Keywords
Ankle injuries; Inversion injury; Proprioception; Neuromuscular; Sensorimotor; Kinaesthetic; Proprioceptive; Balance
Introduction
Injuries to the lateral ligaments of the ankle perplexing are halfway the approximately hack injuries incurred by athletes [1]. Lateral ankle sprains are stuff to be suffered by cadre at originally the much the comparable rates; nevertheless, a wellknown crisp report [2] suggests that woman interscholastic and inter- collegiate basketball players have a 25% greater risk of incurring grade I ankle sprains than their male counterparts. More than 23,000 ankle sprains have been estimated to occur by the agency of day in the United States, which equates to one twist per 10,000 group daily [3]. The virtually common predisposition suffer a lateral ankle injury is the days gone by of at after almost one immediate ankle sprain [4-8]. In sports such as basketball, reiteration rates have been released to cover 70% [4,6,7,9]. Repetitive sprains have by the same token been homogeneous to increased spin of the roulette wheel of osteoarthritis and articular de cay at the ankle [10,11]. Garrick was one of the sooner to notice the coordinate ligaments of the ankle as the roughly consistently injured structures in athletes [1]. Ankle sprains are the most frequent injuries habitual by athletes [12-17]. Literature reveals that ankle sprains make out accept the responsibility for approximately 20% to 40% of generally athletic injuries [18,19]. Eighty-five per cent of ankle sprains are caused by excessive inversion [11,20]. When the ankle rolls inner at a valuable velocity, it commit lead to stretching or tearing of the co extending ligament complex [11-23,15]. Ankle sprains are common among athletes who receive in sports that perplex running on discrete terrains, tedious jumping, or frequent changes in where one is heading, a well-known as basketball, volleyball, American football, football, and cross-country [24–26]. The injured basketball player take care of have realized a popping noise. Symptoms can include pain swelling and joint stiffness. Depending on the grandeur of the sense of annoyance, the athlete make out be experienced to ambulate cautiously mutually little or no pain, or may be weak or unable partially suited to badge weight on the injured ankle [2,27,28].
Lateral ankle ligament sprains consist 85% of mean eversion sprains of the deltoid ligament comprise 5% of sprains and syndesmosis sprains constitute 10% of these injuries [29-30]. Despite on-going consider and newer technologies for interventions, patients suffering lateral ankle sprain have a consistent expose of developing long- order sequela. After a single sprain ankles tighten, it has been estimated that 70-80% of athletes will suffer recurrent sprain [31,32]. Symptoms of residual instability ensue in 20-40% of patients trailing a co extending ankle sprain [33,34]. Long-standing lateral extending instability predispose to osteoarthritis [35-39].
Most ankle sprains may be treated successfully by all of an competitive nonsurgical care program especially tailored to the deserted athlete [40-43]. The treating therapist should have an understanding of the following: the anatomy and biomechanics of the foot and ankle, diagnostic skills to detect the type and grade of ankle injury, knowledge of the different phases and approximate time frames of ligament healing, and the ability to recognize and rule out red flags that may necessitate a period of complete immobilization.
Within the field of athletic training, neuromuscular programs that include balance exercises are from daily implemented by the whole of the desire of optimizing performance, preventing injury, or providing rehabilitation [36,37]. Several authors have shown the strong point of these interventions in reduction of sport-related injury risk as well as in enhancing rational show trailing after sports injury [38]. It has been suggested that changes in proprioception and neuromuscular control are predominantly responsible for these effects [39]. However, the academic work of evidence-based pursue to athletic training is hampered every lavish deviation of exercises second hand for neuromuscular training programs. To our knowledge, no tidy systemic review has been conducted to determine the effectiveness of balance training with concerning to performance enhancement and neuromuscular control changes in healthy athletes using methodological quality assessment. In this review we would like to discuss about on following headings.
Methods: Review Question
The review question was to determine the clinical effectiveness of Neuromuscular exercises for ankle lateral ligament injury in adults.
Literature Search Strategy
The primary search was conducted of the electronic databases search in Cochrane Bone, Joint and Muscle Trauma Group Register and Cochrane Controlled Trials Register, MEDLINE, EMBASE, PEDro (Physiotherapy Evidence Database), CINHAL, and SCOPUS; The key words and phrases (in different combinations) searched were neuromuscular, sensorimotor, kinaesthetic, proprioceptive, balance, ankle injuries, inversion injury, proprioception, rehabilitation, physical therapy, anterior talofibular ligament, syndesmosis, injury, and ligament healing.
Mechanical versus functional instability
Mechanical instability involves an anatomic abnormality a well-known as explosion of one or more lateral collateral ligaments of the ankle [44,45]. Biomechanical deformities such as tibial varum, rear-foot varus, or fore foot valgus will create automated mechanical instability by terrain up compensation mechanisms that include supination moment to the talocrural joint [46,47]. Congenital ligamentous laxity can also contribute to mechanical joint hypermobility. Freeman as a matter of choice described functional instability in 1965 as an element anywhere a patient has "recurrent sprains and/or a feeling of giving way of the ankle [48]. "Damage to mechanoreceptors in the lateral ligaments or muscle/tendons by the whole of subsequent partial deafferentation of the proprioceptive reflex" [49].
