Keywords
Migraine disorders; Trigger point; Pressure pain threshold; Range of motion
Abbreviations
CROM: Cervical Range of Motion; CONSORT: Consolidated Standards of Reporting Trials; DN: Dry Needling; ICC: Intra-Class Correlation Coefficient; MTrPs: Myofascial Trigger Points; NDI: Neck Disability Index; PPT: Pressure Pain Threshold; SCM: Sternocleidomastoid; STT: Soft Tissue Technique; UT: Upper Trapezius; VAS: Visual Analog Scale
Introduction
Migraine headache is one of most frequent health complaints approximately 12% of the world’s adult population. It is associated with problems, such as pain, disability, and economic impact [1]. The vascular, central nervous system, peripheral contributions [2], and nociceptive inputs of myofascial origin [3] are definitive factors in the pathophysiology of migraine headache. Furthermore, muscle dysfunctions, in the craniocervical area, may facilitate migraine pain expression. Specifically, the most muscles involved in migraine patients include the upper trapezius (UT), sternocleidomastoid (SCM), and sub-occipital muscles [4]. Migraine headache is known to be associated with more trigger points in the cervical musculature, forward head posture, reduction in cervical range of motion (CROM), and increased sensitivity on the cervical muscles [3,5]. Therefore, the existence of myofascial trigger points (MTrPs) has been confirmed in migraine patients. Accordingly, these symptoms of migraine headache can be attributed to trigger points in the cervical area [5,6].
Trigger points (TrPs) are hyperirritable spots in skeletal muscle that are associated with hypersensitive palpable nodules in taut bands. TrPs are active or latent. Active TrPs cause spontaneous pain, but latent TrPs are not spontaneously symptomatic unless compression is used [7]. The exact cause of MTrP is still unknown, but it is stated that a variety of mechanical or chemical noxious events may stimulate and sensitize muscle nociceptors play a role in the development of muscle trigger points. Abnormal depolarization of motor end plates and sustained muscular contraction can cause central sensitization [8]. Also, it has shown that more acidic environments in trigger points and high levels of inflammatory mediators which are typically produced pain and tenderness [9]. Myofascial trigger points causing pain and dysfunction are commonly treated by dry needling [10-12] and soft tissue technique [13-15] which are considered by many to be effective options. However, the superiority of one method over the other is unknown. The dry needling (DN) is an invasive method where a solid filament needle is inserted directly into a MTrP site. It is widely used in clinical practice and could be beneficial in alleviating pain associated with active MTrPs [16]. The soft tissue techniques (ischemic compression and stretching) have been recommended as a means of managing TrPs [17]. The soft tissue techniques (STTs) are a commonly utilized method for achieving muscle inhibition to reduce pain, restore the muscle to normal length, and improve the range of both active and passive motion [18]. Although these two techniques are effective in reducing myofascial pain, its mechanism of action and effectiveness have not been found due to lack of objective and subjective measures for pain. We hypothesized that STT is more effective on the improvement of symptoms in the migraine patients compared with the DN method. Thus, we aimed to compare the effects of dry needling and soft tissue technique on active trigger points of the UT, SCM, and sub-occipital muscles in the migraine patients.
Materials and Methods
Study design and ethical approval
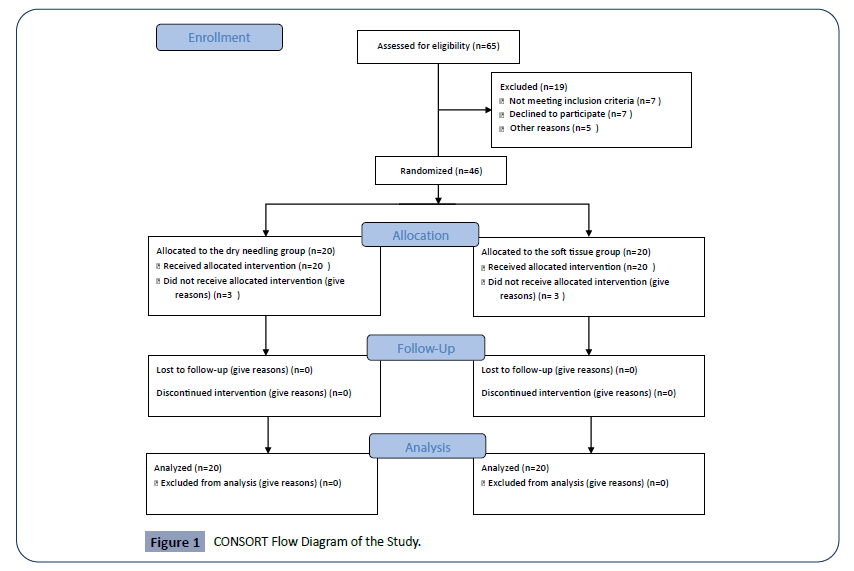
This study was a double-blind randomized clinical trial. All subjects signed an informed consent form which was approved by the Ethics Committee of Social Welfare and Rehabilitation Sciences (Ethics code no: IR.USWR.REC.1395.192). The study process and the individual's role were clearly explained. The subjects were free to leave the study at each stage of the study. Also, this article was extracted from the Iranian Registry Clinical Trial (IRCT) number IRCT20171219037956N1. It was considered according to the Consolidated Standards of Reporting Trials (CONSORT) statement (Figure 1).
