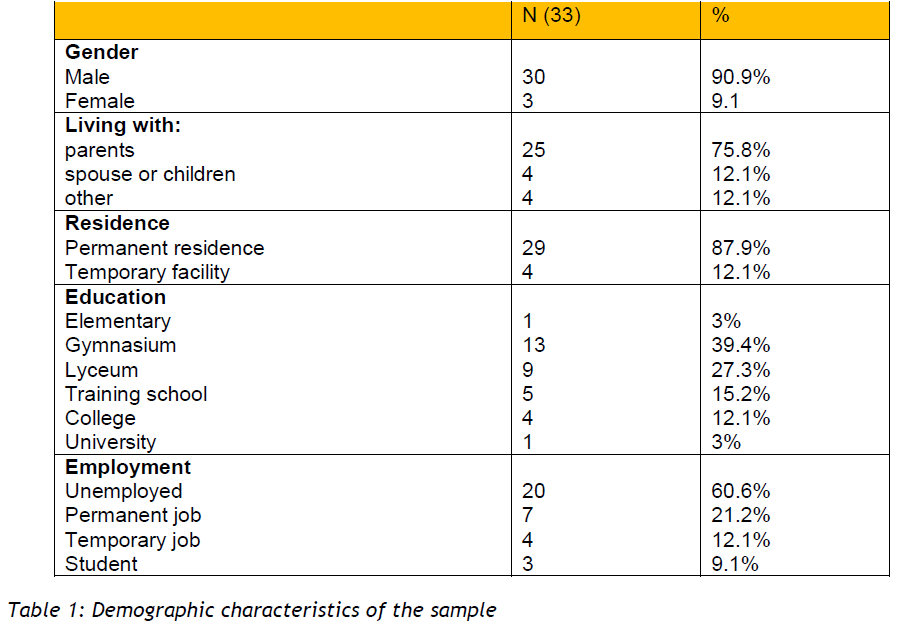
The sample consisted of 30 (90.9%) men and 3 women (9.1%). Their age was between 19 to 51 years old (M=26.2, SD=6.5). Regarding their living conditions, 25 participants (75.8%) were living with their parents and the rest with a spouse, partner or a friend. Most of them (29 or 87.9%) were living on a permanent residence and the others were staying in a temporary facility or were homeless. 20 participants were living in the city (60.6%) 2 in a refugee camp (6.1%) and 11 in a village or a suburb (33.3%). The majority did not work (20 persons or 60.6%), 7 had a permanent job (21.2%), 3 were students (9.1%) and 4 had a temporary job (12.1%). The highest educational status was gymnasium (13 or 39.4%), followed by lyceum (9 or 27.3%), 5 participants had technical school education (15.2%), 4 were college graduates (12.1%), 1 completed the elementary school and 1 was a university graduate (3%). 14 participants (42.4%) gave up school before graduation.
These results are presented in table 1.
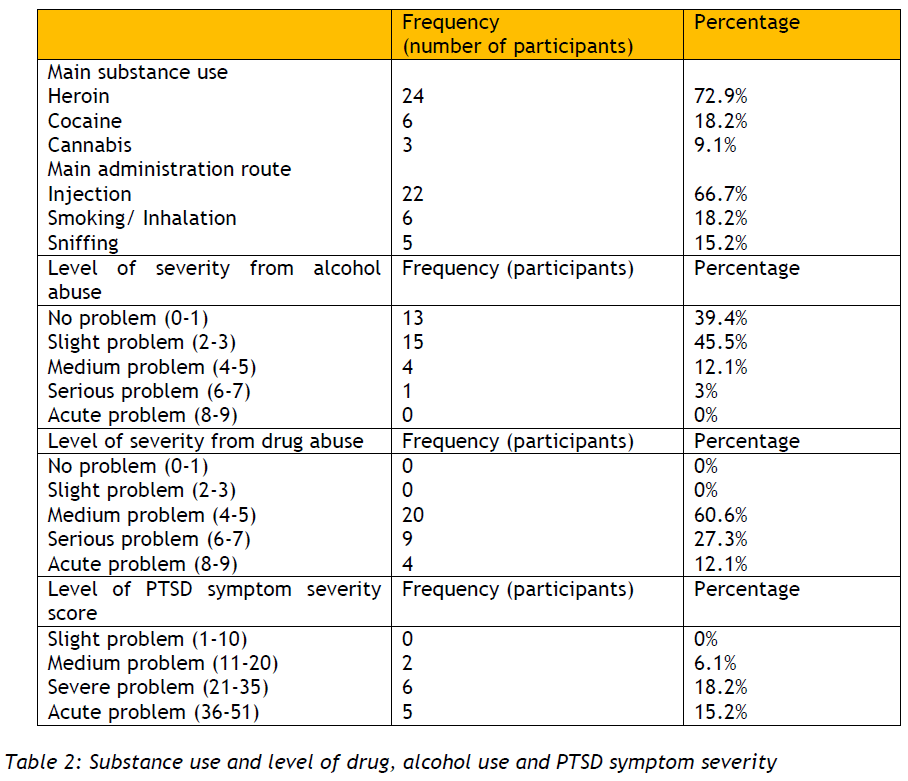
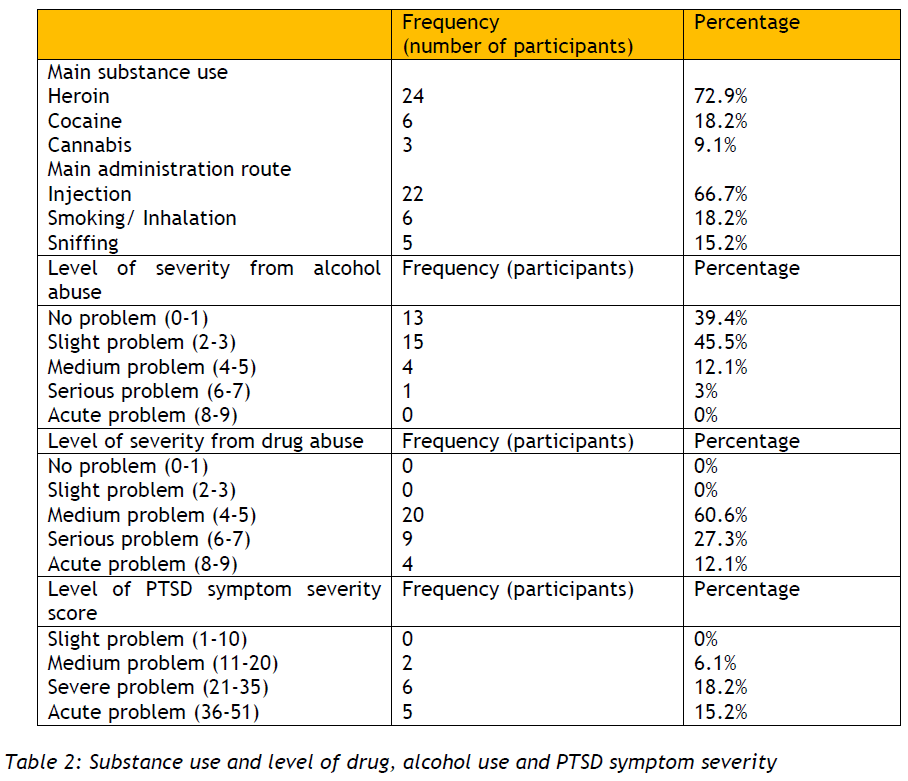
Substance use
The mean age for asking first time help was 23.7 years (SD= 6.9). The youngest age when substance use began was 12 years old and the oldest 40 years old. It is also interesting that 11 participants had various ways of using (injections, smoking, sniffing) and they usually began with cannabis. Regarding their high risk behavior, 23 of the participants (69.7%) used injections and 15 of those or (65.2%) have used the same needle and syringe. The level of substance use severity for the 33 participants was between 4 to 8 according to the ASI score, with a M= 5.4 and SD=1.3. The results also showed that the risk of alcohol abuse is 2.2 (SD=1.5) in a 0 -7 scale.
Post traumatic stress disorder (PTSD):
The results showed that 13 persons (40.6%) reported symptoms of PTSD. From those, the level of impaired functioning showed that 3 people (23%) had a medium problem and the other 10 (77%) had a serious impaired functioning level. The symptom severity score was between 11- 45, M= 30.5 and SD= 10.7.The severity index was: 1-10 mild, 11-20 medium, 21-35 severe, 36-51 acute problems. The rest 20 participants (59.4%) of the 33, which was the sample, did not suffer from PTSD. These results are presented in the table 2.
