Key words
Cryptococcal meningitis, HIV, symptoms, treatment.
Introduction
Cryptococcal meningitis is an infection of the membranes covering the spinal cord or brain, by a yeast, Cryptococcus neoformans. Soil contaminated with pigeon extracts and chicken droppings provide the environmental source of the yeast. Once Cryptococcus reaches lungs through inhalation, the immune system can heal the body without medical intervention, the disease can stay localized in the lungs, or it can be carried by blood and spread throughout the body. In healthy people with normal functioning immune systems, infection is usually self limiting, and the infected person notices no symptoms. If the body does not heal itself, the fungus begins to grow in the lungs and can spread to other parts of the body, particularly the brain and central nervous system causing cryptococcal meningitis [1].
With the arrival of the HIV and AIDS pandemic, the disease has emerged as a leading cause of morbidity and mortality, and a life-threatening opportunistic infection, especially if treatment is not initiated promptly [2]. In Africa, it is associated with higher rates of complications and death, than in the developed countries. Because the symptoms are frequently non-specific, and the symptoms of classic meningitis, such as stiff neck and aversion to light do not occur in many patients with cryptococcal meningitis, awareness of meningitis is often missed by the person infected and consequently there is often a delay of several weeks or months before medical attention is sought [2,3]. Whether geographic differences in rates of cryptococcal meningitis result from variations in socio-economic status, environmental distribution of Cryptococcus neoformans or the distribution of HIV infection is unclear [4]. It is estimated that for every million people living with AIDS, 50,000-100,000 will contract cryptococcal meningitis [5]. In Kenya, up to 40% of people with AIDS develop cryptococcal meningitis [6]. The mortality rate of patients with cryptococcal meningitis having AIDS is 10-25%, most deaths occurring within the first 2 weeks of onset of therapy [7]. In patients with AIDS, cryptococcal meningitis is usually incurable, and individuals who survive the initial infection are given lifelong antifungal therapy to reduce the likelihood of relapse [8,9]. Even when the infection has been treated, individuals may be left with a variety of complications such as, weakness, headache, paralysis, hearing and visual loss [10].
Because of delay in seeking medical attention, during this period there is reduction in quality of life, not only of the person infected, but also the families and communities affected at large. As cryptococcal meningitis occurs at a relatively advanced stage of AIDS, the affected people have reduced productivity and time lost from work may be significant. Therapeutic management improves the condition of people infected with cryptococcal meningitis. However, once the infection is established, patients hardly survive even after proper regimens of specific antifungals [5]. Its fatal outcome highlights the need for a uniform, rational and sustainable approach and concerted action to prevent infection, but all these strategies require studies on the epidemiological aspects of the disease [2]. Hence, early detection is critical. Despite the seriousness of the disease in regions of high HIV and malaria prevalence such as Nyanza Province in Kenya [11], there is no study done on cryptococcal meningitis in this region. Consequently, the relative importance of this infection as a cause of morbidity and mortality is uncertain; therefore the role of prevention and treatment cannot be defined or prioritized. The purpose of this study was to identify factors associated with cryptococcal meningitis among HIV patients attending major hospitals in Kisumu. This study highlights the need for concerted actions to create awareness for the prevention and treatment of the disease.
Methods
Study Area: Kisumu is located in Winam Division of Kisumu District, Nyanza Province, Western Kenya. The District has a total of 49 health care facilities, the majority of which are situated in Kisumu town (Kisumu District Health Report, 2005). Malaria is endemic in the district. Kisumu city covers a total area of 417 square kilometers. It has a population of 355,024, out of 504,359 for the entire Kisumu District (Kenya population census 1999). This study was carried out at the Nyanza Provincial Hospital (NPGH), Kisumu District Hospital (KDH), Aga Khan Hospital (AKH) and Port Florence Community Hospital (PFCH) within Kisumu town. The NPGH is a provincial referral hospital, with 378 beds, and 14 wards (one of them is a medical ward). The medical ward admits on average 20-30 patients a day. KDH, located approximately one kilometer from NPGH, has 150 beds capacity with two medical wards. Approximately 20-25 patients are admitted daily. The AKH consists of 82 beds, with one medical ward while PFCH is located approximately 8 kilometers from Kisumu town center.
Study Population: The study population consisted of all 600 patients attending the NPG, KD, AGK and PFC, hospitals from 1st January 2006 to 31st December 2007, with a diagnosis of cryptococcal meningitis confirmed with a positive India ink or CRAG tests on cerebral spinal fluid. The ICD classification of patients was used. To avoid duplication, three patient identifiers were used; name, medical record number and age.
Study design: This was a cross sectional study.
