Keywords
Reproductive health; Contraceptive security; Knowledge; Attitude and practice; Family planning; Information; Education and communication
Abbreviations
CPR: Contraceptive Prevalence Rate; FP: Family Planning; IEC: Information, Education, Communication; KAP: Knowledge, Attitude and Practice; LAPMs: Long Acting and Permanent Methods; MDGs: Millennium Development Goals; RHCS: Reproductive Health Contraceptive Security
Introduction
Reproductive health contraceptive security exists when every person is able to choose, obtain, and use quality contraceptives and other essential reproductive health products whenever s/ he needs them [1]. Reproductive health contraceptive security emphasizes three important areas: Clients, Commodities and providers, and Sustainability (long term assurance). There is no contraceptive security if people fail to choose, obtain and use contraceptive methods they want, which has to address the needs of all people, including the poor and vulnerable groups. It occurs when users are able to make informed choices from a full range of methods and services of high quality at affordable price to address short and long term reproductive health needs [2].
Contraceptive Security is an integral component of the broad interventions required to ensure reproductive health and it has far reaching contribution to the improvement of health and reduction of poverty. It links with the MDGs in many ways. While access to family planning is not an explicit target, it plays crucial role in achieving MDG 4, 5 & 6. Family planning, also, has significant impact on MDG 1 through reduction in average family size and, thus, increasing per capita family income. Thus, access to contraceptives is a critical and cost-effective means of accentuating progresses towards the achievement of the MDGs [3,4].
At the heart of RHCS is the client utilization of appropriate family planning packages. This requires continuous strives to create demand and successful efforts to fulfill through cost-effective logistics system and service provision. As several actors are involved in provision of these services, securing uninterrupted supply of contraceptives is influenced by many factors. RHCS is affected by contextual factors in the broader environment such as socioeconomic conditions, political and religious concerns, competing health priorities, and reform in health sector. Within these contexts, commitment and coordination between stakeholders is very important in adopting supportive policies, and mobilization and allocation of resources [4,5].
RHCS is a factor of efficiency of the logistics system. While logistics system is concerned with ensuring that right quantities of the right contraceptive methods to be available to users with acceptable quality at right cost, inefficiency often resulted in low method mix at service delivery points, which in turn is correlated with low contraceptive acceptance and utilization [6].
In many developing countries, facility based services remain the backbone for the provision of family planning and other reproductive health services [7,8]. This heightens the demand for competent healthcare providers in addressing the needs of their clients, and convenience of the service delivery environments [9]. Experience of several countries, however, shows otherwise.
Methods
Literature search
Studies were identified through searches of the following electronic publication databases: PubMed Central, Genesis Library, Bio Med Central, Bioline International, Lancet series, doaj, EJHD, and Google scholar for gray articles. The key and free text searches include: ‘Contraception’, Access to contraception’, ‘Contraceptive security’, ‘Determinants of contraceptive use’, ‘Determinants of family planning’, ‘Reproductive Health Commodity Security’, and ‘Developing countries’.
