Keywords
Active smoking, passive smoking, pregnancy, pregnancy outcomes
Introduction
The term "passive smoking" usually refers to the inhalation of smoke that is either exhaled by a smoker or released as sidestream smoke from a burning cigarette. Another name for passive smoking is "involuntary smoking," because the person who inhales it often has no choice in the matter. The effect of cigarettes on the pregnant woman and developing fetus are numerous with a wide range of squeal that will remain with the fetus for the rest of her life.
Maternal smoking during pregnancy has long considered an important risk factor for intrauterine growth retardation [1].
A definite, well-established relationship exists between smoking and low birth weight defined as birth weight less than 2500 grams [2]. A remarkably constant 100-300g differences in baby birth weight between cigarette smokers' and nonsmokers' has been determined in many studies since 1957 [3].
A cross-sectional study conducted in developing countries found that, more babies born to mothers exposed to environmental tobacco smoke (ETS) were small-for-gestation and their mean birth weight was 138g less than that of babies in the unexposed mothers [4]. The risk and magnitude of low birth weight is related to the number of cigarettes smoked during pregnancy [5].
Polanska and Hanke [6] stated that, since 1957 maternal smoking during pregnancy increase the risk of spontaneous abortion, placenta previa (placenta that partly or completely covers the internal cervical os), abruptio placenta (premature separation of the placenta from the uterine wall). Furthermore, cigarette smoking increases the risk of premature rupture of membranes [7], placenta previa [8], and preterm delivery [9]. There is good epidemiological evidence to support a risk of placenta previa, abruptio placenta, premature rupture of membranes and preterm delivery increased with smoking during pregnancy [10]. USDHHS [11] stated that, many studies, showed a positive association between maternal smoking during pregnancy and the risk of spontaneous abortion. A previous report also mentioned that, cigarette smoking is associated with placenta previa. Relative risks range between 1.5 and 3.0, and dose-response relationships. In smokers, level of carbon monoxide is increased at the expense of oxygen; therefore, smokers usually have less oxygen bound to hemoglobin in the blood, compared with nonsmokers. Smoking-induced chronic hypoxemia has been suggested to result in placental enlargement, which increases the risk that the placenta reaches the cervical os [12]. Plasma ascorbic acid levels are lower in smokers than in nonsmokers, which predispose the placenta to early separation in smokers [13]. Ananth et al., [14] found that placental abruption was doubled in mothers who smoked during pregnancy compared to nonsmokers, and the risk increases with number of cigarettes smoked per day.
A Swedish study of women who gave birth during 1983-1996 found that maternal smoking was significantly associated with preterm birth besides other adverse outcome (intrauterine growth retardation, a small head circumference, a low Apgar score at 5 min and stillbirths and neonatal deaths) [15]. In a case-control study on all very preterm births in two regions of Stockholm 1988–1992, Kyrklund-Blomberg et al.,[7] found that, smoking increases the risk of very preterm birth, preterm premature rupture of membranes, and late pregnancy bleedings. There was a dose–dependent association between smoking and risk of very preterm birth, and heavy smokers (10 cigarettes per day) had a threefold increase in risk compared with nonsmokers.
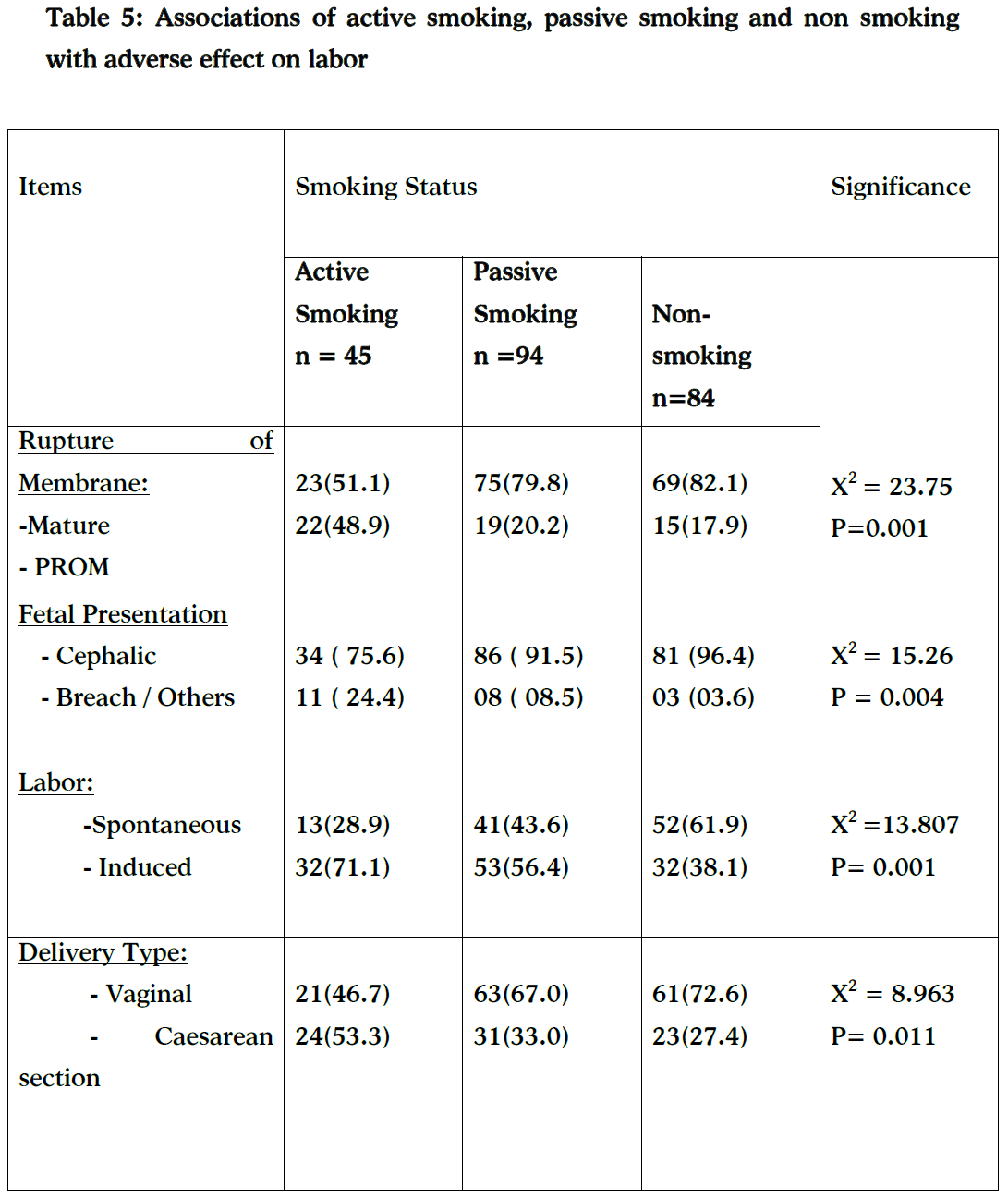
Smoking was also associated with type of delivery with more caesarean births among active and passive smokers. This result is consistent with Habek, et al., [1] who reported an increased rate of cesarean births among mothers who smoked.
