Abulgasem Etraim, Hanan Eljabu*, Ismail Elfortia and Awatif Andisha
Libyan National Fertility Centre- Misurata, Qaser Ahmed, Residential City, Misurata, Libya
- *Corresponding Author:
- Hanan Eljabu
Libyan National Fertility Centre- Misurata, Qaser Ahmed, Residential City, Misurata, Libya
Tel: 00218924562996
E-mail: a.aljabu@lnfc.med.ly
Received Date: December 28, 2020; Accepted Date: January 11, 2021; Published Date: January 15, 2021
Citation: Etraim A, Eljabu H, Elfortia I, Andisha A (2021) Delayed Diagnosis and Management of Second Trimester Cervical Ectopic Pregnancy - Case Report. Health Sci J. 15 No. 1: 785.
Keywords
Second trimester cervical ectopic pregnancy; Medical versus surgical treatment; Preservation of fertility
Introduction
The implantation of the gestational sac in the cervical canal is called an ectopic pregnancy which is a rare kind of pregnancy (only less than 1%) and carries high mortality and morbidity rates [1]. There are various risk factors for cervical pregnancy including insertion of intrauterine devices, previous cervical procedures and/or endometrial curettage [2,3]. Ultrasound technology and improvement in its resolution can provide an early diagnosis of rare types of pregnancies and this positively reflects on management modalities and so reduces the associated morbidities and mortalities [4].
The cervical ectopic pregnancy could be presented as either an asymptomatic condition to a life threatening condition [1]. So, the diagnosis of an ectopic pregnancy can be early (first trimester) or late (second trimester) and that will affect the management modalities used. The management of cervical ectopic pregnancy could be conservative by use of methotrexate or could extend to more invasive intervention that can affect the fertility of the patient such as a hysterectomy [2].
Case Report
A 36 year old female, gravida 1, para 0, presented to the emergency department as a case of 24 weeks and 0 day pregnancy with a 2 week history of on and off vaginal bleeding and rupture of the amniotic membrane. The pregnancy was planned and sure of date. The initial ultrasound at 10 weeks revealed an intrauterine pregnancy with positive foetal heart and had regular antenatal follow ups without complications.
At 22 weeks, the patient complained of multiple attacks of per-vaginal bleeding with abdominal pain and was diagnosed as a threatened abortion. On arrival, the patient was hypotensive and tachypnic (BP: 90/60 mmHg and HR: 100 beat/min). A repeat ultrasound was performed and the gestational sac was noted in the lower part of the uterine cavity and diagnosed as an invetable abortion (positive foetal heart). A positive C-reactive protein was recorded and intra-venous antibiotics (Cefatriaxon and Metronidazole) were started.
As the clinical state of the patient had deteriorated, the decision for pregnancy termination was taken and syntocinon infusion was started immediately. After one hour, the baby was delivered; however the placenta was not. Patient was kept under uterotonic infusion (pabal infusion and per-rectal misoprostol) for almost an hour and it was finally decided to remove the placenta under general anaesthesia. Perfuse per-vaginal bleeding was started and active management was performed in steps (bimanual uterine compression, uterotonic infusion and Bakry balloon), and cervical examination revealed floaby with no tear. Evacuation and curettage was performed.
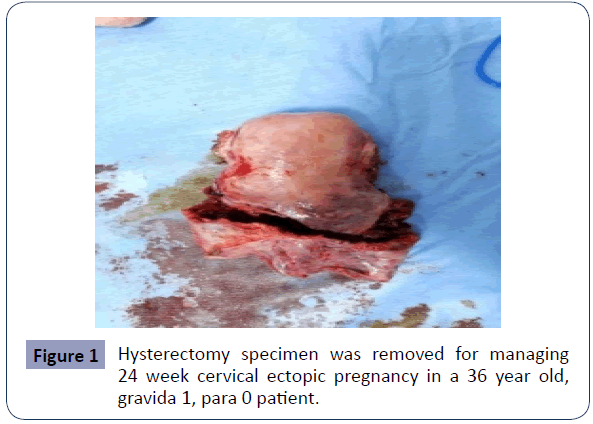
The heavy per-vaginal bleeding was still not in control and the patient`s heamo-dynamic situation was deteriorating, so an exploratory laparotomy was performed and revealed well contracted normal size uterine fundus with floaby lower part of the uterus and cervix (Figure 1). A cervical ectopic pregnancy was diagnosed and a total abdominal hysterectomy was done in steps. Five units of whole blood with three units of fresh frozen plasma had to be transfused between the intra and post-operative care units.
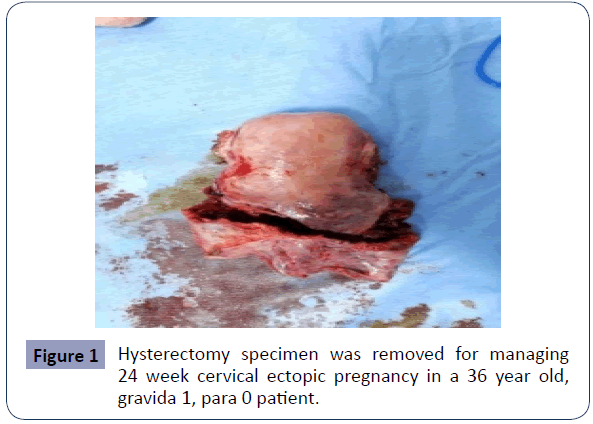
Figure 1 Hysterectomy specimen was removed for managing 24 week cervical ectopic pregnancy in a 36 year old, gravida 1, para 0 patient..
