Key words
Drug dependence, addiction, dual diagnosis, comorbidity, rehabilitation, relapse prevention
Introduction
Individuals who are addicted to a legal or illegal drug often may also qualify for other co-occurring mental health disorder and vice versa. The comorbidity of drug dependence with a non-dependency mental disorder is consistently higher than 50% in clinical populations [1-3] but also remains high reaching 17% in general samples. [4] In some populations the comorbidity of substance misuse has been estimated to reach 90% [5,6] of the mentally disordered population, revealing that at least in some clinical populations dual diagnosis undoubtedly cannot be disregarded, whereas some authors describe dual diagnosis as being the rule and not the exception. [7,8]
Factors contributing to this comorbidity appear to be shared genetic vulnerability, [9,10] developmental processes [11] and/or psychosocial adversities, [9] as well as a possible causality relationship between drugs and mental disorder and vice versa. [12] The direction of the latter correlation has been shown to be from mental disorder to drugs, [12-15] or the opposite, [16-18] but these data do not exclude a possible reciprocal relationship, or in some cases no causal relationship but simple independent coexistence. Current neuroimaging data show that users of cocaine, heroin, inhalants, as well as cannabis, develop anatomical and functional white matter impairment, that are correlated with cognitive, affective and behavioural changes. [19-24] Drug users may have increased risk for developing mental disorder. [16-18] Reversing the time sequence, individuals with a mental disorder may have increased risk for becoming drug users. [12,25,26] Patients with psychosis may abuse substances in order to alleviate negative symptomatology, or the negative symptoms may be a predisposing factor for drug abuse and dependence. [27] Patients with psychosis not only have an increased risk for problematic use of alcohol, cannabis, stimulants, but also for heroin. [12] Depression is also correlated with substance abuse, even depression in schizophrenia. [28] An interesting epidemiological finding is that anxiety disorders usually start at an earlier age than drug dependence, whereas depression usually starts at an older age than drug dependence from legal or illegal substances. [25] Anxious patients commonly use drugs as a way to self-treat their symptomatology, [29,30] and the negative consequences of self-medication, such as worst mental health despite higher usage of mental health services, has been underlined. [14] In addition personality traits have also been found to play a role in substance use. More specifically, the trait of neuroticism as described by five-factor model as well as cluster B characteristics in DSM-IV-TR, seem to play the more significant role. [31-34] Personality traits are also affecting substance selection. [35,36]
In any case, from a clinical point of view dually diagnosed populations do need increased care [37] to the point that even special diagnostic criteria for dual diagnosis has been requested as being necessary in order to ensure best clinical practice. [38] The classical approach to managing these patients has been to treat the disorder with the most dominant clinical picture. [39,40] Nevertheless, currently there is increasing evidence for providing integrative care in dually diagnosed populations, namely for treating these patients in one setting with therapists from the same multidisciplinary team. [41-46]
In both dominant diagnostic systems, ICD-10 and DSM-IV-TR as well as in the upcoming DSM-5, drug dependence is considered to be a chronic axis-I mental health disorder. In this context, the comorbidity of two chronic mental health conditions, namely drug dependence and another axis-I or axis-II disorder, has traditionally been defined as dual diagnosis, even though some authors prefer to keep this term for use only in cases of drug dependency with co-occurring severe psychotic or mood disorder. Despite the fact that the concept of dual diagnosis is progressively replaced by comorbidity, [8] in this study we keep using the term in order to underline the difficulties in treating mentally disordered patients with comorbid substance abuse and/or dependence. In any case, dual diagnosis is correlated with difficulties in treatment, prolongation of the duration of disorders, [14] and a possible worsening of the prognosis.
The aim of this study was to explore whether dually diagnosed patients under integrative treatment have different prognosis compared to drug-dependent patients without a comorbid disorder, with both populations participating into the same therapeutic program, under the care of the same multidisciplinary team.
