Keywords
Eating disorders; Intensive outpatients; Hospitalization; Anorexia nervosa; Bulimia nervosa
Introduction
History
The ED’s history is quite interesting and has a great abundance of casuistry and therapeutic modalities. However, this subject is not one of the objectives in this work. Towards the middle of twentieth century, medicine began to gradually adapt the routines of medical, nutritional and psychotherapeutic treatments in Anorexia Nervosa (AN) and other Eating Disorders, with an interdisciplinary approach, focused on a patient with multivariate etiopathogenesis, from the studies of Hilde Bruch of Baylor College of Medicine and subsequent researchers, who were based on her job [1].
Prevalence
AN (Anorexia nervosa) and BN (Bulimia Nervosa) are prevalent diseases that affect between 1% and 10% of adolescent students in school age [2]. According to Kaye, AN and BN affect only an estimated 0.3% to 0.7% and 1.5% to 2.5%, respectively, of women in the general population.
Prevalence studies are quite variable from country to country. With greater incidence in the West than in Asia, except for Japan which has the highest worldwide prevalence to this disease. Argentina, in the West, follows Japan quite closely. The relationship between the effects on women and men is 3:1 and 10:1, depending on the geographical zone [3]. The highest incidence is found in adolescents between the ages of 9 and 15 AN and a slightly larger average age for patients with BN, Unspecified Feeding or Eating Disorder (UFED) or other Eating Disorders. These disorders are an increasing problem in global healthcare [4,5], both in prevalence and morbidity degree of disorders. Therefore, it is important to invest in prevention programs to help adolescents cultivate a healthy body image, as well as early intervention programs to improve detection rates and better treatment outcomes [6].
DSM Diagnose criteria
DSM V [7,8] considers in the section of Eating Disorders and ingestion of food, these following disorders:
Pica (Persistent eating of non-nutritive substances for a period of at least one month)
Rumination Disorder (Repeated regurgitation of food for a period of at least one month (Regurgitated food may be rechewed, re-swallowed, or spit out)
Avoidant/Restrictive Food Intake Disorder (ARFID) not in AN or BM (An Eating or Feeding disturbance as manifested by persistent failure to meet appropriate nutritional and/or energy needs)
Then, DSM V goes on to consider the three most frequent disorders, which it classifies according to the following syndromes (a synthesis of the notes is presented, for further specification, we suggest to consult DSM V)
(Note: the nomenclature in parentheses corresponds to the ICD 10)
Anorexia nervosa
Persistent restriction of energy intake leading to significantly low body weight
Either an intense fear of gaining weight or of becoming fat, or persistent behavior that interferes with weight gain.
Disturbance in the way one's body weight or shape is experienced, undue influence of body shape and weight on selfevaluation, or persistent lack of recognition of the seriousness of the current low body weight.
Restricting type
Binge-eating/purging type
Regarding the current severity:
Mild: BMI ≥ 17 kg/m2.
Moderate: BMI 16 to 16.99 kg/m2.
Severe: BMI 15 to 15.99 kg/m2.
Extreme: BMI<15 kg/m2
Bulimia nervosa
The participating patients gave their written informed consent, and the study protocol was approved by the regional ethics committee at Ain Shams University and military hospitals.
Recurrent episodes of binge eating- An episode of binge eating is characterized by both of the following:
Eating, in a discrete period of time, an amount of food that is definitely larger than most people would eat during a similar period of time and under similar circumstances.
A sense of lack of control over eating during the episode.
Recurrent inappropriate compensatory behaviour in order to prevent weight gain, such as self-induced vomiting, misuse of laxatives, diuretics, or other medications, fasting, or excessive exercise.
The binge eating and inappropriate compensatory behaviours both occur, on average, at least once a week for three months.
Self-evaluation is unduly influenced by body shape and weight.
The severity is based on the frequency of inappropriate compensatory behaviors:
Mild: An average of 1 to 3 episodes of inappropriate compensatory behaviours per week.
Moderate: An average of 4 to 7 episodes of inappropriate compensatory behaviours per week.
Severe: An average of 8 to 13 episodes of inappropriate compensatory behaviours per week.
Extreme: An average of 14 or more episodes of inappropriate compensatory behaviours per week.
Binge eating disorder
Recurrent episodes of binge eating- These episodes are characterized by both of the following:
Eating, in a discrete period of time (e.g. within any 2-hour period), an amount of food that is definitely larger than most people would eat during a similar period of time and under similar circumstances.
A sense of lack of control over eating during the episode (e.g. a feeling that one cannot stop eating or control what or how much one is eating).
The binge eating episodes are associated with three or more of the following:
eating much more rapidly than normal
eating until feeling uncomfortably full
eating large amounts of food when not feeling physically hungry
eating alone because of feeling embarrassed by how much one is eating
feeling disgusted with oneself, depressed or very guilty afterward
Marked distress regarding binge eating is present
Binge eating occurs, on average, at least once a week for three months
As we have said, a new Disorder was introduced by DSM V: Avoidant/restrictive food intake disorder -ARFID- [9] and other disorders are under evaluation, such as Orthorexia Nervosa (restrictive diet, ritualized patterns of food intake and rigid avoidance of certain foods) [10].
DSM V also specifies other eating disorders or ingestion of unspecified and specified foods such as atypical anorexia nervosa, bulimia nervosa (low frequency and/or limited duration), binge eating disorder (low frequency and/or limited duration), purge disorder, nocturnal food intake syndrome. Currently, attempts are being done to define these and other disorders in a multidimensional way, including, among other aspects, psychopathology, neurobiology, psycho-sociology [11,12], as well as linking the emotional dysregulation of these cases with a history of child abuse at different levels [13].
For the practical purposes of this study and according to the prevalence of the different disorders, we will group the cases in AN, BN and others ED (OED) (all those disorders that are not AN and BN), even considering what Andersen said [14], who estimates that the overwhelming number of atypical cases suggests that the current diagnoses of anorexia and bulimia are too limited, defined by criteria based on research, or necessary additional hierarchies, which are currently catalogued by exclusion in those not specified cases. In addition, the incidence of comorbidity between eating disorders and personality disorders should be borne in mind.
