Review Article - (2022) Volume 0, Issue 0
Covid-19 Post-Acute and Chronic Disease
Celi E1*,
Espinoza C2,
Paredes A3,
Montenegro M4 and
Velin D5
1General Physician, Universidad de las Americas, Quito, Ecuador
2General Physician, Universidad de las Americas, Quito, Ecuador
3Americas, Quito, Ecuador
4General Physician, Universidad Central de Quito, Ecuador
5General Physician, Universidad Tecnológica Equinoccial de Quito, Ecuador
*Correspondence:
Celi E, General Physician, Universidad de las Americas, Quito,
Ecuador,
Email:
Received: 18-May-2022, Manuscript No. Iphsj-22-12784;
Editor assigned: 20-May-2022, Pre QC No. Iphsj-22-12784 (PQ;
Reviewed: 03-Jun-2022, QC No. QC No. Iphsj-22-12784;
Revised: 09-Jun-2022, Manuscript No. Iphsj-22-12784(R);
Published:
17-Jun-2022, DOI: 10.36648/1791-809X.16.S7.951
Abstract
A new coronavirus emerged in Wuhan-China at the end of 2019, apparently originating in a wholesale seafood market in that city due to the passage of the virus from a wildlife animal, probably a bat or pangolin, to humans. This coronavirus achieved an important adaptation in the body and generated a new disease that was called COVID-19, which causes Acute Respiratory Distress Syndrome (ARDS). Little is really known about the possible medium and long-term consequences of this new disease. Many of the patients, due to the severity of their disease and/or due to the invasive management established in them, will develop squeal that could be permanent and that in one way or another are plausible through extensive tests requested by the health personnel. Likewise, it is essential to take into account the knowledge provided by past epidemics caused by other similar coronaviruses, which at the time generated the Severe Acute Respiratory Syndrome (SARS) of 2003 and the Middle East Respiratory Syndrome (MERS) of the 2012. Therefore, in this bibliographic review, the medium and long-term consequences that other coronaviruses have generated and that could generate the one that has been called severe acute respiratory syndrome coronavirus type 2 (SARS�CoV-2) will be exposed.
Keywords
Syndrome; Covid-19; Persistent Covid; Post-acute; Chronic; Long covid;
covid Long haulers; Long haul covid
Introduction
Due to the recent appearance and identification of a new
coronavirus at the end of 2019, little is known about the possible
consequences in the medium and long term. Many of the patients
due to the severity of their disease and/or due to the invasive
management established in them will develop squeal that could
be permanent and that in one way or another are plausible
through extension tests requested by health personnel. However,
the concern lies not only in them, but also in those people who
carry symptoms for months and who in their vast majority were
initially classified as "mild" and managed on an outpatient basis. It
is worth mentioning that, in some of them; it has not been possible
to identify an apparent structural or functional damage that
justifies the symptomatology. It is based on the latter, on patterns
of symptomatology that are evident and on the association of
chronicity with the number of symptoms and their characteristics
during the acute phase, that it has begun to speculate on the
possible causes, within them: the existence of a viral persistence,
an unbalanced immune response characterized by post-viral
hyperactivity of the same, presence of autoantibodies, due to
entities such as small fibre neuropathy, or to pathophysiological
processes similar to myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS), fibromyalgia (FM), central sensitization
syndrome (CFS), orthostatic postural tachycardia syndrome
(POTS), autoimmune autonomic ganglionopathy (GAA), the
disease of small vessels (microangiopathy), deconditioning, a
deficiency state perpetuated mainly by a vitamin deficit such
as those of the B complex, psychiatric disorders that eventually
lead to the somatization of the symptomatology even reaching to
mimic the symptoms of COVID-19, among others [1,2].
On the other hand, it is interesting the knowledge that the past
epidemics caused by other similar coronaviruses have provided
us, that is the Severe Acute Respiratory Syndrome (SARS) of 20031
and the Middle East Respiratory Syndrome (MERS) of 2012 on
persistent symptoms and post-viral syndromes. On the one hand,
it has come to identify countless studies that corroborate the fact
that coronaviruses are very versatile viruses, with a surprising
ability to adapt to organisms and endowed with extremely
effective immune system evading mechanisms, thus generating
very diverse symptoms, variable in intensity and that could last
for an indefinite time. On the other side of the coin, we have
post-viral syndromes, which have already been documented,
but which, nevertheless, remain little known and recognized by health personnel. This is probably due to the fact that the
scientific community in one way or another has ignored research
in this regard due to how infrequent or rather how infrequent
they used to be, the complexity of them and the need to solve
problems that at the time, were more emerging or priority
for health systems. This pandemic may be the opportunity to
interfere in depth in the research of both persistent infectious
diseases and post-viral syndromes, in order to better understand
these processes, and thus provide affected patients with a more
effective and efficient treatment than has been done so far.
Without further ado, we will present in the following section
a bibliographic review of the past and present regarding the
medium and long-term consequences that other coronaviruses
have generated and that could generate what has been called
coronavirus type 2 of severe acute respiratory syndrome (SARSCoV-
2).
Materials and Methods
To carry out this article, a bibliographic search was carried out
in various databases such as Elsevier, Scielo, Medline, PubMed,
Science Direct and Ovid, thus selecting original articles, case
reports and bibliographic reviews from 2018 to 2021, in Spanish
and English using MeSH terms: Syndrome, covid-19, persistent
covid, post-acute, chronic, long-distance carriers, long distance
covid, and Boolean operators and and or. Thus including all the
documents that will deal with post-acute and chronic covid-19
disease, the data found were between 35-45 records, thus using
40 articles for the realization of this document.
Review
Definition
Given the attempt of countries to avoid the greatest number of
deaths from COVID-19, the attention and research of a group of
patients who persist with signs and symptoms after 3 weeks from
the beginning of the picture has been reduced. These patients
are very heterogeneous, which is why it has been difficult to
pigeonhole them into a definition and classify them given that
COVID-19 generates a significant multisystem condition with a
temporal course that, to date, is unclear. Many patients have
not even necessarily had a "moderate" or "severe" disease, but
they have not managed to resume their lives in a normal way,
because in many cases, the symptomatology is so flowery that it
is detrimental to the quality of life, even, in a not inconsiderable
subgroup, it has become disabling. That is why, in search of
defining them, they have come to be called in different ways;
in Spanish as "covid-19 persistent", "covid-19 chronic" and in
English as "long haul COVID-19", "covid long-haulers" or simply
as "long covid".
According to two published articles, the first by the Department
of Biology and Biomedical Sciences at Aga Khan University in
Pakistan and the second published in the journal Jama Network,
there is no clear consensus on the definition of the medium
and long-term effects generated by COVID-19. Well, according
to the first, it is of the utmost importance to designate a name
that has been called "long covid" or "covid long haulers", thus proposing the possibility of naming it as other existing syndrome
processes, either of infectious or non-infectious etiology that
exceed 3 weeks from its beginning, that is, as chronic COVID-192.
According to the second article and supported by the Spanish
Society of Physicians of
Primary Care, it has been considered to opt for a variation to the
aforementioned one, defining COVID-19 in two ways: as postacute
and as chronic [3].
According to the duration of the
symptomatology
• Post-acute Covid-19: It is one that exceeds 3 weeks from
the onset of the disease.
• Chronic Covid-19: It is one that exceeds 12 weeks from
the onset of the disease3.
At the moment, we believe that this classification is the most
appropriate, because considering it as chronic after 3 weeks
could be precipitous since many patients will present a complete
resolution of their symptoms before 3 months, as we will see
later.
According to the clinical characteristics of the
affected patients
It is important to emphasize that those patients who suffer from
both post-acute-chronic COVID-19 are very heterogeneous in
their vast majority. Through an attempt to classify them, we will
divide them into three groups:
1. Those that have a nonspecific disease. Most cases usually
present with fatigue and/or dyspnea as cardinal symptoms4.
The damage and symptoms are not necessarily permanent, but
recovery may take extended periods of time. Mostly, they are
those patients who have been managed on an outpatient basis
with symptomatic treatment [4].
2. Those who have squeal as a result of the disease4, such as,
for example; pulmonary fibrosis, complications associated with a
pulmonary embolism, a stroke, among others. These tend to be
permanent. They are patients who have mostly been hospitalized.
In any case, it has been evidenced that, after discharge, some of
them have developed thrombotic events in the weeks or even
months after the acute phase.
3. Those patients who have required intensive care and who
develop after discharge, a post-intensive care syndrome4. These
patients present temporary and/or permanent symptoms caused
both by the same hospital stay, as well as by invasive and noninvasive
procedures established in the Intensive Care Unit (ICU). is worth mentioning that this classification is not absolute.
Eventually they can overlap each other.