Methods
Participants
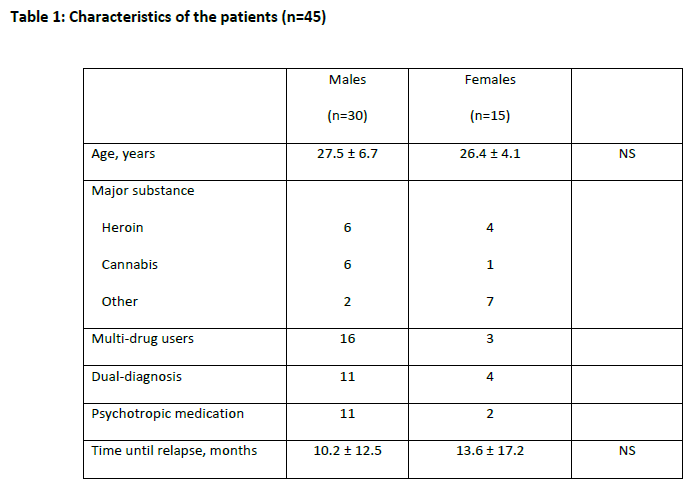
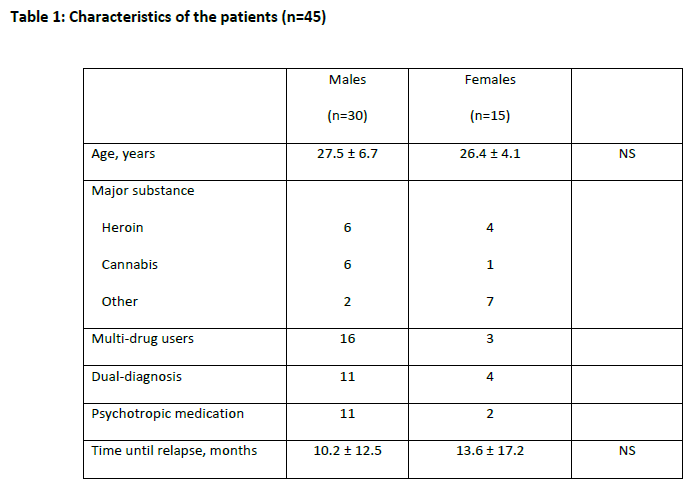
Forty-five consecutive drug-dependent adult patients took part in this study (table 1).
The main outcome considered was retention in treatment, measured in months for the purposes of the analysis. All patients entered voluntarily the treatment program after informed consent, and no patient has been involuntarily treated under section. The study was approved by the ethics committee of the affiliated institutions. No allocation into groups took place, and all patients received the standard care provided.
Treatment offered
The therapeutic program was based on a modified therapeutic community (TC) model [47,48] for drug dependent populations, that incorporates both a residential and an outpatient part in one treatment community, including the drug dependent as well as the dually diagnosed patients. [49] The therapeutic model was also inspired from milieu therapy [50,51] and contingency management approach. [52-55] No methadone or buprenorphine users was accepted in this facility, which were abstinence oriented, despite the fact that opiate substitute receivers could normally admitted into modified TCs. [47,56]
Inclusion criteria
Forty-five consecutive patients with substance dependency entered the study. All of these patients took part in the same treatment program for drug users, with or without dual diagnosis. In order to enter the therapeutic program the patients had to 1)be older than 18 years old, 2)be abstinent from illegal drugs of dependence and alcohol for the 15 last days at least, 3)be highly motivated for treatment as confirmed in 3 initial appointments with a special nurse before entering the program, 4)have a present mental state examination by a Psychiatrist and a Clinical Psychologist in order to exclude or confirm mental health comorbidity, and to exclude mental disability and/organic brain damage eg post-traumatic.
Statistical analysis
After descriptive statistics and correlation analysis, time-to-event as well as univariate and multivariate Cox regression analysis was conducted in order to explore for significant effects of gender, age, and multiple-drug dependence, on time to relapse. Time-to-event and Cox regression analyses conducted according to published methodology. [57] All statistical procedures were performed using the SPSS Statistics version 17.0 (SPSS Inc, Chicago Ill.).
Results
Between gender comparison for difference in age by using t-test showed no significant difference (table 1). Also there was no between gender significant difference in time until relapse (table 1). Correlation analysis did not reveal any significant correlation between time until relapse or retention in treatment and age or gender of the patient, category of the substance, multi-drug use, prescribed psychotropic medication use.