Sample Size: A sample was drawn based on the hospital records that approximately 10% of the patients have cryptococcal meningitis. Fisher’s formula was used to obtain a sample size of 138 [12]. Since the target population is less than 10,000, the sample size was adjustment to 112 as described by Mugenda et. al. 1999 [13].
Data Collection: Every HIV patient with a diagnosis of cryptococcal meningitis during the study period, and gave informed consent to participate was included in the study. In cases where the patient had altered levels of consciousness or were too sick to have dialogue, the interviewer waited till recovery was noted and assistance also sought from the patient’s caretaker. The data was collected for 5 days every week between Monday and Friday. A semi structured questionnaire was used to collect data from every consecutive patient who met the inclusion criteria to elicit responses on demographic characteristics, symptoms presentation and duration, reasons for delay in seeking medical attention, medications taken before admission and awareness on cryptococcal meningitis. Multiple responses were allowed for symptoms, duration of illness and reasons for delay in seeking treatment. The time of commencement of treatment by the patient after admission, length of stay in the hospital and the outcome of the illness were also noted. Permission to carry out this study was obtained from Maseno University School of Graduate Studies which serves as the institutional review board, Medical Superintendents of the respective hospitals, and informed consent from the patients when their diagnosis had been confirmed.
Data Management
At the time of interview, data was first entered manually onto questionnaires. The questionnaires were checked for completeness to ensure all questions were answered. The data was then entered into SPSS ver. 14 computer package and counterchecked against the questionnaires for consistency before analysis by frequencies and percentages.
Results
A total of 202 patients with cryptococcal meningitis were included in the study from the following hospitals: Nyanza Provincial General (36%), Kisumu District (30%), Aga Khan (19%), and PFC (15%). Out of these, 134 (66%) were from public and 68 (34%) from private hospitals.
Demographic Characteristics of the study subjects
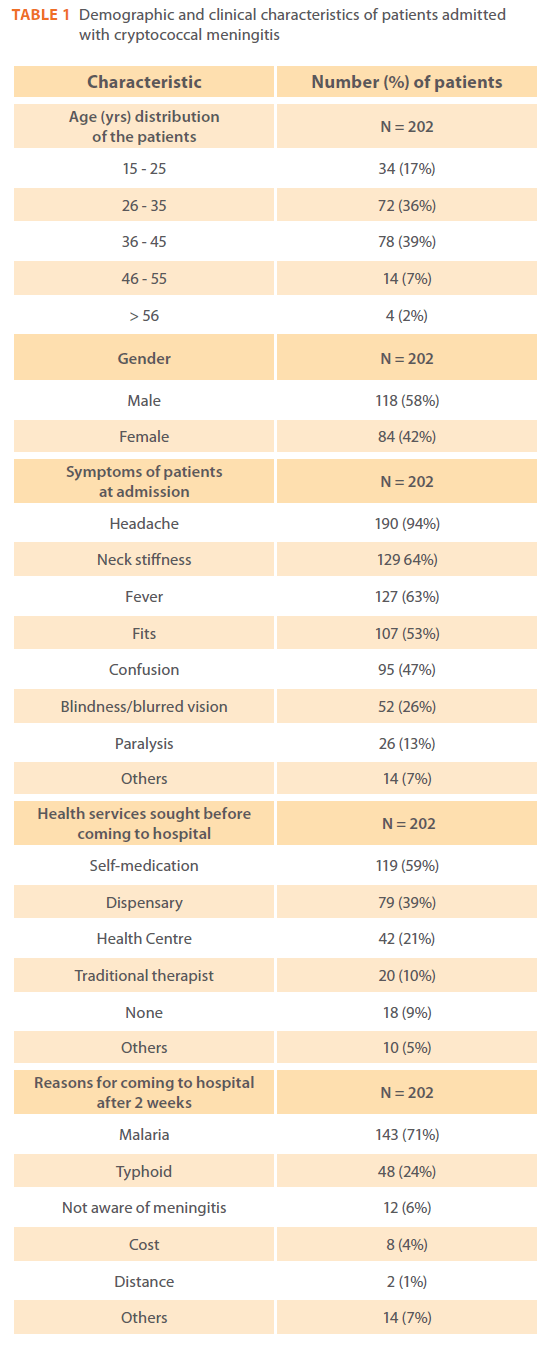
In Table 1, out of the 202 patients sampled, 118 (58%) were males and 84 (42%) females (ratio = 1:1). Up to 150 (75%) were aged between 26 – 45 yrs (range = 16 -75 yrs, mean age = 36 yrs, mode = 37 yrs and median = 36 yrs). One hundred and seventy eight (87%) of them were residents of Kisumu.