Etiology
AN and BN are disorders related to an unknown ethology. Because AN and BN occur more frequently during adolescence in women, it is thought to be caused by cultural pressures that induce thinness, a common model in industrialized countries. However, AN and BN affect only a small percentage of the population at risk of these cultural models for several centuries, so the existence of biological and/or psychopathological vulnerabilities can be assumed [15,16], associated with a variable degree of alexithymia and hyperactivity [17,18].
From the neuropsychological point of view, patients with AN seem to show deficiencies of intentional, visuo-spatial and visuo-constructive type, while patients with BN mainly show some deficit in executive function. The fact that after treatment some patients show improvement in cognitive functioning may indicate, in some cases, that the deficits are functional. The lack of improvement in the cognitive functioning of some patients after various forms of intervention may suggest that these deficits precede the development of an eating disorder (AD) and therefore, can contribute both to their development and to a worse prognosis. A subgroup of patients can also show premorbid brain dysfunction and this may be one of the factors that indicate a worse prognosis [19].
Eating disorders appear to include changes in the neural systems that mediate the reward response, decision making and social behaviours. In such a way that treatments are likely to require individualization based on the specific constellation of the symptoms expressed for each patient [20].
The description of all these etiological theories would demand a greater extension than the present work range.
Comorbidity
In different studies, comorbidities have been found in variable percentages of ED patients, such as bipolar disorder, psychosis, substance and medication abuse, anxiety, mood disorders, insomnia and psychopathic personalities [21-26].
Physical clinical findings
The HEENT (head, ears, eyes, nose and throat), cardiovascular, abdominal and limb evaluations, including the neuromuscular evaluation, should be considered especially in the physical examination.
The ED are shown as emaciated with sunken cheeks, sallow skin, with low, normal or high weight. Make evident bradycardia, hypotension, hypothermia and orthostatic hypotension. The skin is dry, with or without lanugo, opaque or brittle hair, with changes in the nails, subconjunctival haemorrhage, and hypercarotenaemia, sunken eyes, dry lips, gingivitis, loss of the enamel of the teeth on the lingual and occlusal surfaces, dental caries, parotitis. General tissues’ atrophy, eventually prolapse of the mitral valve and/or arrhythmias.
Edema, calluses on the hands’ back (Russell's sign), acrocyanosis, Raynaud's phenomenon Trousseau's sign (test for hypocalcaemia is manifested by neuromuscular excitability) [27].
EA complications
AN complications
The most severe patients show loss of muscle mass, weakness, changes such as low heart rate, low blood pressure and low body temperature. Their extremities can be cold and blue and their skin pale or yellow, Sometimes hair loss from the scalp. Some patients develop lanugo in their torso and arms. Others show abdominal distension or constipation. The main concern is electrolyte variations and cardiac arrhythmias. Dehydration can be observed with abnormal blood levels of sodium and potassium. Those who vomit, using excessive laxatives or diuretics, are more susceptible to electrolyte problems. Patients who drink large volumes of water sometimes develop hyponatremia. The combination of hyponatremia and water intoxication reduces the threshold for seizures and coma and can be fatal. Serum phosphorus levels are typically normal in the first test, but may fall when the nutritional restoration begins, hypophosphatemia may contribute to "refeeding syndrome" characterized by cardiac arrhythmias, neurological changes and unexpected death. Patients usually have slow rest pulses and hypotension, even dizziness or fainting. An ECG that shows a prolongation of the QTc interval can be a precursor of ventricular arrhythmias and unforeseen death. Decreased red blood cells, white blood cells and platelets can also be observed. Leukopenia can increase the time required to heal from infections. With the nutritional restoration, blood cells usually return to normal. Slow growth and short stature can be observed, if the condition begins during the pre and post pubertal stage of physical development. Amenorrhea, one of the defining characteristics of AN, occurs as a result of poor nutrition, during intense exercise, low weight, reduction of body fat and psychological stress. The most serious consequence of amenorrhea and the concomitant decrease in estrogen is osteopenia, which may develop soon after the onset of AN.
Purge complications
Purging through self-induced vomiting is a common way to eliminate calories in BN and AN. Often, people who purge alternate between periods of food restriction, bingeing and purging. The purge often begins with a binge, which can be triggered by distress.
Common laboratory findings related to self-induced vomiting include hypokalaemia, mild ST segment changes, and metabolic acidosis or alkalosis. The chronic regurgitation of gastric contents can lead to an alteration of the teeth’s enamel that can be observed after two years of bingeing and purging; swelling of the parotid glands, soft palate lesion, dry skin due to dehydration, electrolyte imbalance, edema, gastrointestinal problems and an irregular menstrual cycle. As in vomiting, the use of laxatives or excessive exercise can become an addictive cycle.
Excessive exercise can play an important role in the development and/or maintenance of eating disorders. High levels of exercise reduce calories, suppress appetite and increase physical performance in sports.
EA progression
The progression of the AN over time is very variable. Some anorexics recover completely after an episode of the disease, others return intermittently to a normal weight and then relapse, but some subjects, after a chronic course of insidious symptoms for many years, often end in death, which is frequently the result of the physical complications of starvation, electrolyte imbalance, or suicide.
Not much is known about the course of untreated BN. Some subjects may have periods of spontaneous improvement and then a relapse. Others follow a more chronic course, in which the symptoms worsen, becoming enriched over time [28].
The standardized mortality rate (SMR) is high in patients with anorexia nervosa, ranging from 1.36 for women from 20 years old to less than 1.00 for women of 30 years old or more. SMR for patients with bulimia nervosa is not significantly different from the expected rate in the general population [27].
Treatments
First of all, we must consider that the treatment of EA is a challenge, because there are few evidence-based treatments, and the understanding of the mechanisms involved that lead to a sustained recovery is limited [29]. We must bear in mind that there is no consensus or recommendation based on evidence about the most effective way to achieve nutritional rehabilitation, as well as an adequate determination of an target weight.