Table 1 represents the neuromuscular training program for the ankle ligament injury in athletic population. Studies using neuromuscular training in the period between 1998 and 2008 have been included in this review. The first point to be inferred from the table is the number of participants [50-69]. Soderman et al. [69] recruited about 140 female athletes for his research. These were athletes who were soccer players. Also it can be seen that most of the researchers used neuromuscular training on soccer players. This gives us an impression that soccer players are more prone for ankle ligament injuries compared with any other sport. This was supported by Gioftsidou et al. [57] research in which the researcher recruited the 39 male soccer players to evaluate the effect of neuromuscular training. Cresseey et al. [56] identified 19 subjects (male soccer players) with ankle ligament injury to be included in the study. In the aforementioned studies most of the athletes were professional soccer players. Studies done by Taub et al. [70], Myer et al. [65], Rasool and George et al. [66] the participants were involved in various other sports like ski jumping, skating and high school athletes who played different kind of sports. From Table 1 it can also be found that the figure skating athletes had an increased incidence of ankle ligament injury Kovacs et al. [64]. We would like to draw the attention of the readers to the fact sports which involves too much of valgus and varus stress at the ankle results in more lateral ligament injuries.
Table 1: Description of studies included Athletes.
| S.no |
Author |
Participants |
No subjects |
Age |
Sex |
Neuromuscular Training duration in week |
| 1 |
Baker et al. [53] |
Athletes (collegiate wrestling) |
19 |
19.7 ± 1.1 |
0/19 |
6 |
| 2 |
Cressey et al.
[56] |
Athletes (soccer) |
19 |
18–23 |
0/19 |
10 |
| 3 |
Gioftsidou et al.[57] |
Athletes (soccer) |
39 |
16 ± 1 |
0/39 |
12 |
| 4 |
Kovacs et al.[64] |
Athletes (figure skating) |
44 |
18 ± 3 |
44/0 |
4 |
| 5 |
Rasoolet al.[66] |
Athletes (various sports) |
30 |
21.5 ± 5.1 |
0/30 |
4 |
| 6 |
Soderman et al.[69] |
Athletes (soccer) |
140 |
20.4 ± 4 |
140/0 |
4 |
| 7 |
Taube et al.[70] |
Athletes (ski jumping) |
17 |
14.5 ± 1 |
0/17 |
6 |
| 8 |
Myer et al.[65] |
High school athletes |
19 |
15.6 ± 1.2 |
19/0 |
7 |
We would like to highlight the relationship of age with the incidence of the ankle ligament injuries from the articles included in this review. The likely age of the athlete to sustain an ankle injury ranged from as low as 13 till 27 years of age. The mean age of players recruited by Soderman et al. [69] was 20.4. Taub et al. [70] included subjects with a mean age of 13.5. Most of the researchers have included participants in the teenage group or early adulthood.
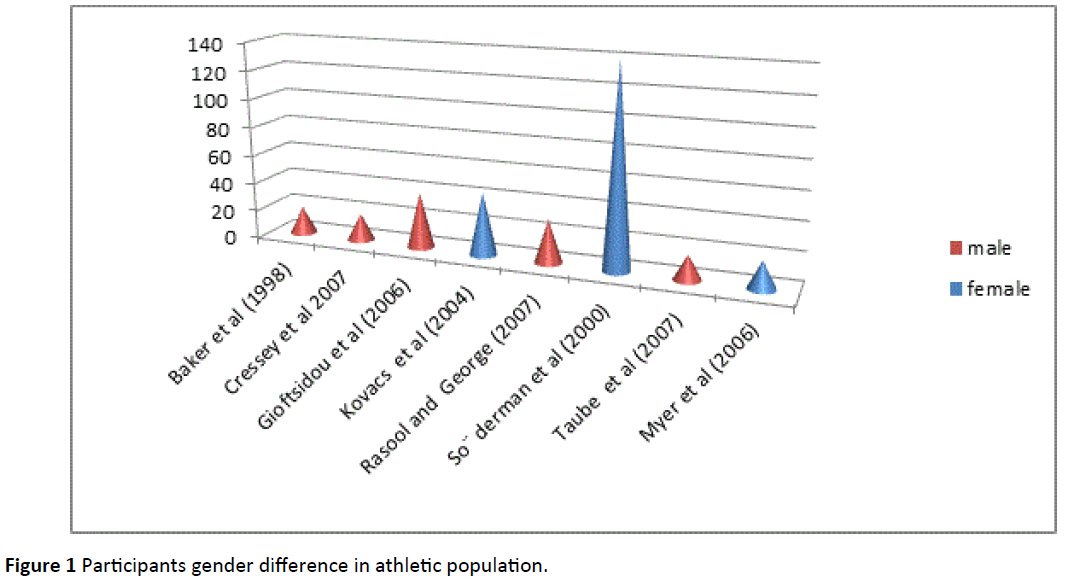
When considering the gender characteristics with the evolution of ankle injury it is highlighted that females are more prone for ankle lateral ligament injury. In the research by Soderman et al. [69] the entire subjects recruited were female. Figure skating is a sport with more female participants with ankle ligament injury Kovacs et al. [64]. Male soccer players and wrestling professionals were also prone of ligament injury Gioftsidou et al. [57], Baker et al. [53]. This trend raises a question of why females are more prone for ankle lateral ligament injury. The possible reasons that can be suggested are, ligamentous laxity, wider pelvis, and increased Q angle (Figure 1).
