Keywords
Compliance; Standard precautions; Nurses; Saudi hospitals
Introduction
Healthcare related infections are common occurrences which may increase the risk of developing dangerous complications whilst receiving treatment [1]. This is a serious issue across healthcare as a whole, and has been for some time [2-33], but considering the nature of the current global pandemic of Covid-19, and the rapid spread of the disease both within the community and within healthcare settings [28], this can be considered a priority area for research [34]. This study seeks to examine the compliance with standard precautions (SPs) – which are a primary strategy for the prevention of healthcare-associated infections – within hospital units in the Tabouk region of Saudi Arabia.
Background, aims and objectives
SPs are based on the principle that all bodily fluids may contain infectious agents that can be transferred to others [9]. SP guidelines state that there is a need for appropriate disposal of waste, appropriate sharps management protocols, safe use of personal protective equipment (PPE), and the following of hard hygiene guidelines [9,18]. By complying with these aspects of care, the chances of contracting infection are reduced, and the disruption of microorganism spread can be achieved [32]. Whilst compliance with SPs is an expectation of those working in clinical settings, in practice there have been reports of suboptimal following of the guidelines [9,26,32].
It is the aim of this current study to examine what the current compliance rates with SPs are in a specific area of Saudi Arabia (Tabouk), and to explore what factors may be associated with poor compliance. In order to achieve this, the objectives for this study were to recruit a sizeable sample from multiple clinical sites in Tabouk, and to use a standard measure to gauge SP compliance. By cross-analysing compliance with other factors such as professional characteristics, it is hoped that a picture of those who need most support to improve their practice can emerge.
Research questions
As an exploratory study, this work will seek to address a number of research questions. These are as follows:
• What are the current compliance rates for SPs within the Tabouk region of Saudi Arabia?
• What measurable factors impact upon compliance with SPs?
Rationale
While infection control is a crucial element of good clinical practice even in the best of times, it becomes even more vital at a time of the global Covid-19 pandemic which is ongoing at time of writing [29]. Being able to provide insights into specific characteristics of staff that need more support to fully engage with and practice SPs regularly will potentially be vital in being able to target these individuals and improve the quality of care and safety levels where they work. This is important for patient experience, safety, and outcomes [14]. This work may also be used to target more effective training processes with regards to ensuring SPs are followed.
Literature Review
Adherence to SP guidelines require both training and a supportive working environment, as well as individual clinician motivation to comply [9]. Within Saudi Arabia, a number of studies have been conducted on student clinician populations, which have reported a concerning lack of overall compliance to SPs. For example, the work of [27] reported a compliance rate of 56.8% among Saudi baccalaureate nursing students during their clinical training. These figures were supported by a similar study conducted by [7] who examined compliance with SPs among baccalaureate nursing students in Saudi Arabia and reported the overall compliance of around 61%. This could be perhaps excusable within students who are just learning their craft, but a study by [24] identified that within Qassim Hospital in Saudi Arabia, registered nurses had a poor knowledge of SPs, with just a third adhering to them. This could be down to a lack of knowledge or poor training, but is clearly an area that requires further examination.
Non-compliance with SPs is the leading cause of medical errors and poor patient outcomes within Saudi Arabia [7]. The combination of poor nurse knowledge [24] and poor patient knowledge [35] creates a perfect storm in which standards are not followed, enforced, or treated as a matter of necessity. Unfortunately, this situation leads to an increase in medical errors that in turn contribute to rising mortality rates [20]. Due to the seriousness of this situation, and particularly in light of the current pandemic and the increased need for infection control standards to be raised [16], this represents an area of research that is not urgent and in need of increased examination.
The issue of non-compliance with SPs is not one that is specific to those healthcare workers within Saudi Arabia, with numerous international studies reporting similarly poor compliance (e.g. 3,19, 22). Whereas the recording of non-compliance across clinical settings and around the world presents an evidence base which can be considered to be robust [13], reasons behind this phenomenon require further examination. A cross-sectional study conducted by [31], for example, indicated that core barriers to SP compliance included the perception that complying with SPs interfered with workers’ other duties. This however was based within a small, single-site study within the specific area of perioperative nursing; the generalizability of this work is limited as a result. Another study examining potential factors within this area was conducted by [10]. Using a focus group approach, combined with content analysis, the authors noted that decisions to comply with SPs revolved around beliefs regarding benefits, barriers, severity, and susceptibility. However, although this study provided a rich set of data from which these conclusions were made, the design and approach taken does not enable specific characteristics of individuals to be identified that could be used to subsequently target interventions aimed at improving SP compliance. Because of the severe nature of infections caused by poor SP practice [7], and the need to be able to identify the characteristics of those most at risk of engaging in poor practice, this current study is an urgent and timely addition to the literature in this field.
Methodology
Research design
This study was conducted within hospitals in the Tabouk region of Saudi Arabia, to examine the levels of compliance with SPs that contribute to the reduction of infection in these facilities. This study is situated within the positivist paradigm, placing value on the observed and measurable [4], and is thus solely quantitative in nature. It employed a descriptive, cross sectional design, with the key dependent variable being level of SP, as self-reported by participants. Independent variables include training and educational history, as well as some demographic variables.