Possible causes
In this article, we will focus on point one according to the
classification made previously, because as we have seen, it is
a group in one way or another little recognized and that needs
immediate answers.
According to an article published in The BMJ, it is not known
exactly what generates the persistence of the symptomatology.
However, some hypotheses have been raised, which will be
presented in the following section:
1. Viremia due to a weak or absent antibody response.
2. Relapse or reinfection.
3. Inflammatory reactions and other immune reactions.
4. Deconditioning.
Mental factors such as post-traumatic stress4. On the other hand,
according to a video published by Dysautonomia International,
the possible mechanisms of persistence of symptomatology are
the following:
1. Persistent SARS-CoV-2 infection.
2. Secondary infection.
3. Resolution of infection, but persistence of tissue damage.
4. Resolution of infection, but persistence of the immune response.
5. Deconditioning
6. Other things still unknown
A combination of them: probably point 3, 4, and 5 according to
the author's opinion5.
On the analysis of these points and the evidence acquired in
the literature review, we believe that the persistence of the
symptomatology is probably due to
1. A persistent-chronic viral infection caused by an inadequate
immune response of the host during the acute phase (includes
viral persistence in the same inflammatory and nerve cells),
accompanied by tissue injury probably triggered by the same viral
replication and consequently an acute inflammatory state that
ultimately progresses into a chronic, low-intensity inflammatory
process, but significant enough to generate signs and symptoms.
In addition, it is possible that there is a deficiency state and a
state of deconditioning either due to the same disease and / or
inactivity.
2. Denervation or neuronal loss and/or endothelial damage
during the acute phase, accompanied by a chronic post-viral
inflammatory state probably due to immune system disease,
perhaps with autoimmune behavior, accompanied by a deficiency
state, and a state of deconditioning caused either by the disease
itself and/or by inactivity [5].
Viral persistence
Persistent viral infection is a condition caused by the entry of a
certain virus into the body generating or not symptoms in the
acute phase and that can last in the body for an indefinite time
(weeks, months or years). These infections may or may not
generate clinical manifestations without killing quickly or causing
excessive damage to the body.
According to the evidence currently available, viruses not only
generate acute illness, but can also generate persistent infection due to their ability to remain in cells after the end of the acute
phase of the disease. This persistence allows the virus to replicate
constantly without generating cell death [6].
Persistent infections can be classified as
• Chronicles: Those that can manifest as a long-term infection,
in which the virus continues to replicate even at low levels for
an indefinite time despite the immunity generated, and may
also produce fluctuating symptoms or even appear after several
years.
• Latent: They are characterized by being inactive within a cell,
that is, they can remain hidden after the initial infection probably
because it does not provide transcription factors necessary to
produce viral replication. Reactivations may occur one or more
times under certain circumstances, such as; hormonal changes,
physical or psychological stress, etc. Both the first infection
and the reactivation can lead to symptoms and these remain
throughout life.
• Slow/prion infections: these affect only the central nervous
system because there is no or mild immune response. Generally
the first infection is asymptomatic however after several years
it can trigger a severe, progressive picture that can even lead to
death.
• Transforming infections: They are those in which the virus
is able to infect cells, but cannot produce viral particles in a
significant way that leads to cell destruction, however, part of
its genes are translated into viral proteins which cause cellular
changes through interaction with genes and proteins which could
lead to the formation of tumour’s whether benign or malignant.
In the event that we consider the possibility that SARS-CoV-2
generates a persistent infection, it would probably be chronic
due to its characteristics.
According to Boggs W, it is possible that SARS-CoV-2 is eliminated
slowly, especially in those patients suffering from primary
or secondary immunodeficiency. It is believed that they can
prolong both the disease and infectivity because their degree of
dissemination, immune clearance kinetics and disease severity
are different from that of immunocompetent patients [7].
In any case, we previously verified the fact that this
cannot necessarily occur in people with some degree of
immunosuppression, but also in immunocompetents by unclear
mechanisms. However, it could be caused by an ineffective
immune response in the acute phase of the disease, especially in
those patients managed on an outpatient basis [8].
Viral persistence in body fluids
Importantly, many patients over the weeks and months shed the
virus through various fluids. It should be noted that it has even
been identified in various tissues of the body. We will describe in
the next section, some studies that prove it.
In a 2003 cohort study in Beijing, patients who were likely
infected with SARS-CoV-1 were recruited from a hospital, based
mainly on criteria stipulated by the World Health Organization
(WHO). Stool and sputum samples were taken for several weeks of hospitalization and for months after discharge (6 months after
disease onset). 514 stool samples and 493 sputum samples were
collected from 56 patients during the study period. The results
showed that sputum and stool samples by RT-PCR did not show
negative results until day 14 and day 16 after the onset of the
disease, respectively. An average duration of viral excretion of 3
weeks in sputum and 4 weeks in feces was evident. In addition, a
prolongation in excretion (> 100 days after the onset of symptoms)
was observed in the feces of 4 patients, which probably suggests
that viral replication may take place in the intestinal tract.
3 of these 4 patients had co-existing conditions (pulmonary
tuberculosis, diabetes, and pulmonary hypertension), a known
risk factor for prolonged SARS-CoV-18 disease. The striking
thing is that viral excretion can be persistent in the feces even
exceeding 3 months from the onset of the disease. Something
to note is that the excreted virus appears not to have been
infectious. Something that has not been fully clarified with the
new coronavirus as we will see later.
In a study conducted in China, between January and March,
respiratory and fecal samples were collected and analyzed from
74 patients infected with SARS-CoV-2 by RT-PCR. It was evidenced
that in about 55% of patients, their fecal samples remained
positive for SARS-CoV-2 RNA for an average of 11.2 days longer
than respiratory samples, even lasting in some cases about 5
weeks after the respiratory tract samples became negative for
SARS-CoV-2 RNA. It is worth mentioning that severity was not
associated with the prolonged duration of viral RNA positivity of
the fecal sample [9].
A study conducted in Guangdong - China, a total of 49 patients
with SARS-CoV-2 were recruited. Mostly (43 patients) with
a mild course of the disease. Samples of pharyngeal smear,
nasopharyngeal, sputum and feces were obtained every 3 days for
4 weeks, which were analyzed by RT-PCR. In the study, persistent
viral RNA spread was evidenced in both nasopharyngeal and
stool samples. The estimated time to loss of viral RNA detection
ranged from 45.6 days for nasopharyngeal smear samples to
46.3 days for stool samples in mild cases, and 48.9 days for
nasopharyngeal smear samples and 49.4 days for stool samples
in severe cases. This was longer than evidenced with other
coronaviruses, i.e. SARS-CoV-1 and MERS-CoV. In this study, virus
isolation and sample infectivity tests were not carried out [10]. It
is again evident that viral excretion can last longer than expected.
Of positive results and symptoms in patients
recovered from Covid-10
According to Read S, the detection of SARS-CoV-2 can occur in
several scenarios
• In people who have recovered from the disease completely and
after it, viral RNA has not been detected in the upper respiratory
tract.
• In people in whom viral RNA continues to be detected after
a complete resolution of the symptomatology, even reaching in
some cases to persist for weeks.
• In people in which, after an apparent elimination of the virus
objectified by obtaining 2 negative viral RNA tests in the upper respiratory tract, and after that, they return to positivity, but
without presenting symptoms.
• Those people who have not presented clinical recovery and
who persist or resort to viral RNA positivity in nasopharyngeal
samples [11].
In those who do not present symptoms, the persistence of viral
RNA may not generate much concern. Based on other viruses
and with the evidence available to date on SARS-CoV-2, these
people would no longer be contagious. The concern basically lies
in those that do not present a resolution of the clinical picture
or that, after an apparent recovery, present new symptoms with
positive detection tests for SARS-CoV-2.
According to Syrek R, it is unclear why many patients continue to
test positive for long periods of time. As reported, some of them,
after having tested negative, with the passage of time come out
positive again, however, it is believed that they are probably no
longer infectious.
A German study mentions that patients with less than 100,000
copies of viral RNA/ml of sputum 10 days after symptoms have
"little residual risk of infectivity [12].
The case of a patient suffering from refractory mantle cell
lymphoma (MCL) and COVID-19 is reported concomitantly, the
patient was admitted several times due to a worsening of the
symptomatology after an apparent remission. On day 156 of the
disease, when the patient had been readmitted for progression of
his lymphoma, the SARS-CoV-2 test remained positive. It is worth
mentioning that samples grown in Vero E6 cells demonstrated
the presence of SARS-CoV2 from day 7 to 119 of the disease. Virus
sequencing demonstrated a progressive evolution with additional
substitutions over time, but phylogenetic analysis basically ruled
out reinfection7. For now, the question must be asked whether
this actually occurs exclusively in immunocompromised patients
or also occurs in those immunocompetent, as we will see below.
