Keywords
Multiple sclerosis; Anxiety; Depression; Occupational therapy
Introduction
Multiple sclerosis is a chronic degenerative disease of the central nervous system with symptomatology that varies both the type and intensity in persons with this disease. It is a disease of the young adult age whose first symptoms usually appear between 20-40 years [1].
Depression can affect 15% to 47% of people with multiple sclerosis [2,3]. Research data record that 25% of people with multiple sclerosis are reporting depressive symptoms and that depression is not diagnosed clinically and has not been addressed interdisciplinary because the emphasis is on treatment of pain and other symptoms the patient is experiencing [3,4]. The annual probability of the occurrence of depression in patients with multiple sclerosis reaches 20%, [3] while exacerbation of depressive symptomatology appears more frequent after disease onset [5]. Finally, depression is an important factor influencing the quality of life of people with multiple sclerosis, while it seems to have an impact on the recovery of neurological symptoms after relapse [6]. Rabinowitz et al. [7] using a longitudinal design examined coping mechanism and cognitive functioning in the development of depression in individuals with multiple sclerosis and found that cognitive dysfunction leads to depression partially due to cognitive’ s effects on coping mechanism.
The anxiety has not been studied as much as depression in people with multiple sclerosis [8]. The prevalence of reported anxiety amongst multiple sclerosis patients has varied from 14% to 41% [9]. Although the studies show fairly high rates of anxiety in this category of patients, they mainly focus in people with relapse who are hospitalized in neurological clinic and therefore do not constitute a representative sample of all individuals with multiple sclerosis [3]. Female patients compared to men patients with multiple sclerosis appear to be more anxious, while the combination of anxiety and depression associated with frequent suicidal thoughts, psychosymptopatology and social withdrawal [9,10].
In multiple sclerosis anxiety and depressive symptomatology are the most frequently observed emotional reactions. Clinically significant degree of anxiety is present in exacerbation phase of the disease, up to 90% of patients. Data also support a relationship between stress from economic factors and depression among individuals with multiple sclerosis [11]. Major depression is doubled in patients who had been hospitalized for multiple sclerosis than in patients who had been hospitalized for others reasons [12]. Data obtained from Feinstein [13] reported that suicidal patients with multiple sclerosis were significantly more likely to have lifetime diagnoses of major depression, anxiety disorder, comorbid depression-anxiety disorder. Bipolar disorder in people with multiple sclerosis occurs at rates ranging from 13% to 40%, while psychotic episodes are not very often, except for some cases where psychotic episodes similar to schizophrenia, coincide with the relapses of the disease [14].
Women seem to react more positively to the onset of the disease, with more optimism, less anxiety and depression, and more willing to stay in their jobs than their male patients [15]. The medicine treatment of depression and anxiety in multiple sclerosis includes appropriate medications and application of appropriate psychosocial response measures to both the patient and his family. One of the no pharmacological services to persons with multiple sclerosis is occupational therapy that provides services in both sensorimotor level and psychological adjustment of the patients, because the patient with multiple sclerosis who has depressive symptomatology and/or anxiety influenced in daily occupations and activities, in role performance, community engagement and finally in his/her quality of life.
Purpose
The first objective of this research was to study the symptoms of anxiety and depressive symptomatology in young women with multiple sclerosis in Greece and secondly investigate whether there was a relationship between certain demographics characteristics and the symptoms of anxiety and depression.
Methodology
Participants
Participants were 37 women. Half of these individuals are members of the Association of multiple sclerosis in Athens; the other half comes from the National Institute of Rehabilitation (E. K. A.). The criterion for their selection was their sex (women only) and the non-pharmacological therapy for pre-existing depression and anxiety. Their age ranged between 18 and 50 years old, with a mean age of 34, 67 years (SD =5, 99).
Procedure
The research took place at the site of the Association of multiple sclerosis, during gatherings of members or in showrooms in collaboration with the Association, as well as in the National Institute of Rehabilitation (E. K. A.). Initially, people were informed about the nature of the study and asked for their voluntary participation. When the participants agreed and their oral content has received, their anonymity was ensured. The demographic were first completed and then the researcher read the instructions of the questionnaires. The researcher herself read and filled out the questions only when the participants showed some weakness in completing the questions themselves. There was no time limit, but usually the required time for the completion of each questionnaire is 20-30 minutes. After the completion of the questionnaires the researcher pleased the participants for participation and cooperation.
