Keywords
Intramuscular pethidine; Intramuscular morphine; Orthopedic population; Caribbean territory
Introduction
Opioids are usually divided into two main groups: endogenous e.g., morphine or synthetic e.g., pethidine.
Pethidine has traditionally been used as the strong opioid at Eric Williams Medical Sciences Complex in Trinidad. It is a synthetic opioid about one tenth as potent as morphine. The intramuscular dose is 50-150 mg every 3-4 hours. Hariharan et al. [1] identified in their study that pethidine was usually prescribed every 4-6 hours or every 6-8 hours with no set pattern in 2010, Pethidine is more lipid soluble compared to morphine, has an elimination half-life of two to four hours and duration of action of only two to three hours. Its increased lipid solubility means a more rapid onset of central nervous system effects and increased abuse potential with drug users. Time to peak effect is 30-50 minutes for intramuscular administration and duration of action is 2-4 hours. The lack of analgesic potency compared with morphine, its shorter duration of action, abuse potential and adverse effects with repeated doses would make a case against using it as the strong opioid for postoperative cases. However, Mac Pherson et al [2] verified it is the strong opioid of choice for cases of severe pain such as during sickle cell crisis which is common in the Caribbean. In this hemisphere, pethidine is traditionally used and administered by health care professionals (HCPs) intramuscularly. As the half-life is about two to four hours, it is usually prescribed every 4-6 hourly or 6-8 hourly.
Morphine on the other hand, is an endogenous opioid, ten times more potent than pethidine. The intramuscular dose is 0.10 mg/ kg, time to peak effect is 30-60 minutes, half-life is 2.5 hours and duration of action is 3-4 hours. At Eric Williams Medical Sciences Complex, it is usually prescribed as morphine 2.5 mg IM/ IV prn for breakthrough pain. It has a lower lipid solubility compared to pethidine and slower penetration of the blood brain barrier. Its main effects are mediated through MOP receptors which can cause nausea and vomiting, sedation, respiratory depression, reward and euphoria, urinary retention, biliary spasm. Morphine is a potent analgesic with good sedative and anxiolytic properties.
The notorious side effect profile of opioids has led to hesitancy by health care staff in administration of opioids due to emphasis on side effects rather than analgesic potential. The main purpose of this study was to evaluate whether intramuscular morphine was superior to intramuscular pethidine for postoperative pain.
“Pain is defined by the International Association for Study of Pain (IASP) as an “unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage” [3].
Allowing pain to persist postoperatively can lead to complications such as decreased vital capacity, alveolar ventilation, pneumonia, tachycardia, deep vein thrombosis, infection, hypertension, myocardial infarction and chronic pain syndromes (occurring in 10-50%) of patients [3,4].
The stress response to surgery is known to affect the entire body and peak during the postoperative period. There are increases in catabolic hormones with decreases in anabolic hormones.
Other complications of an exacerbated stress response include: decreased chest wall compliance, decreased tone of the gastrointestinal and urinary tracts, increased cardiac output and blood pressure, cardiac workload, metabolism and oxygen consumption.
Uncontrolled pain exacerbates the normal stress response resulting in increased rate of complications in high risk patients such as those with cardiac and pulmonary disease. Severe pain also causes reflex muscle spasms worsening the pain, especially in joint and spine surgery. This unrelieved pain results in immune, genetic and neural changes and can lead to chronic pain syndromes if not treated acutely [5].
Inadequate treatment of pain can lead to increased institutional expenditure due to delayed recovery and rehabilitation, delayed discharge from hospital, emotional anxiety, decreased mobility and patient dissatisfaction. Studies have also shown it has a direct effect on quality of life [6].
Many studies have used pain scales to assess the severity of pain in the postoperative period such as the Numerical Rating Scale (NRS), Verbal Rating Scale (VRS) and Visual Analogue score(VAS) [7,8]. The most commonly used scale was the Visual Analogue score, where the patient assessed his/her pain on a non-numeric scale. A mean score was used in these studies to assess severity of pain at rest, at movement at different time periods [6,9]. For this study the VAS was taken on Day 0, Day 1 and Day 2 at 8-hour intervals.
Currently, at Eric Williams Medical Sciences Complex (EWMSC) in the Orthopedic ward, a multimodal approach is used as their standard. Patients were prescribed Paracetamol 1 g orally every eight hours or Tramadol 50mg every 6 hours+ Diclofenac 75 mg- 100 mg IV (intravenous)/IM (intramuscular) every 24 hours, + pethidine 75 mg-100 mg IM every 4- 6 hours. For severe pain Pethidine 75-100 mg IM every 4-6 hours was given +- morphine 2.5 mg IM/IV for breakthrough pain.
Part A of the study compared the normal analgesic regime for severe pain on the orthopaedic ward, (mostly Pethidine group) to a mostly morphine group in which Paracetamol 1 g was given every 8 hours or Tramadol 50mg every 6 hours +Diclofenac 75 mg- 100 mg IV/IM every 24 hours +Morphine 0.10 mg/kg-0.15 mg/kg every 4-6 hours +-morphine 2.5 mg IM/IV for breakthrough pain.
The breakthrough dose of morphine at 2.5 mg IM/IV was subtherapeutic and incidentally no patients in the study received this dose of morphine for breakthrough pain. The study aim was to compare intramuscular doses of a mostly pethidine group versus a mostly morphine group in the Orthopedic population at EWMSC.
An observational study done by Hariharan et al. [1] in 2007 showed the most commonly prescribed opioid was pethidine (prescribed in 64% of trauma patients). Dosage patterns for pethidine were prescribed between 50-100 mg IV/IM with no correlation between dosage selection, route of administration and weight of the patient. It was observed that 73.7% of the patients weighing below 50 kg received 100 mg pethidine and those above 70 kg received 50 mg pethidine [1].
So far there has been a relative paucity of data comparing these two drugs as pethidine (meperidine) is very rarely used in USA or Canada. One study recommended the use of morphine instead of pethidine due to the unique side effect profile of pethidine. This included: serotonergic crisis, normeperidine toxicity, poor efficacy and multiple drug interactions [10].
Patient satisfaction with post-operative pain management depends on a number of variables including patients’ expectations, intensity of pain experienced, promptness of acute pain service response, effectiveness of treatment and healthcare professionals’ attitude.
Part B of the study evaluated patient satisfaction using a modified form of the Revised American Pain Society Patient Outcome Questionnaire designed to assess the quality of pain management among hospitalized adults [11]. It was clear from the findings of the study done on the adult General Surgical and Orthopedic ward in 2007[1], the median Visual Analogue Score was 6 in the Orthopedic group which indicated an inadequate level of analgesia. However, at this time multimodal analgesia was not predominant in the hospital.
The validated questionnaire (based on American Pain Society) taken from the ASSIST trial [12] in India was administered over a postoperative period of three days, where 88.4% of patients had reported postoperative pain within the first 24 hours after surgery (Cardiovascular surgery, Gastrointestinal, Orthopedic), with patients in the Orthopedic category having the least pain after 24 hours [13]. The questionnaire was administered to patients seventy-two hours after surgery or on the last day before discharge.
Literature Review
Poor management of acute post-operative pain can lead to complications such as pneumonia, deep vein thrombosis, infection and delayed healing as well as the development of chronic pain [3]. This adds to the cost of stay in an already burdened healthcare system. It is therefore imperative that patients who undergo surgery should receive appropriate pain management [14,15].
According to Coluzzi et al. [3] between 10-50% of patients develop chronic pain after various common operations. Evidence collected by Sommer et al. [16] who assessed 1490 surgical inpatients three times a day using a visual analogue scale (VAS) found that moderate to severe pain was experienced by 41% of patients on day 0, 30% on day 1, 19% on day 2 and 16% on day 3. There was also a high prevalence of moderate to severe pain in back/spinal surgery patients (30-64%) on days 1-4.
Pain is considered the fifth vital sign, and unfortunately not assessed or charted on the ward. Too often analgesia is administered only when the patient complains. Universally, one-dimensional tools are often used in the assessment of pain e.g. the Numerical Rating Scale (NRS), Verbal Rating Scale (VAS) and the Faces Pain Scale-Revised.