On the other hand, and despite the fact that family-based treatment (FBT) is recommended as the treatment of choice in adolescents with AN, there is a shortage of European studies on the availability and efficacy of it.
Finally, there is an urgent need for new common research efforts to establish more evidence-based clinical guidelines and recommendations for practice areas in the treatment of adolescent AN [30]. The present study is oriented to this matter.
Medical evaluation and treatment
A general medical and psychiatric assessment of the baseline should be made at the time of diagnosis, and later periodically. It is necessary to monitor the physiological and psychological signs of eventual relapses, such as changes in weight, blood pressure, pulse, cardiovascular or metabolic status, or suicidal ideation and planning, and other impulsive and compulsive behaviours, such as self-harm. Although complications that threaten the patient life require hospitalization, most complications are resolved when healthy eating habits are restored and a normal weight is reached. Patients with binge eating disorder may require treatment on the complications associated with overweight or obesity. Osteoporosis may remain a medical concern, especially for patients with anorexia as dental erosions are seen more frequently in patients with bulimia but, are a preoccupation for any patient with purging of vomiting.
Behavioural interventions
Behavioural interventions for the treatment of ED [31] help patients change their unwanted behaviours (for example, binge eating, purging, restricting food intake) and thoughts (for example, the negative image of the body, negative selfevaluation, perfectionist thinking). A first step in the treatment is to assess the patient's motivation for change. Patients with ED are often ambivalent about changes, but the interdisciplinary team may be able to consistently increase their motivation. Cognitive behavioural therapy (CBT) and more specifically dialectical behavioural therapy (DBT), are the interventions of choice for Binge Eating Disorders, they are focused on the teaching of emotional regulation skills [32]. It should also include a guided program of self-help and health education for patients and their families.
Psychotherapy in BN
CBT and other psychotherapies, such as interpersonal therapy, are effective in the treatment of patients with bulimia nervosa.
Psychotherapy in AN
Patients with anorexia nervosa usually require very specialized outpatient treatments, from primary to tertiary healthcare strategies, hospitalization can even be indicated in severe anorexia. Multiple and combined behavioural interventions are used (e.g. CBT + family therapy + psychoeducation)
The cognitive-relational model of AN that includes the concepts and constructions related to cognitive, socio-emotional and interactional personal relationships, clearly defines the main strengths and vulnerabilities in the emotional and social processing of AN, considering Predisposing Factors (increase from) to
Insecure attachment
Sensory stress/negative emotion
Focus on the details
And decrease of the set variation
All this precipitate the factors of anorexia nervosa interact with each other by potentiating:
Increased anxiety/frustration
Decreased enthusiasm, increased criticism, increased overprotection, increased comfort and permissions
Increase of anorexic behaviours [33,34]
Family-Based Treatment (FBT) is also recommended for young people of all stages from pre-puberty to adolescence, through the use of focus groups and individual interviews [35].
Pharmacotherapy
Binge Eating Disorder- Patients may benefit from treatment with second-generation antidepressants-particularly fluoxetine, lisdexamfetamine, topiramate, and CBT (Behavioral Cognitive Therapy) [36]. There are also reports of the use of other SSRIs; for example sertraline, citalopram, tricyclic antidepressants (for example imipramine) and atomoxetine, which showed moderate evidence of the effectiveness.
BN
The efficacy of antidepressant agents in the treatment of BN symptoms has been systematically studied and the combination of CBT plus medications has shown benefits in restoring patients. Recommended as first line agents due to its efficacy and safety profile: Fluoxetine, is the only agent approved by FDA (Food & Drugs Administration) for the treatment of eating disorders, especially for BN. In binge eating disorder, higher doses of SSRIs may be more effective in the treatment of bulimic symptoms. Additional agents that look promising include topiramate and ondansetron.
AN
Antidepressant medications for the treatment of anorexia nervosa have limited efficacy and should not be the only treatment, often requiring the addition of antipsychotics. The neuroleptic to be used should be carefully selected, since side effects such as sudden and significant weight gain may contribute to patient abandonment of treatment, as well as olanzapine, which may be very effective if there is not a considerable increase in weight-patient education is very useful to provide patients and their families with education about the nature of the condition, and the treatment of eating disorders. In the case of children and adolescents, the family must always be included in the integral treatment [37].
Prognosis
Approximately 70% of people with bulimia nervosa and 27% to 50% of people with anorexia nervosa will not show evidence of a clinical eating disorder within 10 years of follow-up after receiving treatment at a third level of care [38]. The rest of the patients will have an erratic evolution with a subclinical evolution in many cases (although these values are very variable and depend on the expertise of the treatment team and the intensity and modality of it) maintain a subclinical eating disorder, or meet criteria for another eating disorder, however, the effectiveness of the treatments depends on a large extent of the therapeutic model and on the synergy and experience of the treating team. As shown in the following study by Golan et al. [39]. That describes a five-phase journey in the treatment of eating disorders, Preliminary phase (the choice of a refuge of understanding), Phase 1: partial recognition of the disease, Phase 2: recognition to erase the previous cognitive posture in the ED, Phase 3: towards the clear stance against the state of "patient", Phase 4: towards the re-authorship of life and the reself- management operation; Phase 5: towards recovery and maintenance. The results obtained according to Golan, in a longitudinal study of patients with severe and debilitating eating disorders treated with this approach, the dropout rate was less than 10%. This occurred during the first two months of treatment for people diagnosed with BN, and was higher than in people diagnosed with AN. At the end of treatment (15 months to 4 years later) up to 68% of those treated for anorexia nervosa and 83% of those treated for bulimia nervosa were fully recovered or with marked improvement [39].
Nutritional treatment
An ideal unit of hospitalization for inpatient eating disorder will have adequate dining space, so that patients can be controlled directly during meals. Day room areas should also be a part for on-site monitoring of patients by the nursing staff. A novel program has used switch controlled by an electronic key in the bathrooms so that patients can have privacy in the bathroom but must wait for a nurse to check the contents of the toilet before it is swept away.
