Perspective - (2024) Volume 14, Issue 5
Drug Interactions: Understanding the Impact of Concurrent Drug Administration
Katsumi Fukamachi*
Department of Pharmacology, University of Puranchuel, Biratnagar, Nepal
*Correspondence:
Katsumi Fukamachi, Department of Pharmacology, University of Puranchuel, Biratnagar,
Nepal,
Email:
Received: 07-Aug-2024, Manuscript No. IPFT-24-15133;
Editor assigned: 12-Aug-2024, Pre QC No. IPFT-24-15133 (PQ);
Reviewed: 26-Aug-2024, QC No. IPFT-24-15133;
Revised: 01-Oct-2024, Manuscript No. IPFT-24-15133 (R);
Published:
29-Oct-2024
Introduction
In the intricate world of pharmacology, drug interactions play
a crucial role in determining the efficacy and safety of
therapeutic treatments. When two or more drugs are
administered simultaneously, they can influence each other's
effects, leading to a range of outcomes from enhanced
therapeutic effects to severe adverse reactions. Understanding
drug interactions is essential for optimizing treatment regimens
and ensuring patient safety.
Description
Drug interactions
Drug interactions occur when the presence of one drug alters
the pharmacological effect of another drug. These interactions
can be beneficial or harmful and may influence the effectiveness
of treatment or increase the risk of adverse effects. The nature
of these interactions depends on various factors, including the
drugs involved, their mechanisms of action and the patient's
individual characteristics.
Types of drug interactions
Drug interactions can be classified into several categories
based on their mechanisms:
Pharmacokinetic interactions are the interactions affect the
absorption, distribution, metabolism or excretion of a drug. For
example:
Absorption: One drug might alter the gastrointestinal pH,
affecting the absorption of another drug. For instance, antacids
can decrease the absorption of certain antibiotics.
Metabolism: Some drugs can induce or inhibit enzymes
responsible for drug metabolism. For example, the antibiotic
rifampin can induce liver enzymes, leading to reduced levels of
other drugs metabolized by the liver, such as oral
contraceptives.
Excretion: Drugs affecting renal function can alter the
elimination of other drugs. Diuretics, for instance, can affect the
renal clearance of other medications, such as lithium.
Pharmacodynamic interactions are the interactions occur
when drugs have additive, synergistic or antagonistic effects on
the same physiological system. For example:
Additive effects: Two drugs with similar effects can lead to an
exaggerated response. For instance, combining two central
nervous system depressants, such as benzodiazepines and
alcohol, can lead to profound sedation.
Synergistic effects: Two drugs can work together to enhance
therapeutic effects. An example is the combination of betalactam
antibiotics with beta-lactamase inhibitors to treat
resistant bacterial infections.
Antagonistic effects: One drug can counteract the effect of
another. For instance, opioid analgesics can be antagonized by
opioid antagonists like naloxone, which is used in cases of
overdose.
Pharmacogenomic interactions are the interactions arise from
genetic variations that affect drug metabolism. Genetic
polymorphisms can lead to differences in enzyme activity,
influencing how individuals respond to drugs. For example,
variations in the CYP450 enzyme system can lead to different
rates of drug metabolism, affecting drug efficacy and safety.
Clinical implications of drug interactions
Drug interactions can have significant clinical implications,
ranging from reduced therapeutic efficacy to increased risk of
adverse events. Some key considerations include:
Increased risk of adverse effects: Interactions that enhance
the effects of a drug can lead to toxicity. For example, combining
anticoagulants like warfarin with other drugs that inhibit blood
clotting can increase the risk of bleeding complications.
Reduced drug efficacy: Some interactions can diminish the
effectiveness of a drug. For instance, the interaction between
antiepileptic drugs and oral contraceptives can lead to reduced
efficacy of the contraceptives, increasing the risk of unintended
pregnancies.
Altered pharmacokinetics: Changes in drug metabolism or
excretion can lead to either subtherapeutic or toxic drug levels.
Monitoring and dose adjustments may be necessary to manage
these interactions effectively.