Patient outcome questionnaires (POQ) have become the mainstay of assessment of quality of care. The American Pain Society [11] developed a standardized questionnaire which was adapted by the ASSIST Trial in India [12] for measurement of quality of pain control. Since it was a validated questionnaire, it was implemented in this study to assess patient satisfaction as a measurement of quality of pain control. The most commonly used pain assessment tools for acute pain in clinical and research settings are the Numerical Rating Scale (NRS), Verbal Rating Scale (VAS) and the Faces Pain Scale-Revised. The VAS and NRS are equally sensitive and were found to function best for patient’s subjective feeling of the intensity of pain by the American Pain Society.
In 2003, Bardieau et al. [8] conducted a study to identify whether institution of a formal acute pain service resulted in reduced Visual analogue scores of patients undergoing different categories of surgery. Orthopedic surgery was classified under survey 1, which had the highest area under the curve, or the highest pain scores. After institution of a protocol, there was a significant reduction in postoperative pain scores (31% to 18%) having VAS score >3.
In this same study by Bardieau et al. [8], 86 questionnaires about knowledge and skills towards postoperative pain were distributed. This survey identified a lack of knowledge and skills among nurses in assessing and managing pain effectively because of absence of guidelines and treatment protocols. It also identified concerns and fears about side effects, tolerance and addiction to morphine.
As outlined by Gould et al [7] VAS scores after 24 hours were used to assess pain in minor, intermediate and major general surgeries. This was a widely used and validated scale. The authors found a significant improvement in VAS scores after institution of an acute pain protocol.
Hariharan et al. [1] evaluated prescription patterns at Eric Williams Medical Sciences complex in Trinidad in 2020. A Mc Gill Pain questionnaire and VAS was implemented. Results showed that pethidine was most commonly prescribed (64%) followed by diclofenac 17% and tramadol 12%. There was actually no real pattern to the frequency of dosage for pethidine. Although morphine was available, pethidine was the opioid of choice. The intramuscular route was also the most favoured with 62% of the patients receiving via the intramuscular route and 31% of patients receiving via the intravenous route. The median visual analogue score was 6. The majority of patients were trauma and orthopedic patients which indicated that these patients experienced a moderate amount of pain.This study chose to extrapolate on this previous study done by Hariharan et al. [1] and compare what was the normal practice (intramuscular pethidine) to intramuscular morphine using a standardized multimodal approach in the orthopedic population.
VAS scores were used as a unidimensional tool to assess pain score during 8-hour periods on the ward as this was the most popular scale used in most studies and easiest to implement. An even better multidimensional tool used to assess the quality of pain control made by the American Pain Society [11], adapted by the ASSIST trial [12].
There was a relative paucity of data on PUBMED concerning comparison of intramuscular pethidine/meperidine to morphine for postoperative patients. The intramuscular route is not considered popular in most first world countries, but favoured in third world countries with low resources. Most of the articles centered on treatment of acute pain in the emergency setting (labour analgesia and renal colic) or treatment of chronic pain.
Rahman et al. [17] compared intramuscular morphine and intramuscular pethidine for postoperative analgesia in major abdominal surgery. Researchers found that the side effect profile morphine and pethidine were similar. Respiratory depression, cough suppression, nausea and vomiting, urinary retention and constipation were the most frequent side effects. Rahman et al. [17] also found VAS scores and patient satisfaction scores were also similar between groups. This would make a strong advocacy for the use of morphine instead of pethidine as morphine is ten times more potent than pethidine and has longer duration of action. In our population the incidence of renal impairment is high and pethidine is contraindicated in renal failure and the elderly, so this would make a strong advocacy for a change to morphine.
Most of the evidence was found in articles pertaining to labour analgesia. Wee et al. [18] compared intramuscular diamorphine and intramuscular pethidine which showed diamorphine provided modestly improved pain score (0.7) compared to pethidine, however diamorphine increased the duration of labour by eighty-two minutes. This study aimed to fill this wide deficit in knowledge concerning the comparison of intramuscular pethidine and intramuscular morphine as it is not commonly administered via this route worldwide for postoperative analgesia.
O’ Connor et al. [19] compared the efficacy and safety of morphine and pethidine for renal colic. They found no difference in efficacy, safety profile or patient satisfaction with the two opioids and due to the issues surrounding pethidine: increased central excitation, metabolites excreted in the urine, worsening renal failure and contraindicated for use in the elderly, morphine was advocated as the drug of choice.
The main aim of this study is to assess whether morphine is superior to pethidine with respect to post-operative analgesia, patient satisfaction and side effect profile.
Aims and Objectives
Null hypothesis: Patients who received intramuscular pethidine had better pain scores compared to those who receive an equipotent dose of intramuscular morphine
Part A of the study
Aims:
To determine whether substituting an equipotent dose of intramuscular morphine for intramuscular pethidine resulted in a decrease in Visual Analogue Score of 15%
Objectives:
• Using standardized conversions, an equipotent dose of Morphine was substituted for Pethidine as the strong opioid in the post-operative plan. Patients were then grouped into a mostly morphine group and a mostly pethidine group
• Visual Analogue Scores were recorded using a standardized questionnaire to these two groups during 8-hour periods until postoperative day 2.
• At the end of the 3-day period the following were recorded: time to mobilization, time to oral intake and time to first bowel movement.
• Incidence of adverse side effects was also recorded: nausea and vomiting, desaturation, constipation was also recorded at the end of the 3-day period
Part B of study
Aim
To determine whether patients were more satisfied with morphine compared to pethidine as the strong opioid using a standardized questionnaire
Objectives
• To determine the quality of pain control using a standardized patient satisfaction survey
• To determine the incidence of common side effects attributed to opioids
Methodology
Setting
Approval was obtained by University Ethics Committee and North Central Regional Health Authority for conducting the study. This was a Prospective Randomized Controlled Study. The study was a single-blinded study. Data was collected from the period of May to December 2018 (thirty-two weeks) in the adult Orthopaedic wards of the Eric Williams Medical Sciences Complex, a tertiary teaching institution in Trinidad.
Using the ClinCalc online sample size calculator at http://clincalc.com, using continuous means by which the primary end point is an average.
Using the values from the ASSIST trial in India [12], the anticipated means in Group 1 :74 +/- 15 and aiming for a decrease in VAS SCORE by 15%, then group 2 :60, with a p value of 0.05 and power of 80%.
The number needed to treat was calculated to be 36.
If 40 patients are obtained, the aim would be for 20 patients in the treated vs. the non-treated group.
The primary outcome of this questionnaire was to assess whether substitution of intramuscular pethidine for morphine will result in a decrease in VAS score of 20%.
Inclusion criteria
• Patients undergoing orthopedic surgery only
• Patients undergoing elective surgery
• Adults >18 years
Exclusion criteria
• Patients who have contraindications to NSAID or opioid use-Asthmatics, Creatinine >1.0, known allergies, heart failure, or adverse reactions to opioids
• Patients who have chronic pain (persistent pain for >3 months)
• Patients who have decreased cognitive function- MINIMENTAL score <24 (impaired cognitive function)
• Pregnancy
• Patients who are institutionalized e.g., prisoners
For this study a total sample size of 75 patients was collected, with 3 patients who were excluded for impaired cognitive function, (defined as a Minimental Score <24). One patient was excluded for issues with visual acuity.
The lists were obtained the night before surgery and all the patients were randomly assigned using an electronic app (www.random.org) to either a mostly morphine group or a mostly pethidine group. A postoperative analgesic plan was discussed with the surgeon regarding the therapeutic dose of opioid to be prescribed based on the weight of the patient.
In the postoperative plan, the Orthopedic surgeons prescribed multimodal analgesia in the following manner: Paracetamol 1 gram po q 6hrly or Tramadol 50 mg IV q 6hrly +Diclofenac 75 mg- 100 mg IV od + Pethidine (as strong opioid) 25 mg-100 mg q 4-6 hourly+-morphine 2.5mg IV for rescue OR Morphine (as strong opioid) 0.10-0.15 mg/kg q 4-6hourly +-morphine 2.5 mg IV for rescue.