Medical treatment and nutritional rehabilitation
In all treatments in general, medical management involves weight recovery, nutritional rehabilitation, rehydration and correction of blood electrolytes. It requires daily monitoring of weight and urine output, and frequent evaluation of electrolytes. The total number of calories in emaciated patients should begin with an intake of 30 to 40 kcal/kg/day and can be increased gradually if there is no evidence of peripheral edema or heart failure. Liquid formulas are an advantage, because they contain the necessary amount of vitamins and minerals and can be given in small amounts such as 6 equal feeds throughout the day. In this stage of treatment, blood hypophosphatemia can be developed during refeeding, which requires phosphate supplementation.
Bed rest may be necessary with assisted walks, accompaniment and special observation to avoid the development of pressure ulcers. Medications that prolong QTc intervals should be avoided. Occasionally, electrolyte disturbances may have to be corrected with intravenous solutions.
During outpatient treatment, patients should receive a nutritional counseling program with the development of meal plans appropriate to their BMI and age. At least one structured meal is advisable in these programs and nutrition counseling along with meal planning is structured in the context of group therapy or in specific individual counseling sessions, in which social skills training is also carried out, social anxiety, the distortion of body image, or their fears [4,5].
The nutritional objective would be to determine if the acquisition of body mass during refeeding is metabolically appropriate – earning an ideal achievement of approximately 20/80% to 25/75% fat in relation to lean body mass, measured by bio impedance BIA, method that is not always on hand, using indirect methods of measurement [40]. A caloric intake of approximately 1200 to 1500 kcal is usually recommended initially, with weekly increments of 500 kcal per day for outpatients to restore a weight of 0.5 to 0.9 kg per week [41,42].
It must be borne in mind that a very low BMI implies a worse prognosis and a higher cost of treatment [43].
The team must be aware of managing the pre, post and post meal moments [44].
Treatment levels and modalities
To describe the different levels, in which attention can be organized, we base on the scheme that the team of Pamela Williams of the American Academy of Family Physicians, adapted from Yager [28], that is organism from greater to lesser complexity in relation to the gravity of each case, according to the following objective parameters:
condition medical (ms - medical status),
suicidality (s),
percentage of healthy corporal weight (w - weight),
motivation for recover (mr),
comorbidities, (c)
structure necessary for eat or win weight (e - eating),
ability for check the practice compulsive of exercises (a - ability)
behaviour of purge (p - purging behaviour)
environmental stress (es - environmental stress)
availability geographical of a program of treatment (g)
To clarify, it is necessary keep always in mind that these patients could develop "excessive" membership to some treatment levels, especially those have residence or any kind of hospitalization. These would become an iatrogenic condition. Besides that, the emotional ambivalence of patient towards the healthcare team members and the clinic environment could work in a potentially protective way, more than harmful, favoring the recovery and the rehabilitation of the treated people [45].
Criteria of derivation to a level of treatment according to the complexity and gravity degree (from greatest to lowest degree).
Hospitalization
Preferably in specialized units, this level are scarce or nonexistent in Argentina and other countries because the really low ED prevalence. It must prepare ad-hoc a location to hospitalization in a general clinic or psychiatric unit (it depends on the EA component, in which case, was more organic or psychopathological).
ms. Adults: cardiac frequency<40 beats/minute; blood pressure <90/60 mmHg; glucose<60 mg/dl (3,33 mmol/l), potassium<3 meq/l (3 mmol/l); electrolytic imbalance, temperature<36.0°C (97.0°F), dehydration, hepatic, renal or cardiovascular dysfunction, bad controlled diabetes.
Children and teens: nightly cardiac frequency 40 beats/ minute; changes in the orthostatic blood pressure; blood pressure<80/50 mmHg; hypokalaemia, hypophosphatemia or hypomagnesaemia.
s. Plan or specific intent, and evident intention or planning.
w. Generally, <85% or acute weight decrease with the refusal to feed, even if it is not <85% of minimum body weight considered as healthy for her/his size and age.
mr: Motivation very poor or poor for recover; patient worried for intrusive and repetitive thinking; patient is not cooperative with the treatment or is cooperative only in a highly structured environment.
c. Any disorder psychiatric adjunct existing requires hospitalization and needs supervision during and after all meals or requires nasogastric feeding or special feeding.
a. It does not generally influence on the decision of hospitalization, except in case of a severe psychiatric symptom that would require hospitalization.
p. She/he needs supervision during and after all meals and in the bathrooms incapable of check daily multiple purge episodes that are serious and disabling, in spite of an appropriated test of ambulatory attention, even if laboratory parameters are normal.
es. Problems or conflicts with family, absence of family, inability to receive structured treatment at home, or patients that live alone without an adequate system of support.
g. The patient lives very far from the program of treatment locations, then she/he cannot attend it at home.
2. Residential treatment centre
ms. Medically stable (patient not requires intravenous fluid, feeding with NG tube, or multiple tests of laboratory daily) adults: cardiac frequency<40 beats/minute, blood pressure<90/60 mmHg, glucose<60 mg/dl (3,33 mmol/l), potassium<3 meq/l (3 mmol/l), electrolytic imbalance, temperature <36.0°C (97.0°F), dehydration, hepatic, renal or cardiovascular dysfunction, bad controlled diabetes.
s. Low or no risk.
w. Generally, <85%.
mr. Deficient reasonable motivation; patient worried for intrusive and repetitive thinking 4 to 6 hours/day, patient with a highly structured treatment.
c. If there is a presence of a comorbid disease, this not requires hospitalization.
e. Patient needs supervision at all meals.
a. Patient has relative external structure beyond self-control required for prevent to compulsive exercise compulsive.
p. She/he can ask and use the support from other people or can use acquired cognitive-behavioural tools, for inhibit the purge.
es. Idem 1.
g. Idem 1.
