Abstract
COVID is a fast-mutating virus that understands the dynamics of the ACE 2 pathways. It is a biphasic disease with three tiers of intervention.
The initial phase is viremic and is optimal for treatment with anti-viremic drugs that target viral replication in distinct parts of viral replication cycle e.g. protease inhibitors like Lopinavir/ Ritonavir and medications that containerize the COVID particles e.g. hydroxychloroquine. This is supplemented by drying inhalers e.g., Breztri or ipratropium bromide that decrease COVID rich secretions going into the lung alveoli.
The addition of H1 blockers e.g., Benadryl prevents the escalation of the bradykinin storm into the cytokine storm. The addition of JAK 2 inhibitors e.g., famotidine shuts down the progression into the cytokine storm.
This phase progresses by 8th-10th day if left unchecked to the second phase (the cytokine storm) where the body creates an acute inflammatory response causing severe damage. This results in thrombosis and pulmonary embolism. The second phase requires both antiviral medications, high dose steroids, famotidine, Benadryl, steroid inhalers e.g., Breztri and Pulmicort as well as Interleukin 7 blockers e.g., Tocilizumab if available.
Once thrombosis or pulmonary embolism has been identified appropriate anti-thrombotic like Eliquis is essential.
The third tier of intervention is identifying and treating the atypical bacteria, viruses and fungi that arise from the immunodeficiency’s that temporally arise from COVID infection.
Keywords
ACE 2 receptors; Bradykinin storm; Hyaluronic acid; Ground glass; Pulmonary embolism; Diarrhea; Smell; Taste; Headache; Facial nerve; Mastoiditis, ACE 2 inhibitors; ARB blockers; Ibuprofen; JAK 2 inhibitors; Famotidine; HIV1,HIV2; SIMV; Spike protein; Viremia; Cytokine storm; Thrombosis; Breztri; Ipratropium bromide; Alevesco; Pulmicort; Monoclonal antibodies; Benadryl; Hydroxychloroquine; Lopinavir/Ritonavir; Protease inhibitor; Nirmatrelvir/Ritonavir; Remdesivir; Renal toxic; Ivermectin; RNA replicase; TMPRSS2 inhibitor; High dose steroids; Prednisone; Interleukin 7 blocker; Tocilizumab; Atypical bacteria; Virus fungi; Clarithromycin; Levofloxacin; Valacyclovir
Introduction
In order to comprehend how a disease manifests we have to understand the anatomy, physiology, and pharmacology of the body as well as the modus operandi of the pathogen. COVID 19 targets the ACE 2 receptor of the body and like other similar viruses e.g., Middle East Respiratory Syndrome virus encroaches on the pulmonary CD4 cells resulting in secondary atypical infections [1].
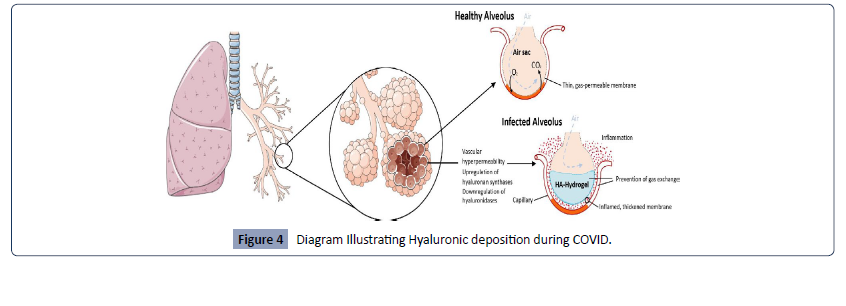
ACE2 receptors are ubiquitous (Figure 1) in the epithelia of the body. ACE 2 enzymes activate bradykinin resulting in increased cellular permeability. The net result of activation is a collection of fluid which is mopped up by secretion of hyaluronic acid notably in the lungs giving the appearance of ground glass on X ray and CT scans [7].S
Figure 1: Diagram illustrating key ACE Receptors.
As the ACE 2 pathways are activated the patient feels acutely short of breath with fluid accumulation in the alveoli, in the pulmonary vessels this activation of ACE 2 receptors leads to a pulmonary embolism [2-7 ] if left unchecked. In the gastrointestinal system the ACE 2 activation causes secretions of fluids with resultant diarrhea. Activation of ACE receptors in the olfactory neuroepithelium results in loss of smell [3] and subsequent taste as the facial nerve is involved. COVID transverses into the basal cisterns causing inflammation with sequential headaches [3,4].