Inclusion criteria and exclusion criteria
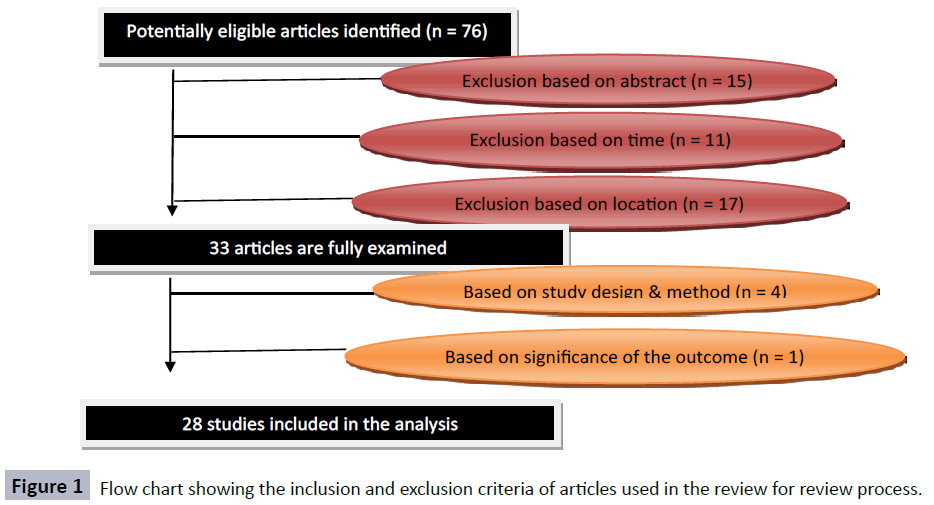
Set of inclusion and exclusion criteria were used to appraise the articles used for analysis. Four parameters were used to define eligibility of the articles: location of the study, time of the study, the study design used, and significance of the outcomes. For a study to be included in the review, it should be conducted in developing countries during and after the 1990s using scientifically plausible designs, and should account for sufficient control of bias (Figure 1). The results of the study should be statistically significant and has to correlate to one of the five determinants of RHCS considered in the objective.
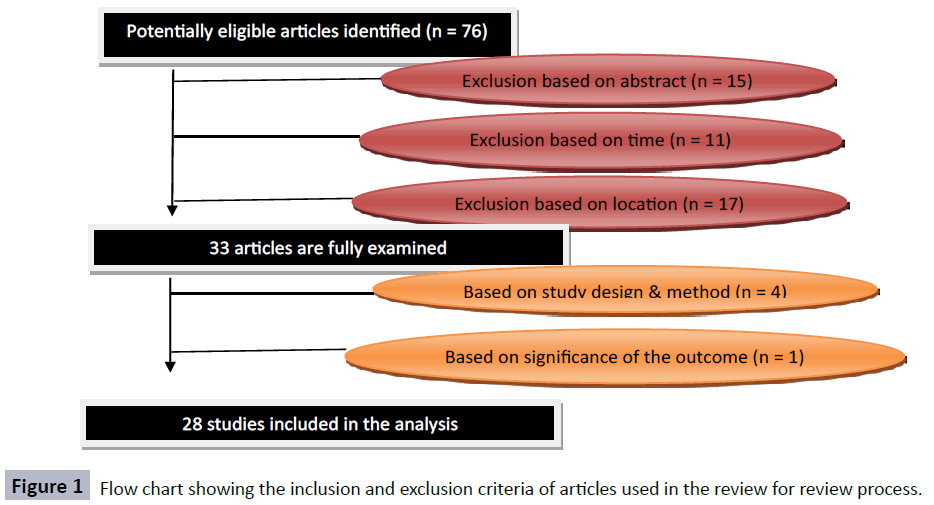
Figure 1: Flow chart showing the inclusion and exclusion criteria of articles used in the review for review process.
Data extraction and evidence rating
Findings of individual articles are reviewed independently and presented to assess cross cutting factors that affect access, choice and utilization of Reproductive Health commodities. Only statistically significant results are assigned to one of the five determinants of RHCS developed. Then, the results are compared to the local context regarding contraceptive security to establish ground factors within the framework of the clients and the healthcare delivery system.
Results and Discussion
Reproductive health contraceptive security exists when users are able to make informed choices from a full range of methods and services of high quality at affordable price to address short and long term reproductive health needs [2]. Contraceptive method choice and utilization, often, is based on the couple years of protection, perceived and actual side effects, effectiveness of methods in providing protection, the level of expertise and competence required to use the methods, the cost of the methods, the knowledge, attitude and belief towards the method, the level of information regarding contraception, education about family planning and the level of communication between the health care providers and clients. These factors can be clustered around: Socioeconomic factors related to clients, The Knowledge, Attitude and Practice of Clients, Information, Education and Communication, Logistics Factors, and Service Delivery Point factors such as provider and health delivery environments.
