JM Pardal-Fernández MD PhD1*, JL Beato-Pérez MD1, E Lozano-Setién MD2, I Iniesta-López MD PhD FRCP3
Department of Clinical Neurophysiology. University General Hospital. Albacete. Spain.
Department of Internal Medicine. General Hospital. Hellin. Albacete. Spain.
Department of Neuroradiology. University General Hospital. Albacete. Spain.
Department of Neurology. The Walton Centre NHS Foundation Trust. Liverpool. United Kingdom.
*Corresponding Author:
Dr. Jose Manuel Pardal Fernández
Department of Clinical Neurophysiologist (Electromyography). University General Hospital
C/Hermanos Falcó, S/N. 02006 – Albacete
Spain
Email: josempardal@yahoo.es
Key words
Denervation hypertrophy; radiculopathy; complex repetitive discharges; botulinum toxin.
Introduction
Muscle denervation is a pathological condition related to a neural dysfunction which ultimately leads to the muscle fibre death. The extensive denervation leads to a reduction in muscle volume. However, occasionally does the opposite phenomenon occur that is, the so-called denervation hypertrophy (DH). Such paradoxical situation has been described in the context of radiculopathies, anterior horn cell disease, spinal muscular atrophy, post-polio syndrome and chronic neuropathies [1-3]. DH has rarely been found to involve the L5 myotome, especially with subsequent hypertrophy of the tensor fascia lata (TFL) muscle. We present a case of DH in the context of an L5 radiculopathy.