This study aims to study the effects of maternal smoking (active, passive and nonsmoking) on pregnancy outcomes. The outcome variables include pregnancy complications such as hypertension, anemia, abruptio placenta, placenta previa; and intrapartum complications such as PROM, preterm labor, caesarean section and fetal distress. We have also examined the associations of active, passive and nonsmoking with neonatal health condition such as ABGAR score at one and fifth minute.
Material and methods:
A cross-sectional study was conducted between January and May 2009 at four Jordanian hospitals. Two hospitals are in Amman, the Capital, and the other two are in the Zarqa Governorate. Public and private hospitals with large occupancy rates in both regions were selected to ensure a variety of socio-demographic variables and an adequate number of cases during the study period.
A purposeful sample of 223 pregnant women aged 20 -35 years was selected from the postpartum wards. Younger than 20 and older than 35 years old were excluded to eliminate age related complications of pregnancy also women who had a multiple pregnancy were excluded. The study was based on singleton live baby and excluded still birth.
After obtaining the hospitals' permission for data collection, women who gave consent for participation were interviewed by the researchers as soon as possible after birth; and before leaving the hospital. They were reassured that their smoking status is confidential and no personal identifiers will be disclosed. Each woman was interviewed with a structured form prepared by the researchers according to literature review.
The structured interview form consists of three parts: part (1) consists of socio-demographic data (age, educational level, occupation & family income).
Part (2): consists of obstetrical data (duration of pregnancy per weeks, gravidity, parity, abortion and other variables related to antenatal health problems & perinatal complications). Part three of the questionnaire that includes: newborn assessment (birth weight, length, head circumference). Also associated disorders such as congenital anomalies or any other abnormalities are included. Apgar score, it was used to evaluate the neonatal condition at the first and fifth minutes after birth.
The questionnaire recorded details of the average daily number of cigarette, daily exposure, besides enquiring into their knowledge and perceptions about passive and active smoking.
Maternal smoking during pregnancy was determined based on clients self-report and was defined in the following way: A "smoker" if she smoked at least four cigarettes per day during pregnancy; a "passive" smoker if she was closely exposed to tobacco smoke by people such as her husband, family members and co-workers. A non-smoker is a woman who stated that she did not smoke during pregnancy or was not exposed to passive smoking [16]. Gestational age is defined as the duration of pregnancy (in completed weeks). Gestational age was estimated by researcher according to Naegela formula, because this is the best available information. A few numbers of women are excluded because the date of last menstrual period was missing. Preterm birth was defined as delivery or expulsion of the fetus before 37 completed gestational weeks [4].
The intrapartum period is defined as the period of onset of labor to the end of the third stage [16].
Main outcomes measures: Adverse effect on pregnancy (preterm birth, fetal condition, congenital neonatal malformation) and adverse effect on labor (premature rupture of membrane (PROM), malpresentation, caesarean section).
The data obtained were computerized and tabulated .SPSS version 11, was employed for data analysis. Chi-square, were used to present the findings and to compare the three groups (non-smokers, passive smokers and active smokers) in relation to pregnancy and intrapartum adverse effects. A p-value of < 0.05 was considered statistically significant.
Results
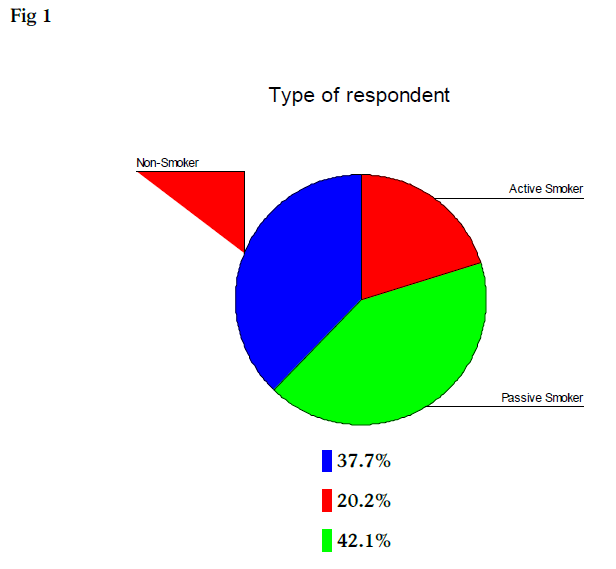
Fig. 1 demonstrated that, 223 participating mothers were categorized according to smoking status into three groups: non-smokers 37.7%, passive smokers 42.1%, and active smokers 20.2%.