According to Rong Yang J, et al, by reporting one case, it was
possible to demonstrate that SARS-CoV-2 infection can have a
clinical course of more than two months. Well, in a 44-year-old
male patient, without precondition of immunosuppression, after
overcoming the acute phase evidencing clinical improvement
from day 15 to 32 approximately, with the negativization of viral
RNA by taking a pharyngeal swab and the formation of antibodies,
there was a reappearance of viral RNA approximately on day 36
of the disease, which persisted for more than 40 days (74 days
after the onset of the picture). In addition, something striking is
that viral persistence was identified in other types of samples,
especially in saliva with extremely high titers [13].
Gousseff et al presented a series of cases of 11 patients infected
with SARS-CoV-2 who presented two acute episodes of the disease
confirmed clinically and virologically. The median duration of
symptomatology was 18 days for the first episode and 10 days for
the second. 4 of the 11 were health care workers, with a median
age of 32.5, with no previous comorbidities, with mild illness and
made a full recovery. However, they had a relapse that did not
require hospitalization, with a symptom-free mean interval of 9
days. On the other hand, 7 patients with previous comorbidities, who underwent a second episode presenting new tomographic
findings. 4 of the 7 worsened, including one, leading to pulmonary
thromboembolism. There was no evidence of super infection
and no differential diagnosis. Here the possibility arises that
both health personnel due to their prolonged exposure and their
immune weakness, have been able to acquire a new infection.
On the other hand, the second group was vulnerable people,
in one way or another immunosuppressed and may also have
acquired a new infection by chance. Despite this, the possibility
of reactivation due to immunosuppressive factors, such as the
use of corticosteroids or due to an inflammatory rebound due to
an inadequate immune response, is also considered. However,
the fact that viral RNA has been detected in all patients – some
of them with a low cycle threshold – and that a viral strain could
be cultured during the second episode for one of them, supports
rather reinfection or reactivation [14].
We must be cautious with the last thing they mention, because so
far there is no solid evidence of the existence of new strains and
reinfection. It is likely that in reality they are genetic variations of
the same virus that are not enough to generate a change in the
behavior of the same and therefore a new immune response and
even less, in such a short period of time. However, reactivation
or replication of greater intensity resulting from a persistent viral
infection could justify the symptomatology.
According to an article published by Xia J, there are two
possibilities in cases where patients come back positive in tests
for SARS-CoV-2 RNA. The first reinfection, this is considered
unlikely because of the little evidence available in this regard, and
two, that there have been false negatives and that there is really
a viral persistence. The latter could be given by viral persistence
in immunologically privileged sites.
Means that there are places in the body that can tolerate the
existence of an antigen, without triggering an immune response.
This is probably due to an evolutionary mechanism that aims to
preserve the structures of the organism in the face of a possible
immune response, which, if it exists, would be detrimental to its
functionality. These sites are mainly: the eyes, placenta and fetus,
testicles, central nervous system (CNS) and hair follicles. This is not
something new, as it has been seen with other types of viruses,
such as Zika and Ebola. Ebola was detected in semen even 3 years
after the onset of infection, while Zika was detected 134 days
in semen after resolution of symptoms caused by the disease.
Interestingly, SARS-CoV-2 shares characteristics with these [15].
On the other hand, as described in an article published in The
Bmj, it is necessary to mention that long-term respiratory,
musculoskeletal and neuropsychiatric "squeal" have already
been previously documented in other coronaviruses (SARS
and MERS). In addition, it is emphasized that mild patients can
prolong their symptoms, within it cough, fever and fatigue, which
tends to be fluctuating, with eventual relapses and remissions,
with variation in intensity and form, even on the same day. They
consider that, for the majority of these patients, who do not
present significant evidence of structural or functional damage,
they will not need to be referred to a rehabilitation service and
that, with a progressive, controlled activity associated with
adequate follow-up with symptomatic treatment for the time being, it is sufficient until the results of the long-term studies are
available. In addition, a slow, gradual and complete recovery is
expected based on other causes of viral pneumonitis and ARDS
in most of them 7. Something that fortunately has been observed
in one way or another in patients who have been diagnosed with
COVID-19 and who persist with symptoms.
In another sense, this may be strengthened by Syrek R, who
mentions that even in those who are not considered to have
persistent symptoms; recovery after overcoming COVID-19 can
be difficult. Exercise tolerance can take 2 to 3 months or even
take longer to return to pre-COVID-1916 fitness [16].
Now, from our point of view, patients who have developed
post-acute COVID-19 may take a while to resume their normal
lives because it can be difficult to overcome convalescence not
only because of the ravages generated by the infection, but also
because of a process of deconditioning that can be resolved in
weeks or months. It is worth mentioning that in those who have
developed chronic COVID-19, this process could be longer and more
complex because both doctors and patients struggle not only against
deconditioning, but also against sequelae, deficiency states and
against a non-specific viral or post-viral disease that is still unknown.
On the other hand, according to the study described in previous
paragraphs published in the journal Jama Network, the most
frequent symptoms after the end of the acute phase are fatigue
and dyspnea3. While in another study conducted by the Spanish
Society of Primary Care Physicians, it was demonstrated through
a survey that fatigue and cough are the main symptoms [17].
So, the list is not limited to a few symptoms that persist after the
acute phase, rather it extends in the same way as the number of
patients who suffer from them increases. Well, support groups
have even been created on various websites, social networks,
and instant messaging services, mainly Facebook (e.g. Long Covid
Support Group, which currently has more than 50,000 members)
and Whatsapp (e.g. persistent COVID Spain), most likely caused
by the neglect they receive, or by the same incomprehension
and impotence of health personnel in the face of the difficulty
of their diagnosis and therefore of their management. It is worth
mentioning that, in these groups, stigmatization by their relatives
is emphasized because they were mostly classified as "mild"
cases and did not require hospitalization. This undoubtedly
makes management difficult, since the lack of support, ignorance
and lack of recognition by the family and health personnel can
eventually lead to or worsen the psychological/psychiatric
problems of the affected patients.
As we have shown, in part the rejection of doctors, and therefore
of the family towards patients, is given by the scarce evidence of
alterations in extension examinations, many of them even being
classified as "anxious" or as "patients who somatize" without any
foundation. This must be taken with tweezers, it is likely that it
is due to a real ignorance of the picture, because anxiety may be
part of the disease of patients but is not the cause of it. Aptly, as
Avindra Nath describes it in an article published in the journal
Neurology on post-acute-chronic COVID-19, "We discovered
the biological basis of diseases such as epilepsy and dystonia, to
name a few, that for centuries had been called 'hysteria'.
Psychological/psychiatric disorders in patients affected by postacute-
chronic COVID-19 are not only caused by the disease,
but are also caused by the pain and discomfort generated by
being in one way or another misunderstood, abandoned and
stigmatized by both their loved ones and their doctors. It is worth
mentioning that as described in previous paragraphs, although
many doctors have lacked the tools to deal with the problems of
"long-haulers", these should be accompanied with symptomatic
treatment, should be recognized and should receive the warmest
and most honest care possible until long-term results are available.
For the ignorance of science does not necessarily reflect the absence
of a morbid condition in these patients. To end the paragraph, I
will quote Avindra Nath again where she says the following "let us
remember that we must study and treat not the disease that affects
the patient, but the patient who is affected by the disease".
On the other hand, it is worth mentioning that many of the
members of these groups mentioned above, have developed a
flu process in their homes, which were never tested for SARSCoV-
2, because they were mostly afraid of contracting the
infection or in turn thought that the origin, it was the product
of a different virus than the one mentioned. After overcoming
the acute phase in their homes, the symptomatology persisted
for months, within them myalgias, arthralgias, thermal elevation,
asthenia, hyposmia, dyspepsia, etc. They dedicated themselves to
looking for information about the cause of the persistence of the
symptomatology on the internet, coming to meet these groups by chance, where they have come to ask if "the members believe
that they have been able to contract the infection by SARS-CoV-2
weeks or even months ago." This is complex, because they are
also not recognized, and less considering that they do not have
previous tests that have shown a SARS-CoV-2 infection. For many
doctors, the absence of a previous positive test excludes the
diagnosis of post-acute-chronic COVID-19. We must not forget
as doctors, that clinical and epidemiological data are relevant
in the diagnosis of most pathology and those complementary
examinations is just that, complementary.
According to a publication made by the World Health Organization
(WHO), a monitoring was carried out between August 27 and
September 2 on the most discussed topics around the long-term
effects of COVID-19 in social networks, where it was evidenced
that around 12,000 interactions corresponded to the long-term
effects on the lungs, 8,000 in the heart and 3,000 in the brain.
The top tweets referencing a review of several studies related
to the possible long-term effects at the heart of COVID-19 by
Scientific American, generated 104,000 interactions on social
media (of which 60% on Reddit, 35% on Facebook, 5% on Twitter).
