Research - (2022) Volume 13, Issue 4
Disciplinary screening of electroencephalography (EEG) referrals by neurologist ameliorates healthcare use economy
Mohammed Gomaa*
Department of Neurology, Fayoum University, Faiyum, Egypt
*Correspondence:
Mohammed Gomaa, Department of Neurology, Fayoum University,
Faiyum,
Egypt,
Email:
Received: 27-Mar-2022, Manuscript No. ipjnn-22-12691;
Editor assigned: 29-Mar-2022, Pre QC No. P-12691;
Reviewed: 19-Apr-2022, QC No. Q-12691;
Revised: 23-Apr-2022, Manuscript No. R-12691;
Published:
30-Apr-2022
Abstract
Background: Electroencephalogram (EEG) serves a vital role in
screening and diagnosing epileptic patients because it is a noninvasive
tool to reveal the aberrant cortical excitability underlying epilepsy.
To compare EEG results in adult neurophysiology units, Neurology
department, Fayoum university hospitals according to the specialty
of referring physicians. This retrospective survey included 1413
consecutive EEG referrals to exclude epilepsy. Epileptic patients
admitted for EEG repetition for follow-up concerns were eliminated.
Patients were classified into Four groups of EEG referrals. Group I
was referred directly by neurologists, group II by psychiatrists, group
III by neurosurgeons, and group IV was referred by physicians of
other specialties.
Results: Among group I, 493 EEG referrals (252 abnormal, 51.1%).
Group II, 134 EEG referrals (41 abnormal, 30.6%). Group III, 68 EEG
referrals (23abnormal, 33.8%). Lastly, 718 EEG referrals were among
group IV (181 abnormal, 25.2%). The p-value (0.0001) indicated a
significant difference among study groups. A higher percentage
of abnormal EEG results was noticed among neurologist referrals
relative to other groups.
Conclusion: Review of EEG referrals by neurologist leading to a
decrease in the number of normal EEG results and better stream
of diagnosis and management. Incorporating data from referral
reports with detailed history taking and provisional diagnosis is
recommended to decrease the number of improper EEG referrals
for non-epileptic patients by better using healthcare resources.
Keywords
Epilepsy; Electroencephalography; Referral.
Abbreviations
EEG: Electroencephalogram; IED: Interictal
Epileptiform Discharges.
Introduction
In combination with the increasingly outstanding array
of other diagnostic procedures developed over the past 30
years, the electroencephalogram (EEG) plays a vital role in
diagnosing and treating patients with seizure disorders. Its
key benefits are that it is a handy and non-invasive technique
to illustrate the physiological symptoms of aberrant cortical
excitability that emphasize epilepsy [1].
Border zone diseases encompass neurological illnesses
with psychiatric symptoms, signs, and disorders with
soft neurological aspects and substantial diagnostic and
therapeutic problems [2].
Non-epileptic paroxysmal abnormalities may present
clinically in the same way as epileptic seizures and should
be addressed in the differential diagnosis of epilepsy like
syncope, migraine, parasomnia, and other disorders [3].
EEG is also a useful diagnostic tool in psychiatric practice
if there is comorbidity between serious mental disease
and epilepsy. In addition, some acute and sub-acute
brain diseases may produce emotional or cognitive core
symptoms; lastly, their association with the classification
of psychiatric disorders [4].
Because of possibly occurring EEG limitations and
diagnostic errors, there will be a low yield of data available
that might be beneficial in treating people with seizure
disorders. It is vital to understand that a normal EEG does
not exclude epilepsy since roughly 10 percent of people with
epilepsy never display epileptiform discharges. Furthermore,
an abnormal EEG demonstrating interictal epileptiform
discharge (IED) does not indicate that a person has a seizure
disorder, as IED is seen in a small percentage of normal
subjects who never developed epilepsy. IED may also be
observed in individuals with neurological disorders that are
not complicated by epilepsy [1].
This research aimed to compare the EEG results in
adult neurophysiology units, the Neurology department,
Fayoum University hospitals according to the specialty of
referring physicians.
Methods
This retrospective study included (1413) de novo
patients with epilepsy and query epilepsy referred to the
adult neurophysiology unit, Neurology department,
Hospitals of Fayoum University, from November 1, 2017,
to the end of November 2020.
All de novo epileptic or query epileptic patients who
presented with single or recurrent provoked or unprovoked
seizures were included. Clinical diagnosis of new-onset
epilepsy when the physician was utilizing EEG to define
epilepsy or to help in selecting antiepileptic medication
was included in this study. While Patients with established
epilepsy referred for EEG repetition for treatment reasons
were omitted.