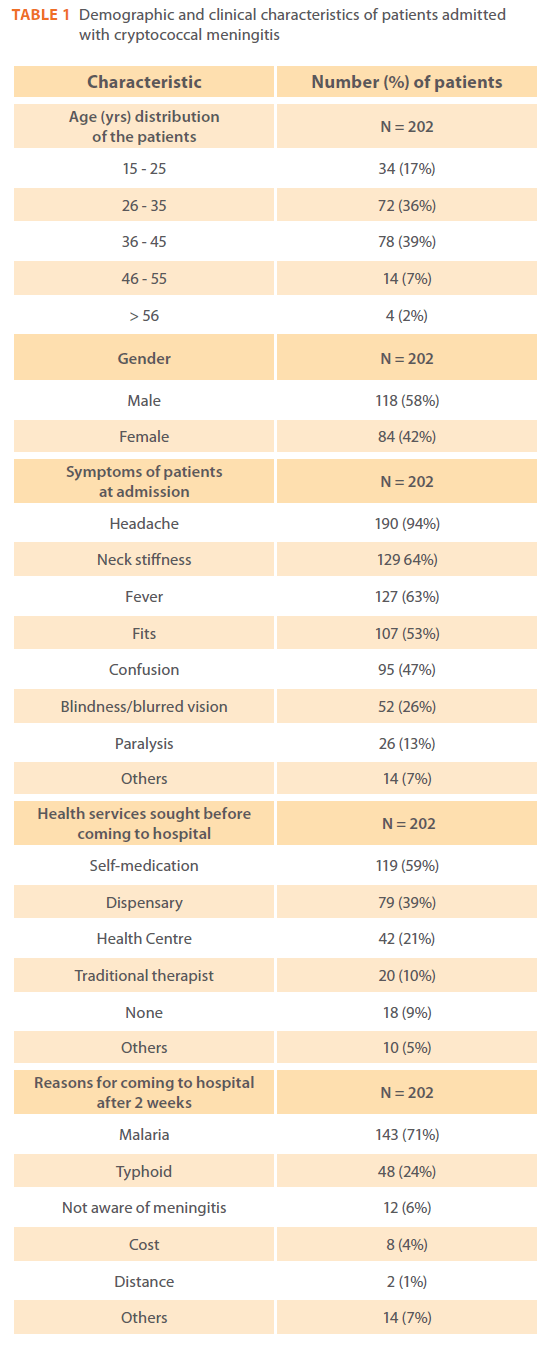
Table 1: Demographic and clinical characteristics of patients admitted with cryptococcal meningitis.
Symptoms of Patients with Cryptococcal Meningitis
The most common symptoms encountered was headache by 190/202 (94%) patients followed by 129/202 (64%) with neck stiffness and 127/202 (63%) fever as shown in Table 1. More severe symptoms were experienced by 13% to 53% of the patients. These included 107/202 (53%) with fits, 95/202 (47%) confusion, 52/202 (26%) blindness/blurred vision and 26/202 (13%) paralysis. Other symptoms experienced by 14 (7%) patients included abdominal pain, coma, diarrhea, vomiting, deafness, dizziness, malaise and nausea.
Duration of Symptoms at admission
The mean number of days patients had symptoms prior to admission was 33 (range 2-200 days). The mean number of days before commencement of treatment for cryptococcal meningitis after admission was 3 days (range 0-20 days). Thus the mean number of days from the onset of symptoms to the commencement of treatment was 36 days. The mean duration of stay in hospital was 12 days (median = 11 days and range = 2-37 days).
Action taken by patients before Admission
Table 1 illustrates options of seeking health services before coming to the hospital. A total of 119/202 (60%) of the patients sought self-medication. Among the health institutions, 79/202 (39%) patients preferred going to dispensaries compared to 42/202 (21.3%) who went to health centres. According to the Ministry of Health, dispensaries are ranked lower in hierarchy than health centres in service delivery. Only 20/202 (10%) used traditional medicines while 18/202 (9%) did not seek any treatment at all. Other modes of health services sought by 10/202 (5%) patients included praying and witchcraft. None of the patients interviewed was aware of cryptococcal meningitis before it was diagnosed at the hospital. The reasons given for coming to hospital after 2 weeks from onset of symptoms were mainly perceived malaria by 143/202 (71%) and typhoid by 40/202 (24%) patients.