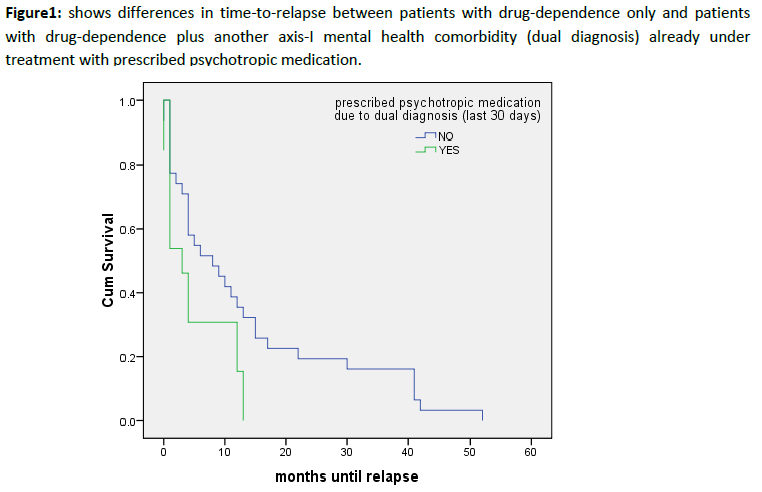
Time-to-event analysis showed differences (figure 1) in time to relapse between the group of drug dependence only and the group of the patients with a comorbid axis-I and/or axis-II mental health disorder (Log Rank Mantel-Cox test shown Chi-Square: 4.52, df=1, p< .05)
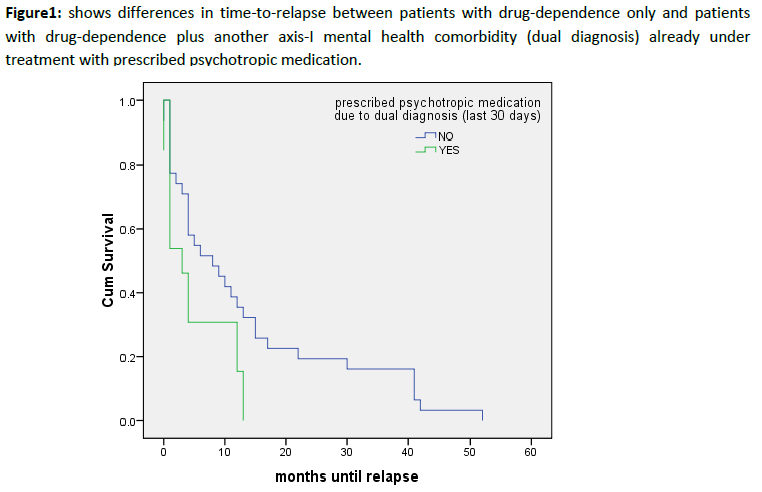
Figure 1: shows differences in time-to-relapse between patients with drug-dependence only and patients with drug-dependence plus another axis-I mental health comorbidity (dual diagnosis) already under treatment with prescribed psychotropic medication.
Univariate and multivariate Cox-regression analysis did not show any significant effects of gender, age, multiple-drug dependence, on time to relapse.
Discussion
Dually diagnosed participants in our study, even though they received integrative treatment, showed poorer prognosis compared to drug dependent only population, when retention in treatment was used as the endpoint for between groups comparison. Other studies also found dual diagnosis to be a poor prognostic factor when compliance or adherence to treatment [58-61] and/or time until relapse and rehospitalisation [58-60,62,63] were used as the endpoint. This finding is also consistent in studies that used other relative endpoints such as the symptom severity, [58-61,64,65] as well as illness duration. [58,61,64] Other authors that also found dual diagnosis to be a poor prognostic factor for relapse, underline that even when concomitant psychotropic medication treatment is used this is still not associated with successful participation in the treatment program. [66] This is also in agreement with our results, even though separate analysis for each mental health disorder category and/or substance category were not possible due to the inadequate sample size.
In our sample, most of participants with dual diagnosis, and predicted shorter time until relapse, were diagnosed with mood or anxiety disorder. A meta-analysis, that retrospectively explored for predictors for continued drug use during and after treatment, also showed depression and anxiety to be significant variables [63] for predicting relapse, even though this meta-analysis included population restricted in opiate users only. These diagnoses are common comorbidities in dually diagnosed drug dependent populations, as well as in our sample in which also consist predictors of worse prognosis.
In this dually diagnosed patients providing integrative care meaning that they were receiving concomitant treatment in the same setting integrated for both disorders, and not only treatment for drug dependence and referring or leaving the patient to navigate the health system in order to join other clinic for treating mental health disorder as was the usual practice in the past. [39,40,95] Integration of treatment has been suggested as best practise in treating different populations of dually diagnosed patients [43-46,95-98] Integrative treatment is also suggested by in practise guidelines, [99] and it is considered the cost-effective approach in dually diagnosed patient management. [100] A possible explanation for this is that a multidisciplinary team is more effective when caring for both the mental disorder and drug dependency as it deals with the patient in a more holistic, biopsychosocial approach. Other possible explanation could be the facilitation for the patient who does not have to navigate anymore in different treatment settings and to deal with different therapists as well as therapeutic approaches.