The resultant increase in pressure in the basal cisterns results in elevated intracranial pressure with subsequent release through the path of least resistance i.e. the internal auditory canal. This occurs in the subarachnoid space causing enhancement of the mastoid segment of the facial nerve [5] and mastoiditis [6]. ACE 2 inhibitors, ARB blockers & Ibuprofen upregulate ACE 2 expression. Hence, I change the ACE inhibitors to alternate blood pressure medications in COVID 19 patients. Additionally, I specifically request the patient to AVOID Ibuprofen for Fever.
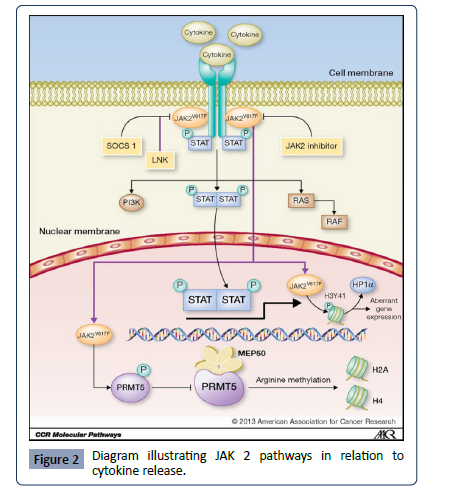
The body also has a novel cytokine signaling pathway activated by the JAK2 pathway that can be blocked by JAK 2 inhibitors [8] famotidine, apoquel and baricitinib limiting the progression pathway set up by ACE2 receptor activation. I standardly give Famotidine 40 mg bid to delay the onset of the inflammatory response (Figure 2).
Figure 2: Diagram illustrating JAK 2 pathways in relation to cytokine release.
COVID 19
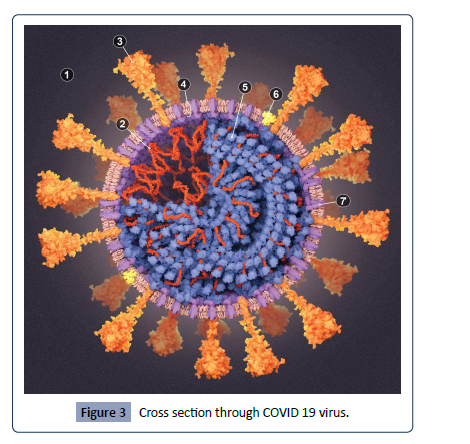
Coronaviruses were initially discovered in 1964 by June Almeida in Glasgow. They are common commensals found in the back of the nose and throat. They have a hallmark crown type accessories externally which harbors the spike protein to attach to the ACE receptor. Internally COVID 19 is an RNA virus with 16 gene fragments of HIV1, HIV2 and SIV [9]. COVID 19 is 1000 times more powerful in attaching to the spike protein compared to Almeida’s coronaviruses (Figure 3).
Figure 3: Cross section through COVID 19 virus.
COVID 19 sits on facial hair and in ventilation systems, studies from Bergamo [10] and Harvard [11] confirm it sits on particulate matter in the air, hence higher incidences of COVID 19 in more polluted atmospheres.
Bronchoalveolar lavages of COVID 19 patients show elevated levels of hyaluronic acid due to up regulation of hyaluronic synthases & down regulation of hyaluronidase [12]. Combined with increased lung hyper permeability from Bradykinin release Hyaluronic acid mops up fluid.
Hyaluronic acid inhibits gas exchange, damages alveoli in inappropriate ventilator settings. (US has the highest mortality rate) (Figure 4).
Figure 4: Diagram Illustrating Hyaluronic deposition during COVID.
COVID 19 TREATMENT
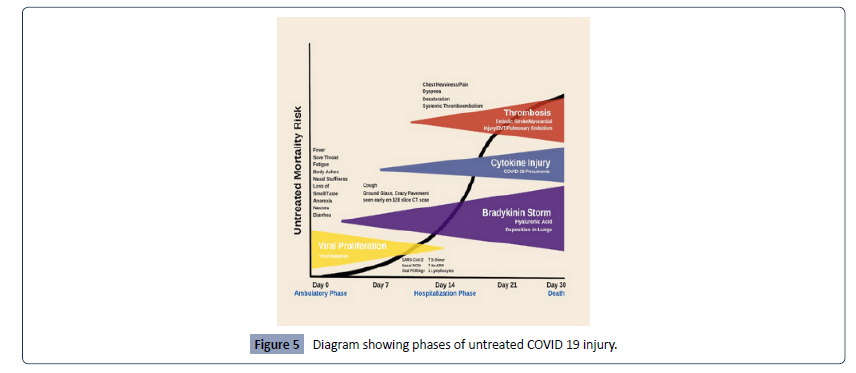
COVID 19 is a biphasic condition if left unchecked results in pulmonary embolism. The first step is a viremic phase which lasts 7-10 days where a four-phase approach can bring the viral load down.