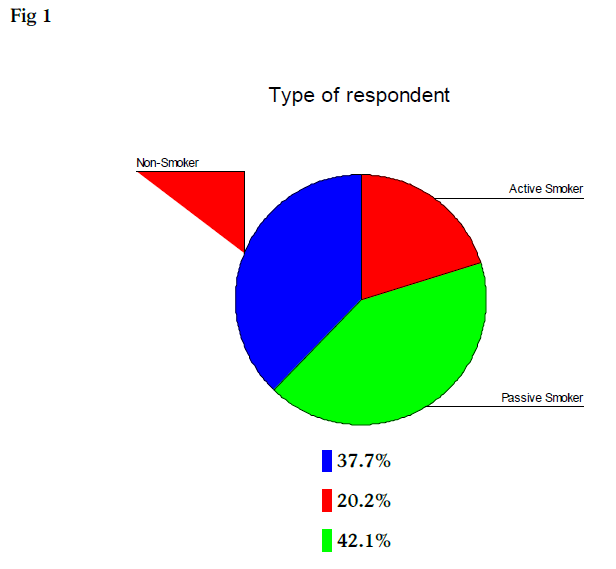
Figure 1
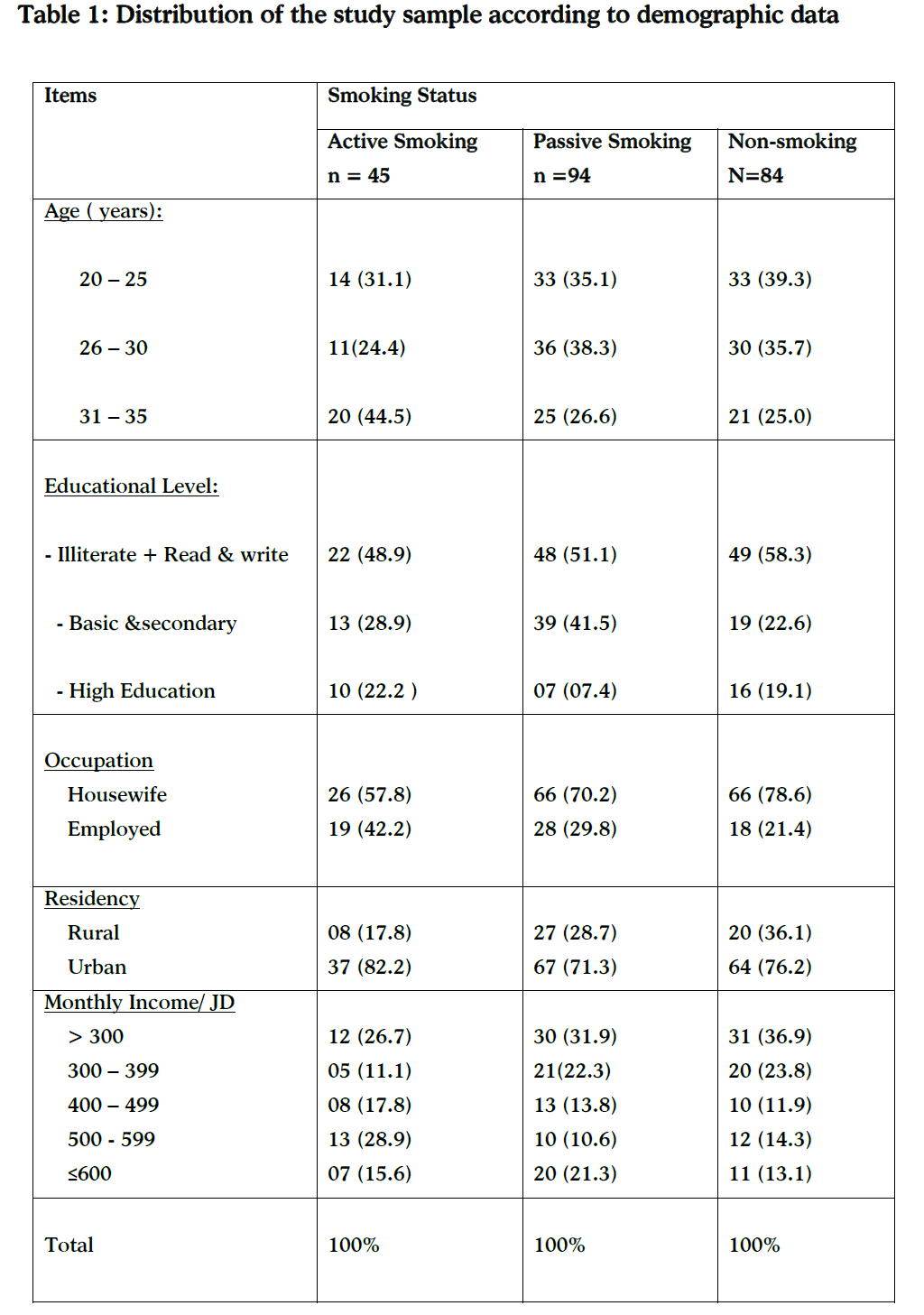
Table (1) showed that the mothers' ages ranged from 20 – 35 years. More than forty-four per cent of active smokers group (n= 45) were 31-34 years of age, compared to one quadrant (25.0%) of the non-smokers group (n= 84). The same table indicated that nearly half (48.9%) of the active smokers group had illiterate or read and write, were not working (57.8%), and living in urban areas (82.2%).The mean score of monthly family income is 391.70 JD's ($ 550).
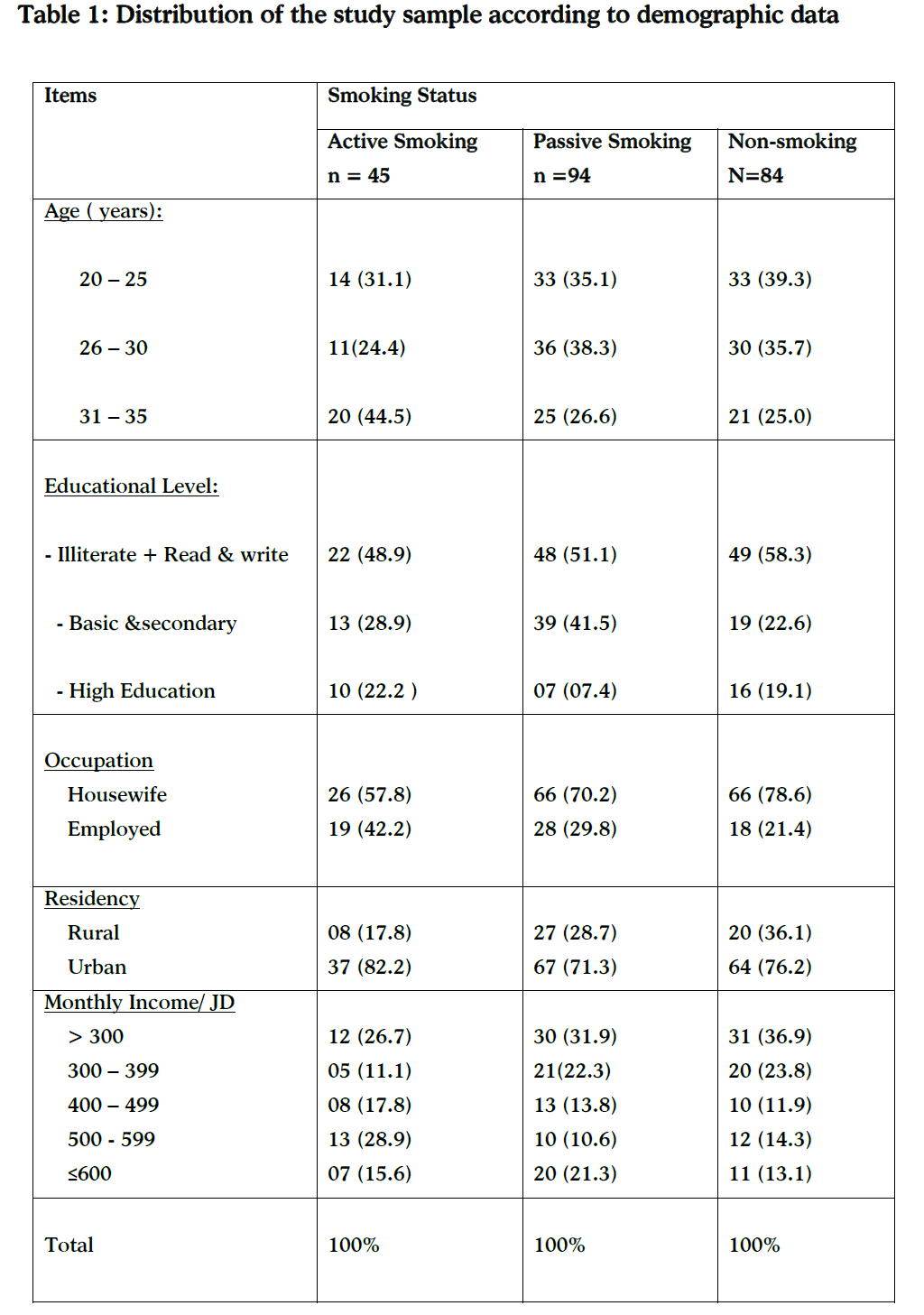
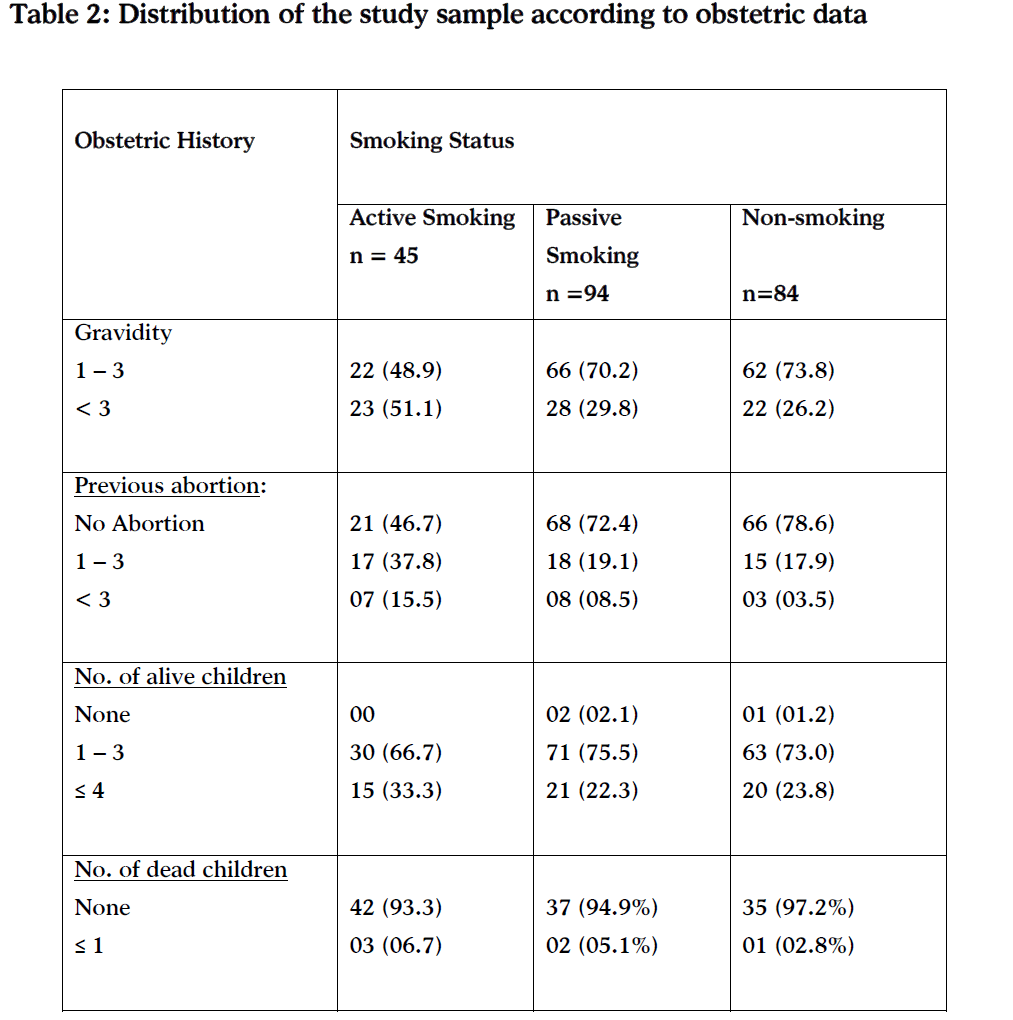
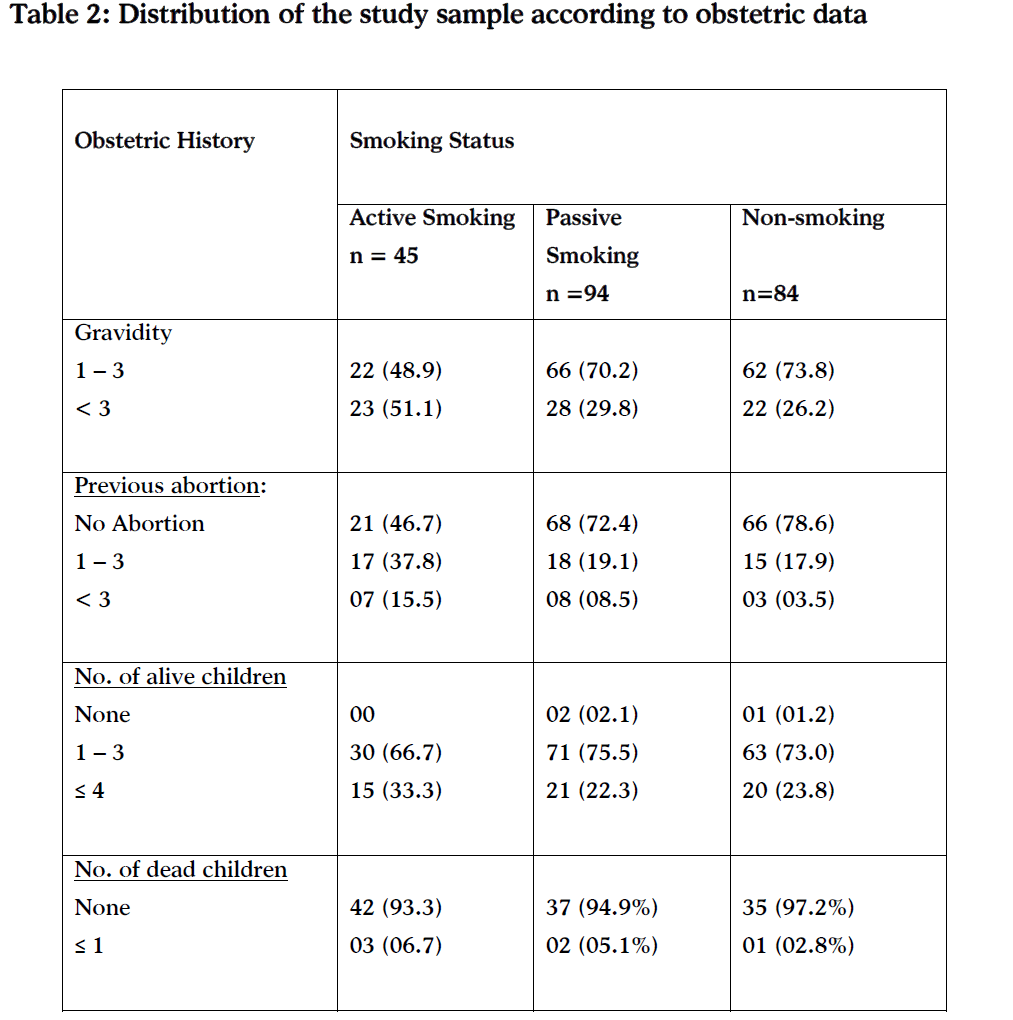