Patients were assigned a code which was used to preserve anonymity which was only known to the investigator and kept in a code book along with the group to which the patient was assigned.
Visual analogue scores (VAS) capturing the severity of pain were checked during the first 8 hours after surgery and approximately 8 hours thereafter for 3 days (Day 0, 1, 2). The twenty- four (24) hour period was divided into 8-hour time zones as follows: midnight to 8am, 8am to 4pm, 4pm to midnight. VAS scores were done at rest and on movement (or coughing) each time and the patient was counselled on filling out the form each time.
Part A of study
The primary outcome was to evaluate whether the morphine group had a 15% decrease in VAS score compared to the pethidine group during the 8am-4pm period on Day 1 postoperatively.
On day 2, the Observation chart was checked over the 3-day period for any signs of opioid overdose such as respiratory depression (Sp02<90%, RR<8), hypotension or nausea/vomiting. Comparison was made between the mostly morphine group and mostly pethidine group.
Secondary outcomes which were evaluated was the incidence of common side effects of opioid use such as nausea, hypotension, decreased respiratory rate and decrease in saturation and whether these were significant between the morphine group and pethidine group. Additionally, other secondary outcomes evaluated were time to oral intake, time to mobilization and length of stay [20].
Inclusion criteria
• Patients undergoing orthopedic surgery only
• Patients undergoing elective surgery
• Adults >18 years
Exclusion criteria
• Patients who have contraindications to NSAID or opioid use-Asthmatics, Creatinine>1.0, known allergies, heart failure, or adverse reactions to opioids
• Patients who have chronic pain (persistent pain for >3 months)
• Patients who have decreased cognitive function- MINIMENTAL score < 24 (impaired cognitive function)
Part B of study
Part B of the study focused on patient satisfaction which was used as a marker to assess quality of care. A standardized survey based the Acute Pain Society [21] and adapted by the ASSIST trial [12] in India was administered to patients on day two postoperatively.
Eight questions were asked in the questionnaire which were graded on a scale from 0-10 from extremely dissatisfied to extremely satisfied. This questionnaire also identified pain which caused the patient to feel anxious, depressed, frightened, sleepless, and led to side effects (nausea, drowsiness, itching, and dizziness).
Inclusion criteria
All patients in the study were included
Exclusion criteria
None
Ethical considerations
Research participants were not in any way subjected to harm during the conduct of this research. This was continuous monitoring for the patient with a plan of action if SpO2 < 90% and RR< 8.
Full informed consent was taken from each participant and each participant was allowed to withdraw at any time
A code was assigned to each participant to protect patient privacy, anonymity and confidentiality
Results were stored on a password protected computer owned by myself, the conductor of the research project
Statistical Issues
Pearson’s correlation was used to assess the relationship between variables
Levine’s test of homogeneity was used to evaluate homogeneity amongst variables
An ANOVA test was done to assess the difference between the morphine and pethidine groups
Results
Part A of study
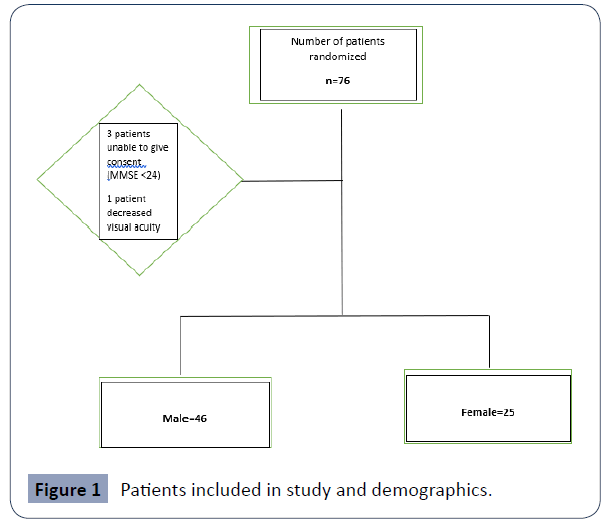
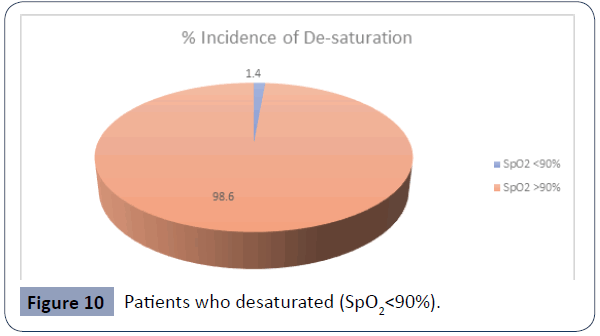
A total of 75 patients were enrolled in the study during the period of May to December 2018. Four patients were excluded from the study: one (1) for issues with visual acuity and three (3) for cognitive impairment i.e. Minimental score (MMSE)<24. There were no patients who were under 16 years old and no institutionalized patients enrolled in the study (Figures 1 and 2).
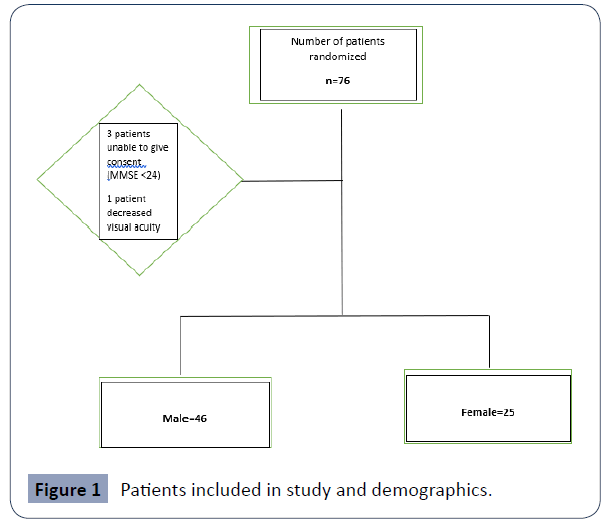
Figure 1 Patients included in study and demographics.
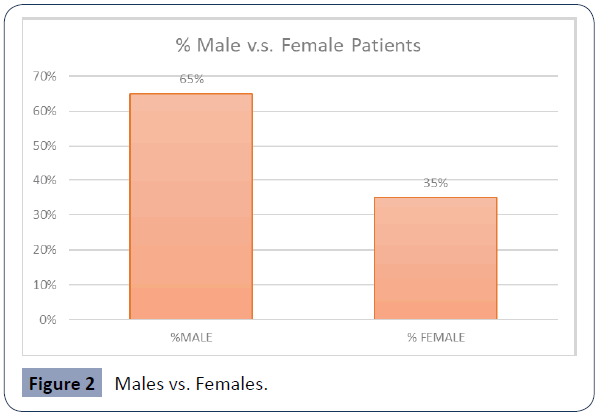
Figure 2 Males vs. Females.
Of the seventy-one (71) patients included in the study, the majority were male 46 (65%) vs. female 25(35%) which represented a ratio of 1.84: 1 male to female. The average age of those enrolled was 49.2 years (Figure 3) (Table 1).

Figure 3 Types of Orthopedic Surgery classified by part of the body.
| Type of Surgery |
No. of Patients |
| Hemiarthroplasty |
3 |
| Dynamic Hip Screw (DHS) |
6 |
| Lower Limb Femur |
15 |
| Lower Limb Tibia/Fibula |
17 |
| Upper Limb Humerus |
3 |
| Upper Limb Ulnar/Radius |
6 |
| Shoulder |
3 |
| Ankle |
1 |
| Metatarsals/Metacarpals/Tendons |
10 |
| Spine |
5 |
| Clavicle |
2 |
| Total |
71 |
Table 1 Patients and Type of Surgery.
Types of orthopedic surgeries were categorized based on part of the body. Lower limb surgeries were by far the most common (32 cases), followed by small bones of hands and feet/tendon surgery (10 cases), then upper limb surgeries (9) cases.
