Sarah El-Abbassi*, Sanae El-Majjaoui, Hanan El-Kacemi, Tayeb Kebdani and Noureddine Benjaafar
Department of Radiation Oncology, National Institute of Oncology, Mohammed V University in Rabat, Morocco
*Corresponding Author:
Sarah El-Abbassi
Resident of Radiation Oncology, Department of Radiation oncology, National Institute of Oncology, Mohamed V University in Rabat, Morocco
Tel: +212661678389
E-mail: drsarahelabbassi@gmail.com
Received date: May 10, 2017; Accepted date: May 26, 2017; Published date: May 30, 2017
Citation: El-Abbassi S, El-Majjaoui S, El-Kacemi H, et al. Complete Genital Prolapse with Cervix Carcinoma: A Case Report and Literature Review. Arch Can Res. 2017, 5: 2. doi:10.21767/2254-6081.1000141
Background: Although genital prolapse and carcinoma of the uterine cervix are not rare event, their association is very uncommon. We report a case of this association.
Case presentation: A-79-year-old female presented with 11 months history of post-menopausal bleeding, pelvic pain and sensation of heaviness which was increasing in intensity over than 8 months. Physical assessment showed a large genital prolapse third degree and ulcerous and necrotic lesion at the lower part prolapse. Histopathological examination of cervical biopsies revealed well differentiated and invasive squamous cell carcinoma. She was staging according to the International Federation of Gynecology and Obstetrics staging system 2009 as FIGO IIIB. The patient was treated by palliative chemotherapy. After 3 months, the patient died.
Conclusion: Genital prolapse with cervical carcinoma is a rare association. In fact, it is necessary to individualize the optimal treatment for each patient to improve life quality and the prognosis.
Keywords
Genital prolapse; Cervix carcinoma; Surgery; Radiotherapy
Abbreviations
FIGO: International Federation of Gynecology and Obstetrics; MRI: Magnetic Resonance Imaging; MRU: Magnetic Resonance Urography; POP: Pelvic Organs Prolapse
Introduction
Genital prolapse affects 30% of women with pic age of 60 years [1]. In Morocco, cervical cancer is the second most common cancer and the second cause of cancer death. The association between cervical cancer and uterine prolapse is rare and sparsely represented in literature, despite the high incidence of the latter. The suitable treatment in this clinical situation is not defined. The objective of this article is to report a case of this association and review published cases about this clinical condition.
Case Presentation
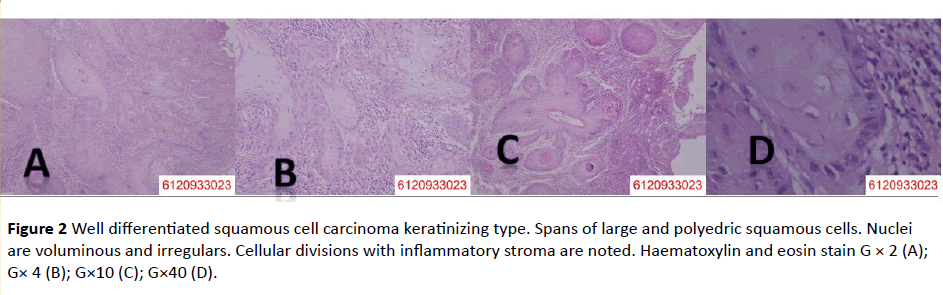
A 79-year-old female presented in our department with 11 months history of post-menopausal bleeding, pelvic pain and sensation of heaviness which was increasing in intensity over than 8 months. Altered urinary and bowel habits were noted too. No history of any comorbid illness was present. She reported two risk factors: age and multiple parity (10 children). Physical assessment showed a large genital prolapse third degree. Whole uterus protruded from vulva (complete procidemia). This uterus prolapse was measuring over than 20 cm × 8 cm. An ulcerous and necrotic lesion at the lower part prolapse was observed, corresponding to cervical tumor (Figure 1). Digital rectal examination showed a bilateral parametrial invasion. Cervical biopsies were performed and histopathological examination revealed well differentiated and invasive squamous cell carcinoma (Figure 2). Pelvis magnetic resonance imaging (MRI) has demonstrated a large ptosis of the uterus vagina and bladder. The upper part of bladder remains over the pubis. Cervical tumor measuring 80 mm × 50 mm × 65 mm in T1 hypo signal and T2 hyper signal with bilateral parametrial invasion were noted. No pelvic lymphadenopathy was found. She was staging according to the International Federation of Gynecology and Obstetrics staging system 2009 as FIGO IIIB. After multidisciplinary board meeting, the patient starts palliative chemotherapy. Given the locally advanced character, no surgery or chemoradiation were done. After 3 months of treatment, she died.