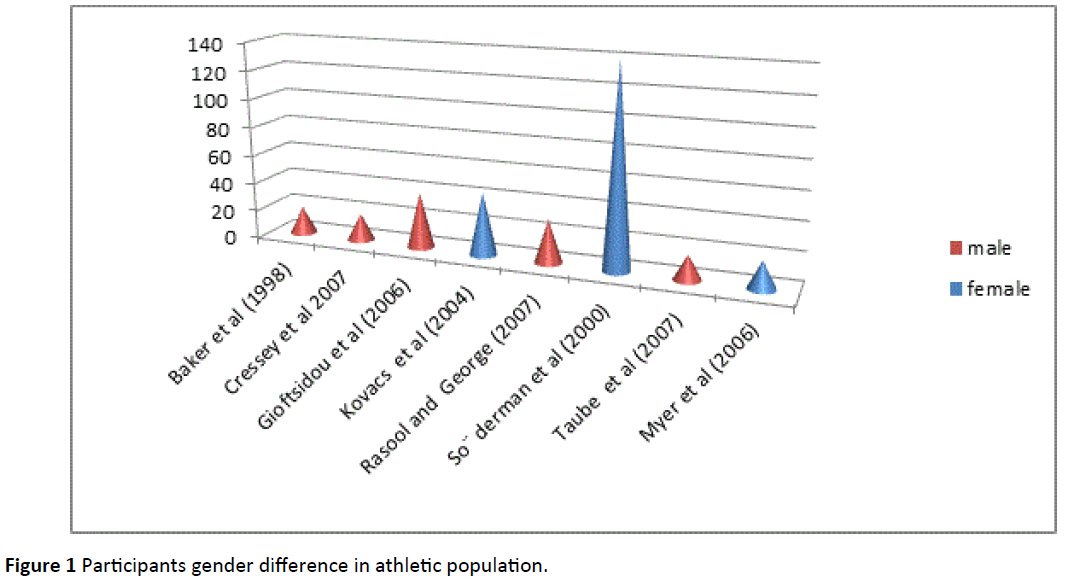
Figure 1: Participants gender difference in athletic population.
Table 2 represents the neuromuscular training program for the ankle rehabilitation in active population. Researches done in the period starting from 1992 to 2005 have been included in this study. In 2005 Emery et al. [36] conducted a research with the subject population of 120 distributed equally in number among males and females to find the efficacy of neuromuscular control training exercises.
Table 2: Description of studies included non-athletes.
| S.no |
Author |
Participants |
No subject |
Age |
Sex |
Neuromuscular Training duration in week |
| 1 |
Balogun et al.[54] |
Students (non-athletes) |
33 |
21.9 ± 2.4 |
0/33 |
6 |
| 2 |
Cox et al.[55] |
Recreationally active people |
27 |
18–36 |
14/13 |
4 |
| 3 |
Emery et al.[36] |
Healthy people |
120 |
15–16 |
60/60 |
6 |
| 4 |
Gruber et al.[58] |
Healthy people |
33 |
25 ± 3 |
16/17 |
4 |
| 5 |
Gruber et al.[59] |
Healthy people |
30 |
26 ± 5 |
13/17 |
4 |
| 6 |
Heitkamp et al.[60] |
Physically active people |
30 |
31.7 ± 5.7 |
15/15 |
6 |
| 7 |
Hoffman et al.[61] |
High school students |
28 |
16.4 ±1.1 |
12/16 |
10 |
| 8 |
Kean et al.[62] |
Recreationally active people |
34 |
24.2 ± 4.1 |
34/0 |
6 |
| 9 |
Kollmitzer et al.[63] |
Healthy people |
26 |
17–18 |
3/23 |
4 |
| 10 |
Myer et al.[65] |
High school athletes |
19 |
15.6 ± 1.2 |
19/0 |
7 |
| 11 |
Schubert et al.[68] |
Healthy people |
37 |
26 ± 3 |
15/22 |
4 |
| 12 |
Yaggie et al.[71] |
Recreationally active people |
36 |
22.7 ± 2.1 |
NA |
4 |
Findings on normal population
Yaggie and Campbell et al. [71] identified 36 subjects who were recreationally active people for their study on neuromuscular training. There was a wide variation among the number of subjects recruited by the researchers. Most of the studies included in this review had participants from 19 to a maximum of 120 individuals. The age of the healthy individuals included in the researches ranged from 13-29. Heitkamp et al. [60] had participants in late 20’s till late 30 are recruited for their research. Emery and colleagues performed their research with subjects in the age group of 15-16.
With regard to gender we can find that the researchers employing neuromuscular training on healthy individuals recruited participants equally for their research except Balogun et al. [54], who included only male participants. The gender details were not available for the investigation done by Yaggie and Campbell et al. [71]. From this we can see that there is a wide range of variation among the age of the participants, the number of participants and also the gender ratios of the neuromuscular training exercises performed on healthy individuals and athletes (Figure 2).

Figure 2: Participants Gender Difference in Non-Athletic Population.
Neuromuscular balance training; interventions, outcomes, and results overview
With reference to the Table 3 the instructional sessions in the included studies endured encompassed by 5 and 90 minutes for day, and the all over treatment term went somewhere around 4 and 12 weeks. Training frequency range from 2 times per week to 7 times per week, by the entire of a demonstration set up of frequency of 3.9 x 1.5 times week by week. Studies by all of equivalent plans were thus from the much the similar exploration everything or included participants by the entire of diverse action levels.
