Perspective - (2024) Volume 14, Issue 4
Drug Interactions: A Comprehensive Overview
Josh Solomon*
Department of Pharmacology, University of Wellassa, Badulla, Sri Lanka
*Correspondence:
Josh Solomon, Department of Pharmacology, University of Wellassa, Badulla,
Sri Lanka,
Email:
Received: 02-Jul-2024, Manuscript No. IPFT-24-14976 ;
Editor assigned: 05-Jul-2024, Pre QC No. IPFT-24-14976 (PQ);
Reviewed: 19-Jul-2024, QC No. IPFT-24-14976 ;
Revised: 01-Aug-2024, Manuscript No. IPFT-24-14976 (R);
Published:
29-Aug-2024
Introduction
Drug interactions are a critical concern in pharmacology,
impacting the efficacy and safety of treatments. Pharmacology,
the study of how drugs interact with the body, explores these
interactions in detail to ensure optimal patient care. This article
delves into the complexities of drug interactions, their types,
mechanisms and implications for clinical practice. Understanding
these interactions is crucial for healthcare professionals to
optimize therapeutic regimens and minimize adverse effects.
Description
Drug interactions
In clinical settings, patients often receive multiple medications
concurrently. Each drug introduces specific chemicals into the
body, where they interact with physiological systems to produce
therapeutic effects. However, these drugs can also interact with
each other, altering their intended effects, leading to adverse
reactions or diminishing therapeutic outcomes. Such
interactions form the basis of pharmacological studies aimed at
understanding their complexities and mitigating risks.
Types of drug interactions
Drug interactions can occur through several mechanisms:
Pharmacokinetic interactions: These involve changes in the
Absorption, Distribution Metabolism and Excretion (ADME) of
drugs. For example, a drug that inhibits liver enzymes
responsible for metabolizing another drug can increase its blood
levels, potentially leading to toxicity.
Pharmacodynamic interactions: These occur when drugs with
similar or opposing effects interact at the same receptor site or
physiological pathway. Combining drugs that have additive
effects (e.g., sedatives) can potentiate their actions, whereas
combining drugs with opposing effects (e.g., stimulants and
sedatives) may diminish therapeutic outcomes.
Combined pharmacokinetic and pharmacodynamic
interactions: Many drug interactions involve both ADME
changes and direct pharmacological effects. For instance, an
antibiotic that inhibits the metabolism of an oral contraceptive
can reduce its effectiveness due to decreased blood levels.
Mechanisms of drug interactions
Understanding the mechanisms behind drug interactions is
crucial for predicting and managing their effects:
Enzyme inhibition and induction: Drugs can inhibit or induce
cytochrome P450 enzymes, altering the metabolism of coadministered
medications. This can lead to increased or
decreased drug concentrations in the body.
Protein binding: Drugs may compete for binding sites on
plasma proteins, affecting the distribution and availability of
bound and unbound drug fractions in the bloodstream.
Renal transport mechanisms: Some drugs may interfere with
renal transport mechanisms, affecting the excretion rates of coadministered
medications and potentially leading to toxic
accumulation.
Clinical implications
Drug interactions pose significant challenges in clinical
practice:
Safety concerns: Certain drug combinations can lead to
severe adverse effects, including organ damage or lifethreatening
conditions.
Therapeutic failures: Ineffective treatment outcomes may
occur when drug interactions reduce the efficacy of
medications, requiring dosage adjustments or alternative
therapies.
Patient variability: Factors such as age, genetics and
underlying health conditions influence individual susceptibility
to drug interactions, requiring personalized approaches to
therapy.
Managing drug interactions
Healthcare professionals employ various strategies to manage
and minimize the risks associated with drug interactions:
Comprehensive medication review: Regular review of a
patient's medication list helps identify potential interactions and
allows for adjustments in therapy.
Drug information resources: Access to databases and drug
interaction software helps healthcare providers quickly assess
potential interactions and make informed prescribing decisions.
Patient education: Educating patients about their
medications, including potential interactions and adverse effects,
empowers them to recognize and report any concerning
symptoms promptly.
Interprofessional collaboration: Healthcare teams, including
physicians, pharmacists and nurses, collaborate to coordinate
care and optimize medication regimens, considering each
patient's unique needs.
Clinical implications and management
Understanding drug interactions is crucial for healthcare
providers to optimize therapy and minimize risks:
Prevention: Screening for potential interactions before
initiating therapy helps mitigate risks. This includes reviewing
patient medication histories and considering pharmacogenetic
testing.