Measurements
Two questionnaires are used in the survey. The first relates to anxiety symptoms and the second to the symptoms of depression.
a) Self-assessment questionnaire of symptoms of anxiety
The Taylor Manifest Anxiety Scale questionnaire [16] (TMAS) measures the self-esteem of the person for symptoms of anxiety or stress which may be experiencing. The questionnaire contains 50 questions in which the person is asked to answer by selecting the "right" or "wrong" answer, depending on what the person feels at that time or period of time. The sum of the "right answer" is the rating of the questionnaire, i.e. the rating can range from 0 to 50.
The TMAS have a good split-half reliability (0.92) and internal consistency (0.92). It also shows high test-retest reliability (intervals of 3 weeks up to 19 months), with its respective indicators ranging between 0.82 and 0.89 [16].
b) Questionnaire of Self-evaluated depressive symptomatology (QD2)
The Questionnaire of Self-evaluated depressive symptomatology (QD2) [17] includes 52 questions which the person is required to respond with "true" or "false". These questions refer to the feelings and believe that the person feels at this particular time or period. The sum of the "true answer" is the rating of the questionnaire, which can range from 0-52.
The QD2 is the Greek version of the questionnaire of selfevaluated depressive symptomatology. The prototype was constructed in France after analysis of the content of questions of 4 most well-known depression questionnaires: the Hopkins Symptoms Check List, the French version of the Beck Depression Inventory, the scale D of M. M. P. I. and the scale D.
The coefficient of uniformity Φ in queries exceeds the materiality threshold .01, except two questions to which the index significance is .05. For checking the reliability of the division method and came up with a pointer r>.90. The assessment of validity gave satisfactory results (Bravais-Pearson coefficient r=.85, between QD2 & Zung). The correlation between the degree of the scale and extent of the clinical examination of depression is r=.30. The factor analysis of the Greek version (QD2) was studied in adult population (students and elderly), gave satisfactory results and confirmed the results of previous studies [18].
Previous studies in Greece have provided satisfactory evidence for the instruments’ psychometric characteristics of QD2 (depression) and TMAS (anxiety) questionnaires [18,19]. Consequently, in the series of statistical analyses that performed in order to investigate the hypotheses of this study, the participants’ total scores on depression and anxiety questionnaires were used.
The data obtained from the survey were studied and analyzed through the Statistical program Package of Social Sciences-v.20 (S. P. S. S.), mainly in relation to the two key variables of the present investigation, i.e. the symptoms of anxiety and depression that a person believes she is experiencing, but also with some demographics characteristics.
Results
Regarding the demographic data, from the 37 people of the sample, 16 (43.2%) were single, 18 (48.6%) married, 2 (5.4%) divorced or separated and one woman (2.7%) was widow. As far as their educational level, 3 people (8.1%) reported that they had finished primary school, 1 person (2.7%) had finished secondary school, 10 people (27%) had finished high school and 23 people (62.2%) had received higher education.
Additionally, from the 37 participants, 17 people (45.9%) live with their spouse, 8 people (21.6%) reside with their parents, 6 people (16.2%) cohabiting with another person, 5 people (13.5%) live by themselves, and one person (2.7%) resides with her child. From the total of 37 individuals, 19 individuals (51.4%) declare that they have no children, 14 people (37.8%) have one child, and 3 people (8.1%) have two children, while a person (2.7%) has three children. Only one person (2.7%) has a child with special needs.
Most women (10), 27% had received a diagnosis of multiple sclerosis in the first year of the survey while 7 women (18.9%) had already received the diagnosis 10-12 years prior to the study.
Furthermore, 31 women (83.8%) of the sample refer to medical services to deal with their disease, 22 women (59.5%) request support from multiple sclerosis associations and 6 women (16.2%) request support by the State Agencies.