Participant recruitment
A convenience sampling strategy was employed to recruit n=354 nurses working in the Tabouk region of Saudi Arabia. Taken from a total population of approximately 4,000 nurses working in this area, it is noted that a randomized approach to sampling would have yielded a more generalizable sample [17]. However, convenience sampling is a widely used approach in cross sectional work such as this [21] and is a pragmatic approach that can facilitate relatively large samples to be collected in a timeefficient manner [8]. It is of note that using Cohen’s seminal 1992 work on power analysis and sample size calculation as a guide, this sample size is appropriately powered to conduct the main inferential statistical analyses (see section 3.6) for a medium effect size and a power of .80, and at an alpha level of .05 [6]. This reduces the chances of the analysis producing a Type II error and enables greater faith to be placed into the veracity of the results.
Materials
Data collection would utilise a small battery of questionnaires that would be relatively quick for participants to complete. This was an important consideration for it was felt that if participants were provided with a large number of measures to fill in, this may act as a barrier to participation, and hence stymie recruitment. The first questionnaire to be used was specifically developed for this study, and consisted of demographic questions – such as age, gender, marital status and ethnicity – as well as work-related questions, which focused on the field of nursing participants were working in, their level of education, clinical experience, and attendance of prior infection control training.
The second questionnaire that was used was the Compliance with Standard Precautions Scale (CSPS) [18], which provided the core data on SP adherence for this study. The CSPS is a 20-item measure, with a 4-point Likert scale, in which answers range from ‘1’ (never) to ‘4’ (always), with higher scores being indicative of better rates of compliance with SP protocols. Example items within the CSPS include the use of PPE, decontamination of spills and used items, disposal of sharp objects and wastes, and prevention of cross-infection. This measure has been judged to be both valid and reliable, and appropriate for usage in differing cultures [18]. The CSPS was used within this study with prior permission to do so obtain from the author.
Procedure
The data collection period for this study lasted approximately one month from 15-07-2020 to 16-8-2020, during which time potential participants were approached and provided with information about the study and were asked about their willingness to take part. Those individuals who wished to take part in the study were asked for their informed consent to do so and were provided with information about their rights to cease participation after this point if they so wished, in line with best practice of research ethics [15]. The procedure for participation was simple, as is often the case with cross sectional studies [8], and consisted of consenting participants being provided with the two measures for completion, and their returning of them to the researcher once done. Completion of the two questionnaires took approximately 5 minutes for participants, following which, they were provided with a full debrief as to the aims of this study and thanked for their participation. Data was transferred from online questionnaire using Google Forms to SPSS and stored in an encrypted. Save file which only the researcher had access to. This file would then be used to conduct the data analysis, as outlined in section 3.6.
Ethics
Prior to conducting this study ethical approval was obtained from the institution review board, general directorate of health affairs, Tabuk region number TU-077/020/044. As part of the design and conduct of this study, there were numerous elements related to the ethical practice of this research that were factored in. For example, participant autonomy was assured by making it clear to potential participants as to the voluntary nature of taking part in the study, and once consenting to take part, they were again assured that they did not need to complete the measures if they suddenly chose not to. Although there were no cases of participant drop-out once taking part, this was an important ethical position to take in this work [30]. As well as autonomy, issues of confidentiality and anonymity were also taken into account in the design of this work. This consisted of ensuring that no personally identifiable information about participants would be collected or stored (anonymity), and that all data was stored securely and all reporting would be related to the cohort as a whole rather than individuals (confidentiality) [30]. Other ethical considerations include justice [11], which was complied with via ensuring all participants were treated in the same manner throughout, and scientific integrity [25] which was assured by the following of a strict data collection and analysis protocol.
Data analysis
The data, once transferred to SPSS, was examined for missing data elements to ensure the integrity of the dataset. The first phase consisted of producing descriptive statistics, relating to the demographic make-up of the recruited sample, and the nature of their adherence to the SPs outlined in the CSPS. Because of the nature of the questions used across both of these measures, this descriptive analysis consisted predominantly of frequency counts and percentages. The second phase of the data analysis strategy related to the conducting of inferential statistical tests.
The data that was collected from the CSPS and the elements of the demographic questionnaire of interest were largely categorical-ordinal by nature. This form of data precludes the use of inferential statistical tests such as t-tests or analysis of variance (ANOVA), or other tests that require parametric continuous or discrete quantitively data [12]. With ordinal data such as that collected for this study, therefore, the key inferential tests to be used will be the chi-squared test, which can use ordinal level predictor and outcome variables to examine the distribution between these levels of data [12]. The alpha level for these inferential tests has been set at p<.05.
Results
Overview of the sample
In total, this study recruited n=354 participants of whom n=21 (5.9%) were male and n=333 (94.1%) were female. The age of participants was mostly between 20 and 40 years (n=267, 75.4%), with n=87 (24.6%) being 41 years in age or older. The majority of participants were married (n=231, 65.3%), with n=112 (31.6%) being single, and n=11 (3.1%) being divorced.