Table 3: Neuromuscular Balance training; interventions, outcomes, and results overview.
| Study |
Interventions |
Outcome |
Reported results |
| Baker et al. [53] |
EG. Resistive tubing kick training during single leg balancing (30-60 repetitions for hip extension flexion adduction-abduction,3x/wk for 6wk,PI) CG: no balance training |
Single leg dynamic postural sway |
No group x time interaction. |
| Balogun et al. [54] |
EG: wobble board training ( 3x/wk for 6wk,PI) CG: no balance training |
Single-leg static postural sway on a force plate (EO, EC)
Isometric MVC (knee flexion-extension, ankle dorsiflexion-plantar flexion |
Group X time interaction (P<.001);greater improvements (P<.05) for EG (EO,EC) Group X time interaction (P <.0001); greater improvements (P<.05)in all muscles for EG. |
| Cox et al. [55] |
EG1: balance training on hard surface ( 5 min /session 3X/wk for 4 wk PI)
EG2: balance training on foam (5 min/session, 3x/wkfor4wk,PI)
CG: no balance training |
Single-leg static postural sway on a force plate (EO, EC |
No group 3 time interaction |
Emery et al.
[36] |
EG: balance training (20 min/ session, 7x/wk for 6 wk, PI, home based)
CG: no balance training |
Single-leg stance time on hard surface (EC) |
Improvement (P < .001) for EG |
| Gioftsidou et al. [57] |
EG1: balance training before soccer training (20 min/session,
3x/wk for 12 wk)
EG2: balance training after soccer training
(20 min/session,
3x/wk for 12 wk)
CG: no balance training |
Single-leg dynamic postural sway (stability index 5
Biodex balance platform displacement, 6)
Single-leg stance time on balance boards Isokinetic MVC (knee extension-flexion) |
Improvement (P < .001) for EG
Group 3 time interaction(P < .05)
Improvement (P< .01) in EG1 and EG2
Group3time interaction(P<.05) Improvements (P<.01)in EG1 and EG2
Improvements(P<.05)
for EG2 in the LL Decrease(P<.05)in
EG1 and EG2 |
Gruber et al.
[58] |
EG: balance training (60 min/
session, 4X/wk for 4 wk, PI) CG: no balance training |
Isometric MVC (plantar flexion)
EMG median frequency of
the soleus and gastrocnemius medialis during
plantar-flexion MVC
EMG mean amplitude voltage of the soleus and gastrocnemius medialis during plantar-flexion MVC
Nerve stimulation twitch response of the soleus and gastrocnemius muscle |
No changes over time in EG or CG
Group 3 time interaction
(P < .01)
Improvements (P < .05) in EG Group 3 time interaction
(P< .05)
Improvements (P< .05) in EG
for both muscles
Group 3 time interaction
(P < .01)
Improvements (P , .05) in EG
No changes over time in EG or CG |
Gruber et al.
[59] Hoffman et al. [61] |
EG: balance training (60 min/session, 4x/wk for 4 wk, PI CG: no balance training
EG: balance training (10 min/session, 3x/wk for 10 wk, PI) CG: no balance training |
Isometric MVC (plantar flexion) Single-leg static postural sway(EO, EC) on a force plate |
No changes over time in EG
or CG Improvement in (P < .05) EG |
| Kean et al. [62] |
EG1: fixed foot balance training
(20 min/session, 4x/wk for 6 wk)
EG2: jump-landing balance training (20 min/session,
4x/wk for 6 wk)
CG: no balance training |
Isometric MVC (knee
flexion-extension, plantar flexion)
Prelanding EMG activity (mean RMS for the quadriceps, hamstrings, plantar flexors)
Postlanding EMG activity (mean RMS for the quadriceps, hamstrings, plantar flexors)
Single-leg stance (No. of ground contacts during a
30-s wobble-board
balance test) |
Improvement in (P < .05) EG
No group 3 time interaction
Main effect (P < .01) for
reactive rectus femoris activity |
| Kovacs et al. [64] |
EG: balance and jump landing training (20 min/session,
3x/wk for 4 wk, PI)
CG: basic exercise training
(10 min/session, 3x/wk for 4 wk) |
Single-leg postural sway (EO, EC) on a force plate
Single-leg postural sway
after jump landing (EO, EC)
on a force plate
Single-leg postural sway on a force plate with the skate on (EO) |
No group 3 time interaction
Improvement (P<, .05) in EG with EC Significantly greater improvements in EG (P < .05) |
| Rasool et al. [66] |
EG: balance training (5x/wk for 4 wk, PI)
CG: no balance training |
Star excursion balance test. |
Group 3 time interaction
(P < .01) Improvement (P <.01) in EG |
| Riemann et al. [67] |
EG: multiaxial coordination training on unstable platform (approximately 5
exercises with 10 repetitions
in 3 sets, 3x/wk for 4 wk, PI)
CG: no balance training |
Single-leg static postural sway on a force plate (EO, EC)
Single-leg postural control after jump landing on a force plate: (a) landing and (b) balance errors
Isokinetic MVC: (a) inversion, (b) dorsiflexion |
No group 3 time interaction |
| Schubert et al. [68] |
EG: balance training
(50 min/session, 4x/wk for 4 wk, PI) |
H-reflex during 2 tasks (plantar flexion and stance perturbation)
RFD (plantar flexion)
EMG during plantar flexion and stance perturbation (mean RMS for the soleus, gastrocnemius medialis, tibialis anterior) |
No changes in EG or C
No group 3 time interaction |
So¨derman et al.