Table (2) indicated that 15.6% of active smokers' mothers experienced abortion more than three times. Compared to only 3.6% of non- smokers.
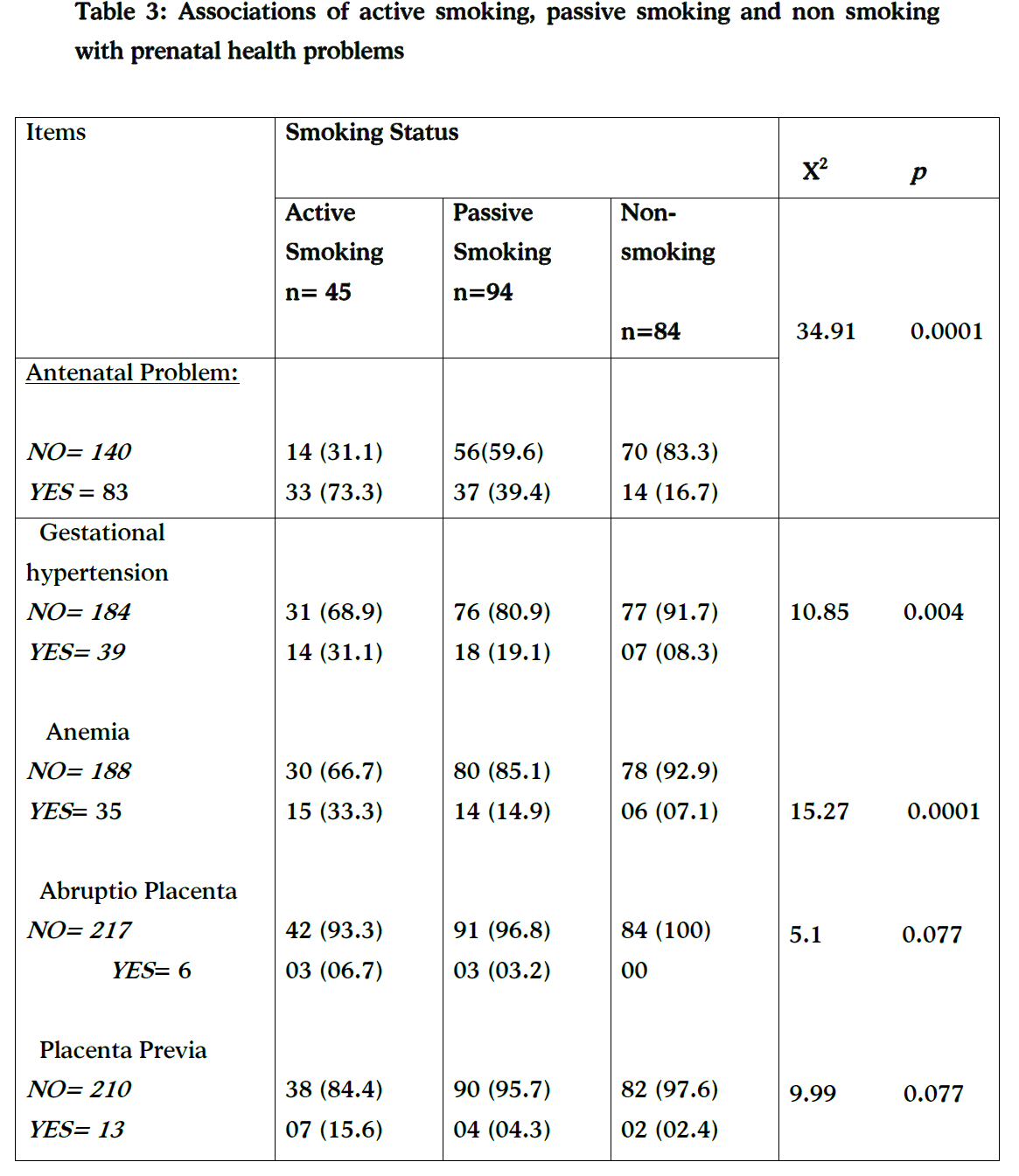
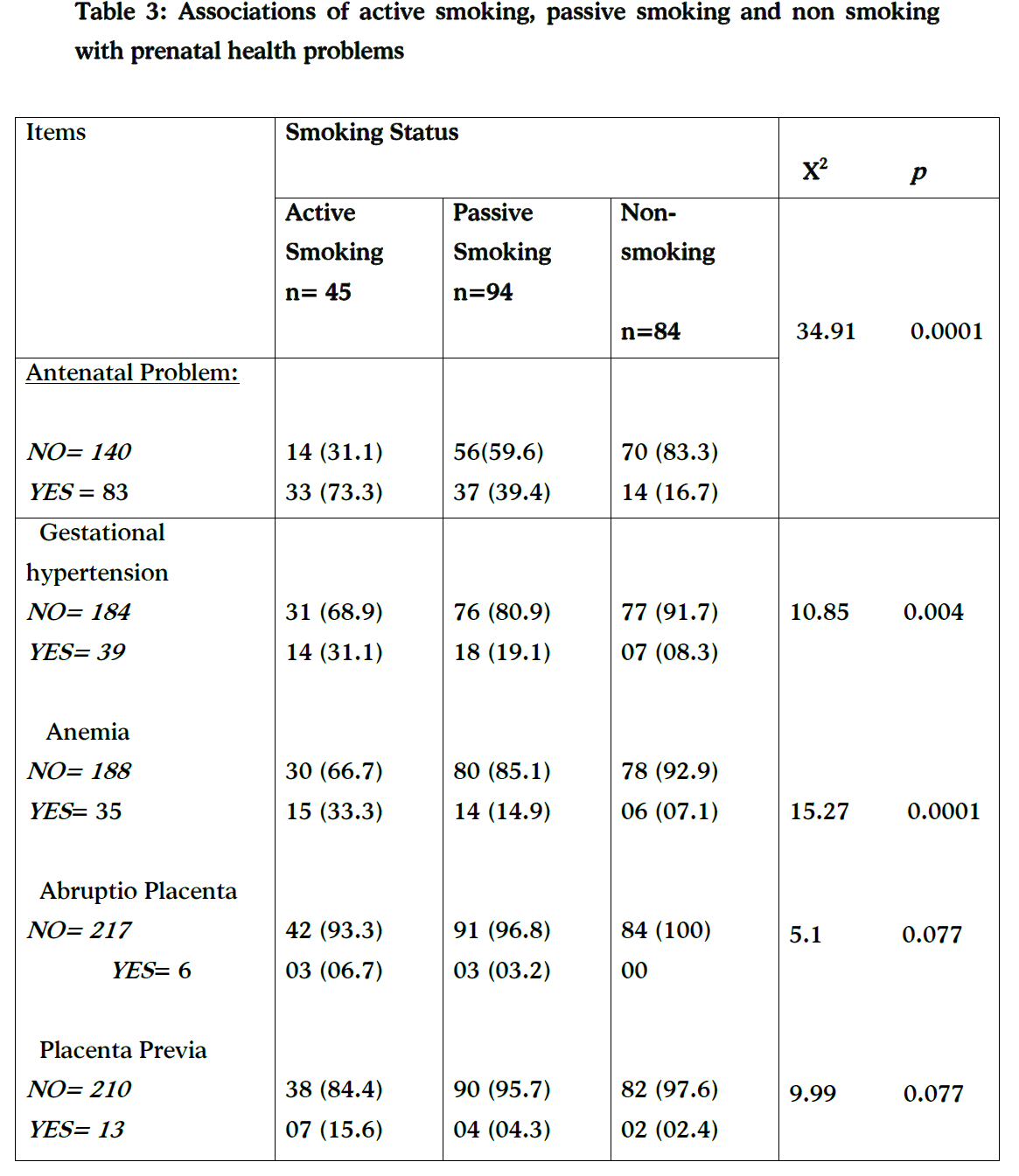
Regarding the association of smoking status and prenatal health problems (hypertension, anemia, abruption placenta and/ or placenta previa) table 3 shows that more than seventy per cent of the active smokers and 39.4% of the passive smokers reported having antenatal health problems. While only 16.7% of non-smoker group suffer from antenatal health problems. A statistically significant difference was found association between smoking status and gestational hypertension (X2 = 10.85, p= 0.004), and anemia (X2 = 15.27, p= 0.0001). Compared to active smokers, passive smokers and non- smokers showed no statistically significant increase in the rate of abruption placenta or placenta previa during their pregnancies (p= 0.077).
The association between smoking status and gestational age according to Naegela' formula table (4) reveals that the gestational age is decreased among active smokers and increased among non-smokers mothers. More than half (53.3%) of active smokers mothers delivered earlier (preterm birth). While the majority (89.3%) of non-smokers mothers were delivered term babies (≥37 week's gestation). The differences was statistically highly significant, (X2= 29.314 at p=0.000). Also, the same table revealed that there was a statistically significant differences in the fetal movement, increasing fetal heart rate and / or fetal distress) and smoking status. The same table demonstrated that 38.5% of active smoking women got an APGAR score of 7 or more versus 71.9% in the non smoking women at 1st minute of delivery, while less than half of active smoking women get an APGAR score of 7 or more at 5th minute of delivery.

Statistically significant difference was found between smoking status and rupture of membrane (p= 0.001) table 5.