The second step is a host mediated reaction with a cytokine storm and thrombosis which requires medications from the first step along with high dosage steroids and additional medications to stop the cytokine storm and thrombosis. Sadly, studies have been done using antivirals without adequately dosed steroids in the second step of this condition reflecting a poor understanding of the disease.
The enclosed diagram (Figure 5) summarizes COVID 19 injury with clinical signs and phase of the disease.
Figure 5: Diagram showing phases of untreated COVID 19 injury.
Step 1 phase 1 treatment
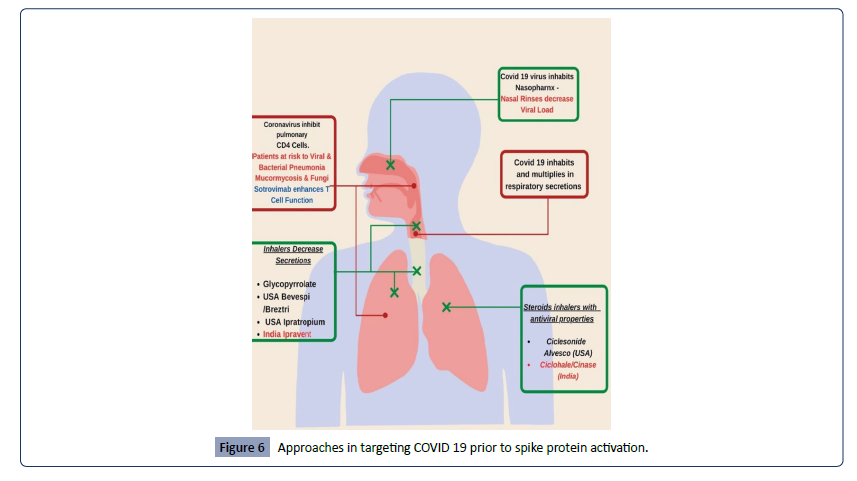
The objective here is to prevent Spike protein adhering to the ACE 2 receptors and stop the bradykinin storm. Monoclonal antibodies prevent adherence but can take 2 to 6 days for the viral load to come to zero. Hence it is important to watch out for thromboembolic phenomenon. Benadryl allergy or Zyrtec will shut down the bradykinin storm (Figure 6).
Figure 6: Approaches in targeting COVID 19 prior to spike protein activation.
This can be done by nasal rinses targeting the back of the nose/ throat area with normal saline. It is simple and most effective as COVID sits at the back of the nose/throat. Additionally, inhalers that dry up the respiratory secretions such as Bevespi/Breztri (containing glycorrpyrrolate) or Ipratropium Bromide. Other inhalers with antiviral and steroid properties are Alvesco and Pulmicort and these can be used along with a drying inhaler.
Step 1 phase 2 treatment
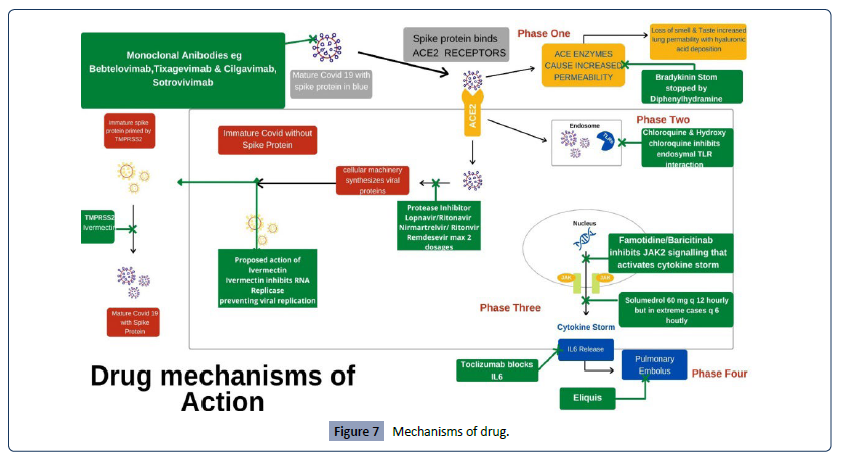
This acknowledges that the spike protein of COVID 19 has adhered to the ACE 2 receptor and the drugs target viral multiplication (Figure 7). These include Hydroxychloroquine which containerizes COVID 19. Protease inhibitors such as Lopinavir/Ritonavir. Nirmatrelvir/Ritonavir and Remdesivir which target viral replication. Remdesevir should not be given to renal impaired patients and no more than two dosages due its renal toxicity. Nirmatrelvir/Ritonavir has multiple drug interactions and I have to stop those drugs when I Use Nirmatrelvir/Ritonavir. There is increasing failure to Nirmatrelvir/Ritonavir as the virus mutates.
