Key words
Ischemic stroke, STA-MCA anastomosis, Cerebrovascular reserve capacity, internal carotid artery occlusion.
Introduction
Stroke remains a leading cause of mortality and permanent disability despite manifold attempts to treat and prevent cerebral ischemia using various medical and surgical treatments, many with still unproven effectiveness. Among these techniques extracranial (EC) to intracranial (IC) artery bypass represents anastomosis of the STA to the MCA. Following its introduction by Yasargil [6] in 1969 this procedure has been applicable to treat numerous patients with MCA stenosis or ICA occlusion. The intent is to increase collateral cerebral blood flow (CBF) distal to the occlusive or stenotic lesion.
Although attractive conceptual point of view EC-IC bypass was shown in an international randomized trail to be ineffective in preventing stroke [3]. This study failed to demonstrate any benefit to surgically treated patients compared to patients receiving medical treatment alone. Since then, only a few reports have been published on the potential beneficial effect of the EC-IC bypass in selected patients [2,7] and this management became rare outside Japan and therefore difficult to find in English literature. We present a case of bilateral ICA occlusion who underwent bilateral double STA-MCA bypass.
Double STA-MCA bypass consists of donor arteries using the parietal and the fontal branches of the STA anastomosed to the recipient arteries of M4 segments. Postoperative course was uneventful without any stroke episodes.
Case Report
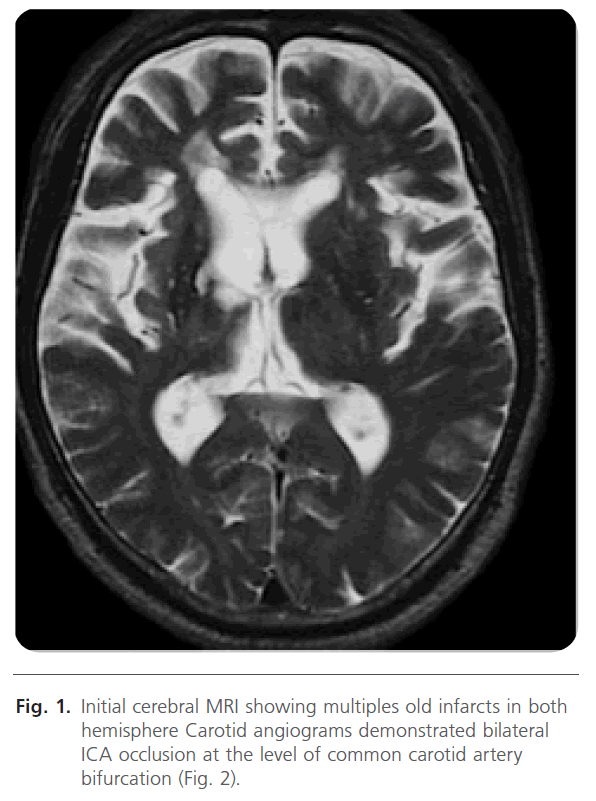
A 54 year-old male known for recurrent transient ischemic attacks (TIA) for three years presented at Suzuka Kaisei Hospital with left hemiparesis, dementia and urinary incontinence. He was also suffering from hypoesthesia in the lower extremities in worsening. When he arrived at hospital, he could not walk and was ambulated by a wheelchair. Initial cerebral magnetic resonance imaging (MRI) showed multiple old infarcts in both hemispheres (Fig. 1).