Despite the advantages of integrative treatment provided, dually diagnosed population still showed worse prognosis. All participants in our study received integrated treatment consisting of interventions based on group behavioural interventions inspired from the abstinence-focused therapeutic community (TC) model, as well as pharmacotherapy when necessary for mental health comorbidities, under the care of a psychiatrist, individualised psychosocial interventions as designed by a multidisciplinary team consisting of a psychiatrist, nurses, addiction counsellors, an occupational therapist, and a social worker. A meta-analysis that explored the effects of psychosocial treatments in dually diagnosed populations, to reduce substance use or to improve mental health, found no compelling evidence to support any one individual psychosocial treatment compared to the others. [67] These findings generate questions regarding how to increase the effectiveness of treatment programs that include dually diagnosed patients. Relative studies also explored the effectiveness of abstinence oriented therapeutic communities (TC) based approach, in a community based or residential setting, for treating dual diagnosis and drug dependent only population found variable results, [68-72] even when including modified therapeutic communities that are open to admiting patients who receive opiod substitutes’ maintenance treatment. [56,73] A recent meta-analysis that was conducted in order to determine the overall effect of abstinence focused-therapeutic communities (TCs), found that there is a little evidence that TCs offer significant benefits, in comparison with other residential treatment, or that one type of TCs is better than another. [74]
Apart from the fact that abstinence oriented communities are not considered an adequately effective treatment for some populations, [74] there are also arise many questions regarding the safety of abstinence oriented therapeutic interventions in general. [75-79] This arises on the basis that patients who successfully completed detoxification were more likely than other patients to have died during the following year, compared to patients who failed to complete detoxification and remained in use. [78] Recent research revealing promising evidence regarding the efficacy of non-abstinence oriented TCs admitting patients receiving opiate substitutes, [47,56] but no other findings regarding substitutes of substances other than opiates have been published yet. This results have to be cautiously interpreted under the prism of studies arising adding evidence on harm reduction approach promising effectiveness, [47,56,80,81] even in the difficult to treat dually diagnosed populations. [82-86]
In our abstinence oriented program dually diagnosed patients stayed less time into treatment meaning that they show an earlier relapse. There were no control group in this study to compare prognosis between dually diagnosed in abstinence and dually diagnosed in treatment with substitutes. Consequently, a question remains if substitutes could decrease or eliminate the difference in effectiveness and prognosis, in an integrative care program. Despite this limitation, it cannot be disregarded that abstinence focused programs have been shown to be ineffective for some populations, and in addition its safety is questioned. Recently, there is some evidence that harm reduction approaches could help dually diagnosed population. In our study abstinence from any illegal substance as well as alcohol was a prerequisite for patients in order to enter and remain in the integrative treatment program. Harm reduction approaches were not incorporated in this study protocol, due to treatment design, inadequate training and consequent inability to apply, meaning that neither treatment work with active users took place in the treatment setting nor patients under treatment with substitutes were admitted, despite some promising published results of harm reduction practises in dually diagnosed populations. [82-87] A recent meta-analysis showed only low evidence supporting the effectiveness of antidepressants in heroin addicts under opiod agonist treatment, with comorbid depression. A recent study showed a better long-term prognosis for dual-diagnosed patients when treated with opiate substitutes. [88] Harm reduction includes treatment approaches that do not require abstinence from the substance but are focused on reducing the harm in biological/somatic health aspect, achieving psychosocial stability and increasing functionality. At the same time abstinence from the substance is desirable but not mandatory. There is increasing evidence that harm reduction approaches are effective in dually diagnosed populations when patients are dependent in legal [89-91] or illegal substances, [92,93] as well as when the comorbidity includes a psychotic [83,92,93] or a non-psychotic [84,94] mental disorder.
To the knowledge of the authors this is the first study comparing intervention effectiveness, as a means of retention in treatment, between dually diagnosed and drug dependent only patients, receiving TC inspired integrated care in a common setting by the same multidisciplinary team. Some important limitations decrease the power and generalisability of the findings, generating interesting questions for future researchers in the field: 1) No structured diagnostic interview was used for the diagnosis of comorbidity. Diagnosis of comorbidity took place after clinical interviews from a Psychiatrist and a Clinical Psychologist. Nevertheless, in the case of disagreement, diagnosis was detailed discussed between them. 2) a small sample size precluded the between gender and/or between category of the substance comparisons 3) there was no control group of patients receiving non-integrating care, neither control group of patients receiving care while they were under active use of the substance or under treatment with substitutes.
Dual diagnosis is a special form of mental disorders comorbidity that could worsen prognosis either in a setting of integrating provided care. The term “dual diagnosis” in relevant medical literature is being partly replaced by the concept of comorbidity. Authors still use it in current bibliography in order to focus in a special case of comorbidity that includes a difficult drug dependent patient with another non-dependent mental disorder, that needs special attention. Taking into account the limitations of abstinence oriented therapeutic programs, even the integrative ones, a need arises for incorporation of more harm reduction approaches into the integrating –community or residential- treatment setting. There is a need for clinical education and research in this field, in order to reduce the harm and rehabilitate difficult to treat dually diagnosed patients.
2739
References
- Lehman AF, Myers CP, Corty E, Thompson JW. Prevalence and patterns of "dual diagnosis" among psychiatric inpatients. Compr Psychiatry. 1994;35(2):106-12.
- Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. Am J Orthopsychiatry. 1996;66(1):17-31.