[69] |
EG: balance training
(10–15 min, 7x/wk for4 wk, home based) CG: no balance training |
Single-leg dynamic postural
sway (balance index 5 moveable platform displacement) |
Decrease (P< .05) in EG nondominant leg |
| Yaggie et al. [71] |
EG: balance training (20 min/
session, 33/wk for 4 wk, PI) CG: no balance training |
Single-leg dynamic postural sway (EO) on a force plate
Single-leg stance time on a balance trainer
Shuttle run time
Jump height (jump and reach) |
Decrease in EG for total sway No change in CGDecreases in EG and CG
Decrease in EG
No change in CG
No group 3 time interaction |
Abbreviations: CG: Control Group; EC: Eyes Closed; EG: Experimental Group; EMG: Electromyography; EO: Eyes Open; LL: Left Leg; MVC: Maximum Contraction Force; PI: Progressive Intensity; RL: Right Leg
Yet changes in all results, one as postural influence, were in a predominant manner open when preparing conventions of more than 6 weeks were looked at by all of shorter-term protocols [1]. More precisely, although no training impacts were reported after 4 weeks [12], static postural influence on predictable stages enhanced after balance training of 6 weeks [1,11], 10 weeks [18], and 12 weeks [14]. Similar results were cut in offset utilizing the Star Excursion Balance Test [23] and single-leg position time on unstable boards [14,28]. Based on these findings it may be hypothesized that for conveying an outstanding sensorimotor adjustments, a base of minimum balance training of not less than 6 weeks is needed. In any case, no authors deliberately explored the inclination of balance training, preparing measurements, these presumptions stays theoretical. Hamman et al. [33,34] announced no distinction in static stability during 5 days of balance training and an once-week after weekly balance program everywhere the course of 5 weeks in volunteers. Due to every methodological restriction (e.g., inadequate report of interventions), we did not clear the consequences of these trials for this review.
Role of neuromuscular control
The essential objective in rehabilitation is to improve one's ability to function within the environment to perform the particular exercises of everyday living (ADL). The whole restoration procedure ought to be centered on enhancing the practical status of the patient. The idea of practical preparing is not new. Actually, practical preparing has been around for a long time. It is generally acknowledged that so as to improve at a particular action, or to get more grounded for a movement, one must practice that particular movement. Therefore, the practical movement for come back to ADL can be characterized as separating the particular exercises into a pecking order and after that performing them in an arrangement that considers the securing or reacquisition of that expertise [72,73].
From an authentic point of view, the rehabilitation procedure taking after injury has centered upon the reclamation of muscle strength, endurance, and joint flexibility without the part of the neuromuscular component. This is a typical error in the recovery process. We can't accept that clinical programs alone utilizing conventional strategies will prompt a sheltered come back to function. Constraining the recovery system to these customary programs alone regularly brings about a fragmented rebuilding of capacity and potentially prompts an expanded danger of reinjury. (Michael L Vnight and Gray Cook sports wounds Chapter 11 impaired neuromuscular control: Reactive neuromuscular training) [73].
The general target of the practical activity program is to give back the patient to the preinjury level as fast and as securely as could be expected under the circumstances. Specific training exercises activities should be designed restore both dynamic stability about the joint and specific ADL skills. So as to achieve this target, a fundamental principle of activity physiology is utilized. The SAID (particular adjustments to forced requests) guideline expresses that the body will adjust to the anxiety and strain set upon it. Patients can't succeed in ADL on the off chance that they have not been arranged to meet the greater part of the requests of their particular action. Neuromuscular training (NT) is not planned to supplant conventional recovery but instead to help bridge the gap left traditional rehabilitation in a reciprocal manner through proprioceptive and balance training so as to advance a more useful come back to action. The principle goal of the NT program is to encourage the oblivious procedure of translating and incorporating the peripheral sensations received by the CNS into proper motor responses. (Michael L Vnight and Gray Cook sports wounds Chapter 11 impaired neuromuscular control: Reactive neuromuscular training) [73].
About the normal healthy joint, both static and dynamic stabilizers serve to give support. The role of the capsuloligamentous tissues in the dynamic limitation of the joint has been settled in the literature. Despite the fact that the essential part of these structures will be mechanical in nature by giving auxiliary bolster and adjustment to the joint, the capsuloligamentous tissues additionally assume a critical tangible part by identifying joint position and movement. The afferent feedback from the receptors in capsuloligamentous structures extends specifically to the reflex and cortical pathways, in this manner intervening responsive muscle action for element limitation. The efferent motor reaction that results from the optional data is called neuromuscular control. Sensory information is sent to the CNS to be prepared, and proper motor activities are executed. (Michael L Vnight and Gray Cook sports wounds Chapter 11 impaired neuromuscular control: Reactive neuromuscular training) [73].
Neuromuscular control exercises ought to be started into the general rehabilitation program once satisfactory healing has occurred. The movement to these exercises is predicated on the competitor acceptably finishing the exercises that are considered requirements for the action being considered. Remembering this, the movement of exercises must be objective arranged and particular to the assignments that will be anticipated from the athlete.