Figure 1 Complete genital prolapse and externalized cervix cancer.
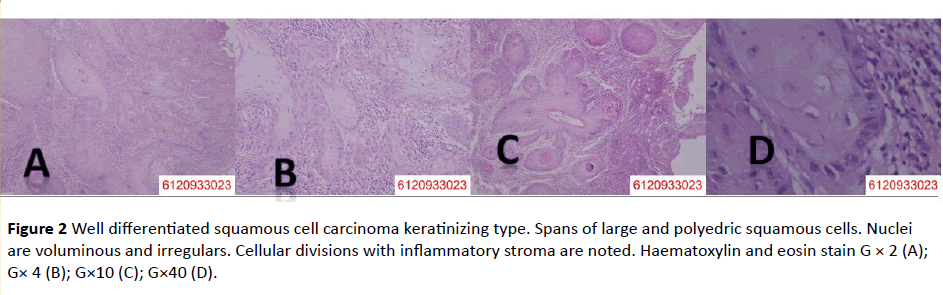
Figure 2 Well differentiated squamous cell carcinoma keratinizing type. Spans of large and polyedric squamous cells. Nuclei are voluminous and irregulars. Cellular divisions with inflammatory stroma are noted. aematoxylin and eosin stain G × 2 (A); G× 4 (B); G×10 (C); G×40 (D).
Discussion
The coincidence of uterine prolapse and cervical cancer is uncommon and usually happens in underdeveloped countries and in older women [2,3]. The rarity of this association precludes any possibility of studying and establishing the exact pathogenesis. The assumption that displacement of the uterine cervix from the natural environment of the vagina may decrease the neoplastic process of viral infection explains the lower risk of cervical cancer in uterine prolapse [2,4]. Although the continual injury of the cervical epithelium may cause neoplasm [1,4]. MRI along with Magnetic Resonance Urography (MRU) is a necessary noninvasive, nonionizing technique in evaluation of uterine prolapse associated with cervical cancer. Radiographic assessment is unnecessary for simple pelvic organ prolapse (POP) [5].
In the most reported cases, POP has been evolving for more than 10 years. Borges da Silva et al. reported two cases of uterine prolapse of more than 10 years of duration that presented with cervical cancer. The patients were respectively of 69 and 73 years old and both were treated with radical vaginal hysterectomy followed by external pelvic radiation [6]. This suggests that the ulcerate lesion of the cervix appeared long after the prolapsed. Our patient reported the beginning of genital prolapse since 9 years. This symptom was ignored for 8 years. The onset of post-menopausal bleeding and genital prolapse increasing size were the reasons of medical visit. We can conclude that genital prolapse occurred long before cervix cancer.
The first diagnosis that should be eliminated (by frequency argument) in post-menopausal bleeding cases is endometrial carcinoma, not cervical cancer [1]. Frick et al. have retrospectively analyzed 644 cases of hysterectomy for patients undergoing genital prolapse. No cervical lesions existed. However they had observed 13% of endometrial lesions [7].