In terms of the professional characteristics of the sample, the majority of participants held a Bachelor of Science (BSc) in Nursing (n=272, 76.8%), with the next most common qualification being a bridging qualification (Diploma to BSc. in Nursing) (n=72, 20.3%). The least common characteristic was the most qualified staff, with n=10 (2.8%) having attained a master's degree in Nursing. The environment in which nurses were working at the time of taking part in this study varied, with the highest proportion of participants working in critical care departments (n=116, 32.8%), followed by surgical (n=47, 13.3%), emergency (n=43, 12.1%), and medical (n=41, 11.6%) departments. A total of n=107 (30.2%) participants worked in departments classified as ‘other’, although no data was collected on what these departments may have been. It is of note that this was a cohort of largely experienced nurses, with over half (n=202, 57.1%) of participants having between 1 and 10 years of clinical experience, and with n=136 (38.4%) having over 10 years of clinical experience. Inexperienced staff were in the minority, with just n=16 (4.5%) having less than a year’s experience in clinical settings. Finally, the majority of this sample reported to having received previous infection prevention seminars or related training courses (n=260, 73.4%), with just n=94 (26.6%) not having done so.
Descriptive statistics: compliance with standard precautions
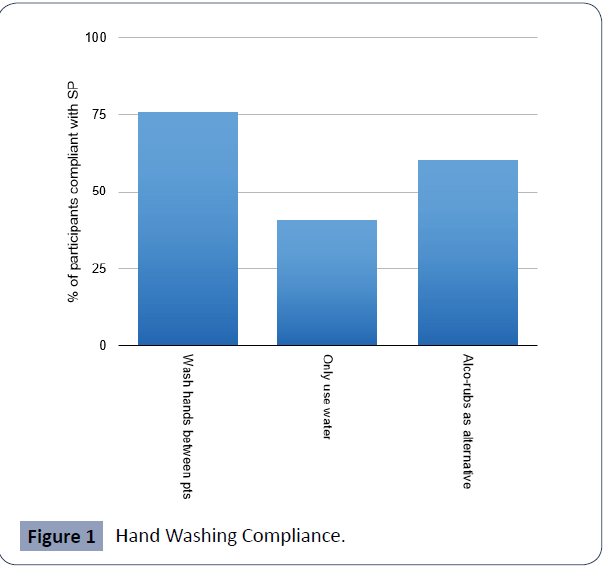
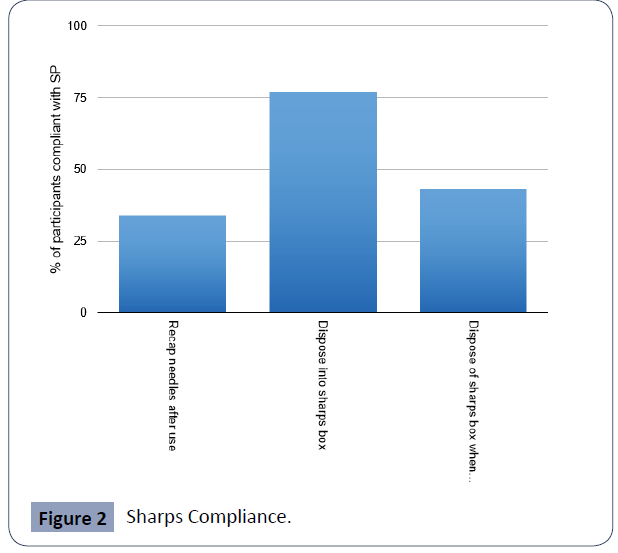
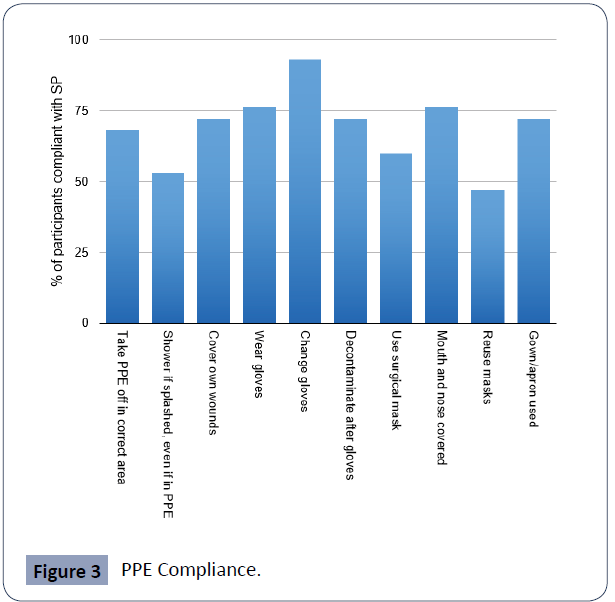
This sub-section relates to the responses of participants to the 20 items of the CSPS. The three figures provided in the appendix provide an overview of the levels of compliance across the core areas measured by the CSPS. Figure 1 shows the compliance levels with regards to washing hands; Figure 2 shows them in association with sharps safety; and Figure 3 covers the use of PPE within clinical settings. Compliance is defined by the participant self-reporting that they ‘always’ follow the SPs for the specific task being examined, within the questionnaire that they completed.