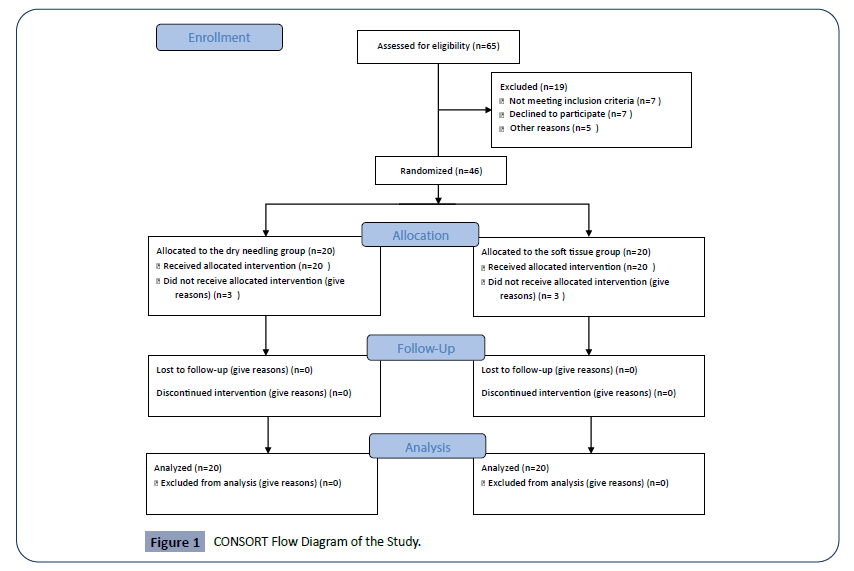
Figure 1: CONSORT Flow Diagram of the Study.
Sample size calculation
To determine the sample size, a pilot study was first performed on 10 migraine patients, then the results were used in the software PASS 11 to calculate the sample size with test Type I error 0.05, and test Type II error 0.20. According to the statistical formula, 20 patients in each group were required.
Participants
Forty subjects, 16 men and 24 women, aged 25-55 years old (mean age: 38.25; SD: 10.94 years), with migraine headache who were referred to a neurology clinic in Shiraz University of Medical Sciences was invited to participate in this study. This study was done at the Physical Therapy Research Center of Shiraz University of Medical Sciences in Iran from April to September 2018. Participants had to be between 25 and 55 years old if they had a diagnosis of migraine headache according to criteria of IHS by a neurologist, presenting with migraine headache for at least 6 months, and diagnosed with active TrPs in their UT, SCM, and sub-occipital muscles reproducing their symptoms. Patients with migraine were examined for finding any active trigger points in UT, SCM, and sub-occipital muscles. The presence of active trigger points was confirmed if 1-There was focal muscle tenderness that was activated by palpation and when it’s done, referred pain replicating patient’s headache complaint. 2-There was a jump sign that was a reaction to compression on a trigger point” [19]. Participants were excluded if they had evidence of neck disc herniation; neck or shoulder area surgery; history of other headaches and unusual migraine; history of acute and chronic psychiatric problems; subjects who have been using muscle relaxants drugs, patients with trigger point therapy in the cervical area within previous 6 months, evidence of cognitive deficits, subjects who had a needle phobia, and subjects who were pregnant or breastfeeding.
In this randomized, clinical trial study, block randomization was performed by a statistical expert using excel software and the block sizes were random. Then, the participants were randomly divided into the dry needling and the soft tissue technique groups. A physiotherapist who administered the treatment was blinded to the objectives of the investigation. Another physiotherapist was responsible for the assessments. Patients were blinded to the group allocation. Also, an unware researcher performed data analysis. Six patients received treatment but did not attend the final follow-up appointment. In all, data from 40 patients were used in our final analyses.
Intervention
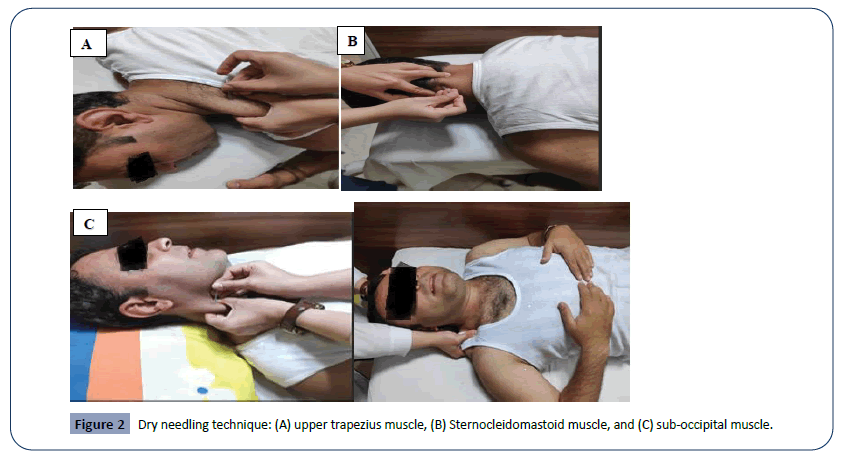
After initial examination, the participants received dry needling or soft tissue techniques. The treatment protocol for the DN group consisted of the DN on active TrP in the UT, SCM, suboccipital muscles. Dry needling of the selective muscles was done according to Dommerholt & Fernandez-de-las-Penas (2013) [20]. With the aid of insertion tubes, the standard single-use sterile acupuncture needles (25 mm, 0.25G) were performed, following the procedure originally described by Simons et al [21] Between 8 and 10 quick needle insertions were inserted deeply into the skin over the trigger points, using a procedure similar to that performed by Hong et al. (1994) [22]. The DN technique was applied for three sessions at intervals of 48 hours and in session four, an assessment of primary outcomes was conducted without any treatment (Figure 2) [20].