Finally, 11 people (29.7%) used aids in ADL, while 26 people (70.3%) were not using. From those who required assistance with mobilizing, 4 women (10.8%) were mobilizing using a wheelchair and 6 women (16.2%) were using a walking aid (i.e. walking stick) for their daily indoor and outdoor transportation.
Regarding the results of the study, the average number of symptoms of anxiety is 17,83 with a standard deviation of 10, 55 and the average number of the symptoms of depressive symptomatology is 14,78 with a standard deviation of 12,85.
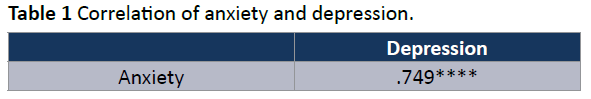
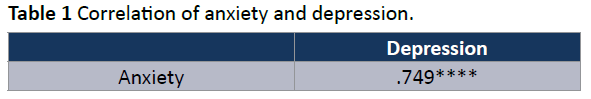
The correlation between depression and anxiety was studied through the use of Pearson. The research findings suggest that there is a positive and statistically significant correlation between depression and anxiety (r=.749, p<.0001). As the anxiety level increases so increases the level of depression or as the level of depression increases so increases the level of anxiety experienced person (Table 1).
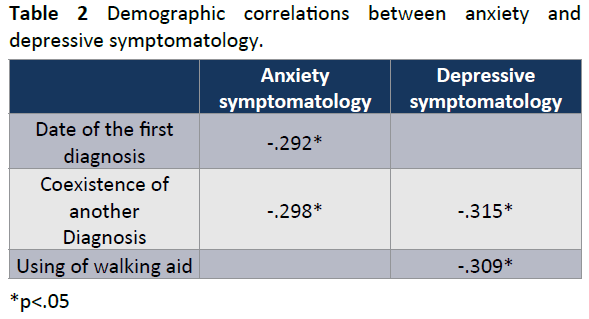
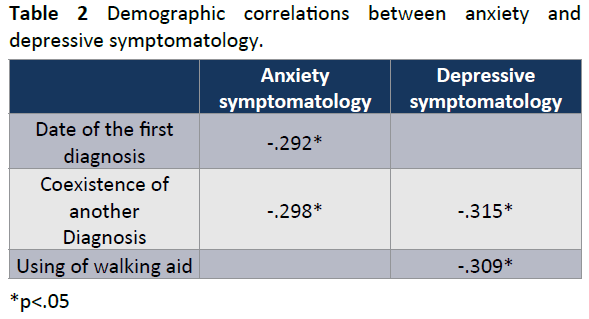
The results by analyzing Spearman, concerning the relationship of depression and anxiety with some variables such as date of the diagnosis, coexistence and other diagnosis and use device during ambulation, are listed in Table 2.
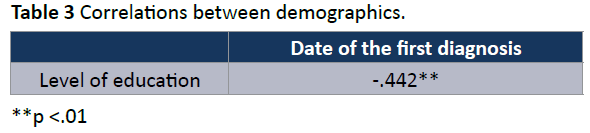
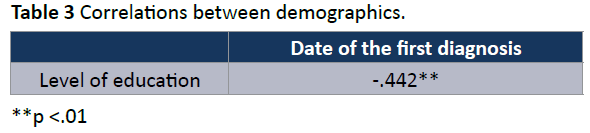
The results with the Spearman analysis concerning the relationship between level of education that had received the asked when was the diagnosis are listed in Table 3.
Discussion
The survey results confirm our assumptions. The correlation of the level of depressive symptomatology and the symptoms of anxiety in women with multiple sclerosis is positive and statistically very significant. As IE stress level increases, so increases the depressive symptomatology and vice versa.
In accordance with our results are the results obtained from other studies which mention the relationship between the measures of anxiety and depression [20,21], and the interaction between stress and cognitive schemata related with the depression of individuals with multiple sclerosis [22]. Furthermore, our results are in congruence with the results of Jopson and Moss- Morris [23] study that confirms that the facets of disease representations are related to depression. Data from another study, between others, demonstrated that people with multiple sclerosis who also reported cognitive problems are most likely to report problems with depression than the younger ones without cognitive problems [24].