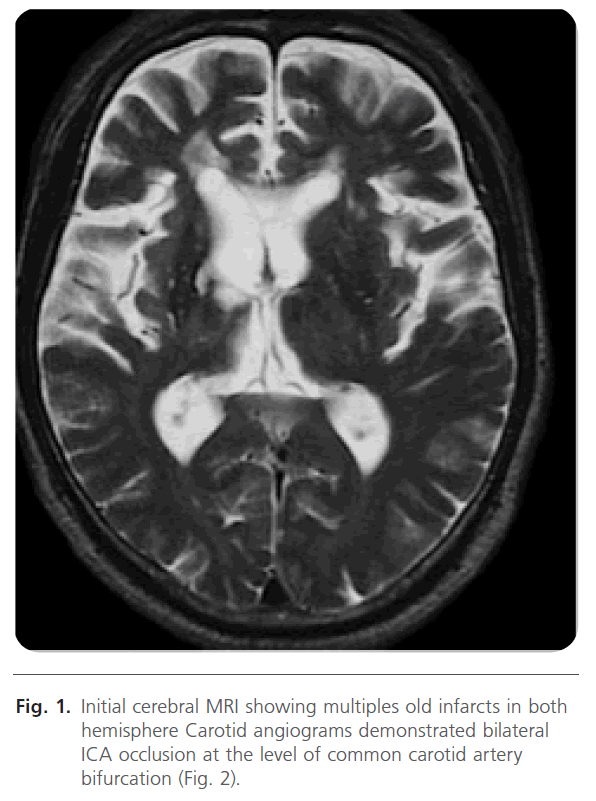
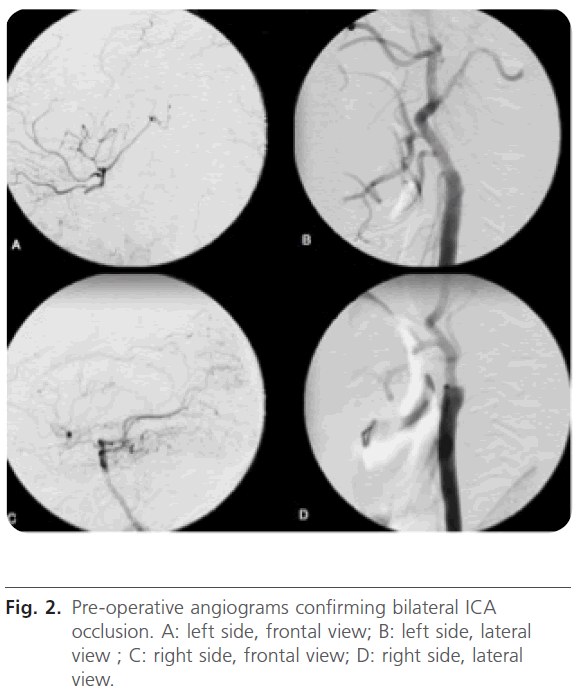
Figure 1: Initial cerebral MRI showing multiples old infarcts in both hemisphere Carotid angiograms demonstrated bilateral ICA occlusion at the level of common carotid artery bifurcation (Fig. 2).
The blood flow to the right hemisphere was supplied from the right posterior communicating artery. The left side blood flow was very limited and supplied mainly from the ophthalmic artery. Late arterial phase on the left side demonstrated lepto-meningeal anastomosis to cortical branches of MCA from that of posterior cerebral artery. On pre-operative
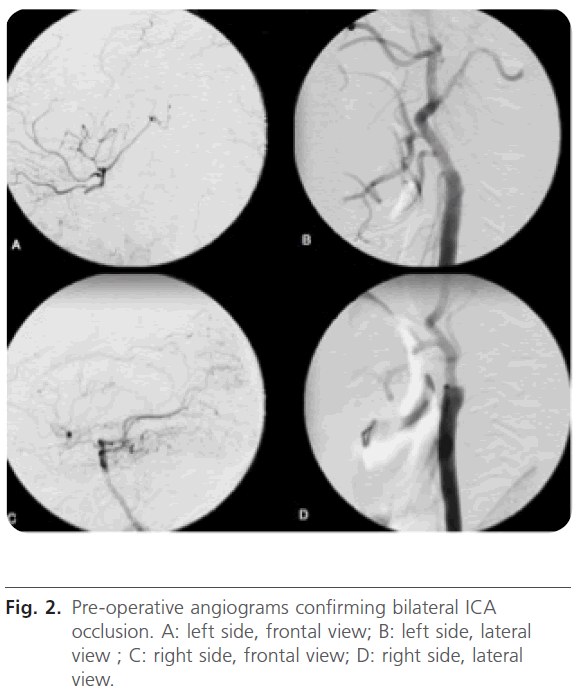
Figure 2: Pre-operative angiograms confirming bilateral ICA occlusion. A: left side, frontal view; B: left side, lateral view ; C: right side, frontal view; D: right side, lateral view.