PART A, aim 1 was to determine whether substituting intramuscular pethidine for an equipotent dose of intramuscular morphine resulted in a decrease in VAS score of 20% (Table 2).
Average VAS Score (Rest)
Day 1 (8am-4pm) Morphine |
Average VAS Score (Rest) Day 1 (8am-4pm) Pethidine |
Difference |
% Decrease In Vas With Morphine |
| 3.51 |
4.11 |
0.6 |
14.5 |
Table 2 Table showing % Decrease in VAS Score in Patients assessed on Day 1 between 8am to 4pm (at Rest).
The average of the VAS scores was taken on postoperative day 1 during the period 8am to 4pm when patients were at rest. Mean VAS at rest for pethidine was 3.51 and Mean VAS at rest for morphine was 4.11. The percentage decrease in VAS score at rest with morphine was 14.5%. Therefore, the null hypothesis was not satisfied as significance was taken at 20% (Table 3).
Average VAS Score (Movement) Day 1
(8am-4pm) Morphine |
Average VAS Score (Movement) Day 1
(8am-4pm) Pethidine |
Difference |
% Decrease In VAS Score With Morphine |
| 3.43 |
4.20 |
0.77 |
18.5 |
Table 3 Table showing % decrease in VAS score on day 1 during 8am-4pm on movement.
Reference made to Table 3: an average was taken of all the VAS scores on movement for the morphine group and for the pethidine group. Mean VAS on movement was 3.43 for morphine and Mean VAS on movement was 4.20 for pethidine. This represented an 18.5% decrease in VAS with morphine.
This was very close to 20% and whilst not significant enough to reject the null hypothesis, it was notable. This decrease VAS was close enough to 20%, assuming this would make a difference in overall patient satisfaction.
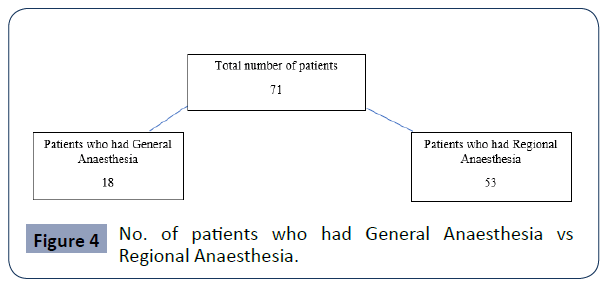
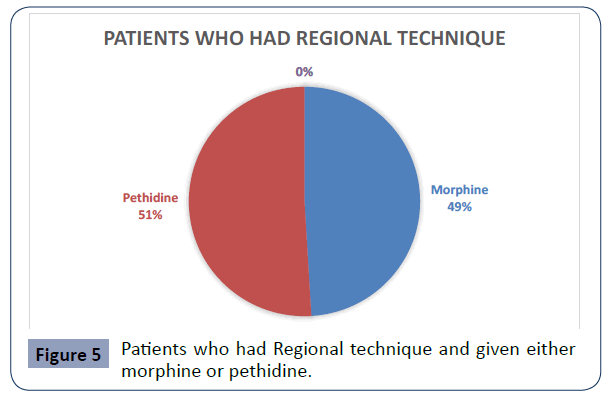
VAS scores were generally higher on Day 0 further indicating that any benefit conferred by Regional Block was not supported. No infusions on the ward were done for the 71 patients who entered into this study (Figures 4 and 5).
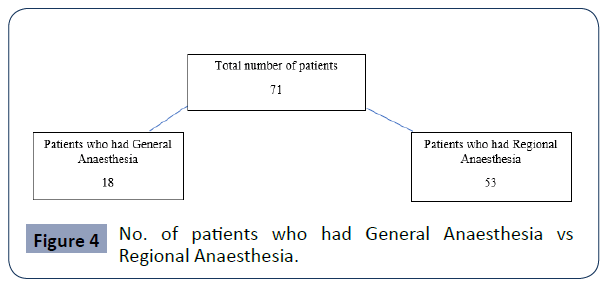
Figure 4 No. of patients who had General Anaesthesia vs Regional Anaesthesia.
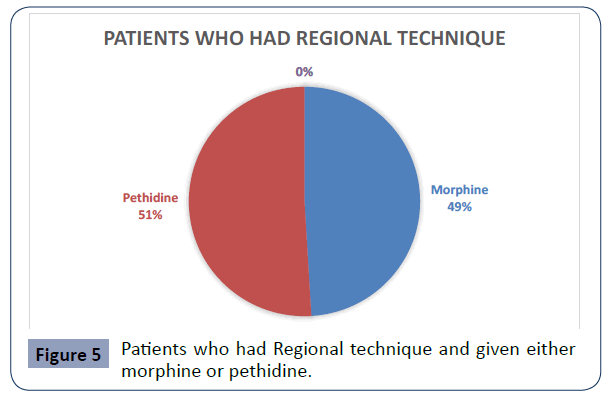
Figure 5 Patients who had Regional technique and given either morphine or pethidine.
Fifty-three patients (53) received regional anaesthesia and were given either morphine or pethidine post-operatively. From the pie chart in Figure 5, twenty-six (26) were given morphine vs twenty-seven patients (27) given pethidine.
Their mean scores were 1.22, 1.30 respectively indicating no difference between the two groups.
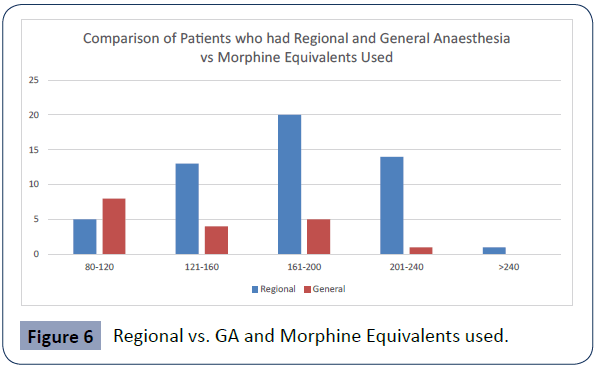
Figure 6 indicated that patients who underwent Regional Anaesthesia received more morphine equivalents than those who underwent General Anaesthesia. It can be concluded that the regional technique did not confer any benefit to the patient postoperatively and did not decrease the amount of opioid on the ward.
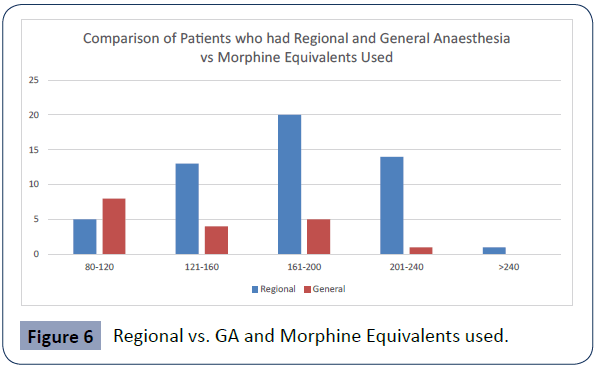
Figure 6 Regional vs. GA and Morphine Equivalents used.
From Figure 6 it was seen that 21 patients received 161-200 morphine equivalents, followed by 14 patients in the 201-240 category. This indicated that for orthopedic surgery, most patients received opioid in the higher range category on postoperative Day 1. This would indicate severe pain and high opioid requirement by these patients, especially after any regional had lost its effect.
Even though these patients received more morphine equivalents, the p value of the Chi Squared was 0.165 indicating no statistical significance between regional technique and morphine equivalents.
Phi and Cramer’s test was used to evaluate the association between morphine equivalents and side effects. Cramer’s V p value 0.165 indicating a very weak association indicating no statistical significance which reinforced the result from the Chi squared test.
PART B of the study was to determine the incidence of common side effects attributed to opioids.
In the descriptive analyses of side effects of opioid use, Pearson’s correlation was used to assess the strength of the relationship between morphine vs. pethidine and the incidence of side effects such as time to mobilization, length of stay, time to oral intake, saturation, respiratory rate, drowsiness, hypotension, nausea.