As can be seen in Figure 1, there was most compliance to SPs when it comes to washing hands between patients, with least about of compliance with SPs with regards to using only water when doing so. It is of note that none of these hand washing relating items saw full compliance, with just 76% of participants being compliant in the best instance.
Figure 1 Hand Washing Compliance.
As Figure 2 shows, sharps compliance is low, especially when it comes to recapping needles once they have been used and disposing of the sharps box when full. Again, there is no item within this sub-scale that participants were fully compliant with, with the best compliance being evident when disposing needles into the sharps box (76%).
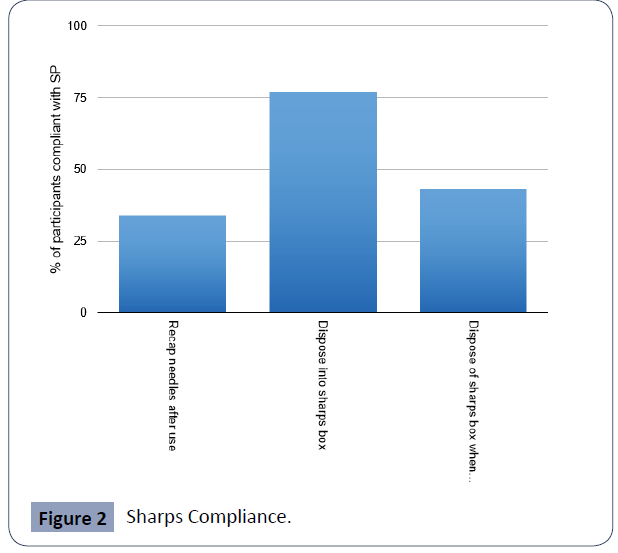
Figure 2 Sharps Compliance
Figure 3 shows that while there is near universal compliance (93%) when it comes to changing gloves between clinical contacts, there are concerning, low compliance levels elsewhere, particularly about steps taken if splashed by fluids (53%) and the reuse of surgical masks (47%).
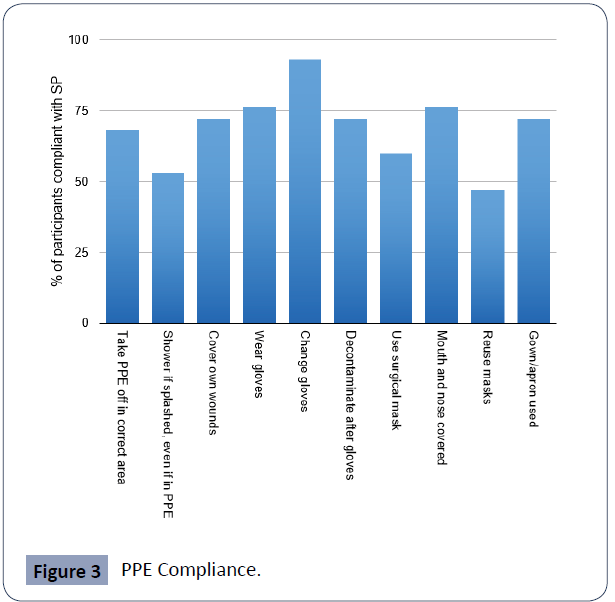
Figure 3 PPE Compliance.
Although purely descriptive in nature, this element of this study provides an insight into the fact that across each and every item on the CSPS there were numerous instances of a lack of compliance to SPs. This has also allowed there to be an identification of the most commonly broken SPs as measured by the CSPS, with particularly low compliance scores being noted with regards to safe practice regarding sharps management, and in relation to hand washing and face mask reuse.
Inferential statistics
This sub-section reports the results of the test of significance conducted on the data. As stated in section 3.6, because of the nature of the data that the CSPS and the demographic measures returned – i.e. categorical in nature for both measures – a chisquared test is the most appropriate form of addressing key questions on this data. This sub-section addresses four key questions: (I) is there a significant difference in SP compliance rates across clinical experience categories? (ii) is there a significant difference in SP compliance rates across clinical departments? (iii) is there a significant difference in SP compliance rates across educational backgrounds of participants? and (iv) is there a significant difference in SP compliance rates between those who have received infection control training and those who have not?
To address the first core question regarding clinical experience and SP compliance, significant differences were found across four items on the CSPS between expected and observed counts. These items related to (I) only using water when washing hands (X^2 (6) = 14.07, p=.029), in which worse compliance was demonstrated by those with less than a year’s and more than 10+ years’ experience; (ii) disposing of a full sharps box (X^2 (6) = 13.64, p=.034), in which expected counts were observed fewer times for those with 1-10 years’ experience, and were higher in those with less than a year’s and 10+ years’ experience; (iii) showering after being splashed with fluid (X^2 (6) = 14.45, p=.025), in which those with less than a year’s experience and those with 10+ years’ experience did this less than expected; and (iv) cleaning up spillages immediately (X^2 (6) = 16.12, p=.013), in which expected counts were observed fewer times for those with 1-10 and 10+ years’ experience, and were higher in those with less than a year’s experience.