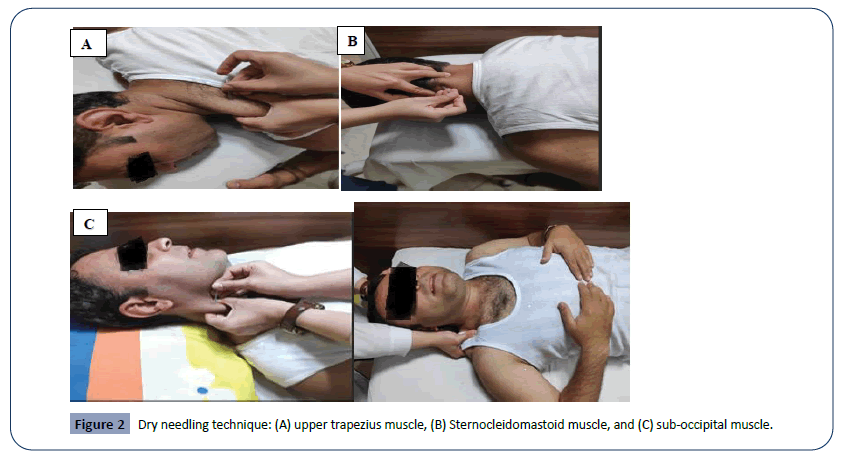
Figure 2: Dry needling technique: (A) upper trapezius muscle, (B) Sternocleidomastoid muscle, and (C) sub-occipital muscle.
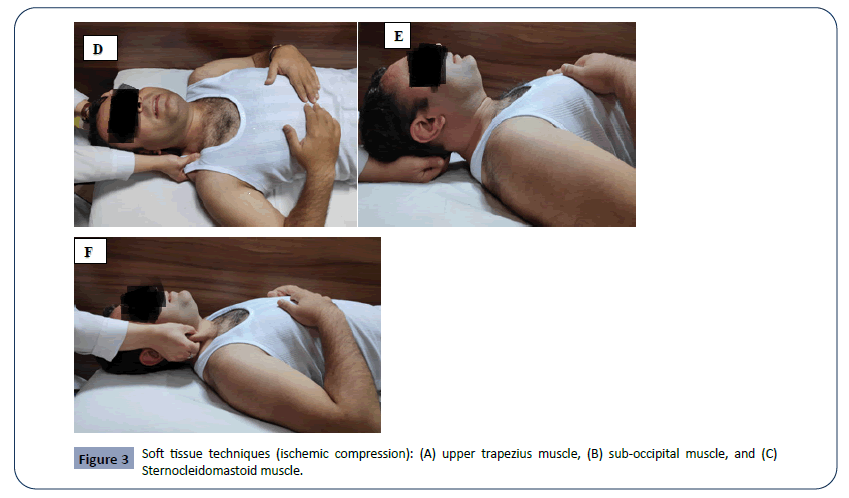
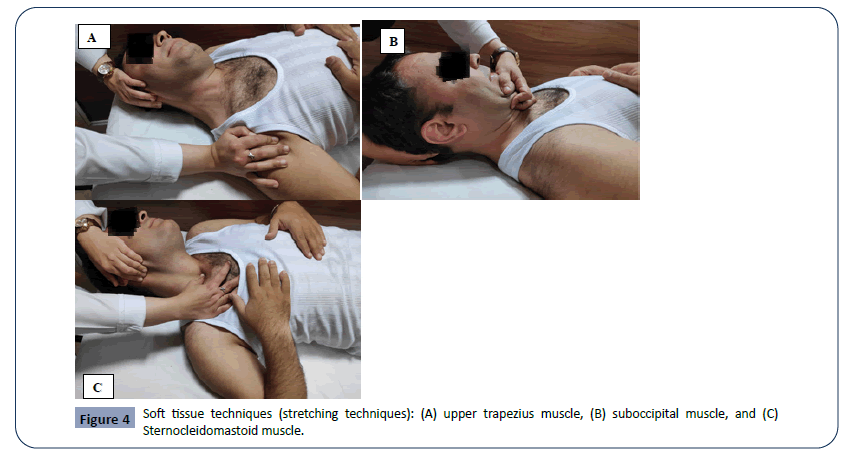
The treatment protocol for the STT group consisted of the ischemic pressure and muscle stretching on the UT, SCM, suboccipital muscles. This technique was done according to Espí- López et al (2018) [15]. In each treatment session, all the stretches were held for 30 seconds, and ischemic pressure process was performed three times for 30-60s with a 30s interval between each repetition. Furthermore, the patients were treated for three sessions ( with a duration of 20 minutes per session in the treatment group) in a one-week period with at least a two-day break between each session, and in session four, an assessment of primary outcomes was conducted without any treatment (Figures 3 and 4) [23].