Case report
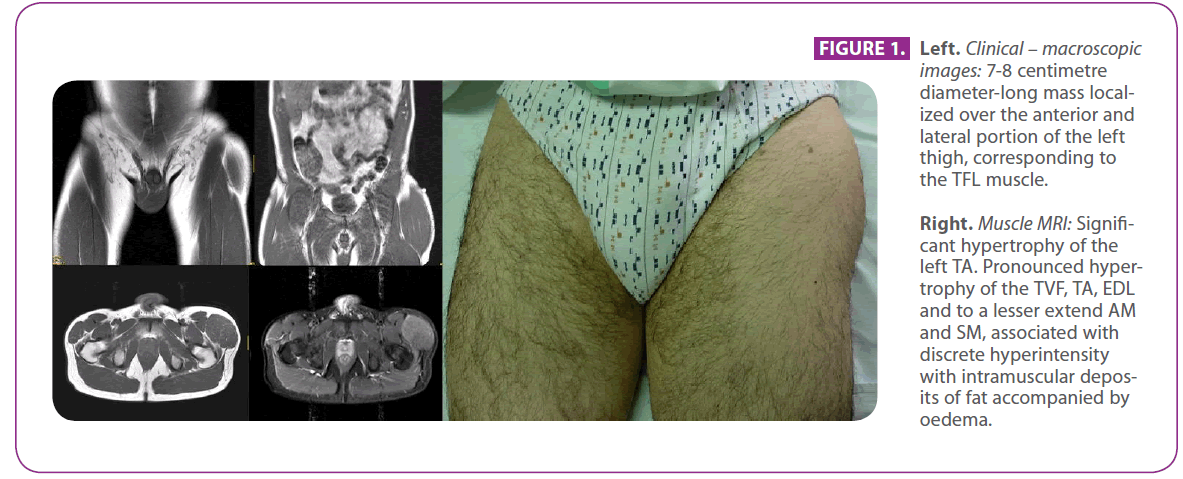
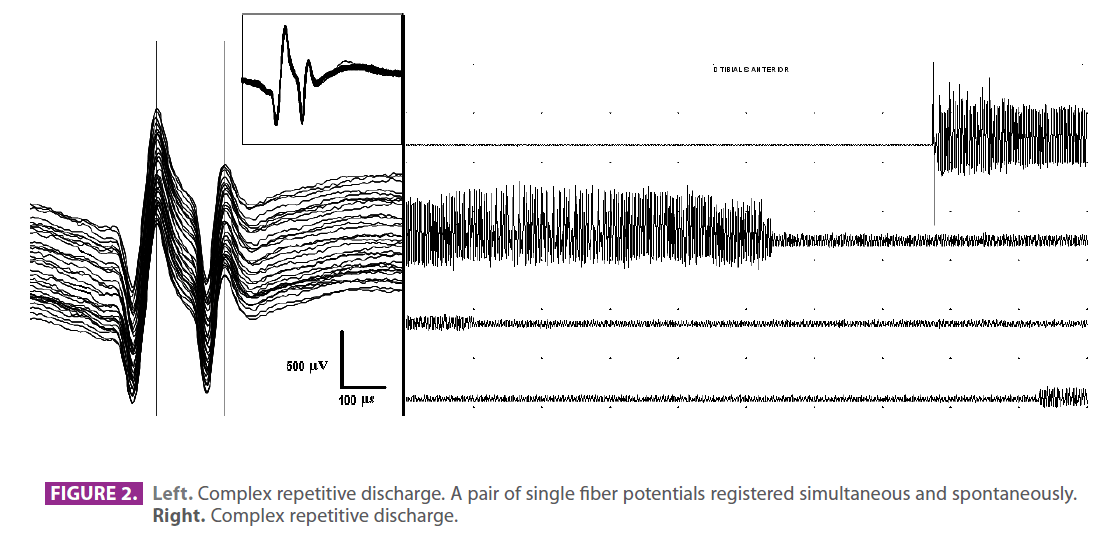
A 47-year-old athletic male with a long-standing history of chronic back pain and left sciatica, presented to us with a hard, slightly painful lump over the anterior and lateral aspect of the thigh [figure 1], which had developed over the previous six months. Muscle MRI showed changes consistent with hyper-trophy involving TFL and tibialis anterior (TA) [figure 1]. Lumbosacral MRI showed a disc protrusion at L4-L5 and into the L5 intervertebral foramen. There was no indication for surgery according department of neurosurgery. Serum CK, myoglobin and aldolase where all raised. Needle electromyogram (EMG) on the hypertrophic muscles showed continuous complex repetitive discharges (CRDs) at rest. When examined under voluntary activity, signs of chronic reinnervation were present. Single fibre EMG (SFEMG) by spontaneous 20 pairs of fibres potentials showed jitter value of less than 5 μs (figure 2). The biopsy of TFL was compatible with chronic neurogenic denervation.
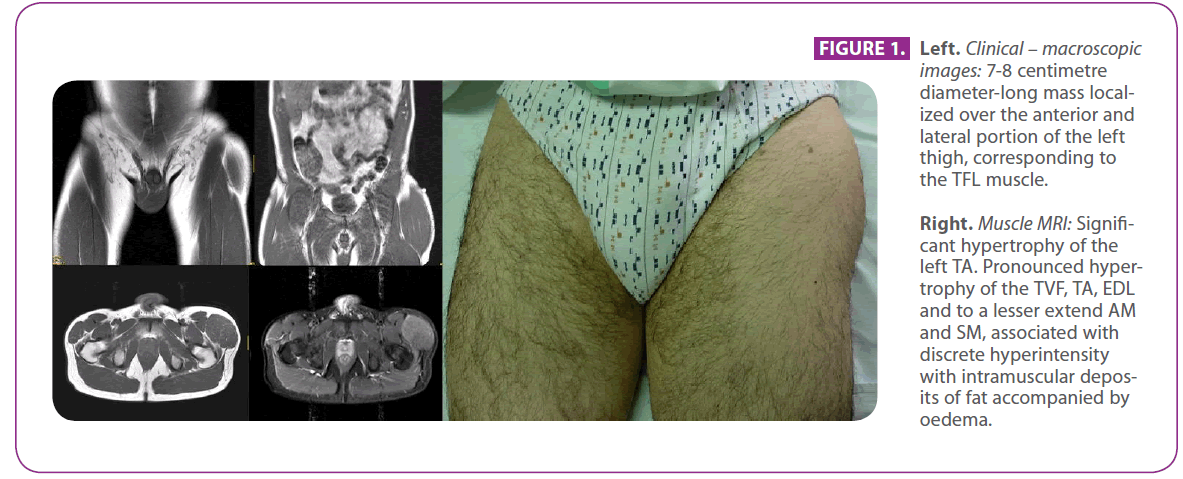
Figure 1: Left. Clinical – macroscopic images: 7-8 centimetre diameter-long mass localized over the anterior and lateral portion of the left thigh, corresponding to the TFL muscle.