- Kessler RC. The epidemiology of dual diagnosis. Biol Psychiatry. 2004;56(10):730-7.
- Vega WA, Canino G, Cao Z, Alegria M. Prevalence and correlates of dual diagnoses in US Latinos. Drug and alcohol dependence. 2009;100(1-2):32-8.
- Emmelkamp PMG, Vedel E. Evidence-based treatment for alcohol and drug abuse: a practitioner's guide to theory, methods, and practice: Brunner-Routledge; 2006.
- Strakowski SM, DelBello MP. The co-occurrence of bipolar and substance use disorders. Clinical Psychology Review. 2000;20(2):191-206.
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-8.
- Cosci F, Fava G. New clinical strategies of assessment of comorbidity associated with substance use disorders. Clinical Psychology Review. 2011;31(3):418-27.
- Comtois KA, Tisdall WA, Holdcraft LC, Simpson T. Dual diagnosis: impact of family history. Am J Addict. 2005;14(3):291-9.
- Zuo L, Gelernter J, Kranzler HR, Stein MB, Zhang H, Wei F, et al. ADH1A variation predisposes to personality traits and substance dependence. Am J Med Genet B Neuropsychiatr Genet. 2010;153B(2):376-86.
- Chambers RA, Sentir AM, Conroy SK, Truitt WA, Shekhar A. Cortical-striatal integration of cocaine history and prefrontal dysfunction in animal modeling of dual diagnosis. Biol Psychiatry. 2010;67(8):788-92.
- Pedersen K, Waal H, Kringlen E. Patients with nonaffective psychosis are at increased risk for heroin use disorders. Eur Addict Res. 2012;18(3):124-9.
- Sareen J, Chartier M, Kjernisted KD, Stein MB. Comorbidity of phobic disorders with alcoholism in a Canadian community sample. Can J Psychiatry. 2001;46(8):733-40.
- Robinson JA, Sareen J, Cox BJ, Bolton JM. Correlates of self-medication for anxiety disorders: results from the National Epidemiolgic Survey on Alcohol and Related Conditions. The Journal of nervous and mental disease. 2009;3(12):873.
- Zimmermann P, Wittchen H, Hofler M, Pfister H, Kessler R, Lieb R. Primary anxiety disorders and the development of subsequent alcohol use disorders: a 4-year community study of adolescents and young adults. Psychological Medicine. 2003;33(7):1211-22.
- Allebeck P, Adamsson C, Engström A. Cannabis and schizophrenia: a longitudinal study of cases treated in Stockholm County. Acta Psychiatrica Scandinavica. 1993;88(1):21-4.
- Andréasson S, Allebeck P, Rydberg U. Schizophrenia in users and nonusers of cannabis. Acta Psychiatrica Scandinavica. 1989;79(5):505-10.
- Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. Journal of Psychopharmacology. 2005;19(2):187-94.
- Romero MJ, Asensio S, Palau C, Sanchez A, Romero FJ. Cocaine addiction: diffusion tensor imaging study of the inferior frontal and anterior cingulate white matter. Psychiatry Res. 2010;181(1):57-63.
- Lim KO, Wozniak JR, Mueller BA, Franc DT, Specker SM, Rodriguez CP, et al. Brain macrostructural and microstructural abnormalities in cocaine dependence. Drug and alcohol dependence. 2008;92(1-3):164-72.
- Warner TD, Behnke M, Eyler FD, Padgett K, Leonard C, Hou W, et al. Diffusion tensor imaging of frontal white matter and executive functioning in cocaine-exposed children. Pediatrics. 2006;118(5):2014-24.
- Shen Y, Wang E, Wang X, Lou M. Disrupted Integrity of White Matter in Heroin-addicted Subjects at Different Abstinent Time. J Addict Med. 2012.
- Yucel M, Zalesky A, Takagi MJ, Bora E, Fornito A, Ditchfield M, et al. White-matter abnormalities in adolescents with long-term inhalant and cannabis use: a diffusion magnetic resonance imaging study. J Psychiatry Neurosci. 2010;35(6):409-12.
- Solowij N, Yucel M, Respondek C, Whittle S, Lindsay E, Pantelis C, et al. Cerebellar white-matter changes in cannabis users with and without schizophrenia. Psychol Med. 2011;41(11):2349-59.
- Christie KA, Burke JD, Jr., Regier DA, Rae DS, Boyd JH, Locke BZ. Epidemiologic evidence for early onset of mental disorders and higher risk of drug abuse in young adults. Am J Psychiatry. 1988;145(8):971-5.
- Hesselbrock MN, Meyer RE, Keener JJ. Psychopathology in hospitalized alcoholics. Arch Gen Psychiatry. 1985;42(11):1050-5.
- Potvin S, Sepehry AA, Stip E. A meta-analysis of negative symptoms in dual diagnosis schizophrenia. Psychol Med. 2006;36(4):431-40.