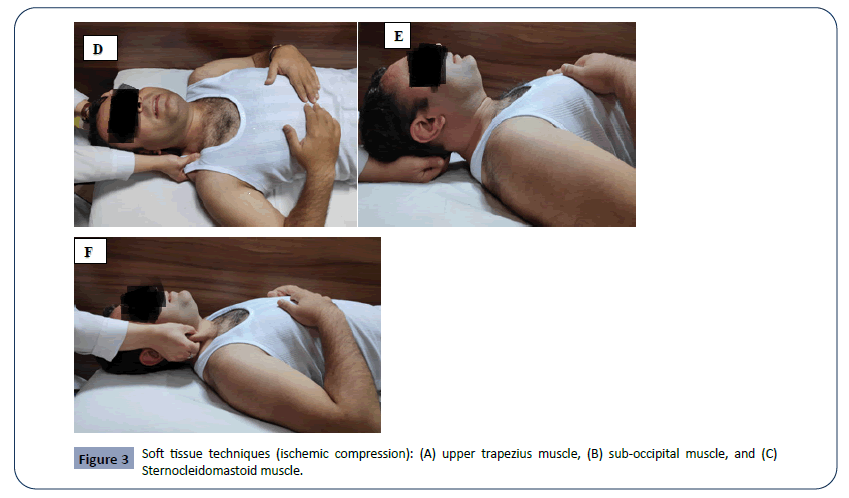
Figure 3: Soft tissue techniques (ischemic compression): (A) upper trapezius muscle, (B) sub-occipital muscle, and (C) Sternocleidomastoid muscle.
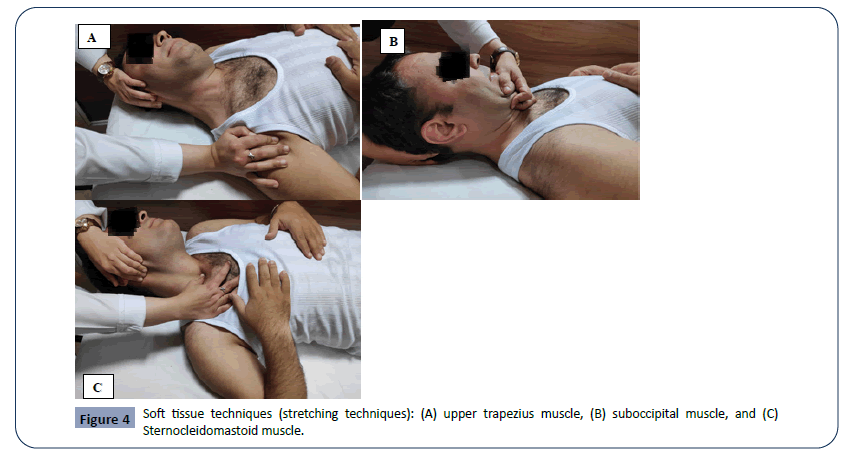
Figure 4: Soft tissue techniques (stretching techniques): (A) upper trapezius muscle, (B) suboccipital muscle, and (C) Sternocleidomastoid muscle.
Descriptive data
Sex, age, weight, height, and body mass index of all participants were recorded.
Outcome measures
The pain intensity, neck disability index (NDI), pressure pain threshold (PPT), and cervical range of motion (CROM) were evaluated at before the intervention and at the end of the intervention.
Pain intensity
The pain intensity was recorded on a visual analog scale (VAS). In this study, a 10 cm VAS for pain was used. Pain level on the VAS was recorded on a 10 cm line that subjects were asked to state their pain level by placing a mark along with this horizontal line [24]. The reliability of this method has been established previously [25].
Disability measures
The NDI is a widely used questionnaire that was designed to assess disability due to neck pain. It consists of 10 items measuring the influence of neck pain on daily activities. Individual items are scored and the total score can range from 0 to 50. Neck disability is classified as follows, as a function of NDI score: 0-4=absence of disability; 5-14=mild; 15-24=moderate; 25-34=severe; 35 or higher=complete [26]. The Persian version of NDI has been shown to be a reliable and valid instrument to measure functional status in Persian speaking patients with neck disorders [27].
PPT
The PPT at trigger point sites was recorded with an algometer (Force gauge, FG-5005, RS232, Lutron Electronic, Arizona, USA). The algometer was used with perpendicular compression to the skin surface. The compression was going to be stopped when the subject was reporting the “pain.” The average value of the three measurements was used for data analysis [28]. An intraclass correlation coefficient (ICC) of 0.95 was obtained for the reliability of measurements of this device.
CROM
The CROM were measured by a clinical goniometer. The subject sat in a chair with a backrest, with the straight column resting on it. Then, it was requested to perform the active cervical movements of flexion, extension, left and right rotation, and left and right lateral flexion with the goniometer on their head, to the point of pain. The reliability of this method has been established previously [29].
Statistical analysis
Statistical analysis was done using SPSS version 23. Descriptive statistics were performed on the demographic characteristics of the samples. The Kolmogorov-Smirnov test was used to assess the normality of distribution. We used independent t test for between-group comparisons. Because of normal distribution of data, the paired t-test were used for within-group comparisons. Effect sizes were calculated using within-group Cohen’s d coefficient. The ICC was being used to assess the intra-tester reliability of the measurement. The significance level was set at 0.05.