An article published in the journal "Undark" on the prolonged
disease caused by COVID-19 in children generated around 2,000
interactions on social networks [18].
Among the signs and symptoms that have been evidenced in these
groups we have those described in the following table (Table 1).
| General Symptoms |
Neurological |
Sense organs |
Otolaryngological |
Cardiovascular |
Fever
-Chills with or without thermal rise
-Hypothermia |
- Headache
-Confusion
-Retrograde & anterograde amnesia
-Bruxism
-Tooth hypersensitivity
-Bladder dysfunction (retention or incontinence)
-Fasciculations
-Intercostal neuritis
-Parestesias
- Monoplegia
-Hemiplegia
-Erectile dysfunction
-Alteration of sweating pattern
-Orthostatic intolerance
-Hiccups
-Vertigo |
- Tinnitus
-Blurred vision
-Myodesopsias
-Anosmia
-Hyposmia
-Ageusia
-Dysgeusia
|
- Rhinorrhea
-Odynophagia
-Nasal obstruction
-Otalgia
-Vertigo |
-Inappropriate sinus tachycardia
-Sinus bradycardia
-Chest tightness
-Chest pain
-Dyspnea
-Hypertension
-Hypotension |
| Pulmonary |
Gastrointestinal |
Genitourinary |
Dermatological |
Rheumatologic |
- Cough
-Wheezing
-Roncus
-Shallow breathing
-Apneas
-Hypopneas
-Chest tightness
-Dyspnea
-Tachypnea
-Central and peripheral cyanosis
-Difficulty inspiring deeply or sighing |
-Nausea
-Vomiting
-Abdominal pain
-Meteorism
-Diarrhea
-Hiccups |
- Dysuria
-Oliguria
-Bladder tenesmus
-Urinary incontinence
-Urinary retention
-Dysmenorrhea
-Metrorrhagias
-Menometrorrhagia
-Amenorrheas |
-Chilblains
-Bruising
-Skin peeling |
Dryness ocular
-Xerostomia
-Enanthema
-Glossodynia
-Glossitis
-Arthralgias
-Myalgia
-Urticaria
-Loss of nail lunula
-Alopecia |
Table 1. Signs and symptoms that have been evidenced in these group
According to Lambert N, who collected and analyzed data obtained
from a survey published on the "Survivor Corps" Facebook
page about the symptoms of post-acute-chronic Covid-19, the
symptoms are more numerous compared to those described by
the CDC, since the problems not only cover the lungs and heart,
but also countless organs and tissues. It was evidenced that skin
and eye problems, in addition to muscle, joint and nerve pain, are
common in this group of patients. In addition, it was estimated
that approximately 26.5% of the symptoms are described as
painful by the participants. On the other hand, it is emphasized
that there is a lack of agreement between the available evidence,
regarding the symptoms actually presented by patients affected
by post-acute-chronic COVID-19 [19].
It is likely that even the symptoms described in your survey will
still be reduced compared to those that actually afflict this group
of patients. It is of the utmost importance to pay due attention
and carry out an adequate follow-up by a multidisciplinary group
to solve the needs of those affected. In addition, research on
these patients who in one way or another have been bypassed
both by severe cases and by the little evidence available on postacute-
chronic COVID-19 in the literature should be encouraged.
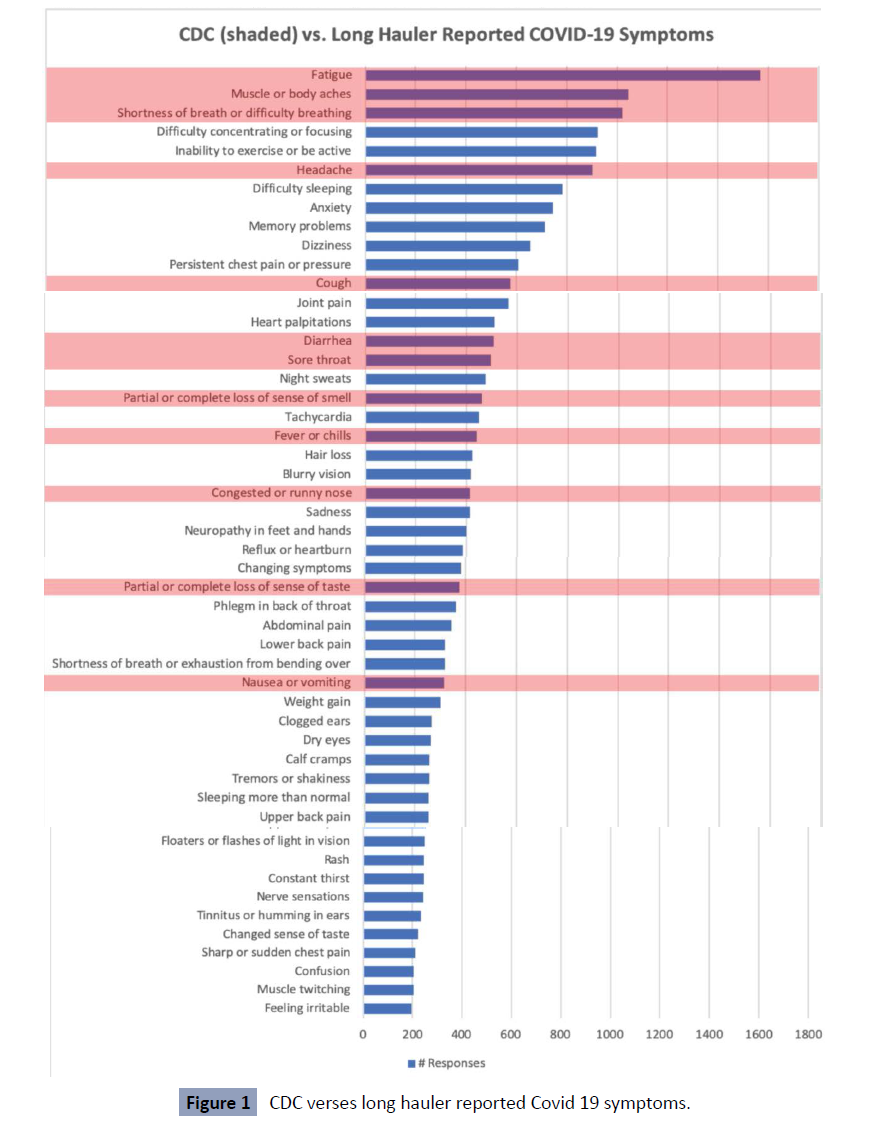
Below is the comparative table between the symptoms described
by the CDC and the symptoms collected through the survey of
long-haulers (Figure 1) [19].
Figure 1: CDC verses long hauler reported Covid 19 symptoms.
To an article published in the journal ERJ open research, 2113 patients were evaluated by a questionnaire, who were members
of two Facebook groups from both the Netherlands and Belgium
and a panel of people registered on the website of the Lung
Foundation Netherlands (a total of 12,200 members combined),
of which 112 were hospitalized patients and 2001 were nonhospitalized
patients.
During the acute phase they presented an average of 14
symptoms. 97% of patients had more than 5 symptoms at this
stage. Something striking was that the mean of symptoms by
subgroups was small but significant, being higher in patients who
were not hospitalized compared to those who were [20].
It was also evidenced in the follow-up, after an average period
of 79 +-17 days, an average of approximately 7 symptoms. This
shows a reduction in symptoms over time [20].
It was also possible to verify the presence of multiple symptoms
approximately 3 months after the onset of the disease. Fatigue
and dyspnea were the most prevalent symptoms both during the
acute phase and at follow-up [20].
0.7% of all patients were symptom-free at 79 days after
infection. And something striking and surprising is the fact that
approximately 2% of patients had an increase in symptoms
compared to the number of symptoms during the acute phase of
infection. It is worth mentioning that most were adult patients,
previously healthy, without evidence of pre-existing pathologies.
It is also evident that both severe and mild patients are affected
by what was called in the article a "post-COVID-19 syndrome"
[20].
This highlights several points. The first, that the "mild" can
present even more symptoms compared to moderate-severe
cases. Second, the symptoms diminish with the passage of time,
even in a small percentage, manages to resolve their symptoms
completely before 3 months, this corroborates the fact that
certain patients should be classified as post-acute and not as
chronic. Third and most striking of the study, a percentage of
those affected may present even greater symptoms in followup
than in the acute phase. Definitely, this last point should be
considered for future research.
Likewise, in a study published in. the journal Jama Network, 143
Italian patients were evaluated in an average of 60.3 days after
the onset of the first symptom. At the time of evaluation, only
12.6% were completely free of any symptoms, while 32% had 1
or 2 symptoms and 55% had 3 or more. In the study, none of
the patients had fever or any signs or symptoms of acute illness.