Correlation studies
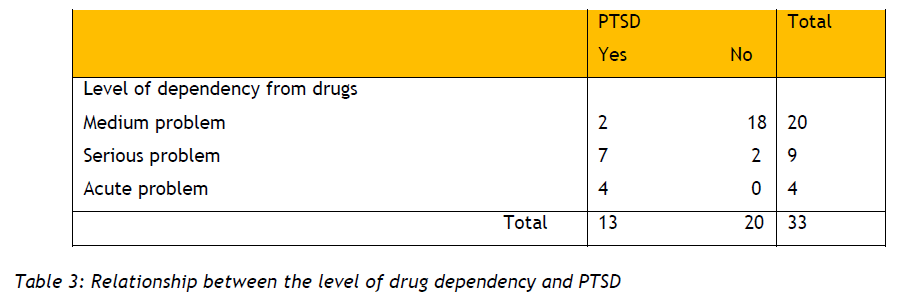
The sample was divided into 2 groups according to the previous analyses: those suffering from SUD only (N=20, group O) and those suffering from SUD and PTSD (N=13, group N).
1. Correlation between the PTSD (symptom severity score) and the level of dependency from drugs. The aim for this analysis was to find if there is a correlation between the level of PTSD severity symptoms and the level of drug dependency in group N.
The Pearson correlation coefficient was used and a statistically significant relation was accepted if the p-value is lower from the level of significance α=5%. The results showed that there was a statistically positive significant correlation between the PTSD symptom severity and the level of dependency from drugs (r=0.678, p-value=0.011). This means that the higher the level of dependency, the higher the PTSD symptom severity index.
2. Correlation between the PTSD (symptom severity score) and the level of alcohol dependency. The aim for this analysis was to find if the persons in group N apart from being dependent on drugs, there is a correlation between the level of PTSD severity symptoms and the level of alcohol dependency. In this case, the Pearson correlation coefficient showed that there is no statistically significant correlation between the PTSD symptom severity and the level of dependency from alcohol (r=0.515, p-value=0.072).
3. Those who are suffering from PTSD may present higher levels of dependency related to those who are not suffering from PTSD
In this case correlations between the O and N group were applied. One way to do this was to use the score of severity of drug abuse as a continuous variable and compare the two groups with a t-test for two independent samples. The results showed that there was a statistically significant difference between the two groups (t=4.9, p-value<0.001), where the N group presented a higher degree of severity of dependency on drugs in relation to group O. More specifically, the mean of the N group is 6.54 (SD= 1.3) and the mean of the O group is 4.65 (SD=0.7) and this shows that PTSD is significantly related to the level of drug dependency.
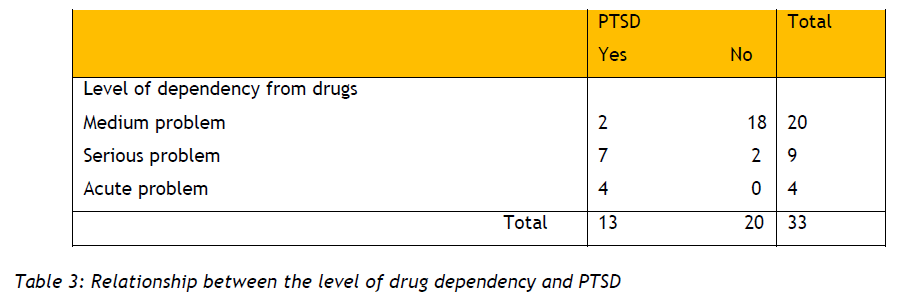
Another way to examine this correlation was to divide the drug dependency severity index in categories (no problem, slight problem etc) and examine if there were more persons in each category, suffering from PTSD. It was examined if PTSD was related to the various levels of dependency. This test was performed with chi-square (Χ2) and the results showed that there was a significant correlation suggesting that those suffering from PTSD presented a bigger problem with drugs (Χ2=18.945, p-value<0.001). Therefore, those participants who had an acute problem in the level of severity of drug abuse were also suffering from PTSD (78%) and those who had a medium problem were not suffering from PTSD (90%). These results are presented in table 3.
4. Those participants suffering from PTSD are more dependent on alcohol:
To test this hypothesis a t-test for 2 independent variables was used and the results showed that there was no significant difference between the 2 groups regarding alcohol dependency (t=1.5, p-value=0.142) which means that PTSD is not related to the level of alcohol dependency. The researchers also used the severity index categories to see if PTSD was related to the various levels of alcohol dependency by using the chi-square test (Χ2). The results showed again that there was no significant relation between PTSD and the level of alcohol dependency (Χ2=2.134, p-value=0.545).