Socioeconomic factors of clients
Equity in health is the most important factor that affects access to and utilization of available health care services [10]. Evidence from several countries show that there exist differences in contraceptive behavior by variations in the social, cultural, economic, and educational status, as well as place of residence [11].
Inequalities in contraceptive behavior by physical capital are larger than the public and human capital dimensions of socioeconomic position [12] as there exists persistent differentials in access to and use of modern contraceptives by wealth quintile, especially in sub-Saharan Africa [13-15]. Women in the richest wealth quintile are more likely than those in the poorest quintile to practice long-term contraception, and poorer women use contraception much less than wealthier women. Among 13 African countries, namely: Ethiopia, Madagascar, Mozambique, Namibia, Zambia, Kenya, Senegal, Uganda, Mozambique, Malawi, and the United Republic of Tanzania, wealth-related inequality in the met need for contraception to limit future births was highest in Ethiopia and lowest in Ghana and Malawi [16].
The use and nonuse of contraception shows huge variation by place of residence in the country, age and parity, marital status and partner approval, the level of education attained, need for larger family size and other community related factors such as service availability and accessibility in specific communities [11,17,18].
Contraceptive behavior is influenced by deep routed social, cultural and economic factors [19]. Assessment of contraceptive behavior in Rwanda and Zambia shows that lack of female decision making, poor economic resources and desires for large families as the most important factors resulting in low contraceptive use, despite their high level of knowledge [20].
In Ethiopia, Contraceptive behavior is highly associated with women’s educational and occupational status, and spousal discussion about family planning. Women’s knowledge and practice is influenced by socio-cultural norms such as male/ husband dominance and opposition to contraception, low social status of women, and lack of formal education, which prevents change in the patterns of contraceptive knowledge and use. In addition, religious belief and wanting more children are reasons for nonuse of modern contraception [21-23].
Knowledge, attitude and practice of clients
The Knowledge, attitude and practice of clients has remained to strongly influence health seeking behavior and health care utilization [24]. Low KAP is strongly associated with low acceptance and utilization of reproductive health contraceptives [25]. Evidences of many countries in the developing world show that nonuse of contraceptives are due to lack of factual information and knowledge about contraceptives [17,18,23], as well as fears of actual and perceived side effects [26,27], strong misconceptions about contraceptives and negative attitudes towards contraceptives [9,28].
Knowledge of contraceptive is often associated with better utilization of reproductive health services. However, the level of knowledge of individuals is not always a good predictor of contraceptive behavior [29]. In Rwanda and Zambia, there is low prevalence of contraception despite very high knowledge (90- 98.8 %) regarding family planning methods and services [20].
The practice of family planning in many countries is highly influenced by the attitudes and beliefs held by individuals and communities. In many developing countries, negative attitude towards contraception in general and certain methods specifically have often resulted into nonuse of contraception. For instance, religious beliefs that long term use of pills result in sterility is commonly associated with discontinuation of methods [26]. Similarly, in Ethiopia, there is lower acceptance and utilization of Long Acting and Permanent Methods (LAPMs) due to negative attitude towards them [30].
Information, education and communication
Provision of information about family planning methods, sexually transmitted disease risk factors, and choice of contraceptive method to family planning clients is important intervention that empowers users in making informed decision regarding their contraceptive behavior. Exposure to family planning information is associated with increased contraceptive practice. Community’s exposure to family planning media messages on the radio increases the use of long-term and permanent methods [11,31], and results in low unmet need for family planning [23].
A randomized control trial to evaluate the role of information in contraceptive method choice shows a statistically significant increase in making decision regarding contraceptive method to use among the intervention groups provided with information and contraceptive choice over the controls, who only have received recommended method by physicians [32].