Results
Flow diagram and descriptive data
All of the variables had normal distribution. Sixty-five participants were screened, but only 40 participants were enrolled in the study, with 20 participants allocated to the DN group, and 20 to the STT group. The mean of subjects’ age in the DN group was 36.10 ± 10.43 and in the STT was 40.40 ± 11.27. There was no significant difference in gender distribution, age, weight, and BMI (Table 1). The clinical characteristics of the participants before treatment are shown in Table 1.
Table 1: Patients’ clinical characteristics at baseline.
| Variables |
Dry needling group (n=20) |
Soft tissue technique group (n=20) |
P-value1 |
| Age(years) |
36.10 ± 10.43 |
40.40 ± 11.27 |
0.21 |
| Weight(kg) |
67.25 ± 10.21 |
70.20 ± 9.15 |
0.34 |
| Height(m) |
1.69 ± 9.03 |
1.68 ± 9.85 |
0.61 |
| BMI (kg/m2) |
24.04 ± 2.06 |
25.07 ± 3.40 |
0.25 |
| VAS (score) |
7.60 ± 0.94 |
7.20 ± 0.95 |
0.18 |
| NDI (score) |
22.20 ± 6.50 |
22.50 ± 7.01 |
0.88 |
| PPT of UT Muscle (kg/cm2) |
11.39 ± 1.06 |
11.48 ± 0.58 |
0.72 |
| PPT of SCM muscle (kg/cm2) |
5.70 ± 1.24 |
6.50 ± 0.87 |
0.07 |
| PPT of sub-occipital muscle (kg/cm2) |
5.40 ± 0.89 |
5.58 ± 0.61 |
0.46 |
| Flexion ( Degree) |
33.05 ± 2.45 |
34.75 ± 3.93 |
0.10 |
| Extension (Degree) |
22.60 ± 3.08 |
23.20 ± 2.83 |
0.52 |
| Right Rotation (Degree) |
40.30 ± 2.83 |
41.55 ± 2.37 |
0.13 |
| Left Rotation (Degree) |
39.25 ± 2.61 |
39.20 ± 3.27 |
0.95 |
| Right Lateral flexion (Degree) |
35.05 ± 2.13 |
35.20 ± 3.67 |
0.87 |
| Left Lateral flexion (Degree) |
35.20 ± 2.64 |
34.55 ± 3.74 |
0.53 |
| Sex (female/male) |
12/8 |
12/8 |
- |
BMI=Body Mass Index; VAS=Visual Analog Scale; NDI=Neck Disability Index; PPT=Pressure pain threshold; P-value1= Indicates Significance at P < 0.05 (between-group comparison according to the Independent t test).
The ICC (first and third measurement) was 0.95 for repeat measures of the PPT measurement using an algometer. Pre- and post-measurement scores for the VAS, NDI, and CROM in the two groups and the results of the paired t- test are provided in Table 2.
Table 2: Pre- and post-measurement scores for of VAS, NDI, PPT of UT muscle, PPT of SCM muscle, PPT of sub-occipital muscle, and cervical range of motion in the subjects.
| Variables |
|
Dry needling group |
Soft tissue group |
P value 1 Dry needling |
Cohen’s d |
P value1 Soft tissue |
Cohen’s d |
P value2 Intra-group |
| Pre–post treatment |
Pre–post treatment |
| VAS (score) |
Pre-treatment Post-treatment |
7.60 ± 0.94 4.00 ± 0.79 |
7.20 ± 0.95 3.20 ± 0.76 |
t=17.12 <0.001 |
4.14 |
t=19.49 <0.001 |
4.64 |
<0.001 |
| NDI (score) |
Pre-treatment Post-treatment |
22.20 ± 6.50 18.55 ± 6.42 |
22.50 ± 7.01 9.45 ± 3.60 |
t=11.17 <0.001 |
2.94 |
t=10.41 <0.001 |
2.34 |
<0.001 |
| PPT of UT muscle (kg/cm2) |
Pre-treatment Post-treatment |
11.39 ± 1.06 13.08 ± 0.98 |
11.48 ± 0.58 13.11±0.78 |
t=20.42 <0.001 |
1.65 |
t=15.81 <0.001 |
2.37 |
0.91 |
| PPT of SCM muscle (kg/cm2) |
Pre-treatment Post-treatment |
5.70 ± 1.24 7.36 ± 1.25 |
6.50 ± 0.87 7.82±0.66 |
t=20.28 <0.001 |
1.33 |
t=15.58 <0.001 |
1.70 |
0.15 |
| PPT of sub-occipital muscle (kg/cm2) |
Pre-treatment Post-treatment |
5.40 ± 0.89 7.08± 0.90 |
5.58 ± 0.61 7.16 ± 0.59 |
t=18.78 <0.001 |
1.87 |
t=14.70 <0.001 |
2.63 |
0.72 |
| Flexion (Degree) |
Pre-treatment Post-treatment |
33.05 ± 2.45 37.10 ± 2.31 |
34.75±3.93 38.35 ± 3.61 |
t=13.35 <0.001 |
1.70 |
t=13.55 <0.001 |
0.95 |
0.20 |
| Extension (Degree) |
Pre-treatment Post-treatment |
22.60 ± 3.08 26.40 ± 2.70 |
23.20 ± 2.83 26.20 ± 2.54 |
t=16.90 <0.001 |
1.31 |
t=10.33 <0.001 |
1.11 |
0.81 |
| Right Rotation (Degree) |
Pre-treatment Post-treatment |
40.30 ± 2.83 45.25 ± 2.98 |
41.55 ± 2.37 46.95 ± 2.18 |
t=13.26 <0.001 |
1.70 |
t=12.01 <0.001 |
2.37 |
0.05 |
| Left Rotation (Degree) |
Pre-treatment Post-treatment |
39.25 ± 2.61 44.30 ± 2.77 |
39.20 ± 3.27 42.70 ± 3.07 |
t=14.07 <0.001 |
1.87 |
t=15.65 <0.001 |
1.10 |
0.09 |
| Right Lateral flexion (Degree) |
Pre-treatment Post-treatment |
35.05 ± 2.13 39.55 ± 1.70 |
35.20 ± 3.67 39.85 ± 3.88 |
t=13.37 <0.001 |
2.33 |
t=11.84 <0.001 |
1.23 |
0.75 |
| Left Lateral flexion (Degree) |
Pre-treatment Post-treatment |
35.20 ± 2.64 40.60 ± 3.11 |
34.55 ± 3.74 39.60 ± 3.63 |
t=11.71 <0.001 |
1.87 |
t=14.68 <0.001 |
1.37 |
0.35 |
Scores are expressed as means (standard deviation). VAS=Visual Analog Scale; PPT=Pressure Pain Threshold; NDI=Neck Disability Index; P1=P value Based on Intra-Group Comparison (based on the paired t test); P2=P Value Based on Intra-Group Comparison (based on the dependent t-test).