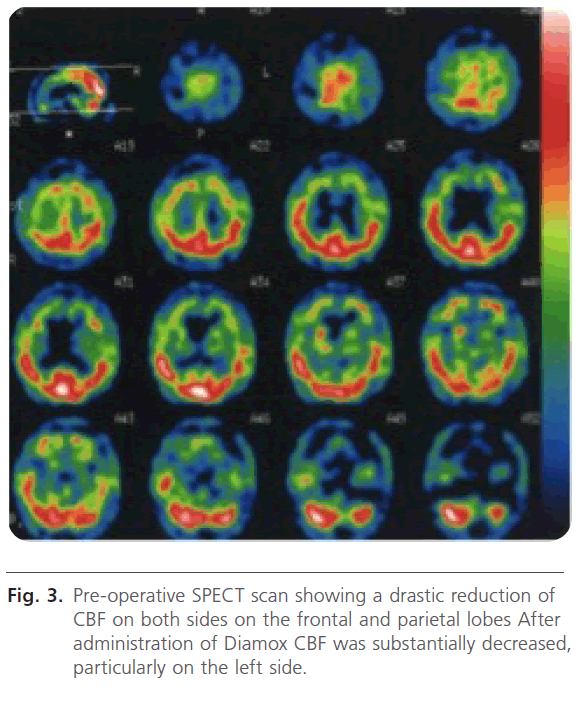
single-photon emission computed tomography scan (SPECT) there was a significant reduction in CBF on the frontal and parietal lobes bilaterally (Fig. 3).
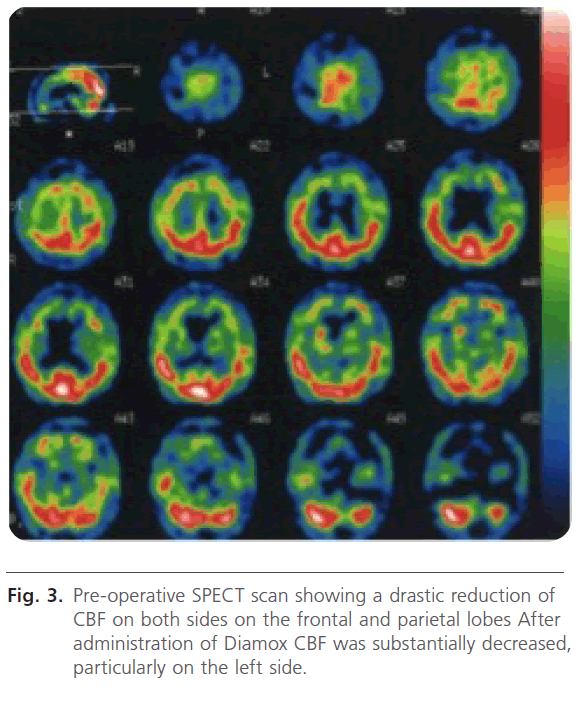
Figure 3: Pre-operative SPECT scan showing a drastic reduction of CBF on both sides on the frontal and parietal lobes After administration of Diamox CBF was substantially decreased, particularly on the left side.
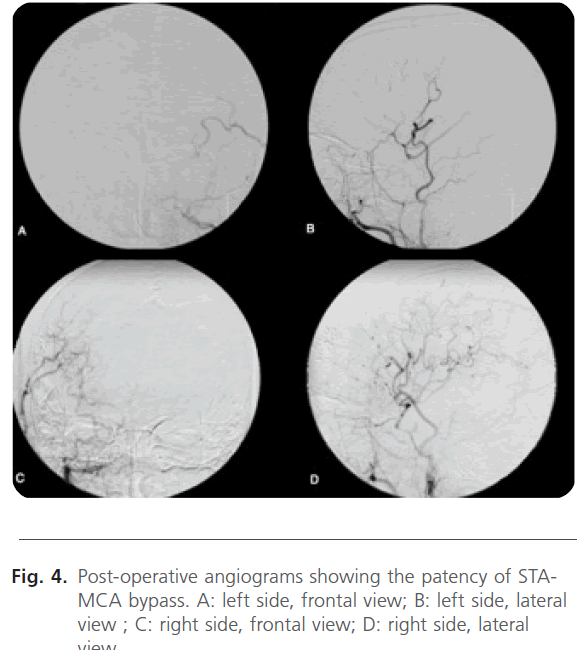
The patient was operated upon double STA-MCA bypass in two stages as right side first and left side second. Because CBF on the right side was worse at risk of cerebral infarction than the left side. The first operation was undertaken an end-to-side anastomosis between the STA and the M4 segment of MCA on the right side. The frontal and the parietal branches of the STA were used as donor arteries. One month later, after confirming no signs of complications and stable neurological condition the second operation was instituted. It was the same technique of double STA-MCA bypass on the left side (Fig. 4).