3. Partial hospitalization
ms. Medically stable. Idem 4 and 5
s. Idem 5, 4 and 2.
w. Generally,> 80%. Idem 4
mr: Partial motivation, although is cooperating, patient worried for intrusive and repetitive thinking>3 hours/day.
c. Idem 5, 4 and 2.
e. She/he needs some support for gain weight.
a. Idem 2.
p. Patient can strongly reduce incidents of purge in a not structured environment; without significant medical complications.
es. At its environment, there are some people capable to provide, at least, a limited support and a structure.
g. Patient lives close to treatment location. Idem 5 and 4
4. Intensive outpatient care
ms. Idem 5 and 3.
s. Idem 5, 3 and 2.
w. Idem 3.
mr. Appropriate motivation.
c. Idem 5, 3 and 2.
e. Self-motivated to gain weight. Idem 5
a. Idem 3 and 2.
p. Idem 3.
es. At its environment, there are some people capable to provide, at least, emotional support and appropriate contention, or environment has a low
es. Idem 5
g. Idem 5 and 3.
5. Ambulatory patient
ms. Idem 4 and 3
s. Idem 4, 3 and 2.
w. Generally, > 85%.
mr. Motivation sufficient and appropriate.
c. Idem 4, 3 and 2.
e. Idem 4.
a. Patient can handle the compulsive exercise compulsive thru on self-control.
p. Idem 4 and 3.
es. Idem 4.
g. Idem 4 and 3
Methods, Design, Settings and Patients
Population under study
In order to compare two treatment levels/modalities, in terms of efficacy, we designed a prospective study over 43 patients admitted to our institution and other ones, in Buenos Aires with the same treatment level/modality (IO) that were selected between January 1st and December 31st, 2016 and 33 patients at different locations in Buenos Aires, with modality PH, during the same period of time. Data was taken from clinical stories and institutional reports, the beginning of the treatment and the evolution of each of them until the indicated date.
Methods and settings
Female and male patients from 15 to 45 years old with diagnoses of AN, BN and others ED.
Statistical analysis
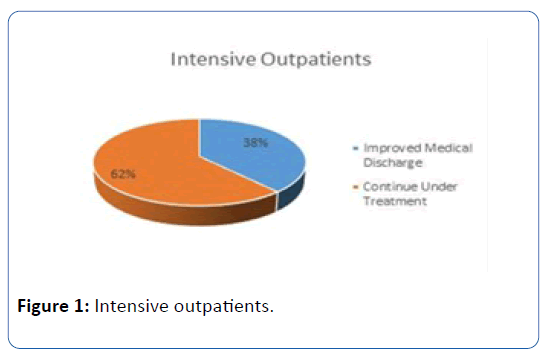
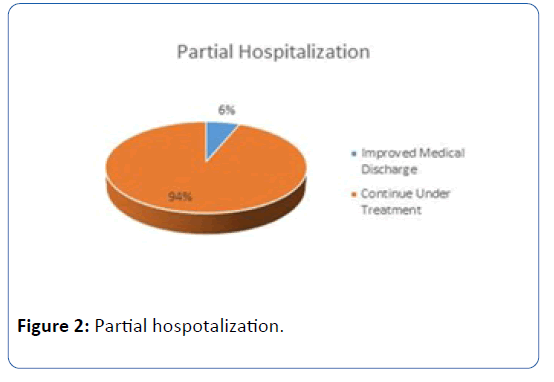
From the data analyzed it was observed that in the IO healthcare level/modality, of a group of 43 patients, 4 of them was derived to other healthcare level into the admission process. 39 started an IO treatment. 15 of them had improved medical discharges, and 24 patients continue under treatment. This corresponds to 38% of improved medical discharges in this type of disorder. On the other hand, in the PH healthcare level/ modality, from a group of 33 multi-centre patients taken from data of healthcare organizations, in the same period, only 2 patients had improved medical discharges and 31 other patients continued on PH treatment (Figures 1 and 2).
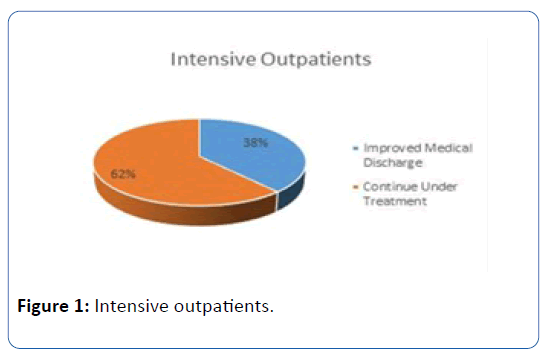
Figure 1: Intensive outpatients.
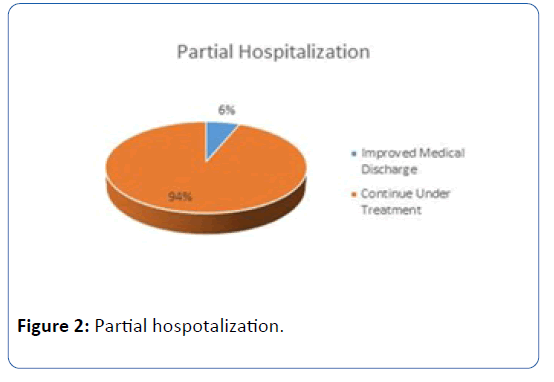
Figure 2: Partial hospotalization.
Results
We analyzed whether there were differences according to the treatment level/modality (IO and PH), about medical discharges that were given. For the calculation the Chi-Square Test was used and the magnitude of the effect was calculated by Phi. A statistically significant difference was obtained in the number of improved discharges according to the treatment level/modality used [Chi-squared with continuity correction (1)=8.685; p=0.0015 (unilateral)]; being the IO level/modality the one that had highest amount of discharges, as it was assumed. The percentage of variance taken from the treatment modality was 14.44%, calculated from the value of Phi=0.380 (Tables 1-3).
| Variables |
Treatment Level /Modality |
Total |
| IO |
PH |
| Medical Discharges |
Improved Discharges |
Count Treatment |
15 |
2 |
17 |
| Level/Modality % |
38.50% |
6.10% |
23.60% |
| Continue Under Medical |
Count Treatment |
24 |
31 |
55 |
| Level/Modality % |
61.50% |
93.90% |
76.40% |
| Total |
Count Treatment |
39% |
33 |
72 |
| Level/Modality % |
100% |
100% |
100% |
Table 1: Medical discharge contingency & treatment level/modality.