Upto 195 (96.5%) of the patients had taken medications before coming to the hospital (Table 1). Among the most common medications, antimalarials, 168/202 (83.2%) and painkillers 151/202 (75.3%) came top on the list, followed by antibiotics 46/202 (23%). For unknown reasons, only 14 (7%) of the patients were on antiretroviral (ARV) treatment. Other modes of treatment included praying and religious beliefs of not accepting medicines to cure disease. None of the patients took any antifungal drugs. There were different types of anti-malaria drugs taken ranging from one by 116/168 (69%) patients, two by 38/168 (22.6%) and three by 14/168 (8.4%). The most common antimalarials taken were quinine (39.5%) and fansidar (26.3%), while consumption of newer antimalarial artemether was only 10.5%. At the study hospitals, once cryptococcal meningitis diagnosis was made, antifungals used included amphotericin B followed by fluconazole or intravenous fluconazole followed by oral doses. This was done in combination with anticonvulsants and intensive care measures as appropriate.
Discussion
Prompt treatment of cryptococcal meningitis depends largely on early reporting of the infected person to a health facility. Thus awareness of symptoms associated with cryptococcal meningitis plays an integral role in the management of the disease. In our study, most of the patients were aged between 26- 45 yrs, which coincides with high prevalence of HIV infections not only in Kenya, but also elsewhere [2]. Headache was the most common symptom followed by neck stiffness and fever. Previous reports from Africa have emphasized the frequency of the classical symptoms of meningitis such as neck stiffness, but the findings from this study suggest broader and perhaps less specific symptoms of cryptococcal meningitis. Among HIV infected adults with cryptococcus meningitis in Ugandan, only half of the patients complained of headache and onefifth presented with neck stiffness [14]. It is evident from these studies that symptoms vary from place to place and it is important to identify those specific to a particular geographical region. Whether geographic differences in rates of cryptococcal meningitis result from variations in socio-economic status, environmental distribution of Cryptococcus neoformans or the distribution of HIV infection is unclear [4]. Findings from our study indicate that headache and fever were among the common symptoms of cryptococcal meningitis, but these are also the common symptoms of malaria [15]. Up to 33% of patients with cryptococcal meningitis may not have neck stiffness. A combination of fever and persistent headache in a patient who is immunocompromised must raise possible meningitis alert. This allows the community to differentiate these symptoms from those of malaria and thus come to the health facility instead of waiting before the disease progresses to a late stage of complications and also to avoid unnecessary consumption of unnecessary drugs. Complications such as confusion and visual abnormalities predict early death from the disease [16].
Antifungals used for cryptococcal meningitis include amphotericin B, azoles (fluconazole, itraconazole, ketoconazole) and flucytosine. In our study, none of the patients knew about cryptococcal meningitis before diagnosis. This may have contributed to the finding that over 70% of the patients were treated for malaria before coming to the hospital. The treatment was done either by self-medication, at the dispensaries or health centers where there are no expert personnel on cryptococcal meningitis. Preference for dispensaries rather than heath centres may be due to greater accessibility of the former or lack of seriousness attached to the symptoms. Many patients and/ or health caretakers may have confused symptoms of malaria with those of cryptococcal meningitis. Consequently, being treated for malaria seemed to be a major factor for delay in coming to hospital. Most of the drugs taken before admission were antimalarials and painkillers. This could contribute to the delay observed in seeking medical attention. The most common antimalarial drugs taken were quinine and fansidar while consumption of newer recommended but expensive antimalarials, Artemether, was lower. Other patients had taken antibiotics, mostly for typhoid, before admission. In resource-limited settings, use of antibiotics is rampant [17,18]. Antibiotics are usually the norm in the health facilities where laboratory tests are not performed due to erratic availability of equipment. In this study, prior to admission, over 30% of patients were treated with antibiotics probably for bacterial instead of cryptococcal meningitis This has grave public health implications because it can lead to increased drug resistance, wastage and unnecessary expenditure, in addition to causing further delay in seeking appropriate treatment, therefore poor prognosis. This may be responsible for the high mortality observed in the study population. Factors that are likely to contribute to high mortality rate of cryptococcal meningitis include late presentation and no access to ARV therapy [15,18,19].
The mean duration of stay in hospital was 12 days. Underlying causes of HIV infection in increasing numbers of meningitis patients would require more hospital beds and an increase the medical expenditures in the study area. Extending the role of clinics and staff into the community might facilitate both earlier presentation and access to services [20]. Factors that predict early death from cryptococcal meningitis include if the person infected is not on ARV therapy. Cryptococcal meningitis occurs at a relatively late stage of AIDS and yet in this study, only 7% of patients were on ARVs. Increasing availability of ARV treatment for HIV should be accompanied by improvements in detection of the cryptococcal meningitis so as to reduce morbidity and mortality.