Logistics factors
The purpose of a logistics system is to ensure that the right goods, in the right quantities, in the right condition, are delivered to the right place, at the right time, for the right cost [6,12]. Unavailability of methods of choice in facilities closest to users, long distances to family planning clinics, and high cost of methods contribute to the nonuse of contraception. In addition, inconsistent, sporadic availability, and poor method mix are limiting factors to the choice of methods by clients in need of contraceptives, and the availability of different contraceptive methods is known to influence contraceptive acceptance [9]. Furthermore, client preference of methods is highly influenced by the absence of side effects, convenience of the methods, and the effectiveness in preventing pregnancy [27].
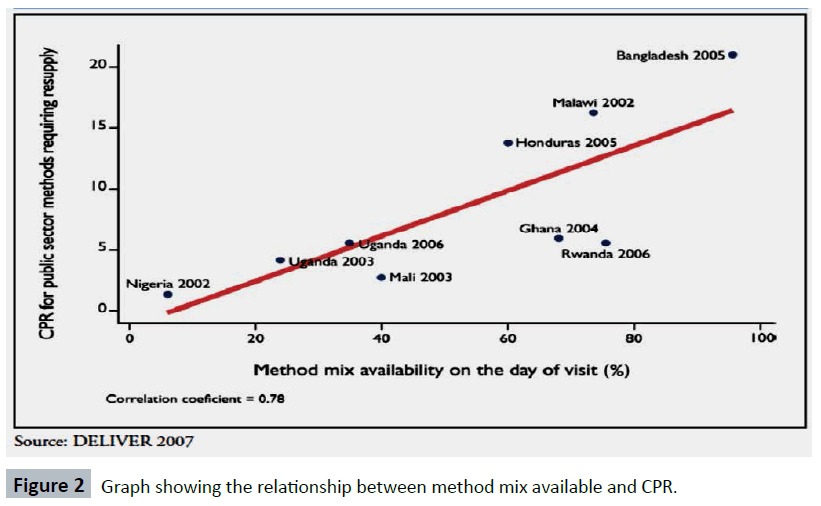
Method mix is one of important factors for short and long term Contraceptive Security. While most contraceptive security efforts have focused on forecasting, procurement, distribution, and advertising for “resupply” methods of family planning of condoms, pills, and injectables, ensuring Contraceptive Security will be much challenging without the Long Acting and Permanent Methods (LAPMs). The LAPMs are widely used when available and accessible, are cost effective compared to the resupply methods in providing longer couple year of protection, and contribute to a tall in saving lives and improving health [33] Figure 2 below shows the relationship between method mix and CPR.
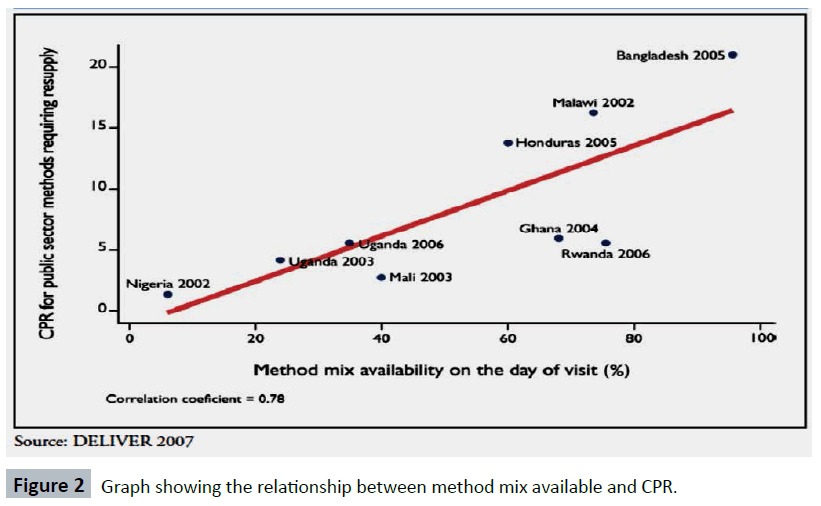
Figure 2: Graph showing the relationship between method mix available and CPR.
High unmet need for contraception is associated with contraceptive insecurity [22]. For this reason, meaningful improvements in the logistics system to ensure continuous availability of all contraceptive methods significantly improve contraceptive acceptance and utilization [31,34].