Deterioration in quality of life was evidenced in about 44% of
patients. In addition, it was observed that a large proportion of
patients presented fatigue (53.1%), dyspnea (43.4%), joint pain
(27.3%) and precordial pain (21.7%) [21].
According to a cohort study conducted internationally by Davis H
et al, in about 3,762 people from 56 countries through a survey,
where only 8.4% had been hospitalized, it was evident that the
ages most affected by persistent symptoms were between 40
and 49 years, with the female sex also being the most affected. A
prevalence of 205 symptoms was estimated in 10 organ systems,
with 66 symptoms tracked over 6 months. The most frequently
observed symptoms after 6 months were fatigue, post-exertional discomfort, and cognitive dysfunction. Something striking is that
of those who presented symptoms for more than 6 months, they
experienced an average of 13.8 symptoms when they reached
the seventh month [22].
In an article published by Nath A, symptoms such as mental
confusion, sleep disturbances, exercise intolerance, autonomic
symptoms, lymphadenopathies, even fever, are highlighted as
the main ones [23]. The latter, like the autonomic symptoms, are
currently poorly described in the literature. It is worth mentioning
that the persistence of fever is relevant to the extent that it
could suggest the persistence of SARS-CoV 2 within the body or
correspond to an overactive response of the immune system, as
we will see later. In addition, this study, by mentioning fever as
one of the persistent symptoms, contrasts in one way or another
with what was suggested in the study published in the journal
Jama Network by Carfì A et al.
Now, in a publication made in the journal Nature, a disturbing but
revealing title stands out: "The lasting misery of coronavirus longhaulers".
This title translated into Spanish "the lasting misery of
long-distance carriers of the coronavirus", highlights the ordeal
that is lived day by day with a condition still unknown and little
recognized. It is mentioned that, in reality, it is a multisystem
disease because ACE2 receptors are found throughout the body
and are also the main target of the virus. It should be noted that
the infection can generate significant immune damage generating
a certain degree of persistent immunosuppression probably given
by a reduction in interferon’s, or quite the opposite, generating
that parts of the immune system become overactive and lead to
inflammation harmful to the body, both things demonstrated
already in the SARS-CoV-1 epidemic in 2003. In a study conducted
at the Peking University People's Hospital in Beijing on SARSCov-
1, in which 71 people who had been hospitalized after
acquiring the virus were tracked, it was evidenced that after 15
years 4.6% of people still had visible lesions in the lungs and that
38% had a reduced diffusion capacity. On the other hand, a study
of patients in China showed that 25% had abnormal lung function
after 3 months, and that 16% were still fatigued [24].
Several posts made on the Medscape website regarding postacute-
chronic COVID-19. The website usually identifies main
search terms, with which, it is dedicated to investigating what
originated the popularity of them and makes info graphic about
it. Something striking is that, during the last weeks, the terms
associated with the long-term consequences of COVID-19 have
prevailed.
According to Ellis R, a study was conducted at the British hospital
North Bristol NHS Trust, where it was shown that 81 out of
110 patients still experienced dyspnea, asthenia, myalgias and
sleep disorders months after discharge. Something important
to note is that in many of these patients it was not possible to
demonstrate alterations in tests of image or lung functionality,
but that, nevertheless, their quality of life was deteriorated to
such an extent that a subgroup of them could not perform tasks
as simple as bathing, dressing or even resuming their working
life. According to the Centers for Disease Control and Prevention
(CDC), people who continue with fever, chills, cough, myalgia,
odynophagia, nausea, vomiting, among other symptoms, may eventually continue with the viral process [25]. It is worth
mentioning that there are patients who after 7 or 8 months of
discharge, persist with symptoms such as chills, cough and fever.
1. In a comparison of the symptomatology between the acute
phase and the "post-covid syndrome" as it has been catalogued
by its author, it was evidenced that 66% did not present any
improvement in the symptomatology. Interestingly, 34% of
the participants have even stated that their symptoms have
worsened. On the other hand, it has been evidenced that 66%
of the respondents have remained ill after 6 months since the
onset of symptoms. This is important in the sense that "covid
long-haulers" could be classified within post-viral syndromes. In
any case, caution is suggested, because as we will see, there is a
possibility that it is not a post-viral disorder but rather, that its
symptomatology is due to a persistent viral infection. It is worth
mentioning that in this survey there is a higher percentage of
participants who have presented a worsening of symptoms, as
demonstrated by the survey described in the article published by
the journal ERJ open research, which was described above.
2. According to a video published on the website of Dysautonomia
International, dysfunction of the autonomic nervous system
is caused by structural damage to the nerves, by their loss, by
a malfunction of the same without structural damage or by a
combination of them. This alteration could be:
• less than 1 month
• Transient: 1 to 6 months after infection
• Chronic: 6 months or more after infection
Among the most frequent infectious causes that trigger
alterations of the autonomic nervous system we have:
HIV, rabies virus, Human T-cell lymphotropic virus, West Nile
virus, enter virus 71, herpes virus, tick-borne viral encephalitis,
bacteria such as borrelia burdorgferi, mycobacterium leprae,
Corynebacterium diphteriae, clostridium botulinum, clostridium
tetani, parasites such as trypanosome cruzy and prions. It is
currently believed that coronaviruses should be included within
the viral etiology causing dysautonomia5.
However, it is necessary and fundamental to highlight certain
pathologies that are closely related to the symptomatology of
post-acute-chronic Covid-19. Because these syndromes are little
known even to health personnel. In addition, the problem is that
all this leads to certain patients being diagnosed with an anxiety
disorder.
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
This is perhaps the most diagnosed chronic or post-viral viral
disorder in the world. So far, most of the literature seems
to support the fact that a large part of the patients who have
studied and who will undergo SARS-CoV-2 infection, will develop
this disorder that, in the same way as the rest of the disorders
exposed in this article, can also generate autonomic alterations.
Well, as we have shown, fatigue in most cases is the main
manifestation.
It should be remembered that in the SARS-CoV-1 epidemic of
2003, a study was evidenced where it was found that 22 health workers who had been infected by this virus, had a post-viral
syndrome, which was called "chronic post-SARS syndrome" in
which chronic fatigue was reported within the main symptoms as
a cardinal symptom, in addition to musculoskeletal pain, sleep
disturbances characterized by non-restorative sleep with apneas
and hypopneas, among others similar to fibromyalgia and ME/
CFS up to three years after the disease, without any returning to
work within the first year [26].
On the other hand, according to E. Tucker M, the persistent
symptoms caused by SARS-CoV-2 overlap with chronic fatigue
syndrome, similar to what we have already described with SARSCoV-
1 of 2003, which is why he mentions that the association
between the two is being sought, especially since it is presumed
that the origin of this disorder, it is also of viral etiology in a large
number of patients.
Among the diagnostic criteria for ME/CFS, are:
• Substantial and deep fatigue for at least 6 months
• Post-exertional discomfort
• Non-restorative sleep and one or both of orthostatic intolerance
and/or cognitive impairment.
There is no presence of other pathologies that may occur with
chronic fatigue Vale clarify, that not all those patients with
persistent symptoms will develop chronic fatigue. One way
perhaps to distinguish them early is to ask if there is a dramatic
exacerbation of post-exercise symptoms, such as fatigue, pain,
and cognitive decline a day or two after exercise rather than
immediately afterward. The objective measures supporting
the diagnosis of ME/CFS are a low natural killer cell count and
autonomic dysfunction assessed by the tilting table test.
Fibromyalgia is a disease characterized by generalized, chronic
pain, accompanied or not by joint stiffness, sleep disorders,
cognitive dysfunction given by difficulty in concentration,
memory problems and depression that affects approximately 2%
to 4% of the general population, however of utmost importance
since it represents a high cost for the health system given the
high number of consultations per year (approx. 10) and the lack
of productivity of diagnosed patients [27].
The pathophysiology of fibromyalgia is given by a disorder in the
regularization of pain and central sensitization; among which is an
excess of excitatory neurotransmitters and low levels of inhibitory
neurotransmitters in the descending ant nociceptive pathways
of the spinal cord and alteration of endogenous opioids. Among
the risk factors identified are genetic, environmental, hormonal,
neural and immunological factors28.
Due to the high number of under diagnostics, in 2010 the
American College of Rheumatology updated the diagnostic
criteria of the disease; among which are:
Pain index (WPI) greater than or equal to 7 and severity symptom
scale (ESS) greater than or equal to 5 or WPI between 3-6 and ESS
greater than or equal to 9.
1. Presence of: Fatigue, non-restorative sleep, cognitive
symptoms
2. Symptoms have been present for at least 3 months
3. Other diagnoses that explain pain have been excluded.
A relationship between fibromyalgia and some viral infections
such as Epstein-Barr virus, parvovirus, among others, has been
found, which is why in the current context in which the world
is going through a pandemic due to the SARS Cov 2 virus, the
relationship between it and fibromyalgia is not ruled out [28].