In conclusion, HIV infection is a major risk factor for cryptococcal meningitis. Changes in public health measures need to be instituted in the management of cryptococcal meningitis to include education of population and health care workers on the non-specific and insiduous clinical presentation of the condition. These headache, neck stiffness and fever which can be mistaken for typhoid or malaria. Emphasis on measures such as health education and prompt reporting of symptoms to appropriate health care facilities followed by india ink laboratory diagnosis may be suitable approaches to avoid unnecessary empirical antibiotics therapy. and prevent cryptococcal disease. Vaccine development should be deemed a priority in the control and prevention of cryptococcal disease. The potential benefit of these interventions for management may only be estimated with appropriate epidemiological surveillance data.
Acknowledgement
We wish to thank Maseno University, management and staff of all the health facilities, and the respondents for their cooperation during the study.
Competing Interests
Authors declare that no conflict of interests exist.
- Woldmanuel D, Halle T (2001). Cryptococcosis in patients from TikurAnbessa Hospital, Addis Ababa, Ethiopia. Ethiopian Medical Journal 39 (3): 185-192.
- Mwaba P, Mwansa J, Chintu C, Pobee J, Scarborough M et. al. (2001). Clinical presentation, natural history, and cumulative death rates of 230 adults with primary cryptococcal meningitis in Zambian AIDS patients treated under local conditions. Postgraduate Medical Journal 77:769-773.
- Wang W. (2001). Clinical manifestations of AIDS with cryptococcal meningitis. Chinese Medical Journal, 114 (8): 841-843
- Levitz SM. (1991). The ecology of Cryptococcus neoformans and the epidemiology of cryptococcosis. Rev Infect Dis 13:1163-1169
- Banerjee U (2005). Progress in diagnosis of opportunistic infections in HIV/AIDS. Indian Journal of Medical Research 121:395-406.
- Ouma C (2001). Treating HIV/AIDS in Kenya, Dying from Lack of Treatment: The International AIDS Crisis. MSF Speech 21/06/2001.
- Aberg J, Powderly WG (2002). Cryptococcosis. In: The AIDS Knowledgebase. A text Book on HIV disease. University of Carlofornia, San Francisco.
- Powderly WG (1992). Therapy for cryptococcal meningitis in patients with AIDS. Clinical Infectious Diseases 14: S54 – S59.
- Spitzer ED, Spitzer SG, Freundlich LF, Kasadevall A (1993). Persistence of the initial infection in recurrent cryptococcal meningitis. Lancet 341: 595 – 596.
- Edwards C, Boucher I, Haslett C, Chilvers E (2005). Diseases due to Infection In: Davidson’s Principles and Practice of Medicine, 17th Edition. Churchill Livingstone, Edinburgh, United Kingdom
- NASCOP 2004. Scaling up Antiretroviral Programme in Kenya.
- Fisher A, Lang J, Stoeckel J, Townsend J (1991). A Handbook for Family Planning Operations Research Design. 2nd Edition. The Population Council. New York.
- Mugenda OM, Mugenda AG. (1999). Research Methods – Quantitative & Qualitative Approaches. Acts Press, Nairobi, Kenya.
- French N, Gray K, Watera C, Nakiyingi J, Lugada E et. al. (2002). Cryptococcal infection in a cohort of HIV-1-infected Ugandan adults. Journal of AIDS 16 (7): 1031- 1038.
- Wang W, Carm AR (2001). Clinical manifestations of AIDS with cryptococcal meningitis. Chinese Medical Journal 114(8): 841- 843.
- PitisuttithumP ,Tansuphasawadikul S, Simpson AJ, Howe PA, White NJ. (2001). A prospective study of AIDS-associated cryptococcal meningitis in Thailand treated with high-dose amphotericin B. J Infect. 43(4): 226-233
- Kakai R, Wamola IA (2002). Minimizing antibiotic resistance to Staphylococcus aureusin developing countries. East African Medical Journal 79 (11): 574 – 579.
- Kisenge PR, Hawkins AT, Maro VP, Mchele J, Ndealilia SS et. al. (2007) CD4 count plus coma predicts cryptococcal meningitis in Tanzania. BMC Infectious Diseases 7:39 – 43.
- Schaars CF, Meintjes GA, Morroni C, Post FA, Maartens G (2006). Outcome of AIDS-associated cryptococcal meningitis initially treated with 200 mg/day or 400 mg/day of fluconazole. Journal of Infectious Diseases 10: 116-118.
- Ki-Zerbo GA (1996). AIDS-related cryptococcal meningitis at the Bobo-Dioulasso Hospital Center: five case reports Medical Tropical Journal 56(1): 63 – 65.
225