Healthcare system factors
As the most populous cohorts in history entered and moved through their reproductive years, and as other public health concerns competed for scarce resources, family planning program managers recognized that service delivery challenges to meeting the need for contraception is growing [9], where interrelation and communication between clients and healthcare providers, and the environment within which service is delivered strongly influence acceptance and use of appropriate methods.
Provider related factor
Service providers play key role in supporting their clients to make informed choice. This requires technical competence of service providers in properly communicating and recommending appropriate procedure and in investigating the indication and contraindication of various methods [27,35].
Healthcare providers’ recommendations, however, are often infiltrated with bias. The choice of method is highly affected by provider bias, where providers recommend method for spacing and terminating child bearing, and fewer providers are willing to consider client’s method preference. Similarly, medical barrier due to provider-imposed eligibility restrictions on specific methods occurs. These restrictions are often observed based on age of client for combined pills, injectables and sterilization; parity for injectables and sterilization; marital status for IUD and female sterilization; spousal consent for female sterilization [35,36]. Providers demonstrate significant bias towards providing Emergency Contraceptives to certain categories of clients, including adolescents, unmarried females and women who have had multiple sex partners [36].
Assessment of the healthcare providers’ related reasons for restriction of family planning services shows that lack of knowledge about contraceptives, negative provider attitudes due to fears, myths, and health and safety concerns related to certain contraceptive methods, and self-initiated denial or restrictions to provide all or some methods based on age [9,26,31]. Such kind of self-imposed restrictions not only affects the contraceptive behavior but also violates reproductive health rights of women. Contraceptive acceptance and utilization is enhanced through healthcare providers’ effective communication with its clients. This is evidenced when poor level of training of providers and ineffective conveyance of relevant information to clients result in low Contraceptive prevalence Rate [17]. Healthcare providers’ attitude towards family planning services is another important determinant for access. In Bangladesh, service providers’ share traditional beliefs that continued use of oral pills may result in infertility [26]. As contraceptive technology is changing over years, service providers need to receive comprehensive training of available methods [31].
Service delivery environments
Various health systems related factors take part in facilitating or hindering the provision and utilization of contraceptives. Infrastructures with limited space to provide both auditory and visual privacy during client consultations, lack of appropriate equipment and educational materials are perceived barriers to provision of family planning services to clients. In addition, poor service quality, long waiting hours, limited number of qualified personnel, and high staff turnover, as well as policy restrictions added to constraints on funding for community sensitization, outreach, and supportive supervision contribute to low contraceptive prevalence use significantly [9,20,22,23].
Integration of family planning services with other health care services promotes contraceptive acceptance. In facilities where both family planning and other health care services are provided together and where larger range of methods are available and offered, there is a significant increase in contraceptive acceptance [37-39]. For this reason, improving counseling, training health care providers, increasing contraceptive choices, and promoting access to contraception may sufficiently challenge low use of contraception and enhance easier acceptance of contraceptive methods.
Limitation of this study
This review has some limitation. The first and the most important limitation is that only clients’ and healthcare systems’ perspectives are considered due to myriad factors: policy, finance, commitment, capacity, clients, service delivery environments, and providers, involved and did not cover all the factors affecting RHCS. As many factors are involved in ensuring RHCS, the effect of one factor may exacerbate or underscore the outcome of the other factor on RHCS. Unless the effect of all factors are identified and approximated, accuracy in judging the impact of each factor may be imprecise. The other limitation of this review is that there are scant researches conducted to assess the impact of healthcare system factors on RHCS, especially in Ethiopia. Due to this, it has been difficult to judge the true extent of these factors in our country’s setup.