Right. Muscle MRI: Significant hypertrophy of the left TA. Pronounced hypertrophy of the TVF, TA, EDL and to a lesser extend AM and SM, associated with discrete hyperintensity with intramuscular deposits of fat accompanied by oedema.
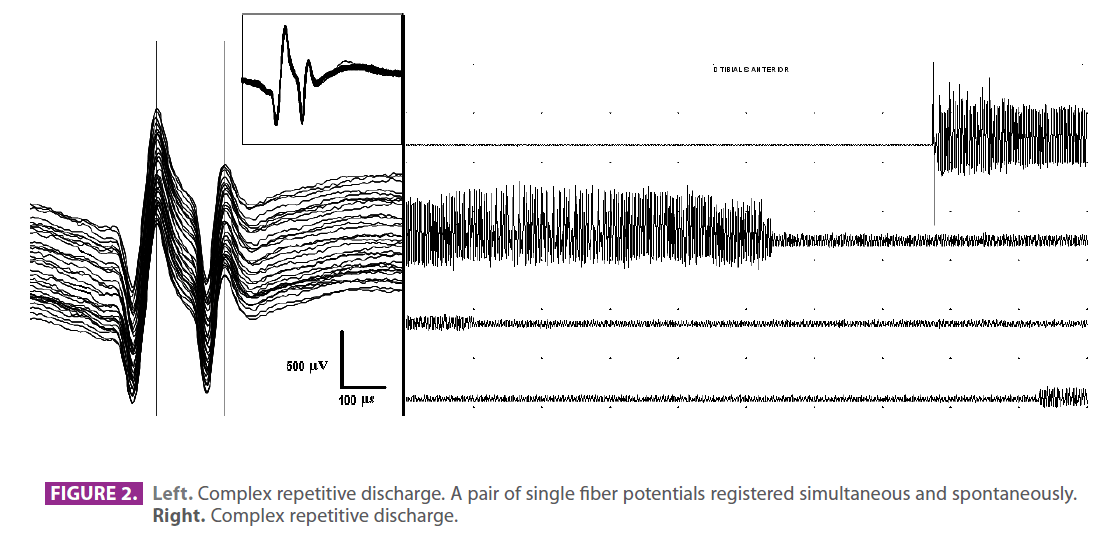
Figure 2: Left. Complex repetitive discharge. A pair of single fiber potentials registered simultaneous and spontaneously.
Right. Complex repetitive discharge.
Outcome
The patient received 3 dosages of botulinum toxin (BT) within 12 months, which was administered on 2 sites, including TFL and TA. An initial dose of 50 U of BT failed to produce any clinical changes, albeit CRDs dropped significantly. After six months 75 U were administered to each muscle, with a slight symptomatic improvement, whilst CRDs were otherwise again diminished. In the next 6 months 120 U made CRPs nearly disappear and the muscle size was reduced slightly. The jitter did not demonstrate significant changes in this time.
Discussion
We present a patient with DH in L5 radiculopathy. This case is a rare condition of botulism toxin responsive radicular DH involving the TFL muscle.
Only 50 cases have been previously documented thus far, since the first case reported by Graves [4]. To our knowledge, the present case is only the second documented with the above described features, particularly the hypertrophy of TFL [1]. The pathophysiology remains speculative [5]. Maybe the denervation could play a significant role for the regulation of muscle mass, including an induction of compensatory hypertrophy (6). Proliferating muscle cell nuclear antigen in denervation may lead to hypertrophy of slow-switch (type I) and slow tonic (type III) muscle fibers (7) or the increasing amino-acid levels (8).