- Potvin S, Sepehry AA, Stip E. Meta-analysis of depressive symptoms in dual-diagnosis schizophrenia. Aust N Z J Psychiatry. 2007;41(10):792-9.
- Bibb JL, Chambless DL. Alcohol use and abuse among diagnosed agoraphobics. Behav Res Ther. 1986;24(1):49-58. Epub 1986/01/01.
- Klein DF. Anxiety reconceptualized. Compr Psychiatry. 1980;21(6):411-27.
- Dolan SL, Bechara A, Nathan PE. Executive dysfunction as a risk marker for substance abuse: the role of impulsive personality traits. Behav Sci Law. 2008;26(6):799-822.
- Ruiz MA, Pincus AL, Schinka JA. Externalizing pathology and the five-factor model: a meta-analysis of personality traits associated with antisocial personality disorder, substance use disorder, and their co-occurrence. J Pers Disord. 2008;22(4):365-88.
- Kotov R, Gamez W, Schmidt F, Watson D. Linking "big" personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol Bull. 2010;136(5):768-821. Epub 2010/09/02.
- Mueller A, Claes L, Mitchell JE, Wonderlich SA, Crosby RD, de Zwaan M. Personality prototypes in individuals with compulsive buying based on the Big Five Model. Behav Res Ther. 2010;48(9):930-5.
- Conway KP, Kane RJ, Ball SA, Poling JC, Rounsaville BJ. Personality, substance of choice, and polysubstance involvement among substance dependent patients. Drug Alcohol Depend. 2003;71(1):65-75..
- Conway KP, Swendsen JD, Rounsaville BJ, Merikangas KR. Personality, drug of choice, and comorbid psychopathology among substance abusers. Drug Alcohol Depend. 2002;65(3):225-34.
- Baigent M. Managing patients with dual diagnosis in psychiatric practice. Current Opinion in Psychiatry. 2012;25(3):201.
- Hryb K, Kirkhart R, Talbert R. A call for standardized definition of dual diagnosis. Psychiatry (Edgmont). 2007;4(9):15.
- Todd J, Green G, Harrison M, Ikuesan BA, Self C, Baldacchino A, et al. Defining dual diagnosis of mental illness and substance misuse: some methodological issues. J Psychiatr Ment Health Nurs. 2004;11(1):48-54.
- Todd J, Green G, Harrison M, Ikuesan BA, Self C, Pevalin DJ, et al. Social exclusion in clients with comorbid mental health and substance misuse problems. Soc Psychiatry Psychiatr Epidemiol. 2004;39(7):581-7.
- Gaillard Wasser J, Dunker Scheuner D, Gammeter R, Daeppen JB. Assessment and treatment of coexisting mental illness or dual diagnosis. Rev Med Suisse. 2005;1(26):1750-4. Prise en charge des patients "double diagnostic": comment sortir du carrousel institutionnel?
- Manley D. Dual diagnosis: co-existence of drug, alcohol and mental health problems. Br J Nurs. 2005;14(2):100-6.
- Farrell M, Marshall EJ. Organization and delivery of treatment services for dual diagnosis. Psychiatry. 2007;6(1):34-6.
- Ridgely MS, Goldman HH, Willenbring M. Barriers to the care of persons with dual diagnoses: organizational and financing issues. Schizophr Bull. 1990;16(1):123-32..
- Drake RE, Morrissey JP, Mueser KT. The challenge of treating forensic dual diagnosis clients: comment on "integrated treatment for jail recidivists with co-occurring psychiatric and substance use disorders". Community Ment Health J. 2006;42(4):427-32.
- Drake RE, Mercer-McFadden C, Mueser KT, McHugo GJ, Bond GR. Review of integrated mental health and substance abuse treatment for patients with dual disorders. Schizophr Bull. 1998;24(4):589-608.
- Bunt GC, Muehlbach B, Moed CO. The Therapeutic Community: an international perspective. Subst Abus. 2008;29(3):81-7.
- Fussinger C. [Elements for an history of the therapeutic community in Western psychiatry of the 2nd half of the 20th century] . Gesnerus. 2010;67(2):217-40. Epub 2010/01/01. Elements pour une histoire de la communaute therapeutique dans la psychiatrie occidentale de la seconde moitie du 20e siecle.
- Sacks S, McKendrick K, Sacks JY, Cleland CM. Modified therapeutic community for co-occurring disorders: single investigator meta analysis. Subst Abus. 2010;31(3):146-61.
- Wolf MS. A review of literature on milieu therapy. J Psychiatr Nurs Ment Health Serv. 1977;15(5):27-33.
- Moline RA. The therapeutic community and milieu therapy: a review and current assessment. Community Ment Health Rev. 1977;2(5):1:3-13.
- Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: a meta-analysis. Addiction. 2006;101(11):1546-60.
- Specka M, Boning A, Scherbaum N. Contingency management in opioid substitution treatment. Fortschr Neurol Psychiatr. 2011;79(7):395-403.
- Stitzer M, Petry N. Contingency management for treatment of substance abuse. Annu Rev Clin Psychol. 2006;2:411-34.
- Stitzer ML, Vandrey R. Contingency management: utility in the treatment of drug abuse disorders. Clin Pharmacol Ther. 2008;83(4):644-7.
- Sorensen JL, Andrews S, Delucchi KL, Greenberg B, Guydish J, Masson CL, et al. Methadone patients in the therapeutic community: a test of equivalency. Drug Alcohol Depend. 2009;100(1-2):100-6.
- Chan Y. Biostatistics 203. Survival analysis. Singapore medical journal. 2004;45:249-56.
- Drake RE, Osher FC, Wallach MA. Alcohol use and abuse in schizophrenia. A prospective community study. J Nerv Ment Dis. 1989;177(7):408-14.
- Osher FC, Drake RE, Noordsy DL, Teague GB, Hurlbut SC, Biesanz JC, et al. Correlates and outcomes of alcohol use disorder among rural outpatients with schizophrenia. J Clin Psychiatry. 1994;55(3):109-13.
- Swofford CD, Kasckow JW, Scheller-Gilkey G, Inderbitzin LB. Substance use: a powerful predictor of relapse in schizophrenia. Schizophr Res. 1996;20(1-2):145-51.
- Kokkevi A, Stefanis N, Anastasopoulou E, Kostogianni C. Personality disorders in drug abusers: prevalence and their association with AXIS I disorders as predictors of treatment retention. Addict Behav. 1998;23(6):841-53.
- Linszen DH, Dingemans PM, Lenior ME. Cannabis abuse and the course of recent-onset schizophrenic disorders. Arch Gen Psychiatry. 1994;51(4):273-9.
- Brewer DD, Catalano RF, Haggerty K, Gainey RR, Fleming CB. RESEARCH REPORT A meta?analysis of predictors of continued drug use during and after treatment for opiate addiction. Addiction. 1998;93(1):73-92.
- Chouljian TL, Shumway M, Balancio E, Dwyer EV, Surber R, Jacobs M. Substance use among schizophrenic outpatients: prevalence, course, and relation to functional status. Ann Clin Psychiatry. 1995;7(1):19-24.
- Mulder RT, Frampton CM, Peka H, Hampton G, Marsters T. Predictors of 3-month retention in a drug treatment therapeutic community. Drug Alcohol Rev. 2009;28(4):366-71.
- Wise BK, Cuffe SP, Fischer T. Dual diagnosis and successful participation of adolescents in substance abuse treatment. Journal of Substance Abuse Treatment. 2001;21(3):161-5.
- Cleary M, Hunt G, Matheson S, Siegfried N, Walter G. Psychosocial interventions for people with both severe mental illness and substance misuse. Cochrane Database Syst Rev. 2008;1.
- Coombes L, Wratten A. The lived experience of community mental health nurses working with people who have dual diagnosis: a phenomenological study. J Psychiatr Ment Health Nurs. 2007;14(4):382-92.
- Helmus TC, Saules KK, Schoener EP, Roll JM. Reinforcement of counseling attendance and alcohol abstinence in a community-based dual-diagnosis treatment program: a feasibility study. Psychol Addict Behav. 2003;17(3):249-51.
- Johnson S, Thornicroft G, Afuwape S, Leese M, White IR, Hughes E, et al. Effects of training community staff in interventions for substance misuse in dual diagnosis patients with psychosis (COMO study): cluster randomised trial. Br J Psychiatry. 2007;191:451-2.
- Staring AB, Blaauw E, Mulder CL. The effects of assertive community treatment including integrated dual diagnosis treatment on nuisance acts and crimes in dual-diagnosis patients. Community Ment Health J. 2012;48(2):150-2.
- Taylor SM, Galanter M, Dermatis H, Spivack N, Egelko S. Dual diagnosis patients in the modified therapeutic community: does a criminal history hinder adjustment to treatment? J Addict Dis. 1997;16(3):31-8.
- Greenberg B, Hall DH, Sorensen JL. Methadone maintenance therapy in residential therapeutic community settings: challenges and promise. J Psychoactive Drugs. 2007;39(3):203-10.
- Smith L, Gates S, Foxcroft D. Therapeutic communities for substance related disorder. Cochrane Database of Systematic Reviews. 2006;1.
- Caan W. Loss of tolerance and overdose mortality with detoxification: results of study need clarification. BMJ. 2003;327(7411):393.