To address the second question regarding differences in compliance rates across clinical departments, the chi-squared test revealed differences across almost all the CSPS items in expected and observed values. Table 1 in the appendix provides an outline of the items which were noted as significant. An examination of the observed and expected rates across these 17 items indicated that those in surgical settings were less likely be compliant with SPs more regularly across these items compared to other departments.
| CSPS item |
X^2 value (df) |
Sig. |
| Washing hands between patients |
69.9 (12) |
<.001 |
| Use of only water |
33.12 (12) |
0.001 |
| Use of alcohol rub |
24.97 (12) |
0.015 |
| Recapping needles |
43.65 (12) |
<.001 |
| Use of sharps box |
59.98 (12) |
<.001 |
| Disposal of full sharps box |
47.65 (12) |
<.001 |
| PPE removal in right places |
81.14 (12) |
<.001 |
| Shower after splashing |
39.96 (12) |
<.001 |
| Covering of own wounds |
48.22 (12) |
<.001 |
| Use of gloves |
60.95 (12) |
<.001 |
| Use of mask |
41.20 (12) |
<.001 |
| Covering nose and mouth |
57.23 (12) |
<.001 |
| Reuse of mask |
54.91 (12) |
<.001 |
| Use of gown/apron |
88.30 (12) |
<.001 |
| Disposal of waste fluids |
61.90 (12) |
<.001 |
| Decontamination of spaces |
66.33 (12) |
<.001 |
| Cleaning up fluids |
67.87 (12) |
<.001 |
Table 1 Differences between Departments in SP Compliance.
In relation to the third question regarding differing SP rates of compliance between the differing qualifications of participants, the chi-square test yielded statistically significant differences between expected and observed counts of compliance across four items of the CSPS. These items related to (i) only using water when washing hands (X^2 (6) = 19.80, p=.003), in which those with a bridging qualification were less compliant than would be expected; (ii) the recapping of needles (X^2 (6) = 28.17, p<.001) in which, surprisingly, Master’s level nurses performed poorly; (iii) the safe removal of PPE (X^2 (6) = 18.54, p=.005), in which again those with a bridging qualification were less compliant than would be expected; and (iv) taking a shower following being exposed to potentially infectious fluids (X^2 (6) = 40.53, p<.001), in which those with a BSc in Nursing were the poorest adherers to SPs.
Finally, to address the issue of whether infection control training had an impact on the rates of SP compliance, Table 2 in the appendix shows that for every single item on the CSPS, there was a highly significant difference (p<.001) in observed counts between those who had received infection control training (n=260) and those who had not had such training (n=94). This so far seems to be an intuitive finding. However, closer examination of the observed and expected counts within the chi-square output provides counter intuitive findings. While for many of the CSPS items, those who had attended previous training demonstrated higher compliance rates than would be expected within the chisquare test, there were a number of items in which there were fewer observed counts demonstrated by these individuals. These have been asterisked in Table 2 and include using only water, recapping needles, disposal of sharps boxes, showering after being splashed with infectious fluids, and reuse of PPE equipment.
Discussion and Conclusion
This cross-sectional study sought to ascertain what the current Table 2 Differences in Training Experience regarding SP Compliance.
| CSPS item |
X^2 value (df) |
Sig. |
| Washing hands between patients |
69.9 (3) |
<.001 |
| Use of only water |
33.12 (3)* |
0.001 |
| Use of alcohol rub |
24.97 (3) |
<.001 |
| Recapping needles |
43.65 (3)* |
<.001 |
| Use of sharps box |
59.98 (3) |
<.001 |
| Disposal of full sharps box |
47.65 (3)* |
<.001 |
| PPE removal in right places |
81.14 (3) |
<.001 |
| Shower after splashing |
39.96 (3)* |
<.001 |
| Covering of own wounds |
48.22 (3) |
<.001 |
| Use of gloves |
60.95 (3) |
<.001 |
| Change gloves between patients |
28.60 (3) |
<.001 |
| Contaminate hands after glove change |
160.82 (3) |
<.001 |
| Use of mask |
41.20 (3) |
<.001 |
| Covering nose and mouth |
57.23 (3) |
<.001 |
| Reuse of mask |
54.91 (3)* |
<.001 |
| Use of gown/apron |
88.30 (3) |
<.001 |
| Disposal of waste fluids |
61.90 (3) |
<.001 |
| Decontamination of spaces |
66.33 (3) |
<.001 |
| Use of gloves when cleaning spaces |
116.97 (3) |
<.001 |
| Cleaning up fluids |
67.87 (3) |
<.001 |
Table 2 Differences in Training Experience regarding SP Compliance.