All patients were submitted to thorough history taking
using a standardized case report form which included:
demographic data: age, sex, residence, clinical presentation,
history of previous disorders and treatment, family history,
previous EEG request, and specialty of referring physician.
All EEGs were conducted utilizing (EEG-1200L, Nihon
Kohden Corporation, Japan) equipment with 20 channels
EEG system, standard montages, and the International
10/20 System. Hyperventilation and intermittent photic
stimulation activation methods were performed in all
cases. The EEGs were recorded by EEG technologists and
reviewed by a neurologist certified for EEG reading.
Data were collected from patients' files and classified
according to referring physicians into four groups: In the
first group, 493 patients were referred from neurologists;
In the second group, 134 patients were referred from
psychiatrists; In the third group, 68 patients were referred
from neurosurgeons; In the fourth group, 718 patients
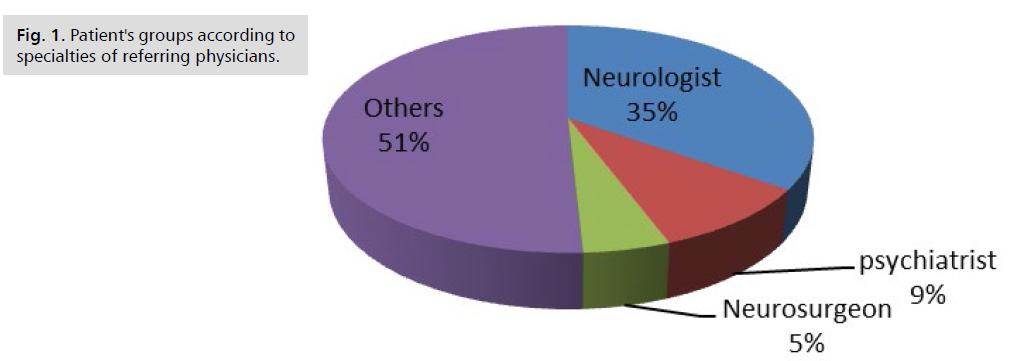
referred from physicians of other specialties. Fig. 1 represents patients' age ranging from 12 to 95 Years. Patients with inadequate collected data were cancelled
from this study.
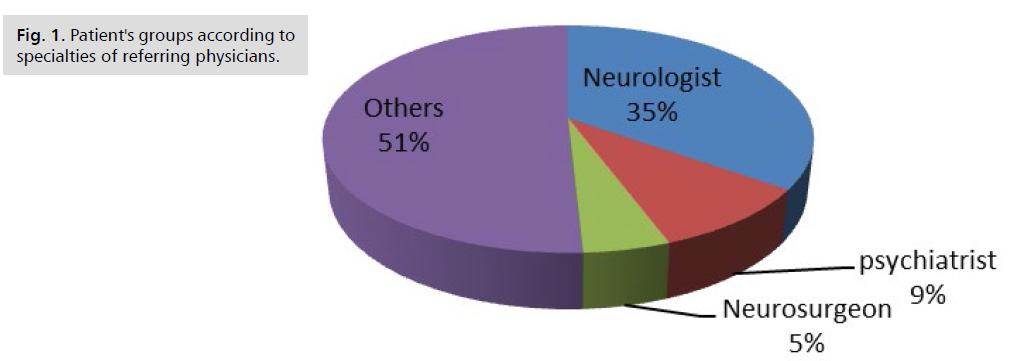
Fig 1: Patient's groups according to specialties of referring physicians.
EEG reports were classified into two groups. The first
group included EEG reports with aberrant epileptiform
activity, including spikes, sharp waves, spike-wave complexes,
polyspike-wave complexes, and paroxysmal rhythmic
frequencies. Also, non-epileptiform activity, including
localized and diffuse slowing included in this category. The
second category was normal EEG reports.
EEG data were gathered and encoded in Microsoft
Access, and data analysis was carried out on Windows
7 using SPSS software version 22.0 Armonk, NY, USA.
For qualitative data, a simple descriptive analysis was
done using numbers and percentages. Arithmetic means
were used to characterize quantitative data. To compare
qualitative categories such as sex, the Chi-square test was
utilized. The significant level of p 0.05 was deemed to be
the cut-off value.