| Variables |
Value |
DF |
Asymptotic sig. (Bilateral) |
Exact sig. (Bilateral) |
Exact sig. (Unilateral) |
| Pearson’s Chi-Square Test |
10.404 |
1 |
0.001 |
- |
- |
| Continuity Correction |
8.685 |
1 |
0.003 |
- |
- |
| Fisher’s Exact Test |
-- |
- |
- |
0.002 |
0.001 |
| Valid Cases N |
72 |
- |
- |
- |
- |
| 0 cells (0%) have an expected frequency of less than 5. The minimum expected frequency is 7.79 |
Table 2: Chi-square test.
| Variables |
Value |
Sig. approximate |
| Nominal by nominal Phi |
0.38 |
0.001 |
| Valid Cases N |
72 |
- |
Table 3: Symmetric measurements.
Discussion
Since expositions of our labour in academic forums, new questions have emerged, one of them and perhaps the most important one, how long is the treatment in each patient? We can say, from our experience, that the duration varies according to each patient. However, it can be observed that after a specific diagnosis was made by an expert team, the treatment times were shorter. In some cases, patients are derived from PH or another healthcare level, in most cases, the patient is derived to IO treatment level/modality. At this level, generally, the treatment time could vary from 8 encounters to 1.5 years of treatment. Another interesting question that appears is how often must the patient attend the institution? We can say that treatments vary from 2 to 4 times a week, 1 to 3 hours a day. In addition, the sequence of attention with the different professionals is irrelevant for the patient's evolution [46-51].
Another issue to be addressed, which emerged like an observation, is to consider a healthy eating plan at the discharge of each person in particular, without going to extremes, which could also be harmful to their health.
Strengths, Limitations and Conclusions
The IO treatment is an outpatient treatment in which the patient, in a comprehensive, intensive and personalized way, is treated on the same day by different specialists, who make up the IO Team (Psychiatry, Clinical Medicine, Psychology, Nutrition, Family, Group and Workshops). This modality enhances the treatment and makes it effective. Due to it is an intensive and comprehensive processing, it produces better and faster evolution for the patient, towards a period of maintenance and subsequent improved medical discharge, in substantially less time than the PH treatment [52-57].
One important element that provides differential value in IO healthcare level/modality (opposite to the PH level/modality) is how the patient motivation is relevant in both, the diagnosis and the treatment.
The determination about the patient motivation degree during a medical admission does not depend as much on the patient as the professional health team. The interdisciplinary team is able to consistently increase the motivation of the patient since the first interview and therefore measure the adherence degree and future positive response to treatment, which can have each patient, from the referral or admission interview to the healthcare level/modality [58].
On the other hand, for treatments to be effective, it is important that the patient should not feel totally comfortable and lodged by the therapeutic team, because this circumstance generally produces negative reactions in the ED patients evolution, as a secondary benefit of the disease. It is important to highlight that there is a bias, in this sense, in many health systems in Argentina and probably in other countries, and that the medical evaluators of the health system who do not notice or understand [59-61]. This ED features will continue to carry out improper and ineffective referrals to a healthcare treatment level or modality, that is not convenient for the patient with ED, as well as errors in the diagnoses, so the first medical evaluators in the line are not experts in relation to this disorder. Maybe the healthcare organization should have an external consultant team for these patients primary evaluation [62-65].
Another differential value provided by IO is a better Cost/ Effectiveness ratio, given the comprehensive and high-frequency treatment, effectiveness on the evolution of patients, who in a short time notice objective improvements, increasing their initial motivation for recovery and generating lower consumption of goods.
The present study shows that the most effective level/ modality of healthcare, in cases that have sufficient motivation for improvement and do not require hospitalization, is IO, which favourably affects the early positive evolution of the clinical picture, unlike what happens under the HD modality, which tends to institutionalization or significantly longer and more expensive treatments. In our experience, over 80% of recently diagnosed cases, could be referred to IO as a first treatment indication [66-69].
One of our hypotheses is the modality of attention in HD for ED, causes the patient to evolve slowly in his treatment, not because of the severity variable of his diagnosis, but an insufficient diagnostic evaluation at the beginning of the treatment, which could only consider syndromic data, without bear in mind the patients’ potential recovery and the initial motivation [70-74]. Also, it is probable that the patient referred to HD tends to reparentalize quickly in a negative way, as a pseudo-advantage, being in a therapeutic modality every day, thus diminishing his autonomy and motivation for recovery.
The patient could generate an inadequate adherence with the treatment and professionals, generating the belief that their improvement depends only on a sanitary team, which is offered to she/he every day of the week. It is likely that this is a determining factor in an unnecessary prolongation of the treatment.
HD, as a healthcare level/modality for TCA, when it is erroneously indicated, is significantly less effective and more expensive, both for the patient and for health organizations. Accordingly, IO should be the logical first referral intention in ED primary evaluators, in most cases that do not require hospitalization or residency.
Acknowledgments
Our special recognition to Veronica Vega PhD at UBACYT (Secretary of Science and Technology of University of Buenos Aires) for the contribution of important data and technical assistance for our present work, and to Juan Carlos Argibay Statistics Specialist for technical assistance at this field in the present paper.
21864
References
- Court JPM, Kaplan AS (2016) The disjointed historical trajectory of anorexia nervosa before 1970. Curr Psychiatry Rep 18: 10.
- Haler E (1992) Eating disorders- A review and update. West J Med 157: 658-662.
- Hotta M, Horikawa R, Mabe H, Yokoyama S, Sugiyama E, et al. (2015) Epidemiology of anorexia nervosa in Japanese adolescents. BioPsychoSoc Med 9: 17.
- Halmi KA (2009) Anorexia nervosa: An increasing problem in children and adolescents. Dialogues Clin Neurosci 11: 100-103.
- Halmi KA (2009) Salient components of a comprehensive service for eating disorders. World Psychiatry 8: 150-155.