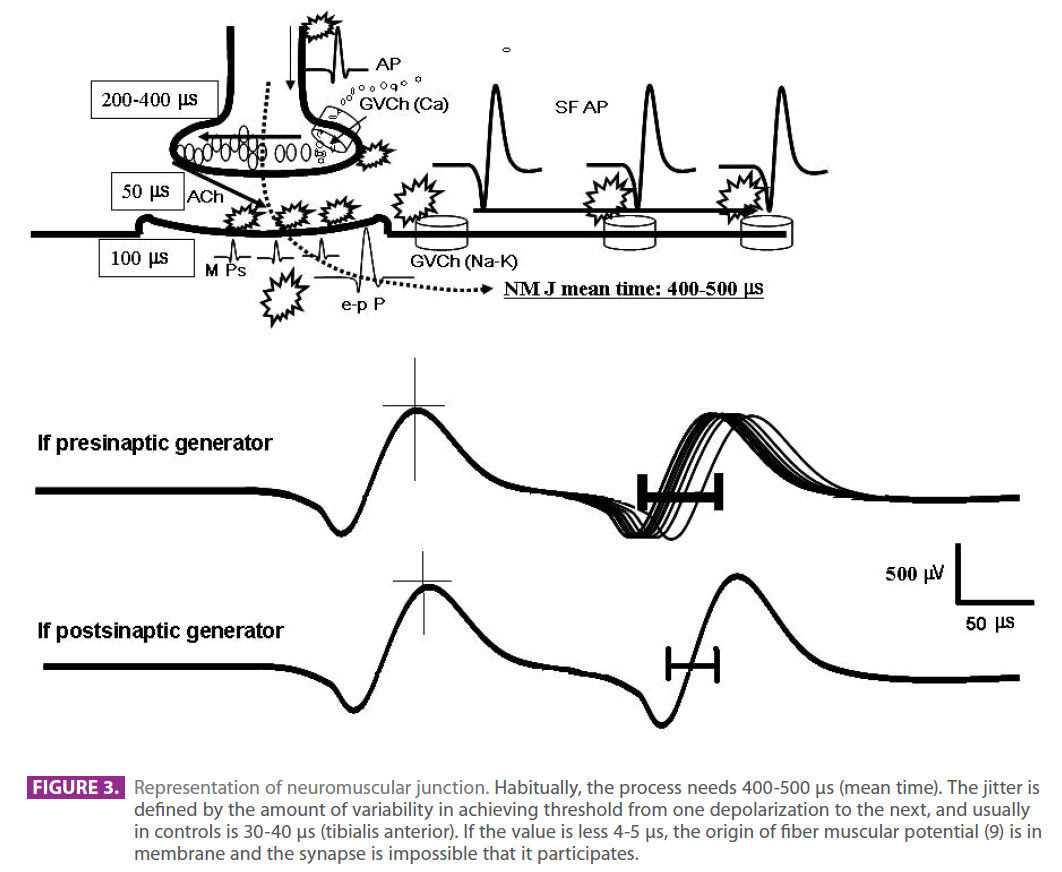
One of the most striking findings in this case was the CRDs. The extremely reduced jitter values of less than 5 μs enables us to rule out the synapse (neuromuscular junction) as a mediator in the diffusion of the CDRs [9] (figure 3), and this feature remained throughout all the time studied. The CRDs reduced after BT injection. This together with the positive response to BT could either be explained by an interaction of BT with membrane structures of the muscle fibre and indeed calcium mediated metabolism [10]. The sligth changes in muscle size could perhaps be justified by the inner balance which was achieved. Finally and in accordance with previous reports this case highlights the potential benefits of using BT in DH.