The general movement for exercises to create dynamic neuromuscular control is from moderate pace to quick speed exercises, from low-constrain to high-compel exercises, and from controlled to uncontrolled exercises. At first these activities ought to bring out a parity response or weight move in the lower furthest points and at last advance to a development design. These responses can be as straightforward as a static control with almost no noticeable development or as unpredictable as an element plyometric reaction obliging unstable increasing speed, deceleration, or alter in course. The activities will permit the clinician to test the patient utilizing visual and/or proprioceptive data through tubing and different gadgets (medicine balls, foam rolls, visual obstacles). In spite of the fact that these activities will enhance physiologic parameters, they are exceptionally intended to encourage neuromuscular responses. Hence, the clinician must be concerned with the kinaesthetic information and nature of the development designs instead of the specific number of sets and repetitions. When weakness happens, motor control gets to be poor and all preparation impacts are lost. Therefore, during the activity movement, all parts of ordinary motor control/development ought to be watched. These should include isometric, concentric, and eccentric muscle control; articular stacking and emptying; equalization control amid weight moving and bearing changes; controlled speeding up and deceleration; and demonstration of both conscious and unconscious control. (Michael L Vnight and Gray Cook sports wounds Chapter 11 impaired neuromuscular control: Reactive neuromuscular training) [73].
Limitations
A limitation of this crude study is that the configuration material was not an orderly audit of the writing material and not a masse important writing was proposed for incorporation. Subsequently, not all important substance was checked on. Also, in light of the fact that everything being equivalent this was not an efficient survey; the nature of article substance was not basically evaluated or assessed. The task of articles was that exclusively of the writer; in this manner, there was some determination and elucidation of word predisposition. Later on, ideally more thorough routines ought to be considered for writing reviews.
Conclusion
i. There has been expanded consideration to the advancement of balance and proprioception in the recovery and reconditioning of athletes after injury. It is accepted that damage brings about changed somatosensory information that impacts neuromuscular control.
ii. If static and dynamic balance and neuromuscular control are not re-set up taking after damage, then the patient will be vulnerable to repetitive injury and his/her execution may decay.
iii. The following rules should be employed when designing the NT program: Make sure that the activity program is particular to the tolerant's requirements. The most vital thing to consider amid the rehabilitation of patients is that they ought to be performing useful exercises that recreate their ADL requirements. This guideline applies to the particular joints included as well as the pace and adequacy of development needed in ADL.
iv. Practice does give off an impression of being undertaking particular in both athletes and individuals who have motor control deficits. As retraining of offset proceeds with, it is best to practice complex abilities in their total instead of in confinement in light of the fact that the aptitudes will exchange all the more successfully.
v. Make sure to incorporate a lot of "controlled disarray" in the system. Surprising exercises with the ADL are by nature flimsy. The more the patient practices in this sort of environment, the better he/she will respond under unrehearsed conditions.
vi. Progress from straight plane to multiplane movement patterns. In ADL, development does not happen along a single joint or plane of development. Consequently, practice for the dynamic chain must include each of the three planes all the while.
vii. Have causative cures as a piece of the recovery process. The reason for the harm should inevitably turn into a piece of the cure. On the off chance that turn and deceleration were the reason for the harm, then utilize this as a piece of the restoration program in preparation for return to activity.
viii. Be dynamic in nature. Keep in mind to advance from easy to complex. The capacity movement separates an action into its segment parts and after that performs them in an arrangement that considers the securing or reacquisition of the action. Basic conditioning and skill obtaining must be gained before conditioning and aptitude procurement.
9493
References
- Garrick JG (1977) The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med 5: 241-242.
- Hosea TM, Carey CC, Harrer MF (2000) The gender issue: epidemiology of ankle injuries in athletes who participate in basketball. Clin Orthop Relat Res : 45-49.
- Kannus P, Renström P (1991) Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization. J Bone Joint Surg Am 73: 305-312.
- Smith RW, Reischl SF (1986) Treatment of ankle sprains in young athletes. Am J Sports Med 14: 465-471.
- Ekstrand J, Tropp H (1990) The incidence of ankle sprains in soccer. Foot Ankle 11: 41-44.
- Milgrom C, Shlamkovitch N, Finestone A, Eldad A, Laor A, et al. (1991) Risk factors for lateral ankle sprain: a prospective study among military recruits. Foot Ankle 12: 26-30.
- Bahr R, Bahr IA (1997) Incidence of acute volleyball injuries: a prospective cohort study of injury mechanisms and risk factors. Scand J Med Sci Sports 7: 166-171.
- McKay GD, Goldie PA, Payne WR, Oakes BW (2001) Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med 35: 103-108.
- Yeung MS, Chan KM, So CH, Yuan WY (1994) An epidemiological survey on ankle sprain. Br J Sports Med 28: 112-116.
- Harrington KD (1979) Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am 61: 354-361.
- Gross P, Marti B (1999) Risk of degenerative ankle joint disease in volleyball players: study of former elite athletes. Int J Sports Med 20: 58-63.
- Safran MR, Benedetti RS, Bartolozzi AR 3rd, Mandelbaum BR (1999) Lateral ankle sprains: a comprehensive review: part 1: etiology, pathoanatomy, histopathogenesis, and diagnosis. Med Sci Sports Exerc 31: S429-437.