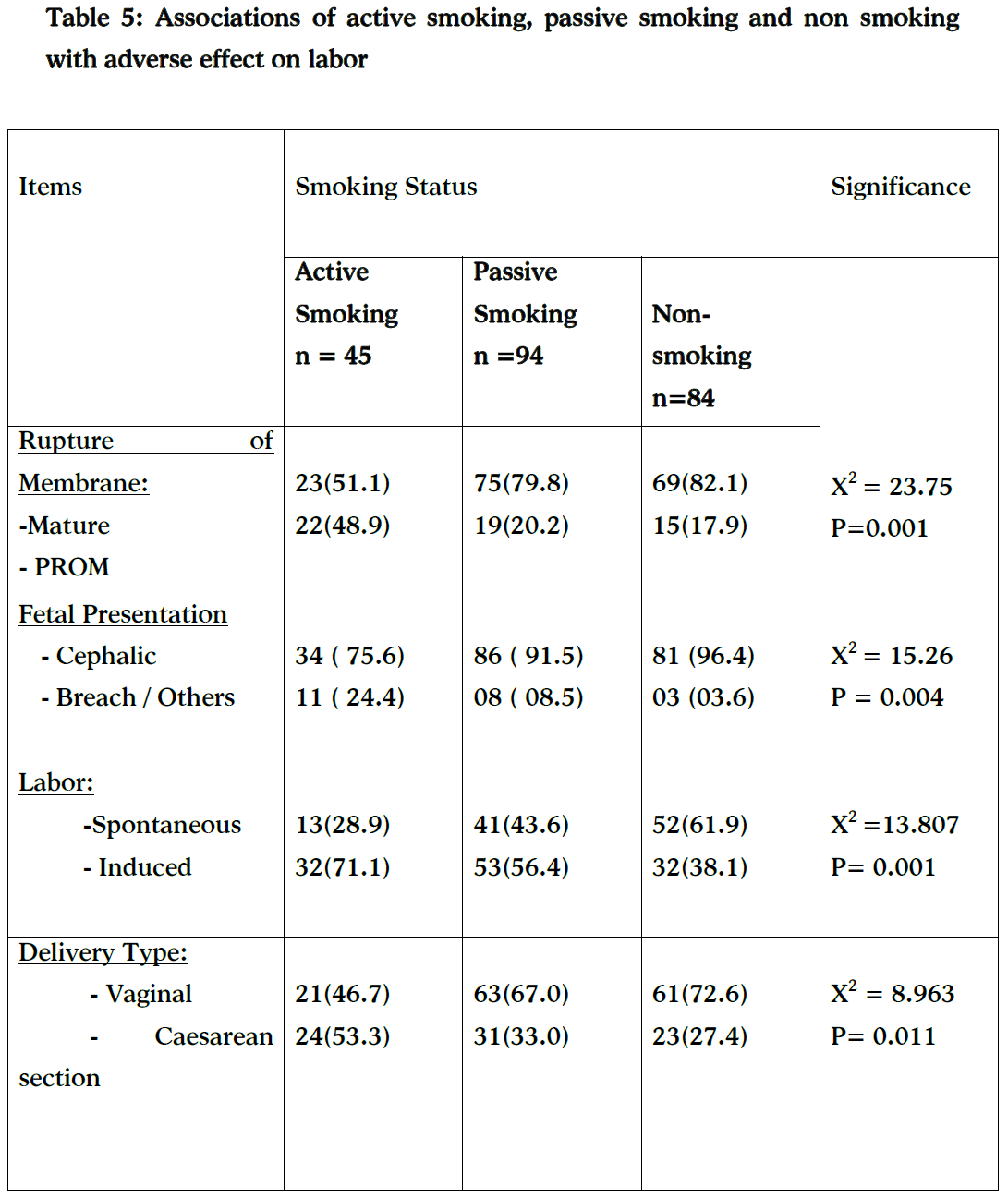
The same table shows that most of the non-smokers (72.6%) have had vaginal delivery while more than half (53.3 %) of active smokers mothers had cesarean birth. Breech presentation was found to be more common in active smokers followed by passive smoking (p= 0.004).
Table (6) illustrated that more than two quarters (68.9%) of active smokers group know the difference between active and passive smoking. All of then reported that smoking was harmful for the fetus and 88.9% of them stated that exposure to smoking during pregnancy from others (passive smoking) could be harmful during pregnancy.

Discussion
Smoking prevalence is commonly defined as the percentage of daily smoking in a population [12]. In Jordan, a study conducted to determine smoking habits among university students shows that 11% of female students smoked cigarettes [17]. While in 2002, Hadad [18] stated that 6.5% of Jordanian female university students are smokers. The present study revealed that the prevalence of active smoking among pregnant women was 20.2%, and 42.1% of studied women exposure to cigarette smoke (passive smoker). Several studies have shown similar results [11,19]. While a recent Germany study assessed the rate as 13% [20]. Also, the present study's smoking rate, however, is higher than the Canadian study [21].
In the present study, it was generally seen that the active smoker women were less educated, unemployed, had monthly family income less than 300 JD, higher gravidity and more number of chilled. This would point to a poorer socio-economic background of these women. This finding is has also been noted in the recent studies who mentioned that smoking during pregnancy was associated with low socio-economic status [21,22]. Heaman and Chalmers [23] reported a dose indicator of low income status associated with higher smoking prevalence.
The current study found that active smokers and passive smokers had significantly higher risks than non-smokers for hypertension, anemia, and premature rupture of membrane (PROM). This result is in agreement with in an observational, multi-center cohort study who mentioned that smokers' were five times more likely to develop eclampsia and a doubling of risk of being delivered premature labor [24].
In the present study we found that there were strong associations between smoking status and preterm birth (p= 0.000) and fetal distress (p= 0.001). This result was similar to Wisborg et al., [25] how found an increase risk of preterm birth and fetal distress associated with maternal smoking.
Smoking during pregnancy has been shown in vitro to result in decreased transfer of amino acids across the placenta [26], and its results in symmetrical growth impairment [27]. Also, the researchers found that smoking during pregnancy was associated with a more than 2-fold increased risk for offspring with hyperkinetic disorder, compared with non-smoking mothers [28]. In this study, we confirmed the smoking during pregnancy results in a significant increase in congenital neonatal malformation, fetal distress, poor APGAR score at first and fifth minutes.
This is an important finding because in many studies the growth deficit of neonates of smokers was found to persist in their postpartum life, affecting their physical development until 1 year of age [29], fetal distress [30], 1 are all found to be increased in rate related to the effect of nicotine and CO in pregnancies complicated by maternal smoking.
In the present study, more than half of the women in three groups knew the differences between active and passive smoking, though most women mentioned that smoking was harmful during pregnancy. Moreover, the smoker women did not take any measures to stop smoking or to avoid exposure to smoking. These differences could be related to socioeconomic and educational factors that influence smoking habits. A study carried out among pregnant women in North Western India has shown that most women believed that smoking was harmful to the developing fetus and did not take any preventive steps to avoid exposure to environmental tobacco [4].
Limitation:
Estimates of smoking prevalence during pregnancy are usually based on self-reported information. Because negative attitudes toward women smoking especially in our countries have increased during recent years, the validity of self-reported smoking information may be a special concern.
Conclusion and Recommendations
The role of maternal smoking during pregnancy on adverse pregnancy has reported in many studies, and this was observed also in our study. In conclusion, smoking during pregnancy (active smoking and passive smoking) is associated with high risk of having preterm birth, breech presentation, caesarean section birth and poor APGAR score. Furthermore, there were statistically significant differences between the three groups regarding to rupture of membrane, induction of labor and or fetal presentation (cephalic/ breach).
It adds to an increasing body of literature on the adverse effects of passive and active smoking on pregnancy outcomes. This result underscores the need to target all women who smoke as well as the public surrounding pregnant women to minimize environmental exposure during pregnancy. This study provides data for policy makers towards developing plans for the improvement of reproductive outcomes. Also, there is urgent need for a comprehensive approach to prevention of maternal smoking in Jordan.
Acknowledgments
We would like to thank Dr. Ream El Safadi for her valuable advices.