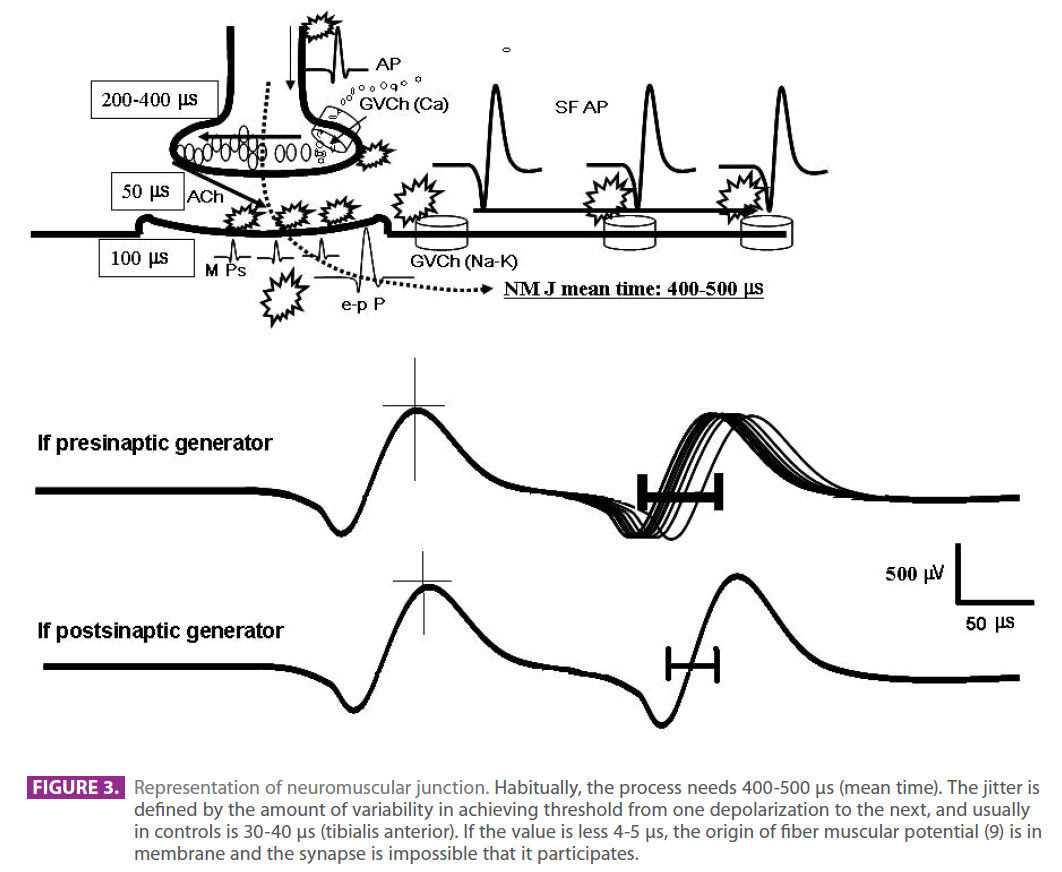
Figure 3: Representation of neuromuscular junction. Habitually, the process needs 400-500 μs (mean time). The jitter is defined by the amount of variability in achieving threshold from one depolarization to the next, and usually in controls is 30-40 μs (tibialis anterior). If the value is less 4-5 μs, the origin of fiber muscular potential (9) is in membrane and the synapse is impossible that it participates.
2206
References
- Chang DG, Magee E, Hughes T. Denervation hypertrophy in lumbosacral radiculopathy. J Neurol Neurosurg Psychiatry 2008; 79: 1170.
- Gutmann L. AAEM minimonograph#46: neurogenic muscle hypertrophy. Muscle Nerve 1996;19:811–8.
- Mattle HP, Hess CW, Ludin H, Mumenthaler M. Isolated muscle hypertrophy as a sign of radicular or peripheral nerve injury. J Neurol Neurosurg Psychiatry 1991;54:325–9.
- Graves JR. clinical lectures on the practice of medicine vol.1.2nd ed. Dublin: Fannin; 1848, p. 498.
- Costa J, Graça P, Evangelista T, et al. Pain and clan hypertrphy associated with spontaneous repetitive discharges treated with botulinum toxin. Clin Neurophysiol 2005; 116: 2847-52.
- Bernat JL and Ochoa JL, Muscle hypertrophy after partial denervation: a human case, 1978;41(8):719-25.
- Bakou S, Cherel Y, Gabinaud B, Guigand L, Wyers M. Type-specific changes in fibre size and satellite cell activation following muscle denervation in two strains of turkey (Meleagris gallopavo). J Anat, 1996;188 ( Pt 3):677-91.
- Turner LV, Manchester KL. Effects of denervation hypertrophy in rat diaphragm muscle on the activity of ribosomes and sap fractions in protein synthesis. Biochim Biophys Acta. 1973 Apr 11;299(4):612-20.
- Trontelj JV, Stålberg E. Single fiber electromyography in studies of neuromuscular function. Adv Exp Med Biol, 1995;384:109-19.
- Semsarian C, Wu MJ, Ju YK, Marciniec T, Yeoh T, Allen DG, Harvey RP, Graham RM. Skeletal muscle hypertrophy is mediated by a Ca2C-dependent calcineurin signalling pathway. Nature 1999; 400(6744):576–81.