SP compliant rates within Saudi hospitals in the region of Tabouk were, and to examine what variables might be identified to explain variance in compliance within the studied population. The findings stemming from this can be considered to be two-fold in nature. Firstly, on a purely descriptive level, the data collected within this study demonstrate that there is much work to be done to ensure that 100% compliance rates are attained across the range of 20 SP items measured by the CSPS. This can be seen to mirror the findings of the work of [1], who reported in multisite study SP compliance rates of around 60%. This was however within a population of nursing students, and the findings from the current study, based within a population of experienced and qualified nurses are particularly stark. The fact that there was not a sole instance of 100% compliance across these items is cause for concern and points to the need for enhanced attention to be paid to this area. To be at a level of less than 100% compliance is to risk serious medical errors or complications [20] and violates patients’ rights to high quality medical care [35].
While there is need for improvement across all areas of SP compliance in order for good practice to be universal within this population, this study has identified that core areas in need of improvement include hand washing protocols – in particular around the use of only water when doing so – as well as face mask reuse. This is particularly concerning considering the importance of correct hand washing techniques and face mask wearing in light of the current global Covid-19 pandemic [5]. Such widespread practice may explain some of the data to come from the Saudi reposes to the Covid-19 pandemic, and the manner in which clinicians have become affected with the illness whilst working on the frontline [2]. There were also highlighted concerns about participants use of sharps safety protocols, including recapping of needles following usage, and the correct disposal both of sharps and of sharps bins.
The second aspect of the findings relate to what the inferential statistical tests were able to identify about the nature of specific factors that may contribute or relate to poor SP compliance in clinical areas. For example, when examining the issue of clinical experience, those with less experience (less than a year) seemed to perform better at cleaning up spillages and disposing of sharps boxes, but worse at hand washing and showering. Similarly, those with over ten years' experience performed worse at cleaning spillages, hand washing, and showering. Although the issue of clinical experience did identify some areas in which there was less compliance than would be expected, it was the issue of clinical department in which participants were situated that produced a huge number of significant differences between compliance rates. By far the most ill-performing participants were those who worked within surgical wards, who consistently demonstrated lower levels of compliance than would be expected if all things were equal between departmental settings.
The issue of qualification did produce a number of differences, although this was perhaps the most inconclusive avenue of investigation, for whereas those with Bridging qualifications were less compliant in two areas, those with BSN and masters were also at fault across the other two identified areas. It is also of note - and perhaps this could be considered one of the most telling findings from this study - that there were a number of areas, including sharps management, PPE re-use, and hand washing protocols in which those who had received prior training in infection control performed worse than would be expected within the observed counts of compliance. This implies that there are either issues with the training that they were provided with, that this training happened too long ago and needs refreshing (data relating to the timing of training was however not collected for the study), or that there is an issue with the attitude of nurses following training that leads to them becoming blasé about following SPs in the manner that they should.
In conclusion, this has been a study that has examined an important and timely issue, and which has provided not only a descriptive insight into the level of compliance currently within units across the Tabouk region of Saudi Arabia but has also provided insights into some of the factors that may be involved within this situation. A timely and assertive response to these findings on a clinical level is urgently required to ensure that patient safety is preserved and the quality of care that is delivered is of a suitably high standard.
The implications of this work indicate that there is much more to be done to improve the compliance rates of nurses in Saudi Arabia in relation to the SPs. Some of this data could, for example, be used to target areas of particularly poor practice – within surgical wards, for example – although based on the descriptive findings, all areas need input to ensure compliance rates rise. Another core implication is the need for regular evaluation of training courses to take place, to identify the effectiveness of particular forms and frequencies of training in relation to infection control. The fact that those who had previously received training were less compliant in a number of areas indicates that a thorough review of this area is needed. It is recommended therefore that based upon the findings of this study, a process of stringent clinical governance - an effective means of boosting quality and raising safety levels [23] - is conducted across the departments that took part in this research. It is further recommended that new training interventions are developed and evaluated, both on an immediate level and to examine the long-term impact on compliance.
Author Contribution
Study conception and design: HA
Data collection: NA, HA
Data analysis and interpretation: HA,NA
Drafting of the article: HA
Critical revision of the article: HA,NA
References
- Alshammari F, Cruz JP, Alquwez N, Almazan J, Alsolami F, et al. (2018) Compliance with standard precautions during clinical training of nursing students in Saudi Arabia: A multi-university study. J Infect Dev Ctries 12: 937-945.
- Alsofayan YM, Althunayyan SM, Khan AA, Hakawi AM, Assiri AM (2020) Clinical characteristics of COVID-19 in Saudi Arabia: A national retrospective study. J Infect Public Health 13: 920-925.
- Amoran OE, Onwube OO (2013) Infection control and practice of standard precautions among healthcare workers in northern Nigeria. J Glob Infect Dis 5: 156-163.
- Bunniss S, Kelly DR (2010) Research paradigms in medical education research. Med Educ 44: 358-366.
- Cheng KK, Lam TH, Leung CC (2020) Wearing face masks in the community during the COVID-19 pandemic: Altruism and solidarity. Lancet.
- Cohen J (1992) A power primer. Psychol Bull 112: 155-159.
- Colet PC, Cruz JP, Alotaibi KA, Colet MKA, Islam SMS (2017) Compliance with standard precautions among baccalaureate nursing students in a Saudi university: A self-report study. J Infect Public Health 10: 421-430.