5. Those participants with high level of drug and alcohol dependency severity index, have a higher degree of impaired functioning. According to the study the participants belonged either to the medium or severe level of impaired functioning. The t-tests showed no significant difference between the functioning and the level of drug dependence. (t=2.1, p-value=0.055). Concerning the relation between the severity of alcohol dependency and impaired functioning the t-test showed that the group with the serious impaired functioning (M=3.4, SD= 1.8) had a significantly higher degree of alcohol dependency compared to those with alcohol dependency is only 0.7 and SD= 0.6. (t=2.5, p-value=0.027)
6. Those participants with a high severity index in drug and alcohol dependency have a higher PTSD symptom index.
This hypothesis was tested with the ANOVA and it showed that the scores differ significantly between the groups with medium, severe and acute problems with drugs (F=7.971, p-value=0.009). More specifically, those with acute problems seemed to have a higher degree of PTSD severity symptoms (M=42.5, SD=2.6) compared to those with medium problems (N=25.5, SD=9.2). The Analysis of Variance was also used to see if the scores of those with a higher PTSD symptom index differed significantly in groups with medium, severe and acute problems with drugs, however the results did not support this hypothesis (F=1.947, p-value=0.1931).
7. There is a relation between the main substance of use and the existence of PTSD in users:
This hypothesis was tested with chi-square (Χ2) and the results showed that there was no correlation between the main substance used and the fact that a user may suffer from PTSD (Χ2=0.190, p-value=0.909).
Discussion
The results of this study support the hypothesis of co morbidity of Substance Use Disorder- SUD and Post Traumatic Stress Disorder-PTSD (r=0.678, p-value= 0.001). These show that indeed there is a statistically significant difference between the two groups, where those individuals with SUD who are also suffering from PTSD, suffer a higher degree of dependency compared to those with no history of PTSD. It is therefore supported that if a person is using substances like narcotics, and at the same time presents symptoms of PTSD, the addiction problems and the dependency on drugs are much greater. These findings agree with other studies who found that there is a tendency of individuals with PTSD to score higher in the ASI instrument suggesting that this disorder may increase the risk for significant abuse or dependency on substances [2,7,20].
The 40.6 percentage of co morbidity in this study is similar to other studies supporting a co morbidity percentage of 25-55% [14,16,18,28,29] . Within treatment-seeking samples of SUD patients, current PTSD rates range from approximately 33-50%. [2-4] . However, there are reports with lower percentages like 24, 3% [20] and even lower with 21.% [30].
Especially, the results of this study are the same with another survey [2] which showed that 38.5% suffer from PTSD. Reynolds et al, also, found that the groups with PTSD had higher ASI score than the non PTSD group. [2] The two studies had similar samples. Both of them had small samples which were taken from therapeutic programs with the same exclusion criteria. Also, the samples had similarities regarding the demographic characteristics, mainly regarding gender, with men being more than women, and employment, with high percentages of unemployed persons. According to the European annual report, opioid users report higher rates of unemployment and lower levels of educational attendance than other clients. [10] . The average age is not significantly different. Also, the A.S.I. instrument was used in both studies.
As regards to gender issues, the majority of the sample were men and is similar to other studies [2,16,29] , supporting the international view [10] that women are less likely to begin substance use. On average men outnumber women opiod clients by three to one with higher proportions of men found in Cyprus, Greece, Bulgaria, Italy, Malta, Portugal, Spain and France [10] . However, although it would have been very interesting, the small women sample did not allow for more statistical analyses to detect gender differences in PTSD and SUD.
Most of the participants live with their family and this can be explained by the strong bonds of the traditional Cypriot family which supports its members during the whole span of their adult life, although this may create another kind of dependency for the addicted person – a dependence on their family members.
It is also found that the most common substance used is cannabis (90.9% of the sample) which is in agreement with the European Monitoring Center for Drugs and Drug Addiction – Annual Report 2008. Regarding their high risk behavior, 65.2% of our sample, have used the same needle and syringe which is lower compared to other studies where this percentage reaches almost the 97% [31] . The level of severity of substance use according to ASI is between 4 and 8 which means that the participants present a medium to severe problem regarding substance use. These results can be considered normal given that the sample is drawn from a program offering therapeutic interventions to already addicted individuals. For the same reason the lower level of severity of alcohol abuse is expected, since this kind of dependency was detected as a secondary problem, or in the framework of a multiple substance use.