Within group comparison of the experimental groups
The VAS, NDI, PPT, and CROM improved significantly in both study groups. The mean VAS and NDI scores decreased pre-test to post-test for the DN and the STT groups after the intervention (P<0.001) (Table 2). Furthermore, the mean PPT of UT, SCM, and sub-occipital muscles increased from before treatment to after treatment in the DN and the STT groups (P<0.001) (Table 2).
Also, the mean CROM scores increased from before treatment to after treatment in the DN and the STT group (P<0.001) (Table 2).
Within-group effects sizes for both groups were found to be large (d>1) in all outcomes.
Between-group comparison of the outcome measurements
The findings of independent t test revealed the soft tissue technique decreased the pain intensity (T=3.23, P=0.003) and the NDI (T=5.52, P<0.001) more than dry needling (Table 2). However, no significant difference was found between the two groups in any other outcome variables (Table 2).
Discussion
To our knowledge, this is the first study that has compared the effect of dry needling and soft tissue technique on changes in the migraine headache symptoms. Both treatments were performed on MTrPs in the UT, SCM and sub-occipital muscles. The results showed that both methods had similar effects in patients with migraine headache; however, soft tissue technique decreased the pain intensity and neck disability more than the dry needling method. Furthermore, there was no significant difference in increasing the PPT and CROM between the two groups after treatment. This study is novel because previous studies have been evaluated the effectiveness of these two treatments in patients with migraine headache separately and no studies have compared the two techniques in these patients. These findings support previous studies that determined the soft tissue techniques and massage as one of the therapeutic options to improve symptoms in migraine patients [6,15,30,31] and those with other types of headaches [14,32,33]. They reported that massage and myofascial release improve the symptoms in migraine headache patients. On the other hand, Hesse et al [34] indicated that the trigger point inactivation by dry needling was equipotent to medicine therapy about the improvement of symptoms in migraine patients. Sedighi et al [35] reported that the application of the DN into trigger points of sub-occipital and UT muscles improve outcomes of headache index, trigger points tenderness, functional rating index, and ROM in patients with cervicogenic headache. Furthermore, a systematic review of the use of the DN in the treatment of MTrPs stated that the DN compared to sham intervention can have a short term effect on pain, ROM and quality of life [36]. However, the current study results gave confirmatory evidence in agreement with these studies.
Various theories try to explain the pathophysiology of trigger points. Muscle overload due to repeated and prolonged activities and low levels of muscle contraction may cause changes in muscle fiber, local stiffness, and blood flow properties of the biochemical environment [28]. According to Simons [17], the use of slow, prolonged passive stretching with a progressively increase in ROM, as used in the current study, appears to inhibit alpha motor neurons response and inhibition of shortened muscle fibers when stretched. These techniques restore the normal length of the muscle sarcomeres and elongate the muscle fiber [17]. Furthermore, STTs helped in breaking adhesions, increasing blood flow and lymphatic drainage to deactivate trigger points and increase soft tissue extensibility which improved range of motion and thus muscle strength [37]. We hypothesize that a greater change in pain intensity and neck disability following the soft tissue application maybe attributed to the elongation of the muscle to its full normal length and being non-invasive of this therapeutic mode. Our study supported the idea that muscle stretching provided pain relief, improvement of disability and increased CROM and PPT in the soft tissue group. Thus, stretching the muscle after TrPs treatment is necessary to provide longer pain relief. The reduction of pain intensity and neck disability after dry needling may be attributable to the various mechanisms, such as mechanical, neurophysiologic, and chemical effects [38]. It was thought that mechanical effects of the DN method might improve the fiber structure, the localized tissue stiffness, and the local circulation of the biochemical milieu associated with the trigger point [38]. However, in this study, we did not measure the chemical and neurophysiological responses in the subjects following the application of the DN.