There is no concrete consensus regarding treatment of this association. From 1999, after the results of five randomized clinical trials, concomitant chemoradiotherapy has become the standard of care for high-risk early-stage and locally advanced cervical cancer and has been offered as an alternative to radical hysterectomy for patients with tumor confined to the cervix but larger than 4 cm (Ib2) [8-12]. In contrast, some authors recommend surgery approach for the association genital prolapse and cervix cancer [1,2,13,14]. The clinical presentation of patients made essential to perform a septic surgery. However, pelvic radiation can be performed [7]. But it seems more appropriate to reserve chemoradiation when surgical treatment is not feasible. An extension of cervical cancer beyond the dissection plane make difficult to treat the prolapse [1]. Uterine prolapse is usually associated with cystocele and rectocele. Tomoradiotherapy is better than conventional radiotherapy in lowering radiation toxicity at the urinary bladder and the rectum [14].
Cabrera et al. had described a case of cervical adenocarcinoma with complete prolapse treated successfully by surgery (radical laparoscopic hysterectomy with lymphanectomy) and adjuvant chemoradiation [4]. Given the locally advanced stage (stage IIIB of FIGO classification), our case was surgically challenged. The radiation therapy was limited by the volume of externalized prolapse. The decision of palliative chemotherapy has been approved. After 3 months, the patient died.
Conclusion
Genital prolapse with cervical carcinoma is a very rare association, with unknown pathogenesis. In fact, it is necessary to individualize the optimal treatment for each patient to improve life quality and the prognosis.
Ethics Approval and Consent to Participate
Written informed consent was obtained from the patient and her family for publication of this case report and any accompanying images.
Funding
The authors would like to specially thank the Faculty of Medicine and Pharmacy of Rabat; the source of funding for all authors.
Acknowledgement
All the authors are thankful for providing the necessary facilities for the preparation the manuscript.
19447
References
- Vieillefosse S, Thubert T, Trichot C, Deffieux X (2014) Cancer du col et prolapses génital exteriorize. Progrès en urologie 24: 533-534.
- Loizzi V, Cormio G, Selvaggi L, Carriero C, Putignano G (2010) Locally advanced cervical cancer associated with complete uterine prolapse. Eur J Cancer Care (Engl) 19: 548–550.
- Dane B, Dane C, Erginbas M, Baran S, Cetin A (2009) Verrucous carcinoma of the cervix in a case with uterine prolapse. Ann Diagn Pathol;13:344–346.
- Cabrera S, Franco-Camps S, García A, Vergés R, Díaz-Feijoo B, et al. (2010) Total laparoscopic radical hysterectomy for cervical cancer in prolapsed uterus. Arch Gynecol Obstet 282: 63-67.
- Jelovsek JE, Maher C, Barber MD (2007) Pelvic organ prolapse. Lancet 369: 1027–1038.
- Da Silva BB, Da Costa Araujo R, Filho CP, Melo JA (2002) Carcinoma of the cervix in association with uterine prolapse. Gynecol Oncol 84, 349–350.
- Frick AC, Walters MD, Larkin KS, Barber MD (2010) Risk of unanticipated abnormal gynecologic pathology at the time of hysterectomy for uterovaginal prolapse. Am J Obstet Gynecol 202: 507.
- Whitney CW, Sause W, Bundy BN, Malfetano JH, Hannigan EV, et al. (1999) Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: A Gynecologic Oncology Group and Southwest Oncology Group study. J Clin Oncol 17: 1339–1348.
- Morris M, Eifel PJ, Lu J, Grigsby PW, Levenback C, et al. (1999) Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med 340: 1137–1143.
- Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, et al. (1999) Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med 340: 1144–1153.
- Keys HM, Bundy BN, Stehman FB, Muderspach LI, Chafe WE, et al. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med 340: 1154–1161.
- Peters WA, Liu PY, Barrett RJ, Stock RJ, Monk BJ, et al. (2000) Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol 18: 1606–1613.
- Reimer D, Sztankay A, Steppan I, Abfalter E, Lunzer H, et al. (2008) Cervical cancer associated with genital prolapse a brief review of the literature and long-term results of successful treatment with radiochemotherapy and surgery in a very frail patient. Eur J Gynaecol Oncol 29: 272-275.
- Du XL, Tao J, Sheng XG, Lu CH, Yu H, et al. (2012) Intensity-modulated radiation therapy for advanced cervical cancer: A comparison of dosimetric and clinical outcomes with conventional radiotherapy. Gynecol Oncol 125: 151-157.