- Morrison CL. Loss of tolerance and overdose mortality with detoxification: deaths have been associated with interventions. BMJ. 2003;327(7411):393.
- Morse GR. Loss of tolerance and overdose mortality with detoxification: abstinence is a valid choice. BMJ. 2003;327(7411):393-4.
- Strang J, McCambridge J, Best D, Beswick T, Bearn J, Rees S, et al. Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study. BMJ. 2003;326(7396):959-60.
- Wines JD, Jr., Saitz R, Horton NJ, Lloyd-Travaglini C, Samet JH. Overdose after detoxification: a prospective study. Drug Alcohol Depend. 2007;89(2-3):161-9. 80. Logan DE, Marlatt GA. Harm reduction therapy: a practice-friendly review of research. J Clin Psychol. 2010;66(2):201-14.
- Ritter A, Cameron J. A review of the efficacy and effectiveness of harm reduction strategies for alcohol, tobacco and illicit drugs. Drug Alcohol Rev. 2006;25(6):611-24.
- Laker CJ. How reliable is the current evidence looking at the efficacy of harm reduction and motivational interviewing interventions in the treatment of patients with a dual diagnosis? J Psychiatr Ment Health Nurs. 2007;14(8):720-6.
- Laker CJ. A literature review to assess the reliability and validity of measures appropriate for use in research to evaluate the efficacy of a brief harm reduction strategy in reducing cannabis use among people with schizophrenia in acute inpatient settings. J Psychiatr Ment Health Nurs. 2008;15(9):777-83..
- Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651-6.
- Phillips P, Labrow J. Dual diagnosis - does harm reduction have a role? Int J Drug Policy. 2000;11(4):279-83.
- Phillips P. The mad, the bad, and the dangerous-harm reduction in dual diagnosis1. International Journal of Drug Policy. 1998;9(5):345-9.
- Phillips PA. Dual diagnosis: an exploratory qualitative study of staff perceptions of substance misuse among the mentally ill in Northern India. Issues Ment Health Nurs. 2007;28(12):1309-22.
- Maremmani I, Pacini M, Lubrano S, Perugi G, Tagliamonte A, Pani PP, et al. Long-term outcomes of treatment-resistant heroin addicts with and without DSM-IV Axis 1 psychiatric comorbidity (dual diagnosis). European Addiction Research. 2008;14(3):134-42.
- Hulse GK, Tait RJ. Five-year outcomes of a brief alcohol intervention for adult in-patients with psychiatric disorders. Addiction. 2003;98(8):1061-8.
- Hulse GK, Tait RJ. Six-month outcomes associated with a brief alcohol intervention for adult in-patients with psychiatric disorders. Drug Alcohol Rev. 2002;21(2):105-12.
- Graeber DA, Moyers TB, Griffith G, Guajardo E, Tonigan S. A pilot study comparing motivational interviewing and an educational intervention in patients with schizophrenia and alcohol use disorders. Community Ment Health J. 2003;39(3):189-202.
- Baker A, Lewin T, Reichler H, Clancy R, Carr V, Garrett R, et al. Evaluation of a motivational interview for substance use within psychiatric in-patient services. Addiction. 2002;97(10):1329-37.
- Carey KB, Purnine DM, Maisto SA, Carey MP. Enhancing readiness-to-change substance abuse in persons with schizophrenia. A four-session motivation-based intervention. Behav Modif. 2001;25(3):331-84.
- Farren CK, Mc Elroy S. Treatment response of bipolar and unipolar alcoholics to an inpatient dual diagnosis program. J Affect Disord. 2008;106(3):265-72.
- Drake RE, Mueser KT, Clark RE, Wallach MA. The course, treatment, and outcome of substance disorder in persons with severe mental illness. Am J Orthopsychiatry. 1996;66(1):42-51.
- Drake RE, Mueser KT. Psychosocial approaches to dual diagnosis. Schizophr Bull. 2000;26(1):105-18.
- Minkoff K, Cline CA. Changing the world: The design and implementation of comprehensive continuous integrated systems of care for individuals with co-occurring disorders. Psychiatric Clinics of North America. 2004;27(4):727-44.
- Barrowclough C, Haddock G, Beardmore R, Conrod P, Craig T, Davies L, et al. Evaluating integrated MI and CBT for people with psychosis and substance misuse: recruitment, retention and sample characteristics of the MIDAS trial. Addictive behaviors. 2009;34(10):859-66.
- Minkoff K. Best practices: developing standards of care for individuals with co-occurring psychiatric and substance use disorders. Psychiatric Services. 2001;52(5):597-9.
- Judd PH, Thomas N, Schwartz T, Outcalt A, Hough R. A dual diagnosis demonstration project: treatment outcomes and cost analysis. Journal of Psychoactive Drugs. 2003;35(sup1):181-92