Patient-specific factors: Individual patient factors, such as age,
sex, comorbidities and genetic variations, can influence drug
interactions. Personalized medicine approaches can help tailor
treatment plans to minimize the risk of adverse interactions.
Managing drug interactions
Effective management of drug interactions involves several
strategies:
Medication review: Regular review of a patient’s medication
list can help identify potential interactions. Healthcare providers
should be aware of all medications, including over-the-counter
drugs and supplements, that a patient is taking.
Drug interaction checkers: Various online tools and databases
are available to help identify potential drug interactions. These
resources can assist healthcare providers in making informed
decisions about drug therapy.
Monitoring and adjustments: Close monitoring of patients for
signs of adverse effects or changes in drug efficacy is crucial.
Dose adjustments and therapeutic drug monitoring may be
necessary to optimize treatment.
Patient education: Educating patients about the potential for
drug interactions and the importance of disclosing all
medications they are taking can help prevent adverse effects.
Patients should be encouraged to report any new symptoms or
concerns.
Collaborative care: Collaboration between healthcare
providers, including pharmacists and physicians, can enhance
the management of drug interactions. Pharmacists, in particular,
play a vital role in identifying and resolving potential
interactions.
Conclusion
Drug interactions are a critical aspect of pharmacotherapy
that can significantly impact patient outcomes. By
understanding the mechanisms of drug interactions and
implementing strategies to manage them, healthcare providers
can enhance the safety and efficacy of treatment regimens.
Ongoing research and advancements in pharmacogenomics will
continue to improve our ability to predict and manage drug
interactions, ultimately leading to better patient care and
outcomes.
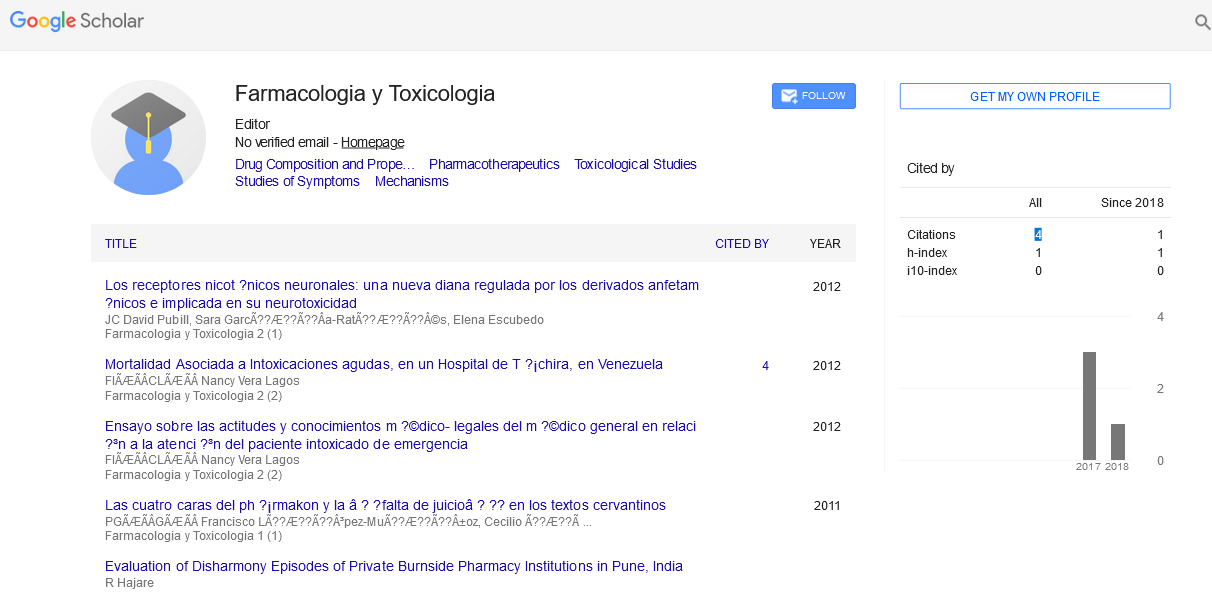
Citation: Fukamachi K (2024) Drug Interactions: Understanding the Impact of Concurrent Drug Administration. Farmacologia Toxicologia, Vol.14 No.
5: 048