The results from the correlation of the date of the first diagnosis and the symptoms of anxiety (Table 2) showed the longest the time from the diagnosis of the disease, the fewer the symptoms of anxiety experienced from the women with multiple sclerosis. In an attempt to interpret this result would suppose that as time passes, the women with multiple sclerosis accept and become familiar with the diagnosis of disease and therefore experience less anxiety.
The results obtained from the correlation of the coexistence of another diagnosis and the anxiety and depressive symptomatology, were negative and statistically significant. This finding suggests that when another diagnosis coexists, anxiety and depressive symptomatology are increasing (Table 2).
Another correlation studied between depressive symptomatology and the use of a walking aid from the women with multiple sclerosis. The results are unexpected because they showed us that in cases where there was use of wheelchair assistance, the depression decreased. To explain this finding one should understand that the relevancy is not between depression and the use of a device, but between depression and the underlying disabilities that lead the person to use this device. So, the more serious the underlying disabilities are, as indicated by the device used, the fewer the symptoms a person is experiencing. This finding is unexpected and requires further interpretation (Table 2). A possible interpretation is that the coexistence of a serious disability does not help the denial and failure to deal with the problem, therefore the person enters in the process of reconciliation and acceptance of the situation. This acceptance of the problem appears to reduce the symptoms of depression.
The need of assistive devices in persons with multiple sclerosis [25], the meaning that the assistive devices have in the lives of persons with multiple sclerosis [26], the types of assistive devices they need [27] as well as the annual cost of them [28] are reported as important in the articles. However, there is no data that concerning with the depressive symptomatology and the use of assistive devices in persons with multiple sclerosis.
Finally, a stronger correlation emerged from the relationship between level of education and years of diagnosis. For example, in women whose educational level was higher the disease had been diagnosed earlier than in those women whose educational level was lower. In an attempt to interpret this result we would hypothesize that women with high educational level are more sensitized to health issues and access earlier the special services for their dysfunction (Table 3).
This research has some limitations. In principle, the questionnaires that were used have not been studied in Greek population with multiple sclerosis. On the other hand, our ability to interpret some of the results decreases as it was not included in the study a similar group of people without multiple sclerosis with which we could make comparisons. Furthermore, the sample was neither random nor representative and does not consist of people of both sexes. We must also take into account the constraints of the survey and the fact that the results were obtained through correlations, which do not generally allow conclusions for causal relationship. Finally, the people who participated in the study were not diagnosed as having depression, but as having depressive symptomatology, therefore our conclusions refer primarily to depressive symptomatology and not to clinical depression.
Conclusions
Depressive symptomatology and anxiety have a strong relationship in women with multiple sclerosis. The occupational therapy and others health allied professions should direct their person-centered programs towards this goal, in order to help patients to cope with their disease more optimistic and to affect as little as possible their quality of life. More research is needed to fully understand the rehabilitation programs’ effectiveness and more specifically the occupational therapy’s effectiveness and the interventions involving physical, psychological, and functional training in people with multiple sclerosis. In the present study, the rules of designing and conducting a scientific investigation and documentation of its results were followed as closely as possible. Nevertheless, the results of this investigation should be confirmed by other studies, with more people and more statistical analyses.
Acknowledgments
The authors would like to thank the Association of persons with Multiple Sclerosis in Athens and especially Ms. T. Galiatsatou, Ms. M. Morozini, the National Foundation of Rehabilitation in Athens, and all the people who participated in this research.