There was a strong positive correlation [r value of 0.751] between morphine and time to mobilization. This indicated that patients in the morphine group took a longer time to mobilize. Patients in the pethidine group took a shorter period of time to mobilize compared to the morphine group [r=0.751, n=71, p=0.000]
The other variables were negatively correlated with morphine and deemed statistically insignificant.
From Table 3, there was a negative correlation between pethidine and drowsiness [r=-0.357, n=71, p=0.002].Patients in the morphine group had suffered from drowsiness more often than the patients in the pethidine group.
There was a negative correlation between pethidine and twenty-four- hour (24 hr.) pain relief
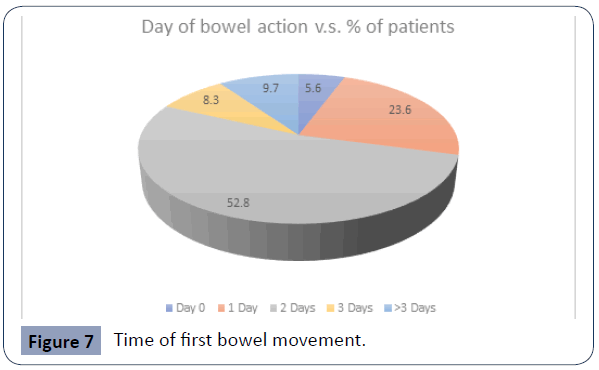
[r=-0.357, n=71, p=0.002]. Morphine provided better 24 hr. pain relief than pethidine (Figure 7).
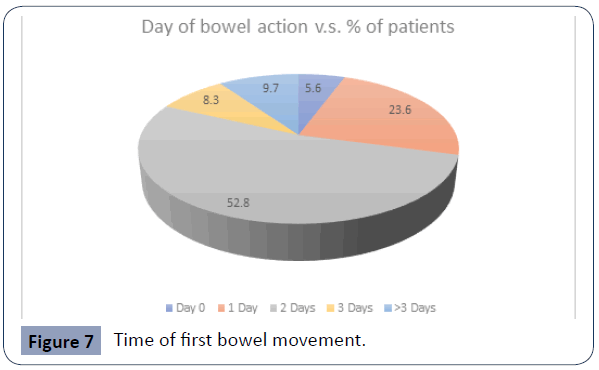
Figure 7 Time of first bowel movement.
Thirty-eight (38) had their first bowel movement on Day 2, followed by seventeen (17) on day 1. Seven (7) patients had first bowel movement after 3 days postoperatively. Most of the patients did experience some level of constipation after surgery (Figure 8).
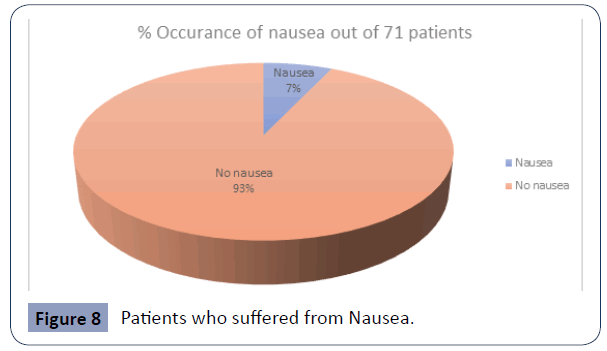
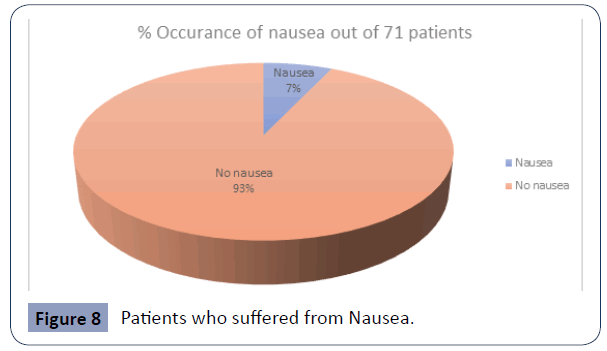
Figure 8 Patients who suffered from Nausea.
Approximately five (5) patients experienced nausea post operatively which represented about 7.0% of the study population. This represented a low incidence of nausea (Figure 9).
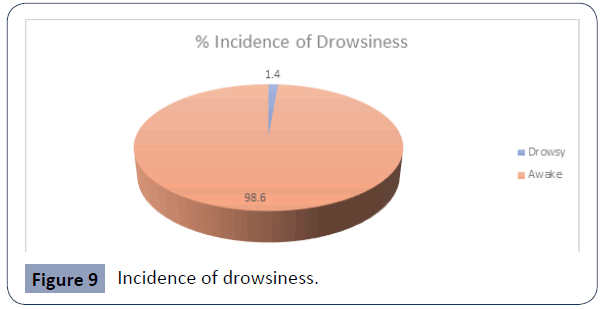
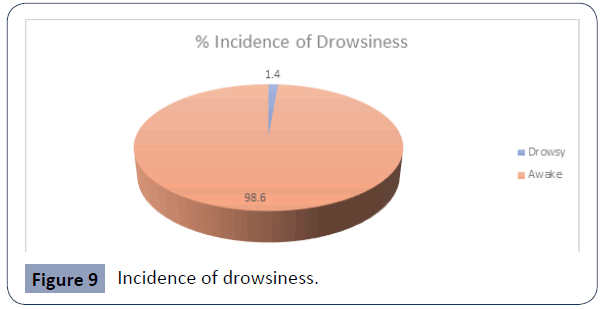
Figure 9 Incidence of drowsiness.
Only one patient suffered from drowsiness on the ward, which represented 1.4% of the study population (Figure 10).
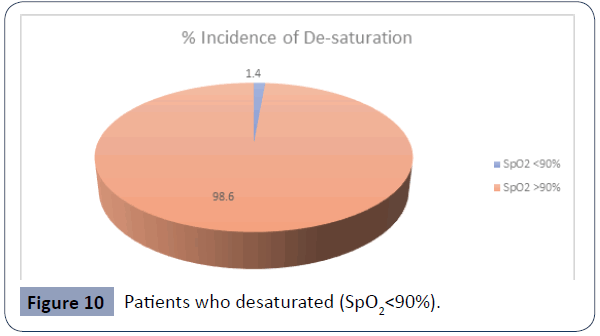
Figure 10 Patients who desaturated (SpO2<90%).
One of the most notorious side effects of opioid is respiratory depression leading to desaturation on the ward. During the trial, only 1 patient had desaturated on the ward (SpO2<90%). This patient was treated with oxygen therapy and the desaturation was transient.
From these results, it can be concluded that the side effect profile of opioids was limited. Constipation itself was not life-threatening.
There was an overall negative correlation between patient satisfaction and opioid use [r=-0.323, n=71, p=0.006]. The less opioid used the less satisfied was the patient. Therefore, the more opioid used, the more the patient was satisfied.
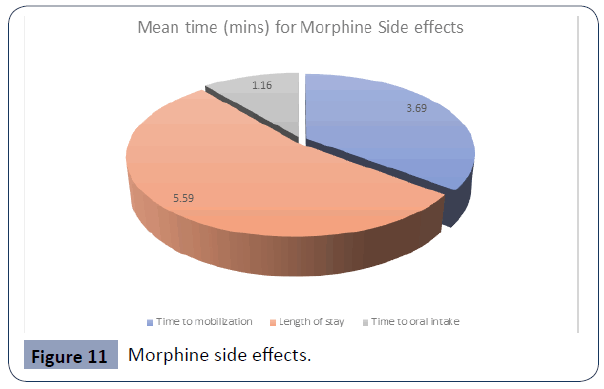
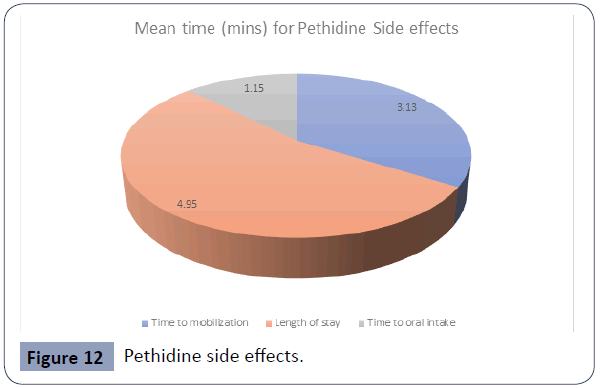
From Figure 11 and Figure 12 it can be shown that patients in the morphine group took longer to mobilize (Mean 3.69) than those in the Pethidine group (mean 3.13), however this difference was not significant.