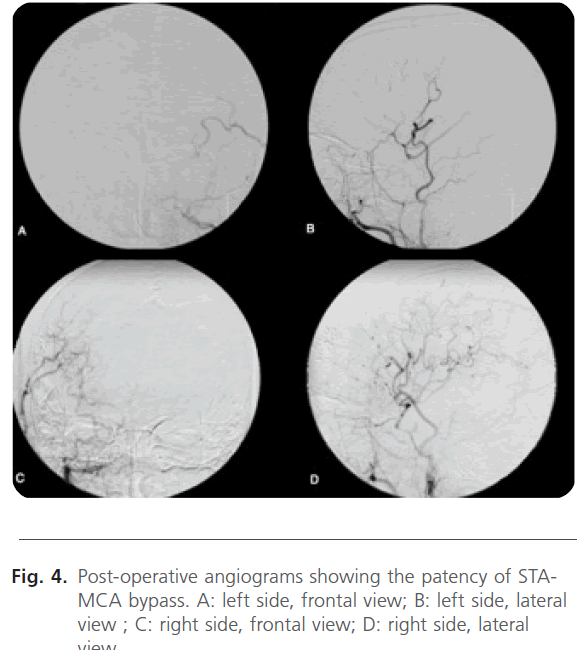
Figure 4: Post-operative angiograms showing the patency of STAMCA bypass. A: left side, frontal view; B: left side, lateral view ; C: right side, frontal view; D: right side, lateral view.
At the operation the patient was placed in a supine position with the head turned to the controlateral side and the ispilateral shoulder was rised using a mattress. The hair was shaved in a width of 2 cm along the courses of the STA branches. A small craniotomy was performed and the dura mater was opened. After determination of the recipient arteries, both branches of the STA were anastomosed to M4 segments using 10-0 nylon sutures. In both sides the shorter branch of the donor artery (the frontal branch) was anastomosed to the
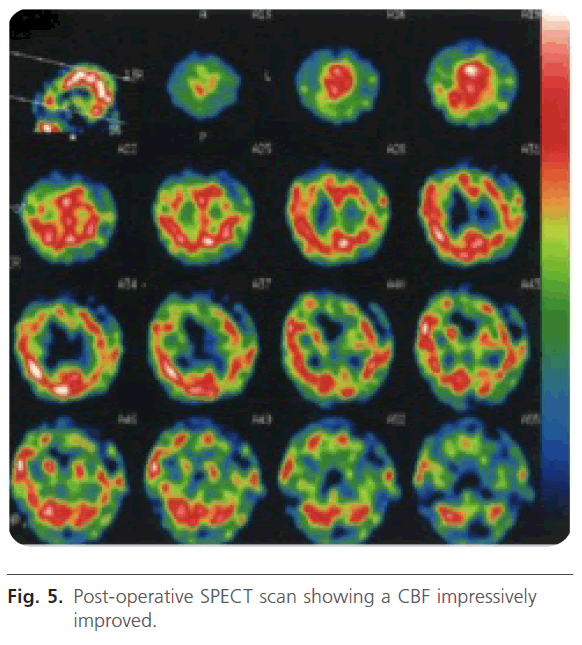
infrasyvian portion of M4 and the longer branch (the parietal branch) to the suprasylvian portion of M4. On postoperative SPECT scan CBF was significantly improved (Fig. 5).