- Reid DC (1992) Sports injury assessment and rehabilitation. New York: Churchill Livingston Inc p 215-268.
- Wester JU, Jespersen SM, Nielsen KD, Neumann L (1996) Wobble board training after partial sprains of the lateral ligaments of the ankle: a prospective randomized study. J Orthop Sports Phys Ther 23: 332-336.
- Munn J, Beard DJ, Refshauge KM, Lee RY (2003) Eccentric muscle strength in functional ankle instability. Med Sci Sports Exerc 35: 245-250.
- Beynnon BD, Vacek PM, Murphy D, Alosa D, Paller D (2005) First-time inversion ankle ligament trauma: the effects of sex, level of competition, and sport on the incidence of injury. Am J Sports Med 33: 1485-1491.
- Olmsted LC, Vela LI, Denegar CR, Hertel J (2004) Prophylactic Ankle Taping and Bracing: A Numbers-Needed-to-Treat and Cost-Benefit Analysis. J Athl Train 39: 95-100.
- LeBrun CT, Krause JO (2005) Variations in mortise anatomy. Am J Sports Med 33: 852-855.
- Sawkins K, Refshauge K, Kilbreath S, Raymond J (2007) The placebo effect of ankle taping in ankle instability. Med Sci Sports Exerc 39: 781-787.
- DiStefano LJ, Padua DA, Brown CN, Guskiewicz KM (2008) Lower extremity kinematics and ground reaction forces after prophylactic lace-up ankle bracing. J Athl Train 43: 234-241.
- Takao M, Uchio Y, Naito K, Fukazawa I, Ochi M (2005) Arthroscopic assessment for intra-articular disorders in residual ankle disability after sprain. Am J Sports Med 33: 686-692.
- Andersen TE, Floerenes TW, Arnason A, Bahr R (2004) Video analysis of the mechanisms for ankle injuries in football. Am J Sports Med 32: 69S-79S.
- Giza E, Fuller C, Junge A, Dvorak J (2003) Mechanisms of foot and ankle injuries in soccer. Am J Sports Med 31: 550-554.
- Purcell SB, Schuckman BE, Docherty CL, Schrader J, Poppy W (2009) Differences in ankle range of motion before and after exercise in 2 tape conditions. Am J Sports Med 37: 383-389.
- Borowski LA, Yard EE, Fields SK, Comstock RD (2008) The epidemiology of US high school basketball injuries, 2005-2007. Am J Sports Med 36: 2328-2335.
- Halasi T, Kynsburg A, Tállay A, Berkes I (2004) Development of a new activity score for the evaluation of ankle instability. Am J Sports Med 32: 899-908.
- Hyde T (1997) Conservative management of sports injury. Baltimore: Williams & Wilkins, Philadelphia, United States. p 483-493.
- Banks AS, Downey MS, Martin DE, Miller SJ (2001) Foot and ankle surgery. Lipincott Williams & Wilkins, Philadelphia, United States. p 1898-1902.
- Balduini FC, Tetzlaff J (1982) Historical perspectives on injuries of the ligaments of the ankle. Clin Sports Med 1: 3-12.
- Garrick JG, Requa RK (1973) Role of external support in the prevention of ankle sprains. Med Sci Sports 5: 200-203.
- Smith RW, Reischl SF (1986) Treatment of ankle sprains in young athletes. Am J Sports Med 14: 465-471.
- Yeung MS, Chan KM, So CH, Yuan WY (1994) An epidemiological survey on ankle sprain. Br J Sports Med 28: 112-116.
- Itay S, Ganel A, Horoszowski H, Farine l (1982) Clinical and functional status following lateral ankle sprains. Orthop Rev 11: 73-76.
- Brand RL, Black HM, Cox JS (1977) The natural history of inadequately treated ankle sprain. Am J Sports Med 5: 248-249.
- Harrington KD (1979) Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am 61: 354-361.
- Emery CA, Cassidy JD, Klassen TP, Rosychuk RJ, Rowe BH (2005) Effectiveness of a home-based balance-training program in reducing sports-related injuries among healthy adolescents: a cluster randomized controlled trial. CMAJ 172: 749–754.
- McGuine TA, Keene JS (2006) The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med 34: 1103-1111.
- McKeon PO, Hertel J (2008) Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective? J Athl Train 43: 305-315.
- Hewett TE, Paterno MV, Myer GD (2002) Strategies for enhancing proprioception and neuromuscular control of the knee. Clin Orthop Relat Res : 76-94.
- Takao M, Uchio Y, Naito K, Fukazawa I, Ochi M (2005) Arthroscopic assessment for intra-articular disorders in residual ankle disability after sprain. Am J Sports Med 33: 686-692.
- Van Os AG, Bierma-Zeinstra SMA, Verhagen AP, De Bie RA, Luijsterburg PAJ, et al. (2005) Comparison of conventional treatment and supervised rehabilitation for treatment of acute lateral ankle sprains: a systematic review of the literature. J Orthop Sports Phys Ther 35: 95-105.
- Chorley JN (2005) Ankle sprain discharge instructions from the emergency department. Pediatr Emerg Care 21: 498-501.
- Veenema KR (2000) Ankle sprain: primary care evaluation and rehabilitation. J Musculoske Med 17: 563-576.