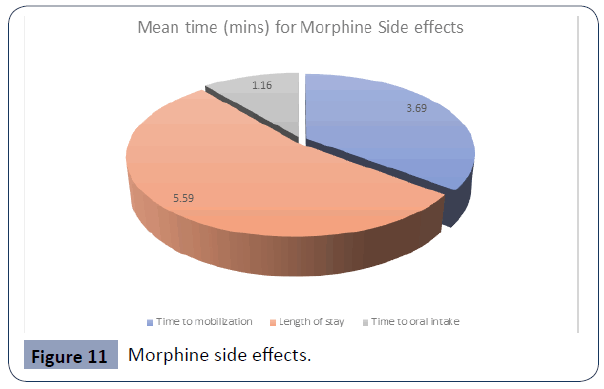
Figure 11 Morphine side effects.
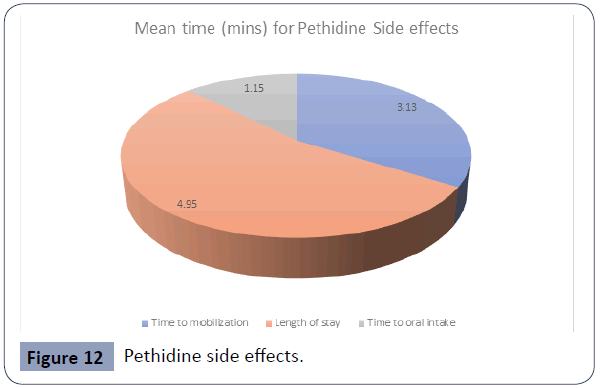
Figure 12 Pethidine side effects.
The length of stay was slightly different between the morphine group (Mean 5.59) vs. the pethidine group (Mean=4.95). This could be due to the increased time to mobilization due to the sedative effect of morphine.
Mean value of time to oral intake was almost the same between the morphine group (Mean=1.16) and the pethidine group (Mean=1.15)
In summary the secondary outcomes
1. Incidence of side effects- uncommon
• Most common was constipation (time to first bowel action was day 3 for most patients)
• Incidence of respiratory depression low (1.7%)
• Incidence of nausea (1.4%)
2. Time to oral intake- was the same between both groups
3. Time to mobilization-was slightly longer for morphine group
4. Length of stay- longer for morphine group
When the descriptive analysis of the side effect profile of Morphine and Pethidine was evaluated, it was clear that the means did not vary significantly between the two groups. It can be concluded that issuing morphine within the therapeutic range would benefit the patient as the side effect profile is safe.
A comparison was made between Mean VAS score in Males and Females at rest and on movement (Table 4).
| |
Mean VAS Score (Males) |
Mean VAS Score (Females) |
| Day 1 rest 2 |
3.76 |
4.00 |
| Day 1 move 2 |
3.76 |
3.96 |
| Overall satisfaction |
6.58 |
4.89 |
Table 4 Mean VAS Scores and Overall satisfaction according to Gender.
In the descriptive analysis looking at Mean VAS score at rest on Day 1 during the 8am-4pm shift, the Mean VAS score for males was 3.76 and for females 4.00, which was a small difference. Levine’s test F=0.001, (1,69)=0.970.
Mean VAS score on movement for males were 3.76 and for females were 3.96 which showed a negligible difference. Levine’s test F=0.045m (1, 69)=0.833.
Overall satisfaction for males was 6.58 out of 10 and for females was 4.89 out of 10. Levine’s test F=1.062 (1,70)=0.306
Using Levine’s test for homogeneity of Variances, all p values were >0.05 indicating the groups were homogenous.
Part B of Study
Part B of the study also included apatient satisfaction survey which was modelled on the ASSIST trial conducted in India [12] (Table 5). This was administered to patients on Day 2 postoperatively or on the day of discharge from the ward if it was less than 2 days. A score from zero to ten was recorded by the patient (a score of zero indicated that the pain did not interfere with certain activities and a score of 10 indicated complete interference with certain activities).
| No. |
Question |
Morphine (Mean Patient Satisfaction Score) |
Pethidine (Mean Patient Satisfaction Score) |
| Q.1 |
in the last 24 hours how much did the pain interfere or prevent you from doing activities in bed such as turning, sitting up, repositioning |
2.50 |
3.78 |
| Q.2 |
“in the last 24 hours, how much did pain interfere or prevent you from doing activities out of bed such as walking, sitting in a chair, or other activities |
2.60 |
3.90 |
| Q. 3 |
in the last 24 hours, how much did pain interfere or prevent you from sleep |
1.84 |
3.30 |
| Q.4 |
“in the last 24 hours, how much did pain interfere or prevent you from staying asleep |
1.56 |
2.85 |
| Q.5 |
How much did the pain cause you to feel? |
|
|
| i. Anxious |
0.91 |
1.58 |
| ii. Depressed |
0.60 |
1.19 |
| iii. Frightened |
1.03 |
1.83 |
| iv. Helpless |
0.20 |
0.56 |
| Q6. |
How often have you experienced any of the following effects in the last 24 hours? |
|
|
| i. Nausea |
0.29 |
1.28 |
| ii. Drowsiness |
0.51 |
0.28 |
| iii. Itching |
0.51 |
0.28 |
| iv. Dizziness |
0.54 |
0.72 |
| Q7. |
In the last 24 hours, how much pain relief did you receive from all your pain treatments combined? |
6.89 |
5.17 |
| Q.8 |
How satisfied are you with the results of your pain treatment while in hospital? |
7.29 |
5.29 |
| |
Overall satisfaction |
6.94 |
5.15 |
Table 5 Patient satisfaction and mean scores.
The first question was as follows, “in the last 24 hours how much did the pain interfere or prevent you from doing activities in bed such as turning, sitting up, repositioning?” The difference in Mean score between the morphine and pethidine group was 2.50 for morphine and 3.78 for pethidine, which would indicate that patients in the pethidine group had more pain on movement.
Question no. 2 in the patient satisfaction survey was “in the last 24 hours, how much did pain interfere or prevent you from doing activities out of bed such as walking, sitting in a chair, or other activities?” the Mean value for the morphine group was 2.60 and for the pethidine group was 3.90 which indicated that use of pethidine was associated with more pain preventing patients from mobilizing.
Question no. 3 asked “in the last 24 hours, how much did pain interfere or prevent you from sleep?”. Mean score for the morphine group was 1.84 and pethidine group was 3.30 indicating that the pethidine group had less sleep compared to the morphine group due to pain.
Question 4 asked “in the last 24 hours, how much did pain interfere or prevent you from staying asleep?” Again, the mean in the morphine group was 1.56 and in the pethidine group 2.85 indicating that the pethidine group experienced more pain which prevented these individuals from staying asleep.
Concerning pain causing anxiety, depression, fear and helplessness scores were <2 for both morphine and pethidine, indicating a low incidence of these particular side effects.
Patient’s subjective analysis of nausea, drowsiness, itching and dizziness (more common side effects of opioids) were generally <1. Interestingly the pethidine group subjectively reported a slightly higher incidence of nausea compared to the morphine group.
In terms of overall satisfaction, the mean score for the morphine group was 6.94 and for the pethidine group was 5.15 indicating that overall, patients were more satisfied with morphine compared to pethidine for postoperative pain relief for orthopedic surgeries. This difference was not deemed statistically significant. Rahman et al. [17] found not much difference in patient satisfaction scores (3.17 for morphine and 3.01 for pethidine).
Discussion
Inadequate treatment of pain remains a huge clinical problem in postoperative patients. This has resulted in physiological, psychological, ethical and financial implications, resulting in increased complication rates and increased cost to the financial institution. In this study, both unidimensional and multidimensional tools were used to assess pain as the Gold Standard to assess quality of care for both the morphine group and the pethidine group.