- Kuek A, Utpala R, Yen Lee H (2015) The clinical pro le of patients with anorexia nervosa in Singapore: A follow-up descriptive study. Singapore Med J 56: 324-328.
- American Psychiatric Association (2000) Practice guideline for the treatment of patients with eating disorders. Am J Psychiatry 157: 1-39.
- Norris ML, Spettigue WJ, Katzman DK (2016) Update on eating disorders: Current perspectives on avoidant/restrictive food intake disorder in children and youth. Neuropsychiatr Dis Treat 12: 213-218.
- Koven NS, Abry AW (2015) The clinical basis of orthorexia nervosa: Emerging perspectives. Neuropsychiatr Dis Treat 18: 385-394.
- Wildes JE, Marcus MD (2013) incorporating dimensions into the classification of eating disorders: Three models and their implications for research and clinical practice. Int J Eat Disord 46: 396-403.
- Wildes JE, Marcus MD (2013) Alternative methods of classifying eating disorders: Models incorporating comorbid psychopathology and associated features. Clin Psychol Rev 33: 383-394.
- Racine SE, Wildes JE (2015) Emotion dysregulation and anorexia nervosa: An exploration of the role of childhood abuse. Int J Eat Disord 48: 55-58.
- Behar RA (2008) Eating disorders not otherwise specified, partial syndromes and subclinical disorders: A warning in primary care. Rev Med 136: 1589-1598.
- Kaye W (2008) Neurobiology of anorexia and bulimia nervosa purdue ingestive behavior research center symposium influences on eating and body weight over the lifespan: Children and adolescents. Physiol Behav 94: 121-135.
- Nowakowski ME, McFarlane T, Cassin S (2013) Alexithymia and eating disorders: A critical review of the literature. Int J Eat Disord 1: 21.
- Rikz M, Lalanne C, Berthoz S, Kern L, Godart N, et al. (2015) Problematic exercise in anorexia nervosa: Testing potential risk factors against different definitions, PLoS One 10: e0143352.
- Duchesne M, Mattos P, Fontenelle LF, Veiga H, Rizo L, et al. (2014) Neuropsychology of eating disorders: a systematic review of the literature. Rev Bras Psiquiatr 26: 107-117.
- McAdams CJ, Smith W (2015) Neural correlates of eating disorders: Translational potential. Neurosci Neuroecon 4: 35-49.
- Alvarez Ruiz EM, Gutierrez-Rojas L (2015) Comorbidity of bipolar disorder and eating disorders. Rev Psiquiatr Salud Ment 8: 232-241.
- Seeman MV (2014) Eating disorders and psychosis: Seven hypotheses REVIEW. World J Psychiatr 4: 112-119.
- Gregorowski C, Seedat S, Jordaan GP (2013) A clinical approach to the assessment and management of co-morbid eating disorders and substance use disorders. BMC Psychiatry 13: 289.
- Aspen V, Weisman H, Vannucci A, Nafiz N, Gredysa D, et al. (2014) Psychiatric co-morbidity in women presenting across the continuum of disordered eating. Eat Behav 15: 686-693.
- Wildes JE, Marcus MD, Crosby RD, Ringham RM, Dapelo MM, et al. (2011) the clinical utility of personality subtypes in patients with anorexia nervosa. J Consult Clin Psychol 79: 665-674.
- Wildes JE, Marcus MD (2011) Development of emotion acceptance behavior therapy for anorexia nervosa: A case series. Int J Eat Disord 44: 421-427.
- Williams PM (2008) Treating eating disorders in primary care. Am Fam Physician 77: 187-197.
- Kontic O, Trisovic M, Jorga J, Lakic A, Gasic MJ, et al (2012) Eating Disorders. Srp Arh Celok Lek 140: 673-678.
- Zerbe KJ (1993) The body betrayed: Women, eating disorders, and treatment. Washington, American Psychiatric Press. Carlsbad CA: Gurze Books.
- Herpertz-Dahlmann B, Annemarie VE, Castro-Fornieles J, Schmidt U (2015) ESCAP expert paper: New developments in the diagnosis and treatment of adolescent anorexia nervosa-a european perspective. Eur Child Adolesc Psychiatry 24: 1153-1167.
- Calugi S, Dalle Grave R, Sartirana M, Fairburn CG (2015) Time to restore body weight in adults and adolescents receiving cognitive behaviour therapy for anorexia nervosa. J Eat Disord 3: 21.
- Wallace LM, Masson PC, Safer DL, von Ranson KM (2014) Change in emotion regulation during the course of treatment predicts binge abstinence in guided self-help dialectical behavior therapy for binge eating disorder. J Eat Disord 2: 35.
- Treasure J, Palazzo Nazar B (2016) Interventions for the carers of patients with eating disorders. Curr Psychiatry Rep 18: 16.
- Treasure J, Schmidt U (2013) The cognitive-interpersonal maintenance model of anorexia nervosa revisited: A summary of the evidence for cognitive, socio-emotional and interpersonal predisposing and perpetuating factors. J Eat Disord 1:13.
- Dimitropoulos G, Freeman VE, Allemang B, Couturier J, McVey G, et al. (2015) Family-based treatment with transition age youth with anorexia nervosa: A qualitative summary of application in clinical practice. J Eat Disord 3:1.
- Berkman ND, Brownley KA, Peat CM, Lohr KN, Cullen KE, et al. (2015) Management and outcomes of binge-eating disorder. Comparative Effectiveness Review, No 160.
- Lindstedt K, Neander K, Kjellin L, Gustafsson SA (2015) Being me and being us- adolescents’ experiences of treatment for eating disorders. J Eat Disord 3: 9.
- Palavras MA, Hay P, Touyz S, Sainsbury A, da Luz F, et al. (2015) Comparing cognitive behavioural therapy for eating disorders integrated with behavioural weight loss therapy to cognitive behavioural therapy-enhanced alone in overweight or obese people with bulimia nervosa or binge eating disorder: Study protocol for a randomised controlled trial. Trials 16: 578.