As previously mentioned, the migraine patients is associated with reduction in CROM and increased sensitivity on the cervical muscles [3,5]. Therefore, the effective management of these problems is of particular importance. This study reported both of therapeutic methods increased CROM and PPT in these patients. In line with the current study, Kamali et al. [39] compared the effectiveness of dry needling and friction massage to treat patients with tension type headache. They reported that both treatment methods significantly increased CROM and PPT at the trigger points [39]. Hou et al. [40] had shown ROM and PPT improvement with stretching associated with other types of interventions in the presence of MTrPs.
Our data showed no significant difference in the PPT and CROM between the two groups after treatment, which can be explained by small sample size and the small between-group differences (Tables 2 and 3). Studies with larger sample sizes or longer treatment durations may reveal important differences between the two treatment methods in their effect on PPT and CROM.
Clinical relevance and future studies
Despite the lack of significant differences between two groups, pain intensity and functional disability differences following soft tissue technique intervention seemed to improve more than dry needling method after treatment and may clinically improve headache associated with MTrPs in the cervical muscle. Further studies are necessary to clarify our findings relative to a control group without treatment. Future studies should consider evaluating the effect of two interventions in conjunction with drug therapy, exercises or manipulation, and include a control group without intervention.
Study limitation
However, we acknowledge several limitations. In this study, only the specific muscles were evaluated and other cervical muscles may be involved in migraine headache patients. Hence, the results shouldn’t be generalized to all subjects with migraine headache. Also this study didn’t focus on the effect of psychosocial factors, which may set intermediating effect. The short duration of therapy was one of the limitations of this study.
Conclusion
The results of this study showed that dry needling and soft tissue techniques produce an improvement in the scores of the VAS, NDI, PPT, and CROM in the migraine patients. However, VAS and NDI scores decreased significantly after soft tissue technique more than the dry needling. According to this result, soft tissue technique is recommended as an effective therapeutic option for the treatment of migraine headache patients with active TrPs in identifiable muscles.
Acknowledgement
This article was extracted from the Iranian Registry Clinical Trial (IRCT) number IRCT 20171219037956N1 which was supported by the University of Social Welfare and Rehabilitation Sciences. We gratefully acknowledge the individuals who participated in this study.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Conflict of Interest
There is no conflict of interest.
29714
References
- Stovner L, Hagen K, Jensen R, Katsarava Z, Lipton RB, et al. (2007) The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 27: 193-210.
- Olesen J, Burstein R, Ashina M, Tfelt-Hansen P (2009) Origin of pain in migraine: evidence for peripheral sensitisation. Lancet Neurol 8: 679-690.
- Calandre EP, Hidalgo J, García‐Leiva JM, Rico‐Villademoros F (2006) Trigger point evaluation in migraine patients: an indication of peripheral sensitization linked to migraine predisposition? Eur J Neurol 13: 244-249.
- Tali D, Menahem I, Vered E, Kalichman L (2014) Upper cervical mobility, posture and myofascial trigger points in subjects with episodic migraine: case-control study. J Bodyw Mov Ther 18: 569-575.
- Fernández-de-Las-Peñas C, Cuadrado ML, Pareja JA (2006) Myofascial trigger points, neck mobility and forward head posture in unilateral migraine. Cephalalgia 26: 1061-1070.
- Ghanbari A, Askarzadeh S, Petramfar P, Mohamadi M (2015) Migraine responds better to a combination of medical therapy and trigger point management than routine medical therapy alone. NeuroRehabilitation 37: 157-163.
- Scotece G (1998) Chronic Pain Management for Physical Therapists. Physical Therapy 78: 435.
- Mense S (1993) Nociception from skeletal muscle in relation to clinical muscle pain. Pain 54: 241-289.
- Shah JP, Danoff JV, Desai MJ, Parikh S, Nakamura LY, et al. (2008) Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil 89: 16-23.
- Ong J, Claydon LS (2014) The effect of dry needling for myofascial trigger points in the neck and shoulders: a systematic review and meta-analysis. J Bodyw Mov Ther 18: 390-398.
- Rayegani SM, Bayat M, Bahrami MH, Raeissadat SA, Kargozar E (2014) Comparison of dry needling and physiotherapy in treatment of myofascial pain syndrome. Clin Rheumatol 33: 859-864.
- Gerber LH, Shah J, Rosenberger W, Armstrong K, Turo D, et al. (2015) Dry needling alters trigger points in the upper trapezius muscle and reduces pain in subjects with chronic myofascial pain. PM R 7: 711-718.
- Szikszay TM (2017) Effectiveness of a Treatment Involving Soft Tissue Techniques and/or Neural Mobilization Techniques in the Management of Tension-Type Headache: A Randomized Controlled Trial. Physioscience 13: 186-187.
- Ferragut-Garcías A, Plaza-Manzano G, Rodríguez-Blanco C, Velasco-Roldán O, Pecos-Martín D, et al. (2017) Effectiveness of a treatment involving soft tissue techniques and/or neural mobilization techniques in the management of tension-type headache: a randomized controlled trial. Arch Phys Med Rehabil 98: 211-219. e2.
- Espí-López GV, Ruescas-Nicolau MA, Nova-Redondo C, Benítez-Martínez JC, Dugailly PM, et al. (2018) Effect of soft tissue techniques on headache impact, disability, and quality of life in migraine sufferers: a pilot study. J Altern Complement Med 24: 1099-1107.