Conclusion
RHCS is an integral component of the broad health intervention package and it exists when users are able to make informed choices from a full range of methods and services of high quality at affordable price to address short and long term reproductive health needs. The determinants of RHCS range from client factors such as socioeconomic status and access to Reproductive Health services, the KAP regarding contraception. Contraceptive information communicated through mass media, higher level of education and better contraceptive communication in community contribute to better contraceptive acceptance and utilization. The absence of side effects and convenience of contraceptive methods are among important factors that affect method choice. Provider’s attitude towards the provision of family planning services also plays crucial role. User friendly service environments create better provider-client communication and better contraceptive acceptance, utilization and behavior. When Family Planning services are integrated with other healthcare services, especially maternal health services, better contraceptive acceptance occurs.
8764
References
- Office of Population Affairs (2010) Reproductive Health and Healthy People 2020 Healthy People.
- Contraceptive Security Team. Contraceptive Security – Ready Lessons: Overview. US Agency for International Development (USAID). Washington DC, United States.
- Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, et al. (2006) Family planning: the unfinished agenda.Lancet 368: 1810-1827.
- Middleberg MI (2004) Promoting Reproductive Security in Developing Countries. Kluwer Academic Publishers, New York, United States.
- Tien M, Sylvia N, Ugochukwu A, Echendu A, Uzo E, Azubike N (2009) Nigeria: Reproductive Health Commodity Security Situation Analysis. Arlington, Va.: USAID | DELIVER PROJECT, Task Order 1.
- USAID | DELIVER PROJECT, Task Order 1 (2011) The Logistics Handbook: A Practical Guide for the Supply Chain Management of Health Commodities (2ndedn.). Arlington, Va.: USAID | DELIVER PROJECT, Task Order 1.
- Sharma S, Dayaratna V (2005) Creating conditions for greater private sector participation in achieving contraceptive security.Health Policy 71: 347-357.
- Sharma S, Almasarweh I (2004) Family Planning Market Segmentation in Jordan: An Analysis of the Family Planning Market in Jordan to Develop an Effective and Evidence-Based Strategic Plan for Attaining Contraceptive Security. The Centre for Development and Population Activities (CEDPA).
- Nalwadda G, Mirembe F, Tumwesigye NM, Byamugisha J, Faxelid E (2011) Constraints and prospects for contraceptive service provision to young people in Uganda: providers’ perspectives. Health Serv Res 11:220.
- Wirth M, Sacks E, Delamonica E, Storeygard A, Minujin A, et al. (2008) “Delivering” on theMDGs?: Equity and Maternal Health in Ghana, Ethiopia and Kenya. East Afr J Public Health 5: 133-141.
- Magadi MA, Curtis SL (2003) Trends and determinants of contraceptive method choice in Kenya.Stud FamPlann 34: 149-159.
- González C, Houweling TAJ, Marmot MG, Brunner EJ (2010) Comparison of physical, public and human assets as determinants of socioeconomic inequalities in contraceptive use in Colombia - moving beyond the household wealth index. Int J Equity Health 9:10.
- Shah IH, Chandra-Mouli V (2007) Inequity and unwanted fertility in developing countries.Bull World Health Organ 85: 86.
- Gillespie D, Ahmed S, Tsui A, Radloff S (2007) Unwanted fertility among the poor: an inequity?Bull World Health Organ 85: 100-107.
- Rahman M, Haque SE, Mostofa MG, Tarivonda L, Shuaib M (2011) Wealth inequality and utilization of reproductive health services in th e Republic of Vanuatu: insights from the multiple indicator cluster survey, 2007. Int J Equity Health 10:58.
- Creanga AA, Gillespie D, Karklins S, Tsui AO (2011) Low use of contraception among poor women in Africa: an equity issue.Bull World Health Organ 89: 258-266.
- Omo-Aghoja LO, Omo-Aghoja VW, Aghoja CO, Okonofua FE, Aghedo O, et al. (2009) Factors associated with the knowledge, practice and perceptions of contraception in rural southern Nigeria.Ghana Med J 43: 115-121.
- Moronkola OA, Ojediran MM, Amosu A (2006) Reproductive health knowledge, beliefs and determinants of contraceptives use among women attending family planning clinics in Ibadan, Nigeria. Afr Health Sci6: 155-159.