The tissue specimen was sent for a histopathology study and the result revealed cervical implantation of the conceptus tissue (cervical pregnancy). The patient was kept in the department for three days and discharged in good physical condition and progressing well with emotional recovery. After a while, the patient made a fully physical and emotional recovery and is now doing well with her family at home.
Discussion
During the last decade, the management of cervical ectopic pregnancy has changed as it results after implantation of an embryo in the cervical canal [1,2]. Previously, the diagnosis was suspected clinically after sudden, uncontrollable bleeding following treatment of incomplete abortion [1] and abdominal hysterectomy was the treatment of choice in order to preserve the life of the patient. Nowadays, early diagnosis of cervical ectopic pregnancy is the main goal to preserve the fertility of the patient [4]. Despite this, a cervical ectopic pregnancy can still be missed and can be ended by loss of one fertility organ (hysterectomy) [5-7].
In this case, the early presentation (in terms of symptoms) was unremarkable and this led to a lack of early diagnosis of cervical ectopic pregnancy and so allowed the pregnancy to progress to the second trimester which negatively affected the fertility of the patient. Binarwan and Hilma[8] presented a case with a second trimester cervical ectopic pregnancy and managed with hypogastric (Internal Iliac) artery ligation and massive bleeding continued after the ligation procedure, therefore a hysterectomy was done. Moreover, other cases reported cervical ectopic pregnancy at 13 weeks and after failure of conservative treatment, a hysterectomy was undertaken [9-11].
On the other hand, early diagnosis by ultrasound has proved very useful in terms of fertility preservation. The conservative management approach usually employs different techniques according to the case response (evacuation suction and curettage, MTX injection, insertion of tamponade and ligation of arteries) and in some situations, all measures had to be performed for the same case [1,12].
Conclusion
The early diagnosis and so management of cervical ectopic pregnancy by using an ultrasound scan and applying conservative management has a positive impact on preserving the fertility of the patient. This case demonstrates the difficulty in diagnosing cervical ectopic pregnancies but also highlights the importance of training in the obstetric and gynaecology departments as recommended by the Obstetrics and Gynaecology Society to eliminate possible suspected complications.
34621
References
- Takeda K, Mackay J, Watts S (2018) Successful management of cervical ectopic pregnancy with bilateral uterine artery embolization and methotrexate. Case Rep Emerg Med 2018:9593824.
- Gun M, Mavrogiorgis M (2002) Cervical ectopic pregnancy: a case report and literature review. Ultrasound Obstet Gynecol 19:297-301.
- Dobrosavljevic A, Nikolic B, Jurisisc A, Zečević N, Aničić R, et al. (2019) Diagnosis and treatment of cervical ectopic pregnancy–case report. Clin Exp Obstet Gyn 46:139-140.
- Shirinzadeh L, Jafarian AH, Davachi B, Seresht LM, Azimi H, et al. (2020) Successful Management of Cervical Ectopic Pregnancy: A Case Report. J Midwifery Reproductive Health 8:2208-2212.
- Munoz JL, Kalan A, Singh K (2018) Second trimester cervical ectopic pregnancy and hemorrhage: a case report and review of the literature. Case Reports Obstet Gynecol 2018: 3860274.
- Massoud D, Halimeh R, Sleiman R, Geahchan A, Abdallah A, et al. (2020) Cervical Ectopic Pregnancy, a Case Report and Literature. J Gynecol Obstet 8:85-90.
- Tanos V, ElAkhras S, Kaya B (2019) Hysteroscopic management of cervical pregnancy: Case series and review of the literature. J Gynecol Obstet Hum Reprod 48:247-253.
- Halim B, Lubis HP (2019) Bilateral hydronephrosis and hydroureter associated with 21-22 weeks gestational age of cervical ectopic pregnancy: a case report. Int Med Case Rep J 12:217-222.
- Khatib Y, Khashikar A, Wani R, Patel RD (2016) Cervical ectopic pregnancy: A case report of missed diagnosis. Med J Dr. DY Patil Univ 9:741-743.
- Mouhajer M, Obed S, Okpala AM (2017)Cervical ectopic pregnancy in resource deprived areas: A rare and difficult diagnosis. Ghana Med J 51:94-97.
- Amani DSM, Ilunga-Mbaya E, Iyawa FE, Nsiangangu BK (2020) Cervical Pregnancy in a Primigravida Patient without Risk Factors: A Case Report. Open J Obstet Gynecol 10:770.
- Buppasiri P, Salang L, Ahooja A, Kietpeerakool C (2020) Successful Conservative Treatment for Large Cervical Ectopic Pregnancy. Thai J Obstet Gynaecol 28: 251-255.