Gregory Tsoucalas*
History of Medicine, Faculty of Medicine, University of Thessaly, Larissa, Greece
- *Corresponding Author:
- Gregory Tsoucalas
Agios Georgios, Hellenic Reference
Centre for Alzheimer Disease and Related
Syndromes, Alykes, Volos, Greece.
Tel: 00306945298205
E-mail: gregorytsoucalas@yahoo.gr
Received date: May 01, 2017; Accepted date: May 04, 2017; Published date: May 11, 2017
Citation: Tsoucalas G. Dementia and Pressure Ulcers in Greece during the Economic Crisis, The Last Samurai. J Univer Surg. 2017, 5:3. doi: 10.21767/2254-6758.100079
Copyright: © 2017 Tsoucalas G. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
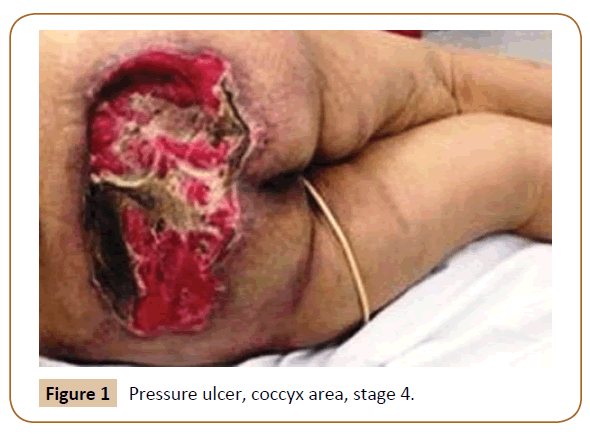
Editorial
Despite our increased efforts in chronic hospitalized dementia patients, pressure ulcers (PU) remain a major health care issue, affecting patient's quality of life and psychological peace of both the caregivers and physicians. A PU is defined as a skin lesion caused by unrelieved pressure resulting in damage to the underlying tissue. Caring for an individual with Alzheimer's disease or a related dementia can be challenging and at times overwhelming. There is a higher rate of functional and cognitive impairment with dementia coinciding with immobility, which results in a higher rate of decubitus ulcers, affecting areas like heel, ball of foot, coccyx [Figure 1], and shoulder blades [1]. Moreover, diabetes, post-fracture state, infections, multiple sicknesses, dysphagia, malnutrition, deep vein thrombosis, are increasing the probability for the appearance of a "bed" ulcer. The term "bed" could be the most appropriate, as duthe end stage dementia most patients spend their time confined on wheel chair or bed [2]. Advanced dementia and pus in the same patient results in earliermortality. The median survival is significantly shorter in comparison with similar patients without PUs [3]. Trajectories of treatable, burdensome symptoms such as PU at the end of life in specialized centres should be a priority focus for quality improvement. Despite all efforts to prevent a PU by providing support surfaces that redistribute pressure and by turning residents to reduce length of exposure (every 2 or 4 hours intervals), they seem as an unavoidable incident. With thorough and comprehensive medical management, much pus may heal completely without the need for surgical intervention. It is most likely though, that a surgical treatment would be needed. Many are the issues to be addressed, spasticity must be controlled, nutritional status must be optimized, and the wound must be clean and free of infection. In the case of a significant fecal soiling into the injury, diverting colostomy should be considered before reconstruction [4,5]. All these barriers they produce a burdensome financial cost regarding the great numbers of dementia patients (almost 200.000) among an aging population in Greece [6,7]. Can Greece manage such a situation during an economic crisis? Do those patients deserve the best treatment? As Greece should attend to it, a series of ethical considerations emerge. Us, the physicians, we are wondering between patients, caregivers, ethical obligations and insufficient funds, as the last samurai, to fight both an emotional-ethical and an economic battle with a doubtful outcome at best.
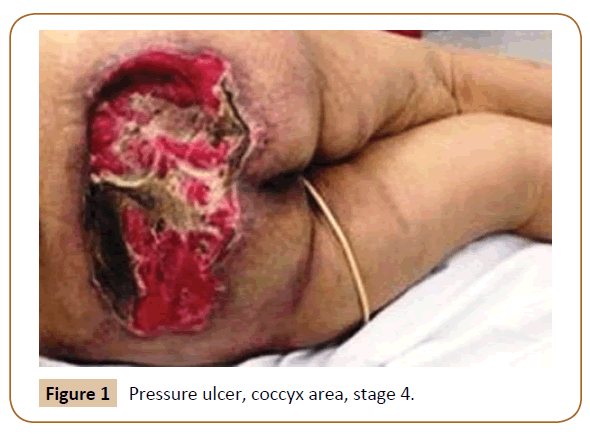
Figure 1: Pressure ulcer, coccyx area, stage 4.
19055
References
- Volicer L (2004) Hospice Care for Patients with Advanced Progressive Dementia. Springer Publishing Company, New York.
- Carlsson ME, Cunningberg L (2017) Predictors for Development of Pressure Ulcer in End-of-Life Care: A National Quality Register Study. J Palliat Med 20: 53-58.
- Jaul E, Meiron O, Menczel J (2016) The Effect of Pressure Ulcers on the Survival in Patients With Advanced Dementia and Comorbidities. Exp Aging Res 42: 382-389.
- Bergstrom N, Horn SD, Rapp M, Stern A, Barrett R, et al. (2014) Preventing Pressure Ulcers: A Multisite Randomized Controlled Trial in Nursing Homes. Ont Health Technol Assess Ser 14: 1-32.
- Doughty D (1990) The process of Wound Healing: A Nursing Perspective. Prog Develop Ostomy Wound Care 2: 3-12.
- Bail K (2016) Costs of Complications in Hospitalised Dementia Patients. Aust Nurs Midwifery J 23: 44.
- Tsolaki M, Fountoulakis K, Chanzi E, Paylopoulos I, Kotanidis A, et al. (1999) Prevalence of Dementia in Greece, 14th Hellenic Congress of Neurologists, Athens 1995. American Journal of Alzheimer's Disease 14: 138-148.