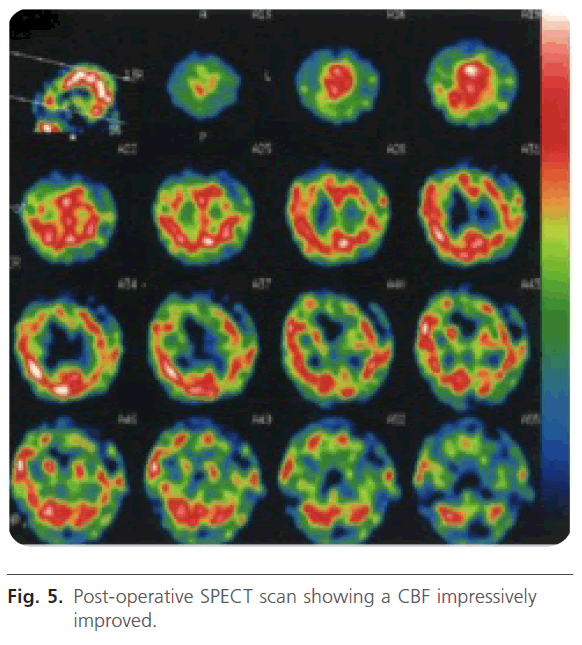
Figure 5: Post-operative SPECT scan showing a CBF impressively improved.
The neurological condition remained stable postoperatively. The right hemiparesis improved appreciably. The patient became to walk with a stick. The urinary incontinence and the intelligence quotient (IQ) were unchanged. TIA disappeared and after 5 years of follow-up there were no evidence of stroke recurrence. At the time of discharge the patient was sent to a rehabilitation center. He was capable of normal conversation and was pleased to spend satisfactory ADL.
Discussion
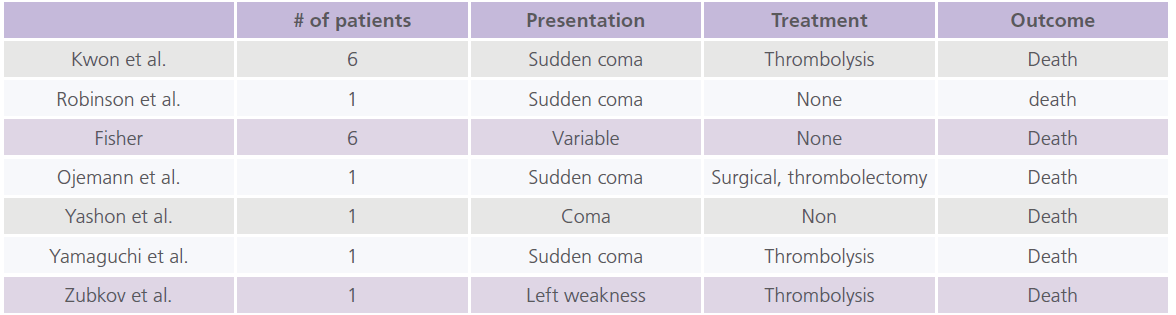
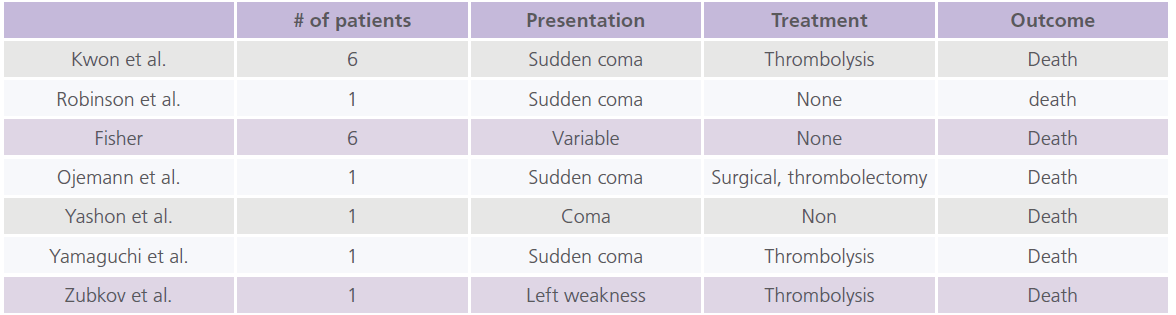
A complete occlusion of the ICA is an important prodrome of cerebrovascular disease. An asymptomatic ICA occlusion has a relatively benign course, whereas symptomatic occlusion increases future risk of strokes. Bilateral carotid occlusion is rare and is associated with high mortality and mobility rates. It was first described by Fisher [4]. Our literature research revealed only 17 cases among the English literature [1] (Tab. 1).