As regards to the severity of the symptoms of the PTSD and the level of dependency on drugs and /or alcohol, it is found that the more severe the symptoms of PTSD, the higher the level of dependency and vice versa. This finding supports other studies [17,21] which point out that violent trauma and psychological malaise is related to the severity of dependency. Evidence from numerous studies supports the notion that a positive correlation exists between symptoms of PTSD and severity of SUD symptoms. [28,29].
The symptom severity score of individuals with PTSD was not correlated with the level of alcohol dependence, which contradicts the findings of other studies by [32,33] . The explanation for this finding is that alcohol consumption was not the main problem of the selected sample, since it was drawn from a drug addiction treatment center where alcohol is not included. Therefore, the analysis in this study was performed for alcohol use as a secondary problem, since the focus and main problem was addiction on drugs.
Limitations of the study
The research used a relevantly small sample, mainly due to the fact that the number of people in therapy for drug addiction is small and secondly because the research concerned only one center. In Cyprus there is only one more therapy center dealing with this group of people. However, it is rather difficult to access these centers.
Due to the small sample repentant researches would have to take place in orso as reach a more holistic view of this aspect.
Conclusion
The coexistence of substance dependence and post traumatic stress disorder between substance users in this study is 30 to 55%. In most cases, one disorder makes the other worse, increasing in this way the possibility of relapse and decreasing the chances for social rehabilitation of these people. This finding illustrates that it is important to investigate more and determine the relationship between the two disorders (PTSD and SUD) in order to find out which one precedes the other, if there is such a case. In addition, it is important to investigate how one disorder affects the development of the other and how they affect, if they do, caring, the therapeutic progress and the development of the person. The study has also shown the need for investigating the existence of Post Traumatic Stress Disorder among people in the therapeutic programs for drug dependence.
3423
References
- Matsa K editor. The puzzle of drug addiction. 1st ed. athens: Arga; 1995.
- Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A. Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug Alcohol Depend. 2005 Mar 7;77(3):251-258.
- Triffleman EG, Marmar CR, Delucchi KL, Ronfeldt H. Childhood trauma and posttraumatic stress disorder in substance abuse inpatients. J.Nerv.Ment.Dis. 1995 Mar;183(3):172-176.
- Dansky BS, Brady KT, Saladin ME, Killeen T, Becker S, Roitzsch J. Victimization and PTSD in individuals with substance use disorders: gender and racial differences. Am.J.Drug Alcohol Abuse 1996 Feb;22(1):75-93.
- Mills KL, Teesson M, Ross J, Peters L. Trauma, PTSD, and substance use disorders: findings from the Australian National Survey of Mental Health and Well-Being. Am.J.Psychiatry 2006 Apr;163(4):652-658.
- American Psychiatric Association editor. Diagnostic and Statistical Manual of Mental Disorder (4th edition). 4th ed. Washington: American Psychiatric Association; 1994.
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch.Gen.Psychiatry 1995 Dec;52(12):1048-1060.
- Alim TN, Graves E, Mellman TA, Aigbogun N, Gray E, Lawson W, et al. Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. J.Natl.Med.Assoc. 2006 Oct;98(10):1630-1636.
- Zatzick DF, Rivara FP, Nathens AB, Jurkovich GJ, Wang J, Fan MY, et al. A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychol.Med. 2007 Oct;37(10):1469-1480.
- European Monitoring Centre for Drugs and Drug Addiction. editor. The state of the drugs problem in Europe. 1st ed. Luxembourg: European Monitoring Centre for Drugs and Drug Addiction; 2008.
- Kessler RC. The Epidemiology of Psychiatric Comorbidity. In: Tsuang M, Tohen M, Zahner G, editors. Text book of psychiatric epidemiology. 1st ed. New York: wiley; 1995. p. 179-197.
- Kokkevi A, Stefanis k. Substance use and psychiatry co-morbiditty. comprehensive psychiatry 1995 June 26;36(5):329-337.
- Keane TM, Gerardi RJ, Lyons JA, Wolfe J. The interrelationship of substance abuse and posttraumatic stress disorder. Epidemiological and clinical considerations. Recent Dev.Alcohol. 1988;6:27-48.