- Creswell JW, Creswell JD (2017) Research design: Qualitative, quantitative, and mixed methods approaches. SAGE Publications.
- Donati D, Biagioli V, Cianfrocca C, De Marinis MG, Tartaglini D (2019) Compliance with standard precautions among clinical nurses: Validity and reliability of the Italian version of the Compliance with Standard Precautions Scale (CSPS-It). Int J Environ Res Public Health 16: 121.
- Efstathiou G, Papastavrou E, Raftopoulos V, Merkouris A (2011) Factors influencing nurses' compliance with Standard Precautions in order to avoid occupational exposure to microorganisms: A focus group study. BMC Nurs 10: 1.
- Rawbone R (2008) (2008) The Oxford textbook of clinical research ethics. In: Emanuel EJ, Grady CC, Crouch RA, Lie RK, Miller FG, Wendler D (Editors). Oxford University Press.
- Field A (2013) Discovering statistics using IBM SPSS statistics. SAGE.
- Gammon J, Morgan?Samuel H, Gould D (2008) A review of the evidence for suboptimal compliance of healthcare practitioners to standard/universal infection control precautions. J Clin Nurs 17: 157-167.
- Huang Z, Zhao S, Li Z, Chen W, Zhao L, et al. (2020) The battle against coronavirus disease 2019 (COVID-19): Emergency management and infection control in a radiology department. J Am Coll Radiol 17: 710-716
- Israel M, Hay I (2006) Research ethics for social scientists. SAGE.
- Joob B, Wiwanitkit V (2020) COVID-19 in medical personnel: Observation from Thailand. J Hosp Infect 104: 453
- Kumar S, Mohri M, Talwalkar A (2012) Sampling methods for the Nyström method. J Mach Learn Res 13: 981-1006
- Lam SC (2014) Validation and cross-cultural pilot testing of compliance with standard precautions scale: Self-administered instrument for clinical nurses. Infect Control Hosp Epidemiol 35: 547-555.
- Luo Y, He GP, Zhou JW, Luo Y (2010) Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis 14: e1106-e1114.
- Makary MA, Daniel M (2016) Medical error—the third leading cause of death in the US. BMJ 353
- Mann CJ (2003) Observational research methods. Research design II: Cohort, cross sectional, and case-control studies. Emerg Med J 20: 54-60.
- McCoy KD, Beekmann SE, Ferguson KJ, Vaughn TE, Torner JC, et al. (2001) Monitoring adherence to standard precautions. Am J Infect Control 29: 24-31.
- McSherry R, Pearce P (2011) Clinical governance: A guide to implementation for healthcare professionals, 3rd Edition. John Wiley & Sons
- Mersal FA, Keshk LI (2016) Compliance to standard precautions among nurses working in Qassim hospitals in KSA. Int J Basic appl Sci 5: 210-214.
- Mertens DM, Ginsberg PE (2009) The handbook of social research ethics. SAGE.
- Moralejo D, El Dib R, Prata RA, Barretti P, Corrêa I (2018) Improving adherence to Standard Precautions for the control of health care?associated infections. Cochrane Database of Sys Rev 2: CD010768.
- Mubaraki MA, Aboshaiqah A, Tumala RB, Hafiz TA, Shamali IM, et al. (2017) Infection control practices of Saudi baccalaureate nursing students during clinical training. EC Microbiology 13: 55-64.
- Nishiura H, Oshitani H, Kobayashi T, Saito T, Sunagawa T, et al. (2020) Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID-19). MedRxiv
- Odor PM, Neun M, Bampoe S, Clark S, Heaton D, et al. (2020) Anaesthesia and COVID-19: Infection control. Br J Anaesth 125: 16-24.
- Oliver P (2010) The student's guide to research ethics. McGraw-Hill Education, UK.
- Osborne S (2003) Influences on compliance with standard precautions among operating room nurses. Am J Infect Control 31: 415–423
- Powers D, Armellino D, Dolansky M, Fitzpatrick J (2016) Factors influencing nurse compliance with Standard Precautions. Am J Infect Control 44: 4-7.
- Rahmqvist M, Samuelsson A, Bastami S, Rutberg H (2016) Direct health care costs and length of hospital stay related to health care-acquired infections in adult patients based on point prevalence measurements. Am J Infect Control 44: 500-506.
- Velavan TP, Meyer CG (2020) The COVID-19 epidemic. Trop Med Int Health 25: 278–280.
- Watson K, Kottenhagen R (2018) Patients’ rights, medical error and harmonisation of compensation mechanisms in Europe. Eur J Health Law 25: 1-23.
41340
References
- Alshammari F, Cruz JP, Alquwez N, Almazan J, Alsolami F, et al. (2018) Compliance with standard precautions during clinical training of nursing students in Saudi Arabia: A multi-university study. J Infect Dev Ctries 12: 937-945.
- Alsofayan YM, Althunayyan SM, Khan AA, Hakawi AM, Assiri AM (2020) Clinical characteristics of COVID-19 in Saudi Arabia: A national retrospective study. J Infect Public Health 13: 920-925.