When confronted with a patient with symptomatic bilateral ICA occlusion in clincal practice, it is essential to know the risk of new vascular events to weigh the risks and benefits of treatment other than antithrombotic medication and control of vascular risk factors, such as revascularization procedures. It is recognized a clinical dilemma that the patients who in theory have the most gain from surgery also carry the highest perioperative risk [5]. One study reported a complication rate of conventional STA-MCA bypass close to 12% in patients neurolgically unstable [8]. Our own continued interest in ECIC bypass results from newly accepted evidence regarding the pathophysiology of cerebral ischemia. In addition to standard clinical and angiographic studies, it is now possible to identify from within the extremely diverse population of patients with cerebral ischemia a small subgroup exhibiting a characteristic deficit, namely impairment of the cerebrovascular reserve capacity. This impairment is due to poorly developed natural collateral vessels and the presence of underlying cerebrovascular occlusive disease, and may result in what we term misery cerebral perfusion. Recent evidence suggests that these patients are at particular risk for subsequent stroke compared to those with similar occlusive lesions [9].
The STA-MCA anastomosis can be used to augment flow to the distal MCA vascular territory. The original technique described by Ya?argil was an end-to-side anastomosis using a distal branch of the STA dissected from the scalp to a surface cortical branch of the MCA near the region of the sylvian fissure. Subsequent variations of this procedure have been described, including double-limb STA-MCA bypass grafts for additional flow and end-to-end anastomoses, using a microanastomotic device for higher-flow bypass. The STA
Table
commonly bifurcates in the preauricular region into a frontal and parietal branch. Variations in the anatomy include one of the two branches dominant, equal caliber of both branches, or atresia of the parietal branch.
In order to treat patients with chronic ischemia we have to identify the small subgroup of surgical candidates. Many factors are operative and of importance in the outcome of any individual case. These include the number of intracerebral and extracerebral occlusions, the degree and capacity of collateral flow, the restrictions to flow via stenotic lesions affecting major alternate channels, and finally the steal mechanisms that may, through other collaterals, actually deprive the brain of part of its blood supply [7]. We also have to take into account the age of the patient and his/her cardiovascular risk factors. Our patient tolerated well to the anesthesia of the two stage operations and had no significant cardiovascular risk factors except of smoking.
Conclusion
To our knowledge this is the first case report in of the bilateral double STA-MCA anastomosis for bilateral ICA occlusion reported in English litterature. Despite the results presented in this case cannot be regarded as proof of the beneficial effect of EC/IC bypass in patients with hemodynamic cerebral ischemia the results of this case is encouraging. The effectiveness and clinical significance of STA-MCA anastomis warrants further investigation.
Acknowledgements
The author wants to thank Dr Kenji Kanamura for giving her the case and for his help and wants to congratulate Dr Kenji Kanamura and Dr Tomohiro Araki for the successful bilateral double bypass.
Conflicts of Interest
The author declares that they have no conflict of interest.
2063
References
- AbuRahma, AF., Copeland, SE. Bilateral internal carotid artery occlusion: Natural history and surgical alternatives. Cardiovasc Surg. 1998; 6 (6): 579-83.
- Anderson, DE., McLane, MP., Reichman, OH., Origitano, TC. Improved cerebral blood flow and CO2 reactivity after microvascular anastomosis in patients at high risk for recurrent stroke. 1992; 31 (1): 26-33.
- No authors listed]. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. The EC/IC Bypass Study Group. N Engl J Med. 1985; 313 (19): 1191-200.
- Fisher, M. Occlusion of the carotid arteries: Further experiences. AMA Arch Neurol Psychiatry 1954; 72 (2): 187-204.
- Kenji, K., Tomohiro, A., Fumihiro, K., Kazuhide, H., Hideki, K., Keita, M., Akitoshi, S., Hidenori, S. STA-MCA bypass for the treatment of ischemic stroke, Trends in Neurovascular Surgery, Acta Neurochirurgica Supplementum 2010; 112: 55-57.
- Yasargil, MG. Microsurgery Applied to Neurosurgery. Stuttgart: Georg Thieme Verlag, 1969. pp. 105-115.
- Yasui, N., Suzuki, A., Sayama, I., Kawamura, S., Shishido, F., Uemura, K. Comparison of the clinical results of STA-MCA anastomosis and the medical treatment in the cerebral low perfusion patients with viable brain tissue. Neurol Res. 1981; 13 (2): 84-8.