6534
References
- Burks JS, Johnson KP (2000) Multiple sclerosis: Diagnosis, medical management, and rehabilitation. Demos Medical, New York
- José Sá M (2008) Psychological aspects of multiple sclerosis. ClinNeurolNeurosurg 110: 868-877
- Siegert RJ, Abernethy DA (2005) Depression in multiple sclerosis: a review. J NeurolNeurosurg Psychiatry 76: 469-475
- McGuigan C, Hutchinson M (2006) Unrecognised symptoms of depression in a community-based population with multiple sclerosis. J Neurol 253: 219-223
- McCabe MP (2005) Mood and self-esteem of persons with multiple sclerosis following an exacerbation. J Psychosom Res 59: 161-166
- Lobentanz IS, Asenbaum S, Vass K, Sauter C, Klösch G, et al. (2004) Factors influencing quality of life in multiple sclerosis patients: disability, depressive mood, fatigue and sleep quality. ActaNeurolScand 110: 6-13
- Rabinowitz AR, Arnett PA (2009) A longitudinal analysis of cognitive dysfunction, coping, and depression in multiple sclerosis. Neuropsychology 23: 581-591
- Beiske AG, Svensson E, Sandanger I, Czujko B, Pedersen ED, et al. (2008) Depression and anxiety amongst multiple sclerosis patients. Eur J Neurol 15: 239-245
- Korostil M, Feinstein A (2007) Anxiety disorders and their clinical correlates in multiple sclerosis patients. MultScler 13: 67-72
- Feinstein A, O'Connor P, Gray T, Feinstein K (1999) The effects of anxiety on psychiatric morbidity in patients with multiple sclerosis. MultScler 5: 323-326
- McCabew MP, De Judicibus M (2005) The effects of economic disadvantage on psychological well-being and quality of life among people with multiple sclerosis. J Health Psychol 10: 163-173
- Uguz F, Akpinar Z, Ozkan I, Tokgoz S (2008) Mood and anxiety disorders in patients with multiple sclerosis. Int J Psychiatry ClinPract 12: 19-24
- Feinstein A (2002) An examination of suicidal intent in patients with multiple sclerosis. Neurology 59: 674-678
- Feinstein A, du Boulay G, Ron MA (1992) Psychotic illness in multiple sclerosis. A clinical and magnetic resonance imaging study. Br J Psychiatry 161: 680-685
- Büchi S, Buddeberg C, Sieber M (1989) [The significance of somatic and psychosocial factors for coping with illness by patients with multiple sclerosis]. Nervenarzt 60: 641-646
- Taylor JA (1953) A personality scale of manifest anxiety. J AbnormPsychol 48: 285-290
- Pichot P, Boyer P, Pull CB, Rein W, Simon M, et al. (1984) Un Questionnaire D’Auto-évaluation de la symptomatologieDépressive, le Questionnaire QD2. Rev PsycholAppl 34: 220-250
- Tzonichaki I (1994) La dépressionet le “locus of control” chez les personnesâgéesGrecques. Thèse de doctorat. Université Paris- X-Nanterre, France
- Karkani X (2000) Symptomatology of anxiety and satisfaction of life in elderly. Department of Occupational Therapy, Technological Educational Institution of Athens, Greece
- Beiske AG, Svensson E, Sandanger I, Czujko B, Pedersen ED, et al. (2008) Depression and anxiety amongst multiple sclerosis patients. Eur J Neurol 15: 239-245
- Janssens AC, van Doorn PA, de Boer JB, van der Meché FG, Passchier J, et al. (2003) Impact of recently diagnosed multiple sclerosis on quality of life, anxiety, depression and distress of patients and partners. ActaNeurolScand 108: 389-395
- Beeney J, Arnett PA (2008) Stress and memory bias interact to predict depression in multiple sclerosis. Neuropsychology 22: 118-126
- Jopson NM, Moss-Morris R (2003) The role of illness severity and illness representations in adjusting to multiple sclerosis. J Psychosom Res 54: 503-511
- Finlayson M, Shevil E, Cho CC (2009) Perceptions of cognitive symptoms among people aging with multiple sclerosis and their caregivers. Am J OccupTher 63: 151-159
- McLaughlin CM (1998) Community programs and resources for persons with multiple sclerosis. Phys Med RehabilClin N Am 9: 689-702
- Stolp-Smith KA, Carter JL, Rohe DE, Knowland DP 3rd (1997) Management of impairment, disability, and handicap due to multiple sclerosis. Mayo ClinProc 72: 1184-1196
- Finlayson M, Guglielmello L, Liefer K (2001) Describing and predicting the possession of assistive devices among persons with multiple sclerosis. Am J OccupTher 55: 545-551
- Whetten-Goldstein K, Sloan FA, Goldstein LB, Kulas ED (1998) A comprehensive assessment of the cost of multiple sclerosis in the United States. MultScler 4: 419-425