Figure 7: Mechanisms of drug.
Additionally, Ivermectin can also be used as it inhibits RNA replicase and is a TMPRSS2 inhibitor preventing the attachment of the immature spike protein during viral replication.
I normally use both a protease inhibitor and HCQ together to expedite viral load reduction and the multidrug approach delays the mitigation of variant resistance viruses.
Those who do have reliable sources of Ivermectin I encourage the addition of 12 mg of Ivermectin daily. Higher dosing can cause dizziness, tachycardia, uveitis, and keratitis resulting in diminished visual acuity. It is important to realize that COVID is a highly inflammatory condition and daily 325 mg aspirin reduces the risk of vascular occlusive disease.
Step 1 phase 3 treatment
The objective here is to stop the progression into the cytokine storm using JAK 2 inhibitors like famotidine, apoquel and baricitinib. Famotidine at 80 mg per day shuts down the cytokine storm pathway.
Step 2 treatment (phase 4)
This presents after 10 days or has had sub therapeutic earlier treatment. The objective is to decrease inflammation by using high dose steroids e.g., prednisone 60 mg bid and treats any thrombo-embolic diseases with Eliquis. Very often people need oxygen supplementation. Cura signa has developed an oxygen concentrator capable of delivering 10 L of continuous oxygen in a non-hospital setting, significantly more than the standard 6 L of continuous flow found in hospitals. Interleukin 7 blockers e.g., Tocilizumab is used at this stage to quell the cytokine storm. Most notably President Trump had this released to the UK for Boris Johnson’s COVID treatment.
Additionally, as we precede the risk of atypical bacterial ,viral and fungal infections mandating clarithromycin/Levaquin/doxycycline or valacyclovir or suitable antifungal.
Clinically it is difficult to break down the individual phases hence I treat giving a 10-day regimen of all the drugs listed from the time I first see the patient.
Patient # 1
• 44 male presents after Christmas family gathering. PMHX: type 1 Diabetes x 39 yrs., BMI 36, Sleep apnea, ARDS 2004 with:
1. Intermittent dry cough X 7 days
2. Sore throat X 3 days
3. Diarrhea 1-2 days
4. Constant headache x 5 days
5. New onset shortness of breath Pulse oximetry 95% with fever x 1 day no chills
6. Loss of taste and smell x 5 days
7. COVID PCR positive.
8. Started on lopinavir/ritonavir, hydroxychloroquine, aspirin, clarithromycin, Benadryl, clarithromycin, Medrol dose pack
9. Patient referred to Monoclonal antibody center, He received Bamlanivimab (the then current monoclonal antibody) infusion on day 9.
10. The infusion staff told him everything OK and they will call him in a week.
11. Patient did not follow up as requested for daily checks.
12. Patient returns on day 14 short of breath on walking up I flight stairs.
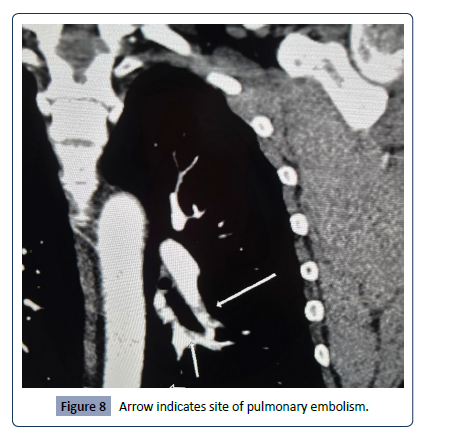
13. CT angiogram chest confirmed a pulmonary embolism: (Figure 8).
Figure 8: Arrow indicates site of pulmonary embolism.
Additionally, CT scan showed multiple ground glass opacities in both lungs compatible with COVID Pneumonitis.