Part A of study- VAS scores
For Part A of this study, the demographic profile of the patients on the orthopedic ward were male (66%) compared to female (34%). This corroborates evidence from Hariharan et al. [10], who found the majority of patients (76%) were male. Their study was also conducted on orthopedic and trauma patients.
Similarly, most of the patients in this study had lower limb injuries which required surgery (45%) compared to the study done by Hariharan et al. in 2010 where 36% of injuries were lower limb injuries.
The Visual Analogue Scale (VAS) score was used as gold standard to [21] assess pain three times a day until day 2 or until day of discharge three times a day during the periods 12am-8am, 8am- 4pm, 4pm till 12pm.
Results were calculated based on Day 1 VAS score between 12 am to 4pm. By then, any conferred analgesia from regional would have subsided.
Mean VAS at rest for pethidine was 4.11 vs. 3.51 for pethidine. Difference at rest was 0.6. The decrease in VAS Score at rest during Day 1 between 8am and 4pm showed that there was a 14.5% decrease compared with pethidine. This did not meet the criteria for significance and therefore the null hypothesis was accepted for “rest pain”.
Mean VAS on movement for pethidine was 4.20 vs. 3.43 for morphine. Difference at rest was 0.77. The VAS score calculated on movement during the same time period on Day 1 showed an 18.5% reduction in pain score. This was very close to the 20% which was deemed to be significant (20%). This finding was indeed noteworthy, as there was a decrease in VAS score for both pain and rest and on movement. Here, the null hypothesis would be accepted for movement pain. Rahman et al. [17] compared intramuscular morphine and intramuscular pethidine for postoperative analgesia in major abdominal surgery and found there was no significant difference between the morphine (1.07) vs. pethidine group (1.23) (p value<0.511).
The Visual Analogue Scale (VAS)was used as gold standard to [21] assess pain three times a day until day 2 or until day of discharge three times a day during the periods 12am-8am, 8am-4pm, 4pm till 12pm.
VAS scores were highest on Day 0 (day of surgery) with mean value of 4.16 for males and 4.00 for females. This was similar to results in the ASSIST trial [12] where 88.4% of patients reported higher VAS scores during the first 24 hours of surgery. The mean VAS in the study done by Hariharan et al. [1] was compared to this current study in which the therefore implied that this difference was due to the standardized protocol of multimodal analgesia which was not enforced in 2010 as that study was purely observational. Bardiau et al. [8] also showed that institution of an acute pain protocol resulted in a significant reduction in postoperative pain scores (31% to 18%) which could have accounted for the difference in Mean VAS score of (6 in 2010 vs. 3-4 in 2019). Similar results were found in a study done by Gould et al [7] where institution of an acute pain protocol led to a significant improvement in VAS Scores.
One of the recommended practical guidelines for management of acute postoperative pain referenced by the American Pain Society [23] was the use of regional anaesthesia [21]. Patients who were given regional anaesthesia received either morphine or pethidine postoperatively.
Thirty-two (32) patients were given morphine and forty patients were given pethidine. Their mean scores were 1.22 and 1.30 respectively which indicated no difference between the two groups. Most patients in the regional group received more morphine equivalents (MEQ) in the following ranges (161-200 and 201-240 MEQ range) compared to those who had general anaesthesia who received (80-120 or 161-240 MEQ).This could be attributed to the fact that on Day 0 of surgery patients may either have not complained or the block wore off by the time they were admitted to the ward, thus requiring a higher dose of opioid compared to those who had general anaesthesia who would have been optimized in the recovery area before discharge to the ward. On Day 1, staff may have been cautious in administering the drug until the regional had completely worn off or the patient had started to ambulate.
Part B of study-side effects
Part B of the study evaluated quality of pain relief using a patient satisfaction survey [12]. This was based on the Mc Gill Pain questionnaire [21,22]. Patients preferred morphine for pain on sitting up and repositioning. They also preferred morphine during periods of walking or sitting up on a chair. This was of paramount significance for the prevention of major complications such as DVT and atelectasis after surgery. The incidence of minor side effects (anxiety, depression, fear, helplessness) was negligible. The major side effect profile for opioids was also negligible and slightly higher for pethidine (increased reported incidence of dizziness).
Part B of the study sought to evaluate the incidence of adverse side effects of opioids: Using a validated questionnaire [12], the incidence of constipation, nausea, drowsiness, respiratory depression (Sp02<90%) was recorded until Day 2. The majority of patients had first bowel movement on Day 2 (38 patients) representing 52.8% followed by 17 patients on Day 1 representing 23.6%. Only 7 patients representing 9.7% of the study population had first bowel movement after day 3.The majority of patients did experience some level of constipation on the ward, with the majority passing stool on day 2. This can be attributed to being kept nil per oral immediately after surgery and also pain leading to ileus.
In terms of nausea, the majority of patients (91.7%) did not experience any symptoms vs. only 6.9% experiencing nausea.
A positive correlation was found between morphine equivalents and drowsiness. Therefore, the more morphine equivalents received, the drowsier the patient, however, this was deemed statistically insignificant (P=0.375). Only 1.4% of patients experienced drowsiness. This represented only 1 patient out of 71. This patient was given morphine as more patients who complained of drowsiness received morphine.
Only 1 patient representing 1.4% of the study population experienced decreased saturation <90%. The patient was given supplemental oxygen with good response.
There was a negative correlation between intramuscular pethidine and 24-hour pain relief [r=-0.357, n=71, p=0.002]. Therefore, intramuscular morphine provided better analgesia over the 24-hour period. This can be explained by the longer duration of action and greater potency of morphine compared to pethidine administered intramuscularly.
After comparing the major side effects, it was evident that the risks of adverse side effects of opioids were minimal and nonlife threatening. Administration of a longer acting opioid such as morphine in a therapeutic dose range should be considered safe for postoperative pain and should not be withheld due to the perceived misconception about the side effect profile of the drug.
In the descriptive analysis between intramuscular morphine and intramuscular pethidine and time to mobilization, the difference between the means was negligible (3.69 for morphine group and 3.13 for the pethidine group). Morphine group took slightly longer to mobilize compared to Pethidine group. This could be explained by increased drowsiness associated with the sedative effect of morphine.
The length of stay was slightly different between the morphine group(Mean 5.59) vs. Pethidine group (Mean 4.95). This could have been due to the increased time to mobilization of the morphine group compared with the pethidine group.
Mean time to oral intake was almost the same between the morphine group (Mean 1.16 and the pethidine group (Mean=1.15). This meant that giving morphine to patients did not lead to increased time to oral intake, even though morphine was associated with increased drowsiness. It did not show statistical significance.
Part B of study-patient satisfaction
A patient satisfaction survey was given to each patient on day of discharge or on day 2 postoperatively. This was a standardized questionnaire taken from the ASSIST TRIAL [12]. There was a non-clinically significant positive correlation between morphine use and pain relief on Day 1 at rest and on movement (P= 0.900).
There was a significant negative correlation between patient satisfaction and opioid use (P=0.006), that is lower doses of opioid resulted in lower patient satisfaction scores.
From the patient satisfaction survey, it was shown that patients who received pethidine had more pain on movement in bed and out of bed, had less sleep, and had more problems staying asleep (1.5 in the pethidine group vs. 2.8 in the morphine group). Sleep is important for postoperative recovery.
In terms of overall satisfaction, patients in the morphine group were more satisfied compared to the pethidine group as they had better sleep patterns, had less pain on movement facilitating easier ambulation and were overall more satisfied.
The results from this study were echoed by O’ Connor et al. [19], who compared the efficacy and safety of morphine and pethidine for renal colic. There was no difference in the efficacy, safety profile or patient satisfaction with the two opioids and it was concluded that morphine could be safely advocated as the drug of choice.
It was concluded from the analysis that the benefits outweighed the risks of prescribing morphine to patients for postoperative pain. Even though there was an association with increased time to mobilization and increased incidence of drowsiness (seen from Part A of the study), patients were overall more satisfied with receiving morphine for their postoperative pain when asked subjectively. These results correlated with the slightly better VAS scores in the morphine group.