Monitoring: Regular monitoring of therapeutic outcomes and
adverse effects can detect interactions early, allowing for timely
intervention.
Adjustments: Modifying drug dosages, changing
administration schedules or choosing alternative therapies are
strategies to manage interactions effectively.
Case studies and examples
Case studies illustrate the impact of drug interactions in
clinical practice:
Warfarin and antibiotics: Antibiotics like fluoroquinolones can
interfere with warfarin metabolism, necessitating close
monitoring of INR levels to prevent bleeding complications.
Statins and grapefruit juice: Grapefruit juice inhibits intestinal
CYP3A4 enzymes, leading to increased statin levels and potential
myopathy.
Factors influencing drug interactions
Several factors contribute to the complexity and variability of
drug interactions:
Polypharmacy: The simultaneous use of multiple medications
increases the likelihood of interactions.
Patient factors: Variations in patient characteristics such as
age, genetics and underlying diseases can influence drug
metabolism and response.
Dosing regimens: The timing, dosage and route of
administration can impact the likelihood and severity of
interactions.
Drug properties: Chemical properties, pharmacokinetic
profiles, and therapeutic indices of drugs play significant roles in
potential interactions.
Future directions in pharmacology
Advances in pharmacogenomics and personalized medicine
offer promising avenues for managing drug interactions more
effectively. Pharmacogenomic testing can identify genetic
variations that influence drug metabolism, guiding individualized
treatment strategies to minimize adverse reactions and enhance
therapeutic outcomes.
Conclusion
In conclusion, drug interactions are multifaceted phenomena
with significant implications for patient safety and treatment
efficacy. Understanding the mechanisms and types of
interactions is crucial for healthcare professionals to mitigate
risks and optimize therapeutic outcomes. Through ongoing
research and collaborative efforts, pharmacology continues to
evolve, offering innovative solutions to enhance medication
safety and patient care in the face of complex drug regimens.
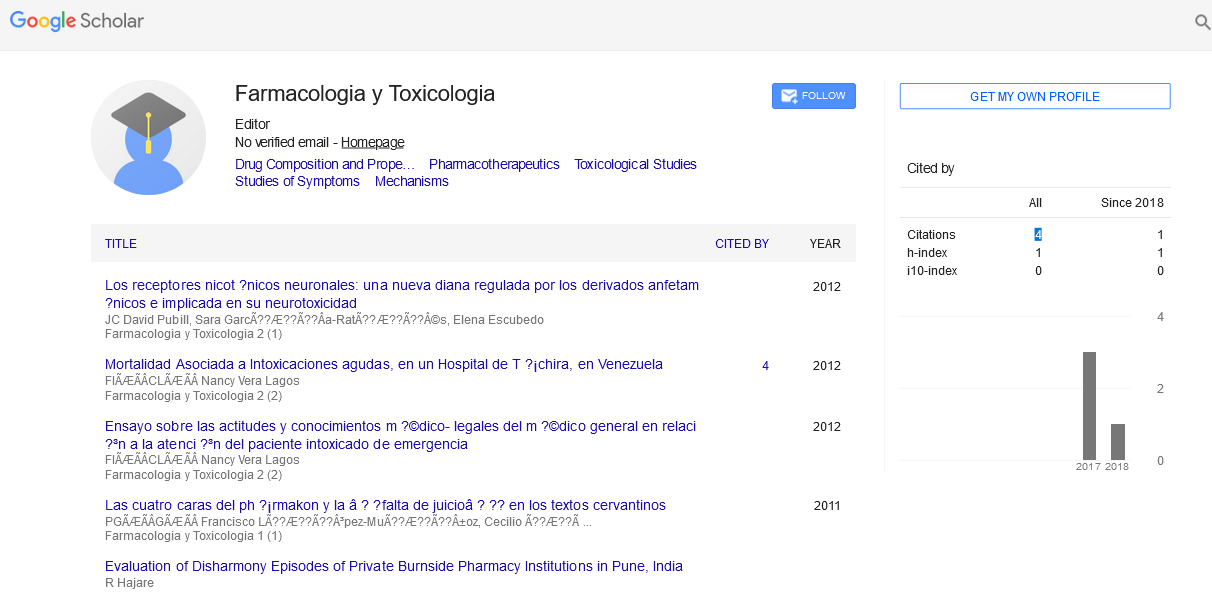
Citation: Solomon J (2024) Drug Interactions: A Comprehensive Overview. Farmacologia Toxicologia, Vol.14 No.4: 039