Patient refused hospitalization, as sister placed on ventilator in ICU
Patient started on:
Eliquis 10 mg bid for pulmonary embolism
Famotidine 40 Mg qd. Started
IV solumedrol 60 mg bid x 5 d & Prednisone Taper.
IV ceftriaxone 2 gm qd x 5 days followed by oral clarithromycin 500 mg bid.
Incentive spirometry
10 days after monoclonal antibody infusion, the patient develops fever and chills. Started on Valtrex 1 gm tid x 7 days. Chills resolved after 24 hours
Patient returned to work 3 weeks after initial COVID infection. His sister returns home 4 weeks after the initial COVID infection with supplemental Oxygen.
Patient # 2
• A 67-year-old 115 lb. female horse dressage trainer presents 12 days after a positive COVID test. PMHx significant for asthma
• She had seen a MD who had prescribed her amoxicillinclavulanate 875 mg-125 mg and prednisone 60 mg qd for 10 days.
• She was acutely short of breath and still COVID positive
Started on
• Aspirin 325 mg.
• Lopinavir/Ritonavir 200-50 two tabs bid #40.
• HCQ 200 mg 2 tabs bid #40.
• Prednisone 60 mg bid.
• Clarithromycin 500 mg bid.
• Famotidine 40 g bid.
• Benadryl 25 mg am and Cetirizine 10 mg qhs.
• Breztri & Alevesco 2 puffs twice daily.
• CT angiogram of the Chest ordered in a 128 Slice scanner.
CT Angio Chest confirms an early right lower lobe pulmonary embolus.
Globular ground glass appearance in both lung fields consistent with COVID 19 pneumonitis and scarring of both lung bases.
Started patient on Eliquis 10 mg bid x week
Started patient on iv Ceftriaxone 2 gm and solumedrol 60 mg bid x 5 days
• On day 18 of COVID patients get yeast infection and senses onset of oral Herpes.
• Patient started on valacyclovir 1 gm tid x week and given fluconazole 150 mg qd.
• Oxygen saturation restored to 95% and at home oxygen at 2 L started. On day 20 of COVID oxygen saturation 97%.
• On day 21 of COVID solumedrol dropped to 60 mg qd.
• On day 22 of COVID oxygen saturation 98% on 2 L oxygen started on Incentive spirometry and clarithromycin 500 mg bid.
• Over the next 6 weeks steroids decreased and oxygen stopped.
• Three months later a repeat CT angiogram done in the same 128 slice scanner confirmed resolution of the pulmonary embolus and pneumonitis.
Patient # 3
A 59-year-old male patient who recently received a heart transplant on immunosuppressive medications with a past medical history of Insulin dependent diabetes, sleep apnea gets sore throat, fever and chills from his children who tested positive for COVID. He tests positive for COVID,
The patient was directed to the transplant unit who admitted him and gave him four dosages of remdesevir, closely monitoring his renal function. He was discharged 5 days later with a Bronchitis cough, producing green phlegm with low grade fever and chills. Patient was started immediately on Lopinavir/Ritonavir. HCQ, Clarithromycin, Benadryl and Pulmicort inhaler, within 10 days chest is clear with no symptoms.
Discussion
COVID has killed over a million people in the US, the Fauci approach of stay at home for 2 weeks and return to your physician if there is a problem loses the valuable opportunity of stopping the progression of this condition in the viremic phase. Secondly it gives time for the virus to take hold and increases the risk of long term COVID.
COVID is a three step disease, the initial phase till day 10 is viremic, but as you approach day 10 you enter the period where the body produces a highly inflammatory reaction requiring high dose steroids along with the anti virals to arrest progression.
The third most important thing to understand that COVID’s immunosuppression causes the rise of atypical bacterial pneumonia, viral pneumonia and fungal infections you have to be aware and treat accordingly.
Not all drugs are created equal, this current administration has let go of monoclonal antibodies which have shown a lower mortality rate than Nirmatrelvir/Ritonavir and paid premium costs. There is increasing failure of Nirmatrelvir/Ritonavir as the virus continues to mutate. Remdesivir has serious nephrogenic possibilities to one kidney patients and those in renal failure In the US it is still administered as a front line treatment whilst in other countries it has been stopped. To prevent resistance we should adopt a multidrug approach and understand the downs stream risks of atypical bacterial, viral pneumonia with fungal infections and treat early.
We have to look in the mirror and understand our wilful ignorance is the cause of the million dead in the USA today. We have to stop living in fear, be bold and treat COVID aggressively and avoid long term complications.