- Golan M (2013) The journey from opposition to recovery from eating disorders: multidisciplinary model integrating narrative counseling and motivational interviewing in traditional approaches. J Eat Disord 1: 19.
- Saladino CF (2014) The efficacy of bioelectrical impedance analysis (BIA) in monitoring body composition changes during treatment of restrictive eating disorder patients. J Eat Disord 2: 34.
- El Ghoch M, Calugi S, Lamburghini S, Dalle Grave R (2014) Anorexia nervosa and body fat distribution: A systematic review. Nutrients 6: 3895-3912.
- El Ghoch M, Soave F, Calugi S, Grave DR (2013) Eating disorders, physical fitness and sport performance: A systematic review. Nutrients 5: 5140-5160.
- Toulany A, Wang M, Katzman DK, Akseer N, Coyte CP, et al. (2015) Cost analysis of inpatient treatment of anorexia nervosa in adolescents: Hospital and caregiver perspectives. CMAJ Open 3: e192-e197.
- Hage TW, Ro O, Moen A (2015) “Time’s up”- staff’s management of mealtimes on inpatient eating disorder units. J Eat Disord 3: 13.
- Eli K (2014) Between difference and belonging: Configuring self and others in inpatient treatment for eating disorders. PLoS One 9: e105452.
- Accurso EC, Fitzsimmons-Craft EE, Ciao AC, Le Grange D (2015) From efficacy to effectiveness: Comparing outcomes for youth with anorexia nervosa treated in research trials versus clinical care. Behav Res Ther 65:36-41.
- Bartholdy S, McClelland J, Kekic M, O’Daly OG, Campbell IC, et al. (2015) Clinical outcomes and neural correlates of 20 sessions of repetitive transcranial magnetic stimulation in severe and enduring anorexia nervosa (the TIARA study): Study protocol for a randomised controlled feasibility trial. Trials 16: 548.
- Brytek-Matera A, Rogoza R, Gramaglia C, Zeppegno P (2015) Predictors of orthorexic behaviours in patients with eating disorders: A preliminary study. BMC Psychiatry 15: 252.
- Cooper M, Kelland H (2015) Medication and psychotherapy in eating disorders: Is there a gap between research and practice?. J Eat Disord 3: 45.
- Fairburn CG (2008) Cognitive behavior therapy and eating disorders. New York: The Guilford Press.
- Fairburn CG, Cooper Z, Doll HA, O’Connor ME, Bohn K, et al. (2009) Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: A two-site trial with 60-week follow-up. Am J Psychiatry 166: 311-319.
- Ferguson CP, La Via MC, Crossan PJ (1999) Are SSRI’s effective in underweight AN?. Int J Eating Disord 25: 11-17.
- Fernandes Maranhao M (2015) The effects of repetitive transcranial magnetic stimulation in obese females with binge eating disorder: A protocol for a double-blinded, randomized, sham-controlled trial. BMC Psychiatry 15: 194.
- Grilo CM, Masheb RM, Wilson GT, Gueorguieva R, White MA (2011) Cognitive-behavioral therapy, behavioral weight loss, and sequential treatment for obese patients with binge-eating disorder: a randomized controlled trial. J Consult Clin Psychol 79: 675-685.
- Guerdjikova AI, Fitch A, McElroy SL (2015) Successful treatment of binge eating disorder with combination phentermine/topiramate extended release. Prim Care Companion CNS Disord 17: 2.
- Hötzel K, Brachel RV, Schlossmacher L, Vocks S (2013) Assessing motivation to change in eating disorders: A systematic review. J Eat Disord 1: 38.
- Jauregui-Garrido B, Jauregui-Lobera I (2012) Sudden death in eating disorders. Vascular Health Risk Manage 8: 91-98.
- Kawai K, Yamashita S, Komaki G, Shimizu M, Nakashima M, et al. (2014) The outcome of treatment for anorexia nervosa inpatients who required urgent hospitalization. BioPsychoSoc Med 8: 20.
- Lindvall Dahlgren C, O Ro (2014) A systematic review of cognitive remediation therapy for anorexia nervosa- development, current state and implications for future research and clinical practice. J Eat Disord 2: 26.
- Miller WR, Rollnick S (2012) Motivational interviewing: Helping people change. New York: Guilford Press.
- Minekatsu A, Takeda A, Nagashima K, Uehara R, Nemoto M, et al. (2011) Medical treatment for burn patients with eating disorders: A case report. Plast Surg Int: 370981.
- Mitchell JE et al. (2013) Biological therapies for eating disorders. Int J Eat Disord 46: 470-477.
- Prochaska JO, DiClemente CC (1992) Stages of change in the modification of problem behaviors. In Progress on behavior modification: 184-214.
- Robin AL, Gilroy M, Dennis AB (1998) Treatment of eating disorders in children and adolescents. Clin Psychol Rev 18: 421-446.
- Schmidt U (1998) Cognitive-behavior therapy for children and families. Eat Disord Obes: 292-294.
- Schlegl S, Quadflieg N, Lowe B, Cuntz U, Voderholzer U (2014) Specialized inpatient treatment of adult anorexia nervosa: Effectiveness and clinical significance of changes. BMC Psychiatry 14: 258.
- Crow S (2014) Treatment of Binge Eating Disorder. Curr Treat Options Psychiatry 1: 307-314.
- Varga M, Dukay-Szabo S, Tury F, van Furth EF (2013) Evidence and gaps in the literature on orthorexia nervosa. Eat Weight Disord 18: 103-111.
- Walsh BT (2002) Pharmacological treatment of anorexia nervosa and bulimia nervosa. Eat Disord Obes: 325-329.
- Walsh BT, Wilson GT, Loeb KL, Devlin MJ, Pike KM, et al. (1997) Medication and psychotherapy in the treatment of bulimia nervosa. Am J Psychiatry 154: 523-531.
- Weiss CV, Mills JS, Westra HA, Carter JC (2013) A preliminary study of motivational interviewing as a prelude to intensive treatment for an eating disorder. J Eat Disord 1: 34.
- Brownell KD (2000) The LEARN program for weight management. Am Health Pub Co.