- Amoran OE, Onwube OO (2013) Infection control and practice of standard precautions among healthcare workers in northern Nigeria. J Glob Infect Dis 5: 156-163.
- Bunniss S, Kelly DR (2010) Research paradigms in medical education research. Med Educ 44: 358-366.
- Cheng KK, Lam TH, Leung CC (2020) Wearing face masks in the community during the COVID-19 pandemic: Altruism and solidarity. Lancet.
- Colet PC, Cruz JP, Alotaibi KA, Colet MKA, Islam SMS (2017) Compliance with standard precautions among baccalaureate nursing students in a Saudi university: A self-report study. J Infect Public Health 10: 421-430.
- Creswell JW, Creswell JD (2017) Research design: Qualitative, quantitative, and mixed methods approaches. SAGE Publications.
- Donati D, Biagioli V, Cianfrocca C, De Marinis MG, Tartaglini D (2019) Compliance with standard precautions among clinical nurses: Validity and reliability of the Italian version of the Compliance with Standard Precautions Scale (CSPS-It). Int J Environ Res Public Health 16: 121.
- Efstathiou G, Papastavrou E, Raftopoulos V, Merkouris A (2011) Factors influencing nurses' compliance with Standard Precautions in order to avoid occupational exposure to microorganisms: A focus group study. BMC Nurs 10: 1.
- Rawbone R (2008) (2008) The Oxford textbook of clinical research ethics. In: Emanuel EJ, Grady CC, Crouch RA, Lie RK, Miller FG, Wendler D (Editors). Oxford University Press.
- Field A (2013) Discovering statistics using IBM SPSS statistics. SAGE.
- Gammon J, Morgan?Samuel H, Gould D (2008) A review of the evidence for suboptimal compliance of healthcare practitioners to standard/universal infection control precautions. J Clin Nurs 17: 157-167.
- Huang Z, Zhao S, Li Z, Chen W, Zhao L, et al. (2020) The battle against coronavirus disease 2019 (COVID-19): Emergency management and infection control in a radiology department. J Am Coll Radiol 17: 710-716
- Joob B, Wiwanitkit V (2020) COVID-19 in medical personnel: Observation from Thailand. J Hosp Infect 104: 453
- Kumar S, Mohri M, Talwalkar A (2012) Sampling methods for the Nyström method. J Mach Learn Res 13: 981-1006
- Lam SC (2014) Validation and cross-cultural pilot testing of compliance with standard precautions scale: Self-administered instrument for clinical nurses. Infect Control Hosp Epidemiol 35: 547-555.
- Luo Y, He GP, Zhou JW, Luo Y (2010) Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis 14: e1106-e1114.
- Makary MA, Daniel M (2016) Medical error—the third leading cause of death in the US. BMJ 353
- Mann CJ (2003) Observational research methods. Research design II: Cohort, cross sectional, and case-control studies. Emerg Med J 20: 54-60.
- McCoy KD, Beekmann SE, Ferguson KJ, Vaughn TE, Torner JC, et al. (2001) Monitoring adherence to standard precautions. Am J Infect Control 29: 24-31.
- McSherry R, Pearce P (2011) Clinical governance: A guide to implementation for healthcare professionals, 3rd Edition. John Wiley & Sons
- Mersal FA, Keshk LI (2016) Compliance to standard precautions among nurses working in Qassim hospitals in KSA. Int J Basic appl Sci 5: 210-214.
- Mertens DM, Ginsberg PE (2009) The handbook of social research ethics. SAGE.
- Moralejo D, El Dib R, Prata RA, Barretti P, Corrêa I (2018) Improving adherence to Standard Precautions for the control of health care?associated infections. Cochrane Database of Sys Rev 2: CD010768.
- Mubaraki MA, Aboshaiqah A, Tumala RB, Hafiz TA, Shamali IM, et al. (2017) Infection control practices of Saudi baccalaureate nursing students during clinical training. EC Microbiology 13: 55-64.
- Nishiura H, Oshitani H, Kobayashi T, Saito T, Sunagawa T, et al. (2020) Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID-19). MedRxiv
- Odor PM, Neun M, Bampoe S, Clark S, Heaton D, et al. (2020) Anaesthesia and COVID-19: Infection control. Br J Anaesth 125: 16-24.
- Oliver P (2010) The student's guide to research ethics. McGraw-Hill Education, UK.
- Osborne S (2003) Influences on compliance with standard precautions among operating room nurses. Am J Infect Control 31: 415–423
- Powers D, Armellino D, Dolansky M, Fitzpatrick J (2016) Factors influencing nurse compliance with Standard Precautions. Am J Infect Control 44: 4-7.
- Rahmqvist M, Samuelsson A, Bastami S, Rutberg H (2016) Direct health care costs and length of hospital stay related to health care-acquired infections in adult patients based on point prevalence measurements. Am J Infect Control 44: 500-506.
- Velavan TP, Meyer CG (2020) The COVID-19 epidemic. Trop Med Int Health 25: 278–280.
- Watson K, Kottenhagen R (2018) Patients’ rights, medical error and harmonisation of compensation mechanisms in Europe. Eur J Health Law 25: 1-23.