Results
Patients varied in age from 12 to 95 years. There were
57.6 % females and 42.4 % men among the patients
(Tab. 1).
| Groups |
Number |
Female |
Male |
| Number |
% |
Number |
% |
| Neurology |
493 |
301 |
61% |
192 |
39% |
| Psychiatrist |
134 |
83 |
61.9% |
51 |
38.1% |
| Neurosurgeons |
68 |
23 |
33.8% |
45 |
66.2% |
| Other specialties |
718 |
407 |
56.6% |
311 |
43.4% |
| Total |
1413 |
814 |
57.6 |
599 |
42.4% |
Tab. 1. Number of EEG referrals according to specialties with a gender distribution.
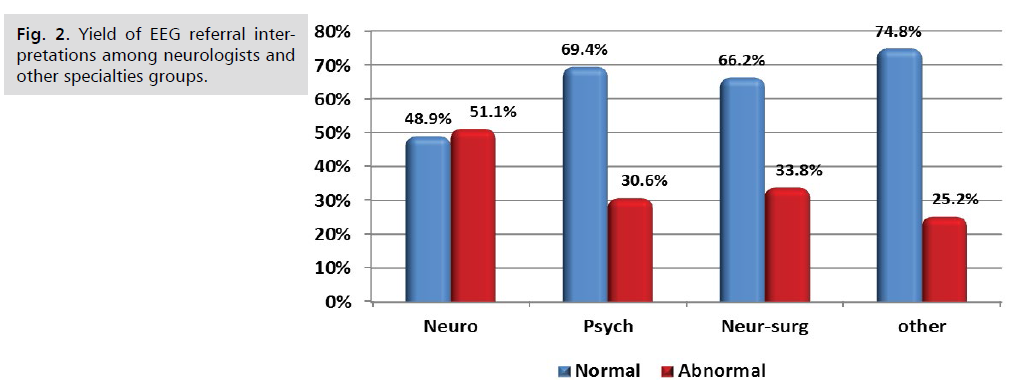
This study revealed a statistically significant difference
(p-value <0.05) between study groups regarding EEG
referral interpretation results. A higher percentage of
abnormal EEG was noticed among neurologist referrals
relative to other groups (Tab. 2 and Fig. 2).
| Groups |
Normal |
Abnormal |
Total |
P- value |
| Number |
% |
Number |
% |
| Neurologists |
241 |
48.90% |
252 |
51.10% |
493 |
0.001 |
| Psychiatrists |
93 |
69.40% |
41 |
30.60% |
134 |
| Neurosurgeons |
45 |
66.20% |
23 |
33.80% |
68 |
0.007 |
| Other specialties |
537 |
74.80% |
181 |
25.20% |
718 |
0.001 |
Tab. 2. EEG results from referral among studied groups.
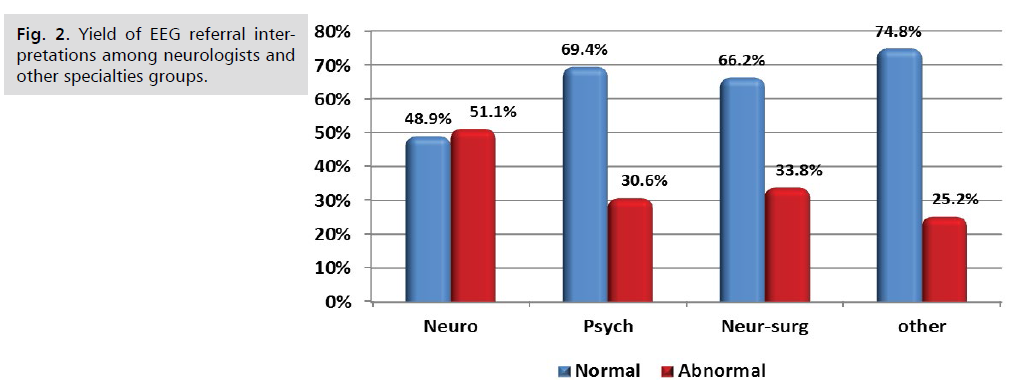
Fig 2: Yield of EEG referral interpretations among neurologists and other specialties groups.
Discussion
Our study revealed a statistically significant difference
(p-value <0.05) between group I patients referred by
neurologist and other groups refereed by a psychiatrist
(group II), neurosurgeons (group III), and those referred
by physicians of other specialties (group IV) with a higher
percentage of abnormal EEG reports were noticed among
neurologist referral. These results agreed with Gurbani
NS, et al. [5], who found that EEG referrals reviewed by a
neurologist revealed more EEGs with epileptiform activity
when EEGs were recommended directly by a neurologist.