Following a review of the currently available literature, it was
observed that
1) Fibromyalgia patients are considered as a vulnerable
population in this pandemic.
2) It is common knowledge the existence of countless stressors
(physical, mental, emotional and financial) to which the human
being is being subjected during this pandemic, it has been seen
that these stressors generate a direct and negative impact on the
central awareness that is the causal mechanism of FM [29].
3) Patients with central sensitization have inadequate control in
the limbic system intensifying the symptoms of depression and
anxiety; which in the context of the pandemic could increase
suicidal ideation
4) Half of patients with FM establish the worsening of their
symptoms after confinement [30].
However, the information reviewed does not establish
fibromyalgia as a consequence of INFECTION by SARS Cov 2 virus,
however, it has been shown that there are several epidemiological
and socioeconomic factors such as insomnia, uncertainty,
decreased physical activity which we go through during this
pandemic that are also involved in the pathophysiology of FM.
A worsening of symptoms was demonstrated in patients with
a previous diagnosis of FM secondary to the large number of
current stressors. Further research is needed in this relationship
in order to establish or not a direct causal link [31, 32].
Central sensitization syndrome
On the other hand, another hypothesis that is handled regarding
the persistence of covid-19 symptoms is the Central Sensitization
Syndrome. This syndrome corresponds to a set of frequently
painful disorders that contribute to the increased risk of opioid
abuse and that tends to decrease the quality of life of patients
[33].
Central sensitization syndrome is understood as an increased
response due to stimulation mediated by an amplification of
signaling in the central nervous system [34].
The International Association for the Study of Pain defined central
sensitization syndrome as an increase in the responsiveness of
nociceptive neurons of the central nervous system to normal or
subnormal afferent entry [35].
The central desensitization syndrome currently includes
diagnoses such as Fibromyalgia, Chronic Fatigue Syndrome,
Migraine or Tension Headache, Restless Legs Syndrome, Multiple
Chemical Syndrome33.
This syndrome is characterized by a generalized sensory sensitivity that contributes to hypersensitivity to pain and polysomatization
[36].
This process is apparently due to synaptic neuroplasticity, which
is characterized by the alteration of neurons depending on
factors, both environmental and genetic, and which has been of
great interest in chronic pain syndromes [37].
This process of synaptic neuroplasticity occurs in neurons within
the limbic region of the brain37.
This mechanism begins with peripheral sensitization, and
progresses to the early phase and then moves to the late phase
leading to allodynia (pain with mild touch) and diffuse hyperalgesia
(generalized increase in sensitivity to painful stimuli) [37].
Sensitization syndrome is divided into acute and late phase. In
the acute phase, the activation potential of neurons in the dorsal
horn of the spinal cord is reduced by increased transmission of
glutamate by N-methyl-D-aspartate (NMDA) and A-amino-3-
hydroxy-5-methyl-4-isoxazol-propionic receptors. This increase
in the amino acid glutamate and substance P lowers the activation
threshold and intensifies the opening of several channels, leading
to increased neuronal excitability. Another characteristic is that
this increase in glutamate causes the death of inhibitory neurons,
thus reducing the modulation of pain signals. These inhibitory
neurons are replaced by more afferent excitatory neurons
allowing pain signals to increase.
In the late phase there is an alteration in gene expression within
the neurons of the dorsal horn, in this way it becomes more
difficult to recover from hyperalgesia. This causes changes in the
dorsal root ganglia that give these neurons the ability to induce
pain without the entry of nociceptors. This continuous afferent
outflow without the relevant inhibition results in a greater
transmission of pain to the brain, specifically in the insula,
which is the area responsible for the interpretation of sensory
information [37].
Due to the pandemic caused by COVID 19 there has been a
decrease in the physical and emotional condition of people,
however, this picture may be more marked in those who suffer
from central sensitization syndrome.
Although COVID 19 can be a very stressful circumstance for all
patients, those with central sensitization syndromes may be more
affected and have an increased risk of developing symptoms of
psychological distress36.
Postural Tachycardia Syndrome (POTS)
Regard to Orthostatic Postural Tachycardia Syndrome (POTS), a
similar picture had already been described in the Xlll century. In
1871 during the American Civil War, young soldiers developed
abnormal postural tachycardia after an intestinal infection,
combat wound, or overexertion. In its time, it was referred to as
"irritable heart" or "soldier's heart" [5].
Something interesting that Cotelo J reports in his publication is
a textual quote from what dr. Ramos mentioned where he says
the following "dyspnea during hospitalization was associated
with subsequent fatigue, with polypnea post activity and with
increased resting heart rate. Also a history of asthma during hospitalization was associated with the subsequent squeal of
polypnea post activity. In addition, having a heart rate greater
than 90 beats per minute during hospitalization was associated
with an increase in this parameter at rest during convalescence"
[32].
With the latter, it may be evident that both the history of
patients, such as possible dyspnea, as well as alterations in heart
rate during the acute phase, could be crucified if no action is
taken. That probably shows us lights, that orthostatic postural
tachycardia syndrome can be triggered even from the acute
phase of the disease. If this is the case, it could eventually be
diagnosed early, before the stipulated 6 months, in order to
intervene in a timely manner with the intention of improving
the picture and therefore the quality of life of the patients. It is
worth mentioning that the especially temporary criteria for the
diagnosis of this disease must be revised again.
On the other hand, Syrek R in a publication on COVID-19
syndromes says the following "Heart-related symptoms such
as residual palpitations and persistent tachycardia have been
reported without any residual inflammation"16.
This again strengthens the fact that "unexplained" cardiac
symptoms already appear in early stages of the disease.
Going into orthostatic postural tachycardia syndrome (POTS),
it is believed to be one of the possible causes of dysautonomia
in patients who have developed COVID-19. It is characterized
by being a little-known disorder, which generates orthostatic
intolerance. It is estimated that 50% of people who have
developed POTS previously had a specific viral exposure5.
The estimated prevalence in 2019 was 1-100/1-1000 people in
the United States 5.
It is believed that within the possible mechanisms involved
we have: Autoimmune/post-infectious, mast cell activation, a
genetic component, deconditioning5.
Other triggering causes: bacterial infections, bruises, pregnancy,
traffic accidents 5.
is defined as:
1. heart rate greater than or equal to 30 bpm (40 bpm 12 to 18
years) when standing still after being in supine position for the
first 10 minutes (for most patients it exceeds 120 bpm).
2. Absence of orthostatic hypotension defined as a fall greater
than or equal to 20/10 mmhg within 3 minutes in standing
position.
3. Symptoms of orthostatic intolerance greater than or equal to
6 months.
4. Symptoms that are exacerbated by standing and improved at
bedtime.
5. Absence of another cause of orthostatic symptoms or
tachycardia5.
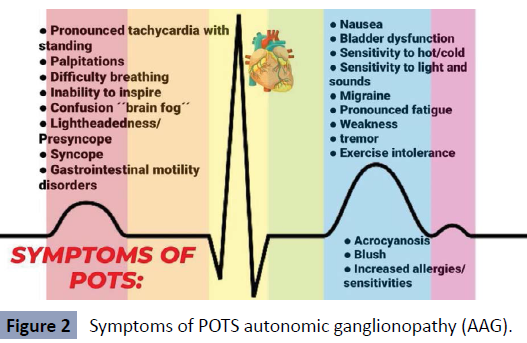
Symptoms of POTS
Pronounced tachycardia with standing up, palpitations, difficulty breathing, inability to breathe deeply, confusion "brain fog",
light-headedness/presyncope, syncope, gastrointestinal motility
disorders, nausea, bladder dysfunction, sensitivity to cold/heat,
sensitivity to light and sounds, migraine, pronounced fatigue,
weakness, tremor, exercise intolerance, acrocyanosis, flushing,
increased allergies/sensitivity to food, medicines and/or
environment5.
Something that patients with POTS suffer from is sub occipital
and/or paracervical pain, probably caused by low blood flow to
the muscles of the upper back and neck5. Interestingly, symptoms
manifested by a large proportion of patients with post-acutechronic
COVID-19.
It is believed that it can become as disabling as Congestive Heart
Failure (CHF) or Chronic Obstructive Pulmonary Disease (COPD)
5 (Figure 2).
Figure 2: Symptoms of POTS autonomic ganglionopathy (AAG).
It is an autoimmune disease that affects the autonomic ganglia,
in half of the cases it is caused by antibodies against the nicotinic
acetylcholine receptors of the ganglia that produce their
internalization damaged synaptic transmission. The vast majority
are preceded by a respiratory infection.