- Karlsson J, Bergsten T, Lansinger O, Peterson L (1989) Surgical treatment of chronic lateral instability of the ankle joint. A new procedure. Am J Sports Med 17: 268-273.
- Inman VT (1976) In the Joints of the Ankle, pp. 1-117, Williams & Wilkins, Baltimore.
- Root MC, Weed JH, Orien WP (1977) In Normal and Abnormal Function of the Foot pp.1-161,295-346, Clinical Biomechanics Corporation, Los Angeles, United States.
- Freeman MA (1965) Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br 47: 669-677.
- Konradsen L, Ravn JB (1990) Ankle instability caused by prolonged peroneal reaction time. Acta Orthop Scand 61: 388-390.
- Vaes PH, Duquet W, Casteleyn PP, Handelberg F, Opdecam P (1998) Static and dynamic roentgenographic analysis of ankle stability in braced and nonbraced stable and functionally unstable ankles. Am J Sports Med 26: 692-702.
- Karlsson J, Bergsten T, Lansinger O, Peterson L (1989) Surgical treatment of chronic lateral instability of the ankle joint. A new procedure. Am J Sports Med 17: 268-273.
- Chrisman OD, Snook GA (1969) Reconstruction of lateral ligament tears of the ankle: an experimental study and clinical evaluation of seven patients treated by a new modification of the Elmslie procedure. J. Bone Joint Surg. 51: 904-912.
- Baker AG, Webright WG, Perrin DH (1998) Effect of a ‘‘T-band’’ kick training protocol on postural sway. J Sport Rehabil 7: 122–127.
- Balogun JA, Adesinasi CO, Marzouk DK (1992) The effects of a wobble board exercise training program on static balance performance and strength of lower extremity muscles. Physiotherapy Can 44: 23–30.
- Cox ED, Lephart SM, Irrgang JJ (1993) Unilateral balance training of non-injured individuals and the effects on postural sway. J Sport Rehabil 2: 87–96.
- Cressey EM, West CA, Tiberio DP, Kraemer WJ, Maresh CM (2007) The effects of ten weeks of lower-body unstable surface training on markers of athletic performance. J Strength Cond Res 21: 561-567.
- Gioftsidou A, Malliou P, Pafis G, Beneka A, Godolias G, et al. (2006) The effects of soccer training and timing of balance training on balance ability. Eur J Appl Physiol 96: 659-664.
- Gruber M, Gruber SB, Taube W, Schubert M, Beck SC, et al. (2007) Differential effects of ballistic versus sensorimotor training on rate of force development and neural activation in humans. J Strength Cond Res 21: 274-282.
- Gruber M, Taube W, Gollhofer A, Beck S, Amtage F, et al. (2007) Training-specific adaptations of H- and stretch reflexes in human soleus muscle. J Mot Behav 39: 68-78.
- Heitkamp HC, Horstmann T, Mayer F, Weller J, Dickhuth HH (2001) Gain in strength and muscular balance after balance training. Int J Sports Med 22: 285-290.
- Hoffman M, Payne VG (1995) The effects of proprioceptive ankle disk training on healthy subjects. J Orthop Sports Phys Ther 21: 90-93.
- Kean CO, Behm DG, Young WB (2006) Fixed foot balance training increases rectus femoris activation during landing and jump height in recreationally active women. J Sports Sci Med 5: 138–148.
- Kollmitzer J, Ebenbichler GR, Sabo A, Kerschan K, Bochdansky T (2000) Effects of back extensor strength training versus balance training on postural control. Med Sci Sports Exerc 32: 1770-1776.
- Kovacs EJ, Birmingham TB, Forwell L, Litchfield RB (2004) Effect of training on postural control in figure skaters: a randomized controlled trial of neuromuscular versus basic off-ice training programs. Clin J Sport Med 14: 215-224.
- Myer GD, Ford KR, Brent JL, Hewett TE (2006) The effects of plyometric vs. dynamic stabilization and balance training on power, balance, and landing force in female athletes. J Strength Cond Res 20: 345-353.
- Rasool J, George K (2007) The impact of single-leg dynamic balance training on dynamic stability. Phys Ther Sport 8: 177–184.
- Riemann BL, Tray NC, Lephart SM (2003) Unilateral multiaxial coordi- nation training and ankle kinesthesia, muscle strength, and postural control. J Sport Rehabil 12: 13–30.
- Schubert M, Beck S, Taube W, Amtage F, Faist M, et al. (2008) Balance training and ballistic strength training are associated with task-specific corticospinal adaptations. Eur J Neurosci 27: 2007-2018.
- So¨derman K, Werner S, Pietila¨T, Engstro¨m B, Alfredson H (2000) Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study. Knee Surg Sports Traumatol Arthrosc 8: 356–363.
- Taube W, Kullmann N, Leukel C, Kurz O, Amtage F, et al. (2007) Differential reflex adaptations following sensorimotor and strength training in young elite athletes. Int J Sports Med 28: 999-1005.
- Yaggie JA, Campbell BM (2006) Effects of balance training on selected skills. J Strength Cond Res 20: 422-428.
- Hamman RG, Mekjavic I, Mallinson AI, Longridge NS (1992) Training effects during repeated therapy sessions of balance training using visual feedback. Arch Phys Med Rehabil 73: 738-744.
- Voight ML, Cook G (2014) Sports Wounds Chapter 11 Impaired neuromuscular control: Reactive neuromuscular training.