- Escobar JI, Randolph ET, Puente G, Spiwak F, Asamen JK, Hill M, et al. Post-traumatic stress disorder in Hispanic Vietnam veterans. Clinical phenomenology and sociocultural characteristics. J.Nerv.Ment.Dis. 1983 Oct;171(10):585-596.
- Keane TM, Caddell JM, Taylor KL. Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: three studies in reliability and validity. J.Consult.Clin.Psychol. 1988 Feb;56(1):85-90.
- Brown PJ, Recupero PR, Stout R. PTSD substance abuse comorbidity and treatment utilization. Addict.Behav. 1995 Mar-Apr;20(2):251-254.
- Brewer DD, Catalano RF, Haggerty K, Gainey RR, Fleming CB. A meta-analysis of predictors of continued drug use during and after treatment for opiate addiction. Addiction 1998 Jan;93(1):73-92.
- Back SE, Brady KT, Jaanimagi U, Jackson JL. Cocaine dependence and PTSD: a pilot study of symptom interplay and treatment preferences. Addict.Behav. 2006 Feb;31(2):351-354.
- Najavits LM, Weiss RD, Shaw SR. The link between substance abuse and posttraumatic stress disorder in women. A research review. Am.J.Addict. 1997 Fall;6(4):273-283.20.
- Chilcoat HD, Breslau N. Investigations of causal pathways between PTSD and drug use disorders. Addict.Behav. 1998 Nov-Dec;23(6):827-840.
- Clark HW, Masson CL, Delucchi KL, Hall SM, Sees KL. Violent traumatic events and drug abuse severity. J.Subst.Abuse Treat. 2001 Mar;20(2):121-127.
- Ouimette PC, Brown PJ, Najavits LM. Course and treatment of patients with both substance use and posttraumatic stress disorders. Addict.Behav. 1998 Nov-Dec;23(6):785-795.
- Simon R, Donmall M, Hartnoll R, Kokkevi A, Ouwehand AW, Stauffacher M, et al. The EMCDDA/Pompidou Group treatment demand indicator protocol: a European core item set for treatment monitoring and reporting. Eur.Addict.Res. 1999 Dec;5(4):197-207.
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The Fifth Edition of the Addiction Severity Index. J.Subst.Abuse Treat. 1992;9(3):199-213.
- Blacken P, Hendriks V, Pozzi G, et al editors. European Addiction Severity Index (EuropASI) 5th ed. Athens: EMCCDA; 1994.
- Foa EB editor. Posttraumatic Stress Diagnostic Scale Manual. 1st ed. USA: PEARSON; 1995.
- Foa eb, Riggs ds, Dancu cv, Rothbaum bo. Reliability and Validity of Brief Instrument for Assessing Post-Traumatic Stress Disorder. journal of traumatic stress 1993 Jul;6(4):460-464.
- Brown PJ, Stout RL, Gannon-Rowley J. Substance use disorder-PTSD comorbidity. Patients' perceptions of symptom interplay and treatment issues. J.Subst.Abuse Treat. 1998 Sep-Oct;15(5):445-448.
- Back S, Dansky BS, Coffey SF, Saladin ME, Sonne S, Brady KT. Cocaine dependence with and without post-traumatic stress disorder: a comparison of substance use, trauma history and psychiatric comorbidity. Am.J.Addict. 2000 Winter;9(1):51-62.
- Najavits LM, Runkel R, Neuner C, Frank AF, Thase ME, Crits-Christoph P, et al. Rates and symptoms of PTSD among cocaine-dependent patients. J.Stud.Alcohol 2003 Sep;64(5):601-606.
- Miller PG. Safe using messages may not be enough to promote behaviour change amongst injecting drug users who are ambivalent or indifferent towards death. Harm Reduct J. 2009 Jul 25;6:18.
- Xian H, Chantarujikapong SI, Scherrer JF, Eisen SA, Lyons MJ, Goldberg J, et al. Genetic and environmental influences on posttraumatic stress disorder, alcohol and drug dependence in twin pairs. Drug Alcohol Depend. 2000 Dec 22;61(1):95-102.
- Volpicelli J, Balaraman G, Hahn J, Wallace H, Bux D. The role of uncontrollable trauma in the development of PTSD and alcohol addiction. Alcohol Res.Health 1999;23(4):256-262.