The symptoms described have been classified as autonomic or
extra autonomic: within the autonomic ones are: orthostatic
hypotension, dry skin, anhidrosis, heat intolerance, pupillary
dysfunction, diarrhea or constipation, dysuria, urinary retention,
sexual dysfunction. On the other hand, within the extraautonomic
symptoms are sensory alterations (paraesthesia’s
and dysesthesias), central nervous system involvement,
endocrinological disorders (amenorrhea, SIADH, hyponatremia,
adrenal insufficiency), autoimmune diseases (Sjogren, systemic
lupus erythematous, rheumatoid arthritis, systemic sclerosis,
polymyalgia rheumatic, primary biliary cirrhosis, Sill's disease,
Hashimoto's thyroiditis, Grave's disease and fibromyalgia), and
tumors (ovarian tumor, small cell lung cancer, gastric cancer)
For an adequate diagnosis of this disease, several tests are
required, including positive serology for gAChR antibodies and
a thorough exploration of autonomic symptoms including tilting
table test, measurement of the coefficient of variation of R-R
interval, noradrenaline infusion test, levels of catecholamine’s in
blood, sweat test, pupillary response, Valsalva manoeuvre, study
of gastrointestinal motility, urodynamics and customary.
Small fibre neuropathy
The following section is considered fundamental, because a
large proportion of patients suffer from symptoms that could be
correlated with a viral or post-viral dysautonomia, understood
as an over activity or alteration in the sympathetic and
parasympathetic components of the autonomic nervous system,
which can manifest itself with sinus arrhythmias, profuse sweating,
cold, constipation, bronchospasm, chest tightness, alterations
in blood pressure, dizziness, presyncope, among others. It is
worth mentioning that this symptomatology can simulate panic
attacks and in turn, psychological disorders could worsen such
dysfunction. This may be due to several factors, perhaps in part
due to a hypothalamic alteration mediated by cytokines, due
to a small fiber neuropathy, already demonstrated with other
viruses such as influenza, viral persistence or viral fragments
in leukocytes, such as monocytes, which are easily distributed
throughout the body, alteration of the renin angiotensin
aldosterone system, by alteration in the hypothalamic-pituitaryadrenal
axis, by a microangiopathy, or by direct affection of
nerves such as the vagus nerve or glossopharyngeal In a letter
to the editor published by The Canadian Journal Of Neurological
Sciences, regarding the morbidity of patients recovered from
SARS-CoV-1. It was evidenced that, although younger patients
tend to survive, they may present with post-infectious disorders,
including alterations of the nervous system. In a study conducted
in 14 patients who overcame SARS-CoV-1 infection, it was
evidenced that 100% of the participants presented fatigue and
discomfort and of this group of patients 50% of them presented
dysautonomias. It is believed that orthostatic hemodynamic
alterations with subclinical behavior could contribute to fatigue
and dizziness39.
Novak P mentions that several autoimmune post-infectious
complications have been reported, which can affect both the
brain and large and small nerve fibers. In it, the case of a patient
who developed orthostatic hypo perfusion syndrome (OCHOS)
and painful neuropathy of small fibers (SFN) is reported.
Both OCHOS and SFN were confirmed. The first by tilt test with
Trans cranial Doppler monitoring and the second confirmed by
skin biopsy.
It is striking that these patients have a favourable response to
immunotherapy. Well, here a new question arises: Could an
early intervention through immunotherapy in those patients
who manifest alteration of the autonomous component avoid its
chronicity?
It is something that we must consider for the future. Another
thing to highlight from what Novak P described is the fact that
these disorders are beginning to be described more and more
frequently associated with SARS-CoV-2.
A question that must be answered sooner or later is whether
fibromyalgia, chronic fatigue syndrome, as well as orthostatic
postural tachycardia syndrome, can be pigeonholed with the
same name, perhaps as the same disease with slightly different
forms of presentation. Well, all three share similar aspects such
as viral origin, small fiber neuropathy in many cases, autonomic
dysfunction and therefore symptoms such as fatigue, muscle pain, cognitive alterations, alterations in cardiovascular function,
etc. In some countries, a "central sensitization syndrome" is
beginning to be diagnosed, which includes chronic fatigue
syndrome and fibromyalgia, but not orthostatic postural
tachycardia syndrome. It would be interesting to see to what
extent this last diagnosis can be included in it and thus begin to
decipher the pathophysiology behind these disorders to offer an
adequate treatment.
Deconditioning We believe that we cannot fail to address a crucial issue, of vital
importance within those patients who are undergoing postacute-
chronic COVID-19. This is post-viral deconditioning.
Deconditioning is a serious alteration of the organism, which can
occur to anyone, including athletes in just a few days 5.
Among the symptoms we have
Increased heart rate while lying down or exercising, decreased
blood pressure when upright, decreased ability to exercise,
weakness, loss of appetite, nausea, constipation, loss of bladder
control, electrolyte disturbance, tendency to develop blood clots,
impaired response to insulin, elevated blood glucose, impaired
balance and coordination, confusion, disorientation, anxiety,
depression.
Both deconditioning and dysautonomias can coexist and generate
a vicious circle that is detrimental to the health and therefore
the quality of life of the people affected. It is worth mentioning
that many people in the world live with dysautonomias or postviral
deconditioning. Many of them will fully recover, some will
improve over time, and others will not recover.
We believe that viral or post-viral deconditioning is part of the
problem of patients suffering from post-acute-chronic COVID-19.
However, we believe that it is not the causal axis of his condition.
Discussion
So far, both the persistence of politicization, new politicizations,
relapses or the reappearance of symptoms and in many cases
the persistence of it with fluctuating intervals of intensity, and
variables over time, could suggest the presence of a persistent -
chronic viral infection. This is further strengthened in the sense
that a large part of those who have these characteristics are
patients who have been with mild COVID-19 in which it has been
demonstrated, for the most part, low antibody titers and this
could justify a real difficulty in eliminating the virus effectively.
It is expected if it is the case, that the virus with each replication
generates failures that make it disappear from the body and
therefore the symptomatology in an indeterminate time.
On the other hand, there is a possibility based on what has been
evidenced with other viruses,that this symptomatology is due
to a post-viral syndrome such as fibromyalgia, chronic fatigue
syndrome, orthostatic postural tachycardia syndrome (POTS) and
autoimmune autonomic ganglionopathy. Orthostatic postural
tachycardia syndrome (POTS), the most likely cause due to the
characteristics of the symptomatology. In any case, it is necessary
to analyze to what extent post-viral syndromes are related. Well, perhaps, they are part of the same disease with slightly different
forms of presentation as previously mentioned. In addition, it is
necessary to analyse what role deficiency states play in the "long
covid", such as deficiencies of vitamins such as B3, B12, vitamin
D, amino acids such as acylcarnitine or other disorders such as
mastocyte activation syndrome. On the other hand, we do not
interfere much in the issue of small fiber neuropathy, however,
as we have evidenced, it is believed that it can collaborate with
the development of chronic fatigue syndrome, fibromyalgia,
orthostatic postural tachycardia syndrome and autoimmune
autonomic ganglionopathy. This neuropathy is characterized by
the injury of poorly myelinated Aδ peripheral afferent fibers and
non-myelinated C fibers.
Also, it is necessary to carry out an exhaustive investigation on
what relationship could exist between the infections passed by
other viruses such as Epstein Barr, cytomegalovirus, herpes type
1 and type 2 with the subsequent infection by Sars-CoV-2 and the
development of persistent symptomatology.
Addition, it is necessary to investigate to what extent they are
post-viral syndromes and not chronic viral syndromes.
It is necessary to analyze to what extent the persistence of SARSCoV-
2 in the body is the cause of chronic symptoms. Well, not
necessarily the existence of it or its fragments can be the cause
of this disorder.
The last possibility that we consider is that SARS-CoV-2, having
an important neuroinvasive capacity, could have persisted
due to unclear mechanisms in the nerves, perhaps due to the
formation of immunocomplexes, generating a process of both
central and peripheral neuroinflammation, either at the level
of the hypothalamus or perhaps also due to nerve injury such
as the vagus, the phrenic and the glossopharyngeal, generating
an autoimmune and inflammatory response in these places,
thus manifesting with symptoms associated with the autonomic
component of the nervous system, which could trigger symptoms
similar to postural orthostatic tachycardia syndrome, chronic
fatigue syndrome, fibromyalgia, among others. These disorders,
whether of viral or post-viral origin, generate similar symptoms
and may even overlap with various psychiatric disorders, such
as generalized anxiety disorder, post-traumatic stress disorder,
or panic attacks, etc. It is important to clarify that psychiatric
disorders worsen autonomic symptoms and by coexisting both
together with viral persistence, a state lacking nutrients, a state
of deconditioning of the individual, could be the cause of the
symptomatology, which is confusing and difficult to manage by health personnel. In any case, blood markers in each of the phases
of the disease are being investigated, as well as certain important
imaging tests for diagnosis such as PET-SCAN or functional
magnetic resonance imaging of the brain or heart. In any case,
more studies are required to later find the pathophysiological
origin and the development of an appropriate treatment.
is not yet clear what percentage of patients and in what time
they will recover, in addition, an approximate number of patients
suffering from post-acute-chronic COVID-19 is not yet known,
given that they have been diagnosed mostly incorrectly, have not
had a diagnosis so far by their doctors or because they have not
attended them. It is imperative to recognize and assign an ICD-10
to this condition and it is urgently required in the same way, to
create "post-covid" clinics or centers, as they have done in some
countries.