Limitations
This study did pose some limitations as only Orthopaedic patients were considered. The majority of surgeries performed were long bone fractures of the lower limb and hip surgery which are longer procedures and may be associated with more pain.
It was difficult to collect a larger sample size during the time period the study was conducted as there were many issues with equipment (C-arm) during this time period (May-December 2018). This issue could not be predicted. The equipment issue resulted in the postponement of many cases and referrals to other hospitals were made.
VAS for pain is an instantaneous measure and does not take into account the temporal arrangement for pain. Patient related outcome questionnaires involving patient satisfaction have been shown to correlate with VAS scores [22].
Initially the nurses on the ward were educated to fill out VAS scores, however, due to non-compliance and missing data the investigator undertook the initiative to fill out the forms in order to have completed data.
The time periods during which the VAS scores were collected were divided into 8-hour periods (12am-8am, 8am-4pm and 4pm to midnight).
It was difficult for the investigator to collect data at the exact same time during these time periods and this may have skewed the results depending on time of administration of the drug according the nursing schedule.
The incidence of nausea was reported more often in the patient satisfaction score than when evaluated clinically on the ward. This could be due to the transient nature of the nausea itself and the patient recalling it later on in the patient satisfaction survey before discharge
The project would have liked to assess VAS Scores in patients taking oral morphine, however, due to Pethidine being the most common opioid prescribed for severe pain and the most popular route of administration being Intramuscular, this study compared a comparable dose of Morphine also administered intramuscularly. Future studies may look into comparison of oral doses of morphine and analgesic profile.
Recommendations
Further studies can be done to evaluate the analgesic effect of oral morphine as this was not done in this study.
It is recommended that continuous medical training be provided for all levels of staff, within the institution regarding acute pain management for postoperative patients. The HCP would therefore be able to advocate for better analgesia for the patient, which would incidentally be less labour intensive for the staff members and result in greater patient satisfaction.
Conclusion
Patients who received intramuscular morphine had lower VAS scores compared to those who received intramuscular pethidine. This resulted in a decrease in VAS score of 18.5% on movement which was greater than predicted the 15% reduction. The null hypothesis was therefore rejected, the difference in VAS was noteworthy to afford consideration towards advocating for intramuscular morphine. It is also noteworthy that the intramuscular route remains the most popular route for postoperative administration on the surgical wards and patient satisfaction was also positively correlated with good pain control with morphine.
Overall, the incidence of side effects with opioids were negligible.
There was an increased incidence of nausea and drowsiness associated with the use of morphine, but this was small, 1.4% of patients.
Patients who received regional anaesthesia in theatre did not benefit from this on the ward as they required more morphine equivalents as the block wore off.
The patient satisfaction survey indicated that patients were more satisfied with the morphine regime vs. pethidine regime used currently prescribed by the surgeons. It can be suggested that since the incidence of side effects is small, that morphine should be used instead in a 4-6 hourly dosing regimen to achieve steady therapeutic levels.
The knowledge and attitudes survey identified that most HCPs held the belief that opioids are good drugs and that patients should not be in pain or refuse their medication. More positive attitudes were seen amongst senior doctors compared to senior nurses.
Most health care professionals had a positive attitude regarding respiratory depression and opioids; however, this was not seen with the other side effects such as abdominal distension, nausea and vomiting, and constipation where negative attitudes were expressed by the senior nursing body. This may be attributed to lack of continuous medical training regarding pain management on the ward.
35458
References
- Hariharan S, Chen D, Morapedi O, Bathusi D, Segakolodi B (2010) Prescription patterns of analgesics and pain relief for hospitalized trauma patients in a tertiary care teaching hospital of a Caribbean developing country. J Pain Manag 3:241-246.
- MacPherson C, Aarons D (2003) Overcoming Barriers to Pain Relief in the Caribbean. Dev World Bioeth 9:6-8.
- Meissner W, Coluzzi F, Fletcher D, Huygen F, Morlion B, et al. (2015) Improving the management of post-operative acute pain: priorities for change. Curr Med Res Opin 31:2131-2143.
- Vadivelu N, Mitra S, Narayan D (2010) Recent Advances in Postoperative. J Biol Med 83:11-25.
- Taylor R, Ullrich K, Regan S, Broussard C, Schwenkglenks M, et al. (2013) The Impact of Early Postoperative Pain on Health-Related Quality of Life. Pain Pract 13:515-523.
- Gould T, Crosby D, Harmer M, Lloyd S, Lunn J, et al. (1992) Policy for controlling pain after surgery: effect of sequential changes in management. BMJ 305:1187-1193.
- Bardiau F, Taviaux N, Albert A, Boogaerts J, Stadler M (2003) An Intervention Study to Enhance Postoperative. AnesthAnalg 96:179-185.
- Solhi H, Sanaei-Zadeh H, Solhi S, Nadian M, Gharibi M, et al. (2016) Meperidine (Pethidine) versus morphine in acute pain management of opioid-dependent patients. Open Access Emerg Med 8:57-59.
- Latta KS, Ginsberg B, Barkin RL (2002) Meperidine:a critical review. Am J Ther 9:53-68.
- Gordon DB, Polomano RC, Pellino TA, Turk D,McCracken LM, et al. (2010) Revised American Pain Society Patient Outcome Questionnaire (APS-POQ-R) for Quality Improvement of Pain Management in Hospitalized Adults: Preliminary Psychometric Evaluation. J Pain 11:1172-1186.
- Subramanian B, Shastri N, Aziz L, Gopinath R, Karlekar A, et al. (2017) ASSIST-Patient satisfaction survey in postoperative pain management from Indian subcontinent. J Anaesthesiol Clin Pharmacol 33:40-47.
- Fizzah F, Khan R, Ahmed A (2016) Assessment of patient satisfaction with acute pain management service: Monitoring quality of care in clinical setting. Indian J Anaesth 60:248-252.
- Srisawang P, Rashid H, Hirosawa T, Sakamoto J (2013) Knowledge, attitudes and barriers of physicans, policy makers/regulators regarding use of opioids for cancer pain management in Thailand. Nagoya J Med Sci 75:201–212.
- Samarkandi O (2018) Knowledge and Attitudes of Nurses Towards Pain Management. Saudi J Anaesth 12: 220-226.
- Sommer M, deRijke JM, van Kleef M, Kessels AGH, Peters ML, et al. (2008) The prevalence of postoperative pain in a sample of 1490 surgical inpatients. Eur J Anaesthesiol 25:267-274.
- Rahman Z, Parveen N, Murad D, Qurayeshi A, Hossain M (2016) A Comparative Study Of Intramuscular Morphine And Pethidine For Post- Operative Analgesia In Major Abdominal Surgeries - To Establish Preference Of Morphine In Bangladesh. Anesth Analg 123:386.
- Wee M, Tuckey J, Thomas P, Burnard S (2014)A comparison of the efficacy of intramuscular diamorphine with intramuscular pethidine for labour analgesia: a two-centre randomised blinded controlled trial. BJOG AnInt J Obstet Gynaecol 121:447-454.
- O’Connor A, Schug S, Cardwell H (2000)A comparison of the efficacy and safety of morphine and pethidine as analgesia for suspected renal colic in the emergency setting. J Accid Emerg Med 17:261-264.
- Edwards HE, Nash RE, Najman JM, Yates PM, Fentiman BJ, et al. (2001) Determinants of nurses’ intention to administer opioids for pain relief. Nurs Heal Sci 3:149-159.
- Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, et al. (2016) Management of postoperative pain: A clinical practice guideline from the American pain society, the American society of regional anesthesia and pain medicine, and the American society of anaesthesiologist's committee on Executive Committee, and Administrative Council. J Pain 17:131-157.
- Chandrasekaran S, Gui C, Walsh JP, Lodhia P, Suarez-ahedo C, et al. (2013) Correlation Between Changes in Visual Analog Scale and Patient-Reported Outcome Scores and Patient Satisfaction After Hip Arthroscopic Surgery. Orthop J Sports Med 5: 1-6.