- Kietrys DM, Palombaro KM, Azzaretto E, Hubler R, Schaller B, et al. (2013) Effectiveness of dry needling for upper-quarter myofascial pain: a systematic review and meta-analysis. J Orthop Sports Phys Ther 43: 620-634.
- Simons DG (2008) New views of myofascial trigger points: etiology and diagnosis. Arch Phys Med Rehabil 89: 157-159.
- Simons DG (2002) Understanding effective treatments of myofascial trigger points. Journal of Bodywork and Movement Therapies 6: 81-88.
- Chaitow L, Delany J (2008) Clinical application of neuromuscular techniques: The upper body, Shoulder, arm and hand. Elsevier, London.
- Fernández-de-las-Peñas C (2013) Trigger Point Dry Needling: An Evidence and Clinical-based Approach. Churchill Livingstone.
- Simons DG, Travell J, Simons LS (1999) Myofascial pain and dysfunction: the trigger point manual.
- Hong CZ (1994) Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. American journal of physical medicine & rehabilitation 73: 256-263.
- Lari AY, Okhovatian F, Naimi SS, Baghban AA (2016) The effect of the combination of dry needling and MET on latent trigger point upper trapezius in females. Man Ther 21: 204-209.
- Hsieh YL, Kao MJ, Kuan TS, Chen SM, Chen JT, et al. (2007) Dry needling to a key myofascial trigger point may reduce the irritability of satellite MTrPs. Am J Phys Med Rehabil 86: 397-403.
- Carlsson AM (1983) Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 16: 87-101.
- Vernon H (2008) The Neck Disability Index: state-of-the-art, 1991-2008. J Manipulative Physiol Ther 31: 491-502.
- Mousavi SJ, Parnianpour M, Montazeri A, Mehdian H, Karimi A, et al. (2007) Translation and validation study of the Iranian versions of the Neck Disability Index and the Neck Pain and Disability Scale. Spine 32: E825-E831.
- Tsai CT, Hsieh LF, Kuan TS, Kao MJ, Chou LW, et al. (2010) Remote effects of dry needling on the irritability of the myofascial trigger point in the upper trapezius muscle. Am J Phys Med Rehabil 89: 133-140.
- Fletcher JP, Bandy WD (2008) Intrarater reliability of CROM measurement of cervical spine active range of motion in persons with and without neck pain. J Orthop Sports Phys Ther 38: 640-645.
- Bevilaqua-Grossi D, Gonçalves MC, Carvalho GF, Florencio LL, Dach F, et al. (2016) Additional effects of a physical therapy protocol on headache frequency, pressure pain threshold, and improvement perception in patients with migraine and associated neck pain: A randomized controlled trial. Arch Phys Med Rehabil 97: 866-874.
- Chatchawan U, Eungpinichpong W, Sooktho S, Tiamkao S, Yamauchi J (2014) Effects of Thai traditional massage on pressure pain threshold and headache intensity in patients with chronic tension-type and migraine headaches. J Altern Complement Med 20: 486-492.
- Espí-López GV, Gómez-Conesa A, Gómez AA, Martínez JB, Pascual-Vaca AO, et al. (2014) Treatment of tension-type headache with articulatory and suboccipital soft tissue therapy: A double-blind, randomized, placebo-controlled clinical trial. J Bodyw Mov Ther 18: 576-585.
- Bodes-Pardo G, Pecos-Martín D, Gallego-Izquierdo T, Salom-Moreno J, Fernández-de-Las-Peñas C, et al. (2013) Manual treatment for cervicogenic headache and active trigger point in the sternocleidomastoid muscle: a pilot randomized clinical trial. J Manipulative Physiol Ther 36: 403-411.
- Hesse J, Møgelvang B, Simonsen H (1994) Acupuncture versus metoprolol in migraine prophylaxis: a randomized trial of trigger point inactivation. Journal of Internal Medicine 235: 451-456.
- Sedighi A, Ansari NN, Naghdi S (2017) Comparison of acute effects of superficial and deep dry needling into trigger points of suboccipital and upper trapezius muscles in patients with cervicogenic headache. J Bodyw Mov Ther 21: 810-814.
- Espejo-Antúnez L, Tejeda JFH, Albornoz-Cabello M, Rodríguez-Mansilla J, de la Cruz-Torres B, et al. (2017) Dry needling in the management of myofascial trigger points: A systematic review of randomized controlled trials. Complement Ther Med 33: 46-57.
- Saratchandran R, Desai S (2013) Myofascial release as an adjunct to conventional occupational therapy in mechanical low back pain. Indian J Occup Ther 45: 3-7.
- Dommerholt J, Grieve R, Layton M, Hooks T (2015) An evidence-informed review of the current myofascial pain literature–January 2015. J Bodyw Mov Ther 19: 126-137.
- Kamali F, Mohamadi M, Fakheri L, Mohammadnejad F (2019) Dry needling versus friction massage to treat tension type headache: a randomized clinical trial. J Bodyw Mov Ther 23: 89-93.
- Hou CR, Tsai LC, Cheng KF, Chung KC, Hong CZ (2002) Immediate effects of various physical therapeutic modalities on cervical myofascial pain and trigger-point sensitivity. Arch Phys Med Rehabil 83: 1406-1414.