Conclusions
Both persistent viral infections and post-viral syndromes have
been little studied so far. It is perhaps time to interfere in depth
in the investigation of chronic infections, their impact on the
body, as well as entities that generate dysautonomias and that
are usually associated with chronic or post-viral viral pathology,
especially chronic fatigue syndrome, fibromyalgia, autoimmune
autonomic ganglionopathy and orthostatic postural tachycardia
syndrome. The first two are already included in a disorder
known as central sensitization syndrome. Well, it would not be
uncommon for POTS to end up being part of the latter. More
research is needed on blood markers, the presence of viruses
in tissues and possible risk factors to prevent chronicity of the
disease. Patients with sub-acute-chronic COVID need answers,
because the impact on their quality of life, in the workplace,
social, psychological has been very great and without a doubt, of
not taking action, of not taking corrective prevention measures, of
not facilitating vaccination freely worldwide, health systems will
be saturated and / or collapsed by a new disease. It is imperative
not only to focus on prevention, but also on the treatment of
it. Well, we do not know if vaccinated patients are protected
against the development of chronic covid.. It is essential to look
for a treatment that is equally widespread as the vaccine and at
low costs, since the latter is important since most of those who
suffer from this chronic disease are people with limited economic
resources. It is not possible to dismiss as we have seen, the impact
on the nutritional deficiency state generated by the disease nor
the deconditioning, which definitely generate repercussions and
a worsening of the picture of people who persist with symptoms.
REFERENCES
- Baig AM (2021) Syndrome de COVID cronico Necesidad de una terminologia medica adecuada para los transportistas de largo recorrido de COVID y COVID. J Med Virol 93:2555-2556.
Google Scholar, Crossref
- Del Rio C, Collins LF, Malani P (2020) Consecuencias para la salud a largo plazo del COVID-19. JAMA 324:1723-1724.
Indexed at, Google Scholar, Crossref
- Greenhalgh T, Knight M, A Court C, Buxton M, Husain L (2020) Management of post-acute covid-19 in primary care. BMJ 370:3026.
Indexed at, Google Scholar, Crossref
- DisautonomIa International (2020) Seminarian web: Síntomas de disautonomía en large distance COVID 19.
Google Scholar
- Liu W, Tang F, Fontanet A, Zhan L, Zhao Q-M et al. (2004) Long-term SARS coronavirus excretion from patient cohort, China. Emerg Infect Dis 10:1841-1843.
Indexed at, Google Scholar, Crossref
- Wu Y, Guo C, Tang L, Hong Z, Zhou J et al. (2020) Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol 5:434-435.
Indexed at, Google Scholar, Crossref
- Sun J, Xiao J, Sun R, Tang X, Liang C et al. (2020) Prolonged persistence of SARS-CoV-2 RNA in body fluids. Emerg Infect Dis 26:1834-1835.
Indexed at, Google Scholar, Crossref
- Jennifer S Read (2020) Healthvermont.gov. COVID-19 Patients with Persistent or Recurrent Positive PCR TesT.
Google Scholar
- Trending clinical topic Chronic COVID Medscape 2020.
Google Scholar
- Yang JR, Deng DT, Wu N, Yang B, Li H J et al. (2020) Persistent viral RNA positivity during the recovery period of a patient with SARS-CoV-2 infection. J Med Virol 92:1681-1683.
Indexed at, Google Scholar, Crossref
- Gousseff M, Penot P, Gallay L, Batisse D, Benech N et al. (2020) Clinical recurrences of COVID-19 symptoms after recovery: Viral relapse, reinfection or inflammatory rebound. J Infect 81:816-846.
Indexed at, Google Scholar, Crossref
- Xia J (2020) does immune privilege result in recovered patients testing positive for COVID-19 again? Biosci Trends 14:209-211.
Indexed at, Google Scholar, Crossref
- Ryan Syreck (2020) Sindromes de COVID-19. Medscape.
Google Scholar
- Alfonso Barquilla García, Francisco Javier Gamir Ruiz (2021) Protocol de actuation en pacientes con COVID-19 asistidos en atencion primaria.
Google Scholar
- Los effects a largo plazo de la COVID-19 Who.int (2022).
- Lambert N J (2020) Survivor Corps. COVID-19 “Long Hauler” Symptoms Survey Report. Indiana University School of Medicine.
Indexed at, Google Scholar
- Goertz YMJ, Van Herck M, Delbressine JM, Vaes AW, Meys R et al. (2020) Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Res 6:00542-2020.
Indexed at, Google Scholar, Crossref
- Carfì A, Bernabei R, Landi F (2020) Gemelli against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA 324:603-605.
Google Scholar
- Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ et al. (2020) Characterizing Long COVID in an international cohort: 7 months of symptoms and their impact. 24:20248802.
Indexed at, Google Scholar, Crossref
- Nath A (2020) Long-haul COVID. Neurology 95:559-560.
Indexed at, Crossref
- Marshall M (2020) the lasting misery of coronavirus long-haulers. Nature 58:339-341.
Indexed at, Google Scholar, Crossref
- Ellis R (2020) Some COVID-19 symptoms last for months, study finds Medscape.
Google Scholar
- Moldofsky H, Patcai J (2011) chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome a case-controlled study. BMC Neurol 11:37.
Google Scholar, Crossref
- Bair MJ, Krebs EE (2020) Fibromyalgia Ann Intern Med 172:ITC33-48.
Google Scholar, Crossref
- Garcia Rodriguez DF, Abud Mendoza C (2020) Physiopathology of fibromyalgia. Rheumatol Clin 16:191-194.
Indexed at, Google Scholar, Crossref
- Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS etal. (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 62:600-610.
Indexed at, Google Scholar, Crossref
- Mohabbat AB, Mohabbat NML, Wight EC (2020) Fibromyalgia and chronic fatigue syndrome in the age of COVID-19. Mayo Clin Proc Innov Qual Outcomes 4:764-766.
Indexed at, Google Scholar, Crossref
- Sars-Cov-2 Manifestations Persistence’s De La Covid-19 Guía De Practice Clinical Societat Catalana de Medicina Familiar I Communitarian Semfyc.es.
Google Scholar
- Nuevo kit para (2020) COVID-19 persistent guia para el medico y amparo del paciente Medscape.
Google Scholar
- Miller JS, Rodriguez-Saona L, Hackshaw KV (2020) Metabolomics in central sensitivity syndromes. Metabolites 10:164.
Indexed at, Google Scholar, Crossref
- Central nervous system sensitization MeSH NCBI.
Indexed at
- Loeser JD, Treede RD (2008) the Kyoto protocol of IASP Basic Pain Terminology. Pain 137:473-477.
Indexed at, Google Scholar, Crossref
- Serrano-Ibanez ER, Esteve R, Ramirez-Maestre C, Ruiz-Parraga GT, Lopez-Martínez AE (2021) chronic pain in the time of COVID-19: Stress aftermath and central sensitization. Br J Health Psychol 2021 26:544-552.
Indexed at, Google Scholar, Crossref
- Bettini L, Moore K Central sensitization in functional chronic pain syndromes: Overview and clinical application. Pain Manag Nurs 17:333-338.
Indexed at, Google Scholar, Crossref
- Nakane S, Mukaino A, Higuchi O, Watari M, Maeda Y et al. (2018) Autoimmune autonomic ganglionopathy an update on diagnosis and treatment. Expert Rev Neurother 18:953-965.
Indexed at, Google Scholar, Crossref
- Loa YL, Leonga HN, Hsua LY, Tana TT, Kurupa A et al. (2005) Autonomic dysfunction in recovered severe acute respiratory syndrome patients. Can J Neurol Sci 32:264-264.
Indexed at, Google Scholar
- Novak P (2020) Post COVID-19 syndrome associated with orthostatic cerebral hypo perfusion syndrome, small fibre neuropathy and benefit of immunotherapy: a case report. E Neurological Sci 21:100276.
Indexed at, Google Scholar, Crossref
Citation: Citation: Celi E, Espinoza C, Paredes A, Montenegro M, Velin D (2022) Post-Acute Covid-19 Disease-Chronic. Health Sci J. Vol. 16 No. S7: 951.