- Giusti C, Vignoli D (2006) Determinants of contraceptive use in Egypt: a multilevel approach. Stat Methods Appt15: 89-106.
- Grabbe K, Stephenson R, Vwalika B, Ahmed Y, Vwalika C, et al. (2009) Knowledge, use, and concerns about contraceptive methods among sero-discordant couples in Rwanda and Zambia.J Womens Health (Larchmt) 18: 1449-1456.
- Beekle AT, McCabe C (2006) Awareness and determinants of family planning practice in Jimma, Ethiopia.IntNurs Rev 53: 269-276.
- Mekonnen W, Worku A (2011) Determinants of low family planning use and high unmet need in Butajira District, South Central Ethiopia. Reprod Health 8:37.
- Hailemariam A, Haddis F (2011) Factors affecting unmet need for family planning in southern nations, nationalities and peoples region, ethiopia.Ethiop J Health Sci 21: 77-89.
- Glanz K, Rimer BC, Viswanath K (2008) Health Behavior and Health Education: Theory, Research, and Practice (4th Edition), Jossey-Bass, San Francisco, United States.
- Ferreira AL, Souza AI, Lima RA, Braga C (2010) Choices on contraceptive methods in post-abortion family planning clinic in the northeast Brazil.Reprod Health 7: 5.
- Ullah ANZ, Humble ME (2006) Determinants of oral contraceptive pill use and its discontinuation among rural women in Bangladesh. Reprod Med Biol5: 111-121.
- Credé S, Hoke T, Constant D, Green MS, Moodley J, et al. (2012) Factors impacting knowledge and use of long acting and permanent contraceptive methods by postpartum HIV positive and negative women in Cape Town, South Africa: a cross-sectional study. Public Health 12:197.
- Cleland JG, Ndugwa RP, Zulu EM (2011) Family planning in sub-Saharan Africa: progress or stagnation?Bull World Health Organ 89: 137-143.
- Kayembe PK, Fatuma AB, Mapatano MA, Mambu T (2006) Prevalence and determinants of the use of modern contraceptive methods in Kinshasa, Democratic Republic of Congo.Contraception 74: 400-406.
- Alemayehu M, Belachew T, Tilahun T (2012) Factors associated with utilization of long acting and permanent contraceptive methods among married women of reproductive age in Mekelle town, Tigray region, north Ethiopia. BMC Pregnancy Childbirth 12:6.
- Chen S, Guilkey DK (2003) Determinants of contraceptive method choice in rural Tanzania between 1991 and 1999.Stud FamPlann 34: 263-276.
- Lazcano Ponce EC, Sloan NL, Winikoff B, Langer A, Coggins C, et al. (2000) The power of information and contraceptive choice in a family planning setting in Mexico.Sex Transm Infect 76: 277-281.
- Wickstrom J, Jacobstein R (2011) Contraceptive security: incomplete without long-acting and permanent methods of family planning.Stud FamPlann 42: 291-298.
- Prata N (2009) Making family planning accessible in resource-poor settings.Philos Trans R SocLond B BiolSci 364: 3093-3099.
- Askew I, Mensch B, Adewuyi A (1994) Indicators for measuring the quality of family planning services in Nigeria.Stud FamPlann 25: 268-283.
- Judge S, Peterman A, Keesbury J (2011) Provider determinants of emergency contraceptive counseling and provision in Kenya and Ethiopia.Contraception 83: 486-490.
- McDougall J, Fetters T, Clark KA, Rathavy T (2009) Determinants of contraceptive acceptance among Cambodian abortion patients.Stud FamPlann 40: 123-132.
- O’Brien M, Richey C (2010) Knowledge Networking for Family Planning: The Potential for Virtual Communities of Practice to Move Forward the Global Reproductive Health Agenda. KM&EL 2: 109-121.
- Mayhew SH, Lush L, Cleland J, Walt G (2000) Implementing the integration of component services for reproductive health.Stud FamPlann 31: 151-162