3311
References
- Habek D; Habek JC; Ivanisević M; Djelmis. Fetal tobacco syndrome and perinatal outcome. Fetal Diagnosis and Therapy [Fetal Diagn Ther] 2002; 17 (6): 367-71.
- Walsh RD. Effects of maternal smoking on adverse pregnancy outcomes: Examination of the criteria of causation, Hum. Biol 1994:66; 1059-1092.
- Ingvarsson RF, Bjarnason AO, Dagbjartsson A, Hardardottir H, Haraldsson A, Thorkelsson T. The effects of smoking in pregnancy on factors influencing fetal growth. Acta Pædiatr 2007; 96: 383-6.
- Goel P, Radotra A, Singh I, Aggarwal A, Dua D. Effects of passive smoking on outcome in pregnancy. Journal of Postgraduate Medicine 2004; 50 (1): 12-16.
- Li CQ, Windsor RA, Perkins L, Goldenberg, RL, Lowe JB. The impact on infant birth weight and gestational age of continine-validated smoking reduction during pregnancy. JAMA 1993; 269(12):1519-1524.
- Polańska K, Hanke W. Effect of smoking during pregnancy on maternal condition and birth outcome--overview of epidemiologic studies. Przegl Epidemiol. 2004;58(4): 683-91.
- Kyrklund-Blomberg NB, Granath F, Cnattingius S. Maternal smoking and causes of very preterm birth. Acta Obstet Gynecol Scand, 2005; 84: 572– 577.
- TikKanen M, Nuutila M, Hiilesmaa V, Paavonen J, Ylikorkala O. Pre-pregnancy risk factors for placental abruption. Acta Obstet Gynecol Scand. 2006;85:40-44. doi:10.1080/0001634500324241.
- Ng SP, Zelikoff JT. Smoking during pregnancy: Subsequent effects on Offspring immune competence and disease vulnerability in later life. Reprod Toxico. 2007; 23:428-437. doi: 10.1016/j.reprotox.2006.11.008.
- Fantuzzi G, Aggazzotti G, Righia E, Facchinetti F, Bertucci E, Kanitz S, et al. Preterm delivery and exposure to active and passive smoking during pregnancy: a case-control study from Italy. Paediatr Perinat Epidemiol. 2007; 21: 194-200.
- U.S. Department of Health and Human Services. (2001b). Health consequences of tobacco use among women. In Women and smoking: A report of the surgeon general (pp. 177–450). Rockville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health.
- Cnattingius S. The epidemiology of smoking during pregnancy: Smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob Res. 2004;6(2): 125-140. doi: 10.1080/14622200410001669187.
- Faruque M. O., Khan M. R., Rahman, M. M., Ahmed F. Relationship between smoking and antioxidant nutrient status. British Journal of Nutrition, 1995;73(4): 625–632.
- Ananth CV, Smulian JC, Vintzileos AM. Incidence of placental abruption in relation to cigarette smoking and hypertensive disorders during pregnancy: a meta-analysis of observational studies. Obstetrics and Gynecology, 1999; 93 (4): 622-628.
- Kallen K. The impact of maternal smoking during pregnancy on delivery outcome. European Journal of Public Health, 2001;11(3): 329-333.
- Stedman’s Medical Spellchecker. Lippincott Williams & Wilkins 2006. Available from: https://www.wrongdiagnosis.com/medical/intrapartum_period.htm. Accessed on 1/4/2006.
- Khader YS., Alsadi AA. Smoking habits among university students in Jordan: prevalence and associated factors. Eastern Mediterranean Health Journal, 2008;14(4): 897-904.
- Haddad LG, Malak MZ. Smoking habits and attitudes towards smoking among university students in Jordan. International journal of nursing studies, 2002;9(8):793–802.
- Nabet C, Ancel PY, Burguet, Burguet A, Kaminski M.: Smoking during pregnancy and preterm birth according to obstetric history: French national perinatal surveys. Paediatric and Perinatal Epidemiology.2005;19(2),88-96.doi:10.1111/j.1365-3016.2005.00639.x
- Schneider S, Maul H, Freerksen N, Postchke-Langer M. Who smokes during pregnancy? An analysis of the German perinatal quality survey 2005. Public Health. 2008; 122:1210-1216. doi: 10. 1016/j.puhe.2008.02.011.
- Al-Sahab B, Saqib M, Hauser G, and Tamim H.: Prevalence of smoking during pregnancy and associated risk factors among Canadian women :a national survey. BMC Pregnancy and Childbirth. 2010; 10: 10-24. doi:10.1186/1471-2393.
- Nagahawatte NT, Goldenberg RL. Poverty, maternal health, and adverse pregnancy outcomes. Ann N Y Acad Sci.2008; 1136:80-85. doi:10.1196/annals. 1425.016.
- Heaman MI, Chalmers K. Prevalence and correlates of smoking during pregnancy: A comparison of aboriginal and non-aboriginal women in Manitoba. Birth. 2005; 32: 299-305.doi:10.1111/j.0730-7659.2005.00387.x.
- Pipkin FB: Smoking in Moderate/Severe Preeclampsia Worsens Pregnancy Outcome, but Smoking Cessation Limits the Damage. Hypertension. Journal of the American Heart Association. 2008;April, Doi: 10.116/HYPERTENSIONAHA.107.106559.
- Wisborg K, Kesmodel U, Henriksen TB, Olsen SF, Secher NJ. Exposure to tobacco smoke in utero and the risk of stillbirth and death in the first year of life. Am Journal Epidemiol. 2001; 154(4):322-327. doi: 10.1093/aje/154.4.322.
- Pastrakuljic A, Derewlany L, Koren G. Maternal cocaine use and cigarette smoking in pregnancy in relation to amino acid transport and fetal growth. Placenta 1999; 20: 499–512.
- Ingvarsson RF, Bjarnason AO, Dagbjartsson A, Hardardottir H, Haraldsson A, Thorkelsson T. The effects of smoking in pregnancy on factors influencing fetal growth. Acta Pædiatr 2007; 96: 383-6.
- Linnet KM, Wisborg W, Obel C, Wisborg K, Rodriguez A: Smoking during pregnancy and the risk for hyperkinetic disorder in offspring. Pediatrics 2005; 116(2):462-467.
- Vielwerth SE, Jensen RB, Larsen T, Greisen G. The impact of maternal smoking on fetal and infant growth. Early Hum Dev 2007; 83: 491-5.
- Andres RL, Day MC. Perinatal complications associated with maternal tobacco use. Semin Neonatol 2000; 5: 231-41.