This result emphasizes that the expertise in epilepsy of a
neurologist has a key role in establishing the right EEG
referrals compared to other referrals from different
specialties physicians.
Our investigation indicated a high output of normal
EEGs referenced directly by non-neurologists in groups II,
III, and IV (69.4%, 66.2%, and 74.8%, respectively). The
findings of this investigation come in accord with those of
studies reported from other community EEG labs. Airoldi L,
et al. [6] analysed 290 adult EEGs and revealed that 67% of
the EEGs were categorized as normal. Smith D, et al. [7] from
the UK revealed 65% normal EEGs in their investigation.
According to Gurbani NS, et al. [5], in both the pediatric
and adult groups, 200 individuals (100 pediatric and 100
adult EEGs) revealed a high yield of normal EEGs referred
directly by non-neurologists (77% and 69%, respectively).
All of these studies showed that EEGs are used
indiscriminately in the community, and primary health care
professionals do not reliably clinically identify seizures and
rely on the diagnostic usefulness of EEGs for any patient
with paroxysmal disorders.
Nicolaides P, et al. [8] conducted an audit of EEG requests in general pediatrics and found that two-fifths of the
inquiries were incorrect, and 50-60% of referring doctors
believed the technique could diagnose or rule out epilepsy.
According to a prospective study of 850 children admitted to
neurologists, 92 % with seizures could be clinically identified
primarily on history [9]. This implies that if clinicians relied
more on their patients' histories, they would prescribe fewer
EEGs.
Conclusion
In conclusion, this research found substantial
discrepancies in EEG results between non-neurologists and
neurologists, with a higher percentage of abnormal EEG
reports, were noticed among neurologist referrals relative
to non-neurologists.
This emphasizes our recommended approach of
neurologist screening of EEG referrals requested by nonneurologists
to reduce the proportion of usual EEGs
and produces results similar with neurologists and could
beneficially incorporate such reporting data on the stream of
diagnosis and management.
This would implicate that careful review and inclusion of
non-neurologists' referral reports received with a neurologist's
request for an EEG may minimize the number of incorrect
EEG referrals of non-epileptic patients. This would result
in normal EEG results and ascertain health care provider
cooperation for more accurate diagnosis and management,
reduce the diagnostic error and utilize healthcare resources
appropriately. In order to guarantee the correct use of EEG,
coordination between non-neurologists and neurologists
on the patient's clinical status is critical. Also, the training
of general practitioners may minimize the frequency of
unneeded EEG requests.
REFERENCES
- Smith SJM. EEG in the diagnosis, classification, and management of patients with epilepsy. J Neurol Neurosurg Psychiatry. 2005;76(Suppl 2):ii2-ii7.
Google Scholar, Crossref
- Chandra SR, Asheeb A, Dash S, et al. Role of electroencephalography in the diagnosis and treatment of neuropsychiatric border zone syndromes. Indian J Psychol Med. 2017;39(3):243-249.
Google Scholar, Crossref, Indexed at
- Noachtar S, Güldiken B. Diagnose nichtepileptischer paroxysmaler Störungen und epileptischer Anfälle. Der Nervenarzt. 2017;88(10):1109-1118.
Google Scholar, Crossref, Indexed at
- Sand T, Bjørk MH, Vaaler AE. Is EEG a useful test in adult psychiatry? Tidsskr Den Nor legeforening. 2013;133(11):1200-1204.
Google Scholar, Crossref, Indexed at
- Gurbani NS, Gurbani SG, Mittal M, et al. Screening of EEG referrals by neurologists leads to improved healthcare resource utilization. Clin EEG Neurosci. 2006;37(1):30-33.
Google Scholar, Crossref, Indexed at
- Airoldi L, Beghi E, Bogliun G, et al. Rational use of EEG in adults in clinical practice. J Clin Neurophysiol. 1999;16(5):456.
Google Scholar, Crossref
- Smith D, Bartolo R, Pickles RM, et al. Requests for electroencephalography in a district general hospital: retrospective and prospective audit. BMJ. 2001;322(7292):954-957.
Google Scholar, Crossref, Indexed at
- Nicolaides P, Appleton RE, Beirne M. EEG requests in paediatrics: an audit. Arch Dis Child. 1995;72(6):522-523.
Google Scholar, Crossref, Indexed at
- Arts WFM, Geerts AT, Brouwer OF, et al. The early prognosis of epilepsy in childhood: The prediction of a poor outcome. The dutch study of epilepsy in childhood. Epilepsia. 1999;40(6):726-734